Published online Jul 6, 2023. doi: 10.12998/wjcc.v11.i19.4677
Peer-review started: February 16, 2023
First decision: March 24, 2023
Revised: March 28, 2023
Accepted: May 8, 2023
Article in press: May 8, 2023
Published online: July 6, 2023
Processing time: 134 Days and 3.9 Hours
Spontaneous intracranial hypotension syndrome is a relatively uncommon neurological disorder of unknown etiology with a good prognosis. Cerebral venous sinus thrombosis is a specific type of cerebrovascular disease caused by multiple etiologies of cerebral venous sinus or vein thrombosis that obstructs cerebral venous return and is associated with impaired cerebrospinal fluid absorption; this entity is rarely seen clinically. Spontaneous intracranial hy
A 29-year-old young woman presented with postural headache. Lumbar puncture suggested a pressure of 50 mmH2O (normal 80 mmH2O-180 mmH2O), and magnetic resonance imaging cerebral venography suggested thrombosis of the supratentorial sinus. These findings were considered indicative of cerebral venous sinus thrombosis due to spontaneous intracranial hypotension syndrome after ruling out immunological causes, tumor, infection, abnormal coagulation mechanism, and hypercoagulable state, etc. She was treated with rehydration and low-molecular heparin anticoagulation for 15 d, and follow-up magnetic resonance imaging cerebral venography suggested resolution of the thrombus. The patient had complete improvement of her headache symptoms.
Spontaneous intracranial hypotension syndrome is one of the rare causes of cerebral venous sinus thrombosis, which is frequently misdiagnosed or missed and deserves consideration by clinicians during differential diagnosis. Dehydration should be avoided in such patients, and early rehydration and anticoagulation therapy are effective treatment options.
Core Tip: In patients with cerebral venous sinus thrombosis of unknown origin, spontaneous intracranial hypotension syndrome may be considered as a rare cause. Lumbar puncture and cerebral venous sinus angiography are important diagnostic tools.
- Citation: Huang P. Rare cause of cerebral venous sinus thrombosis: Spontaneous intracranial hypotension syndrome: A case report. World J Clin Cases 2023; 11(19): 4677-4683
- URL: https://www.wjgnet.com/2307-8960/full/v11/i19/4677.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i19.4677
Intracranial hypotension syndrome is a group of clinical syndromes characterized by postural headache and cerebrospinal fluid (CSF) pressure < 60 mmH2O. Spontaneous intracranial hypotension syndrome (SIH) may be considered in cases of intracranial hypotension with unknown etiology. The annual incidence of SIH is estimated at 4/100000[1]. Cerebral venous sinus thrombosis (CVST) refers to a special type of cerebrovascular disease caused by cerebral venous sinus or venous thrombosis. CVST may arise due to a variety of causes, and obstructs cerebral venous return and is frequently accom
The patient, a 29-year-old female, was admitted to the hospital with a 3-d postural headache.
Three days prior to admission, the patient had a headache after waking up in the morning. The headache was located in the bilateral temporal and occipital areas, with persistent, severe, and unbearable distending pain. The headache was accompanied by a pulling pain in the back of the neck, which worsened with sitting or standing positions, and improved in a lying position. The patient also endorsed nausea and vomiting several times. She denied loss of consciousness, fever, limb convulsions, incontinence, slurred speech, and limb weakness.
The patient had no pertinent past illness history.
The patient had no pertinent personal or family history.
At admission, the patient’s vital signs were as follows: Temperature 36.3℃, pulse 64 beats/min, respiration rate 19 breaths/min, and blood pressure 137/79 mmHg. No significant abnormalities were seen in the heart, lungs, or abdomen. The patient was clearly conscious, fluent in speech, and had normal orientation. The pupils were round and equal in size (about 3 mm in diameter) with a sensitive light reflex and no nystagmus. There was no facial tongue palsy and the pharyngeal reflex was present. The muscle tone of the extremities was normal and the muscle strength was grade 5. Sensory examination was normal. Bilateral pathological signs were negative, meningeal stimulation signs were negative, and tendon reflexes of all 4 limbs were present and symmetrical.
The following blood tests were performed: Liver function, renal function, serum electrolytes, thyroid function, coagulopathy, markers of myocardial injury, syphilis, HIV, glycosylated hemoglobin, lipids, rheumatoid factor, C-reactive protein, antistreptolysin-O, erythrocyte sedimentation rate, immune panel, and tumor markers. All laboratory values were within reference ranges. An electrocardiogram demonstrated sinus bradycardia.
