Published online Jun 26, 2023. doi: 10.12998/wjcc.v11.i18.4454
Peer-review started: March 20, 2023
First decision: April 19, 2023
Revised: April 27, 2023
Accepted: May 22, 2023
Article in press: May 22, 2023
Published online: June 26, 2023
Processing time: 95 Days and 4.4 Hours
In this letter to the editor, the authors discuss the findings and shortcomings of a published retrospective study, including 120 patients undergoing surgery for gastric or colon cancer under general anesthesia. The study focused on perioperative dynamic respiratory and hemodynamic disturbances and early postsur
Core Tip: Letter to the editor discussing the findings and shortcomings of an article published in World J Clin Cases of a retrospective study, including 120 patients having undergone gastric or colon cancer surgery under general anesthesia, focusing on the perioperative dynamic respiratory and respiratory and hemodynamic disturbances with an early postsurgical inflammatory response.
- Citation: Idrissov KS, Mynbaev OA. Erroneous presentation of respiratory-hemodynamic disturbances and postsurgical inflammatory responses in patients having undergone abdominal cavity cancer surgery. World J Clin Cases 2023; 11(18): 4454-4457
- URL: https://www.wjgnet.com/2307-8960/full/v11/i18/4454.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i18.4454
With great interest, we read an article by Wang et al[1] recently published in World J Clin Cases 2022; 10(33): 12146-12155. The authors examined the anesthesiology management in 120 patients undergoing gastric or colon cancer surgery under general anesthesia. They focused on the effects triggered by the surgery, such as dynamic respiratory and hemodynamic changes with the subsequent postsurgical inflammatory response. Next, these patients were equally divided into two groups. All patients were ventilated with 6.0 mL/kg of tidal volume during general anesthesia. Patients in group A were managed with positive end-expiratory pressure (PEEP) of 5.0 cm of water, whereas in group B the PEEP was maintained on 8.0 cm of water. At four points in time, blood gas, respiratory and hemodynamic measurements were performed: before anesthesia induction (T0), during mechanical ventilation 10 min and 60 min (T1 and T2), and finally after catheter removal (T3). Blood samples were collected at 0 and 4 h after surgery to explore the inflammatory factors (TNF-α, IL-6, and IL-10).