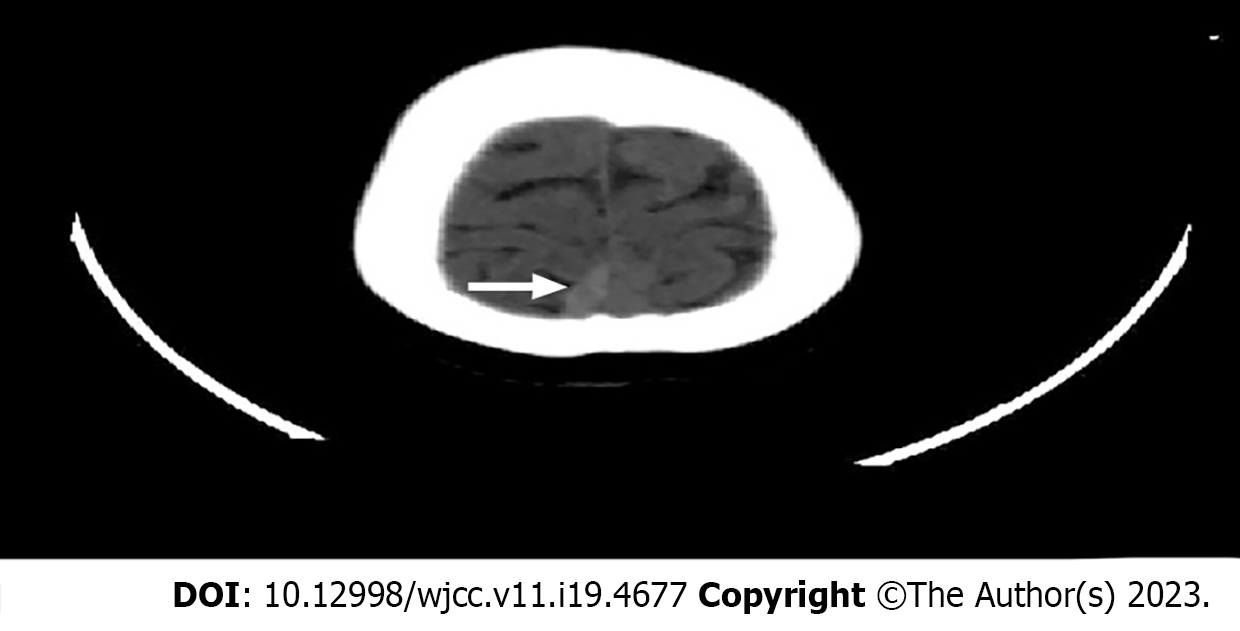
Computed tomography of the head suggested a nodular, linear high-density shadow in the right parietal cerebral cortex, superior parietal sagittal sinus with a differential of venous embolism or vascular malformation with thrombosis (Figure 1). No abnormality was seen in brain parenchyma, and magnetic resonance imaging (MRI) with magnetic resonance venography (MRV) was recommended (Figure 2). Computed tomographic venography of the head and neck suggested a hypodense filling defect in the cortical veins of the right parietal sagittal sinus, consistent with venous thrombosis (Figure 3).
An opening pressure of 50 mmH2O was measured by uncomplicated lumbar puncture, and the CSF was colorless with no significant laboratory abnormalities. A cranial MRI enhancement scan demonstrated a localized filling defect in the right superior sagittal sinus strip with striped low signal in weighted sequences (T1WI and T2WI), suggesting a possible focal thrombus.
Taking into consideration the clinical symptoms, absence of medical history, the physical exam findings, and the laboratory and radiographic findings, a final diagnosis of spontaneous intracranial hypotension syndrome with cerebral venous system thrombosis was made.
The patient was admitted to the hospital as subarachnoid hemorrhage could not be excluded. Initial treatment included nimodipine to prevent vasospasm, rehydration, and symptomatic analgesia. The patient's headache symptoms were partially resolved after 2 d of treatment. After the diagnosis of spontaneous intracranial hypotension syndrome with cerebral venous system thrombosis was clear, the treatment was adjusted to include rehydration and anticoagulation with low molecular weight heparin (5000 IU every 12 h via subcutaneous injection). After 13 d of treatment, the patient's headache symptoms completely resolved, and she was discharged on oral warfarin anticoagulation and recommended to increase her water intake to 2000 mL-3000 mL per d).
Fifteen d after discharge, the patient had no further postural headache symptoms, and a follow-up head MRI with MRV suggested no residual venous sinus thrombosis (Figure 4). Three mo later, the patient was seen again in follow-up, and she again endorsed no further headache symptoms, and anticoagulant therapy was discontinued.
The presenting symptom of this patient was postural change-related headache. Intracranial hypotension syndrome was considered after uncomplicated lumbar puncture and related examinations were performed. The patient had no history of infection or fever during or near the onset of symptoms, the CSF opening pressure was low, and the CSF was normal on laboratory evaluation, so infectious meningitis could be excluded. There was no nodule-like enhancement on MRI, there were no features of hypertrophic cranial pachymeningitis, and there were no abnormalities on immunological examination, so hypertrophic cranial pachymeningitis was excluded. The patient’s symptoms followed an acute course, there was no blood in the CSF, no subarachnoid hyperdensity was seen on computed to
In addition to SIH, further refinement of head and neck angiography in this patient suggested CVST, which is a rare and potentially fatal cerebrovascular disease with an annual incidence of 0.5/100000, accounting for 0% to 3% of all ischemic strokes[9]. The order of occurrence of spontaneous intracranial hypotension syndrome and cerebral venous thrombosis has been uncertain, however, with the advancement of science and technology, it has been confirmed that spontaneous intracranial hypotension syndrome is one of the risk factors for CVST[3]. The pathophysiological mechanism is not definitively known, but several hypotheses have been proposed. First, the Monro-Kellie theory states that due to the loss of CSF, the compensatory blood volume in the venous cavity increases, causing the cerebral venous system to dilate resulting in the slowing and stagnation of venous blood flow promoting thrombosis[10]. In support of this theory, Kranz et al[11] found that patients with low intracranial pressure had dilated cerebral venous sinuses and that their cross-sectional area was 70% larger than the corresponding section in normal subjects. Another possibility is outlined by the theory of abnormal CSF buoyancy, which suggests that the loss of CSF buoyancy results in intracranial tissue structure sagging, pulling the cerebral veins and venous sinuses leading to disruption of venous hemodynamics or even stagnation of venous blood flow[12]. A final possible mechanism to consider is that if a CSF loss occurs, this can reduce the absorption of CSF by the venous system, resulting in increased viscosity and hypercoagulability of blood in the cerebral venous sinus cavity, thus increasing the risk of thrombosis[13].
Treatment of SIH includes conservative approaches (e.g., bed rest, massive fluid replacement, oral caffeine, hormone therapy), epidural blood patching, epidural saline injection, surgical treatments (e.g., CSF leak repair or other cause-specific procedures), and various treatments for complications[3]. One study showed the success rate of conservative treatment to be approximately 24.47%, and suggested that hormone therapy may be a potential first-line treatment option. The use of hormones was proposed to significantly improve the clinical symptoms of SIH and reduce the probability of need for invasive epidural blood patching[14,15]. In addition, hormone therapy may also be effective in improving postural headache in some patients who fail epidural blood patch treatment[16]. However, the ideal duration, type, dose, and route of administration of hormones are still inconclusive; however, the majority of patients could have symptom relief within days of administration[17]. Hormones may exert their pharmacological effects by: (1) Ameliorating brain edema and inhibiting inflammation caused by brain herniation; (2) Inhibiting meningeal inflammation and that of CSF cells or proteins, thus reducing CSF leakage; (3) Inhibiting excessive absorption of CSF; and (4) Promoting reabsorption of CSF from the epidural space and increasing the overall CSF volume[18].
In cases where SIH symptoms persist or are associated with CVST, epidural hemopexy is recommended abroad to close the CSF leak before treating CVST[19,20]. Treatment of CVST includes anticoagulation and endovascular intervention, with anticoagulation being the first-line treatment option. Anticoagulation is an important treatment modality in patients with SIH with CVST. Endovascular therapy is only indicated in patients with CVST with severe thrombotic load, psychiatric abnormalities during the course of the disease, or worsening symptoms with systemic anticoagulants.