The authors concluded that in protecting the lung ventilatory function of patients, lower PEEP with a 5.0 cm of water regimen was more effective than higher PEEP with 8.0 cm of water, resulting in better effects concerning hemodynamic stability and inflammatory reactions[1].
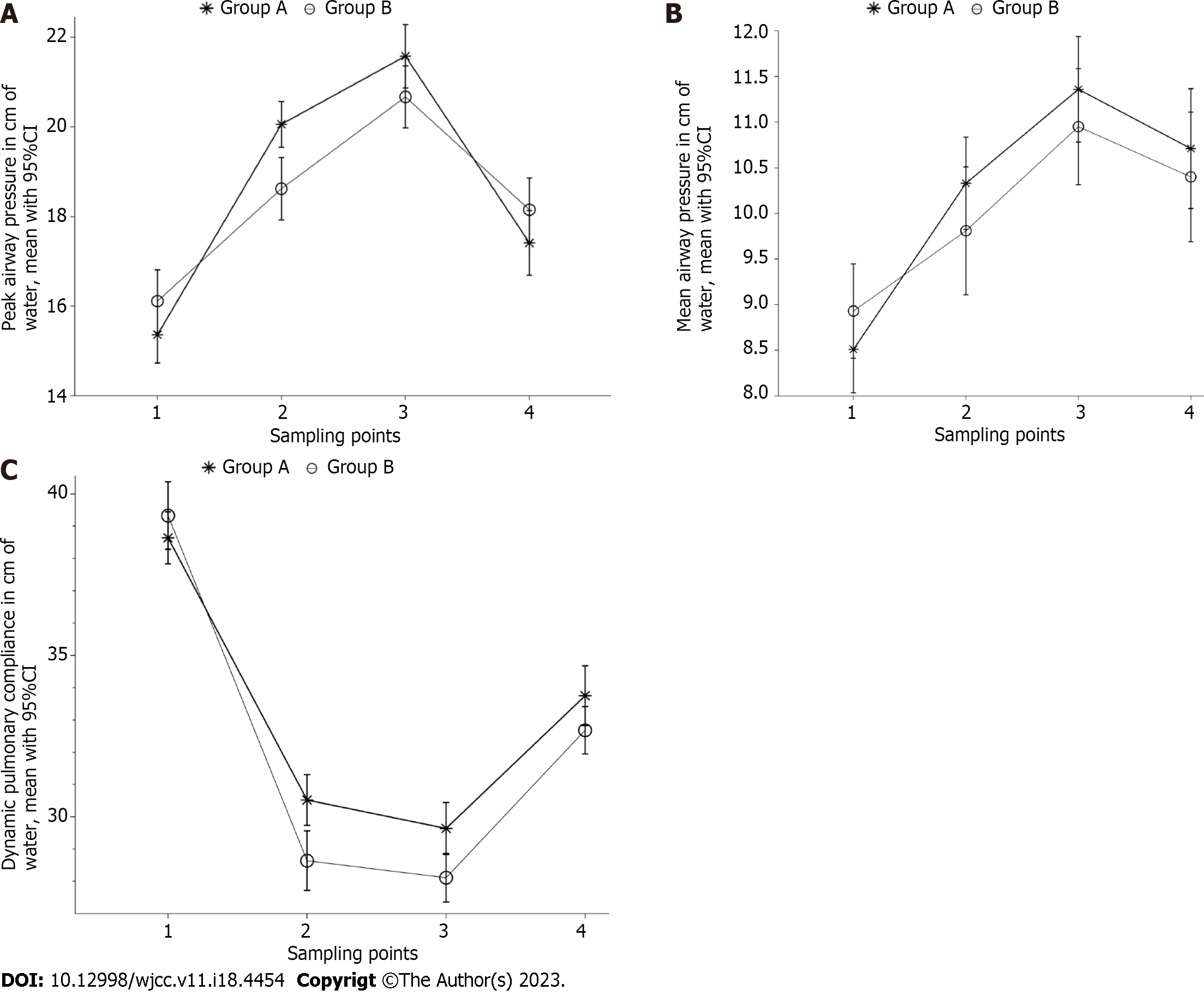
While reading this article, the data presentation and statistical analysis puzzled us: the authors, having performed repeated measurements in four-time points in two groups of patients with their equal number in groups[1], should have applied an appropriate study design and statistical tests. To illustrate our opinion, we reanalyzed the results of the perioperative airway compliance indexes in Table 4 from the original article[1] using two-way multiple measures ANOVA with post hoc Tukey's multiple comparisons tests using Graph Pad Prism 8.4.2 software and generated figures with dynamic perioperative airway compliance changes in different sampling points (Figure 1) for airway pressures (peak – A and mean – B) values and pulmonary compliance (C) with P values of differences in Table 1. This reanalysis resulted in significant interaction (P = 0.0009) and time impact (P < 0.0001) on peak airway pressure parameters (Figure 1A) with no significant differences neither between the total values of groups A and B (P = NS) nor between the values at all sampling points (T: 0 vs 0; 1 vs 1; 2 vs 2; 3 vs 3). However, there were significant differences between the sampling points as such in both groups (Figure 1A and Table 1). Regarding mean airway pressure value, there was significant time influence (P < 0.0001) without either interaction or group impact (Table 1 and Figure 1B). In contrast, dynamic pulmonary compliance values showed a significant interaction (P = 0.0137) with both time (P < 0.0001) and group (P = 0.0018) impact (see Table 1 and Figure 1C), as well as between the T1 time points of group A vs group B (P = 0.0399).
| Measurements | Group A | Group B | ||||||
| Comparisons | P value | Comparisons | P value | Comparisons | P value | Comparisons | P value | |
| Peak airway pressure | T0 vs T1 | P < 0.001 | T1 vs T2 | P < 0.05 | T0 vs T1 | P < 0.001 | T1 vs T