In conclusion, SIH can often lead to the rare complication of CVST, which is frequently misdiagnosed or missed in clinical practice. For patients with postural headache with focal neurological deficits or imaging findings of venous sinus thrombosis, clinicians should consider the possibility of coexistence of both diseases, and lumbar puncture and cerebral venous sinus angiography should be performed. Patients whose clinical symptoms and imaging improve after conservative management with rehydration and anticoagulation likely do not need epidural hemorrhage patching, but should be monitored for intracranial hemorrhage.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Clinical neurology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Arboix A, Spain; Sidoti A S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Ma YJ
| 1. | Schievink WI, Maya MM, Moser FG, Simon P, Nuño M. Incidence of spontaneous intracranial hypotension in a community: Beverly Hills, California, 2006-2020. Cephalalgia. 2022;42:312-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 2. | Ferrante E, Trimboli M, Rubino F. Spontaneous intracranial hypotension: review and expert opinion. Acta Neurol Belg. 2020;120:9-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 52] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 3. | Ferrante E, Trimboli M, Petrecca G, Allegrini F. Cerebral venous thrombosis in spontaneous intracranial hypotension: A report of 8 cases and review of the literature. J Neurol Sci. 2021;425:117467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Arboix A, Jiménez C, Massons J, Parra O, Besses C. Hematological disorders: a commonly unrecognized cause of acute stroke. Expert Rev Hematol. 2016;9:891-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 63] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 5. | Schievink WI. Spontaneous Intracranial Hypotension. N Engl J Med. 2021;385:2173-2178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 91] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 6. | Kranz PG, Malinzak MD, Amrhein TJ, Gray L. Update on the Diagnosis and Treatment of Spontaneous Intracranial Hypotension. Curr Pain Headache Rep. 2017;21:37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 54] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 7. | Kranz PG, Tanpitukpongse TP, Choudhury KR, Amrhein TJ, Gray L. Imaging Signs in Spontaneous Intracranial Hypotension: Prevalence and Relationship to CSF Pressure. AJNR Am J Neuroradiol. 2016;37:1374-1378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 71] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 8. | D'Antona L, Jaime Merchan MA, Vassiliou A, Watkins LD, Davagnanam I, Toma AK, Matharu MS. Clinical Presentation, Investigation Findings, and Treatment Outcomes of Spontaneous Intracranial Hypotension Syndrome: A Systematic Review and Meta-analysis. JAMA Neurol. 2021;78:329-337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 181] [Article Influence: 45.3] [Reference Citation Analysis (0)] |
| 9. | Arboix A, Bechich S, Oliveres M, García-Eroles L, Massons J, Targa C. Ischemic stroke of unusual cause: clinical features, etiology and outcome. Eur J Neurol. 2001;8:133-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 67] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Mokri B. The Monro-Kellie hypothesis: applications in CSF volume depletion. Neurology. 2001;56:1746-1748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 592] [Cited by in RCA: 617] [Article Influence: 25.7] [Reference Citation Analysis (0)] |
| 11. | Kranz PG, Tanpitukpongse TP, Choudhury KR, Amrhein TJ, Gray L. How common is normal cerebrospinal fluid pressure in spontaneous intracranial hypotension? Cephalalgia. 2016;36:1209-1217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 60] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 12. | Haritanti A, Karacostas D, Drevelengas A, Kanellopoulos V, Paraskevopoulou E, Lefkopoulos A, Economou I, Dimitriadis AS. Spontaneous intracranial hypotension: clinical and neuroimaging findings in six cases with literature review. Eur J Radiol. 2009;69:253-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Savoiardo M, Armenise S, Spagnolo P, De Simone T, Mandelli ML, Marcone A, Morciano G, Andreula C, Mea E, Leone M, Chiapparini L. Dural sinus thrombosis in spontaneous intracranial hypotension: Hypotheses on possible mechanisms. J Neurol. 2006;253:1197-1202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Ferro JM, Aguiar de Sousa D. Cerebral Venous Thrombosis: an Update. Curr Neurol Neurosci Rep. 2019;19:74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 116] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 15. | Pascual LF, Santos S, Escalza I, Iñiguez C, Morales-Asín F. Spontaneous intracranial hypotension: quick clinical and magnetic resonance imaging response to corticosteroids. A case report. Headache. 2002;42:359-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Hannerz J, Dahlgren G, Irestedt L, Meyerson B, Ericson K. Treatment of idiopathic intracranial hypotension: cervicothoracic and lumbar blood patch and peroral steroid treatment. Headache. 2006;46:508-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Goto S, Ohshima T, Yamamoto T, Shimato S, Nishizawa T, Kato K. Successful steroid treatment of coma induced by severe spontaneous intracranial hypotension. Nagoya J Med Sci. 2016;78:229-236. [PubMed] [DOI] [Full Text] |
| 18. | Tonello S, Grossi U, Trincia E, Zanus G. First-line steroid treatment for spontaneous intracranial hypotension. Eur J Neurol. 2022;29:947-949. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 19. | Zhang D, Wang J, Zhang Q, He F, Hu X. Cerebral Venous Thrombosis in Spontaneous Intracranial Hypotension: A Report on 4 Cases and a Review of the Literature. Headache. 2018;58:1244-1255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 20. | Paris P, Joubert M, Clavelou P, Moisset X. Cerebral venous thrombosis due to spontaneous intracranial hypotension: Reperfusion after epidural blood patch only. Rev Neurol (Paris). 2021;177:1039-1041. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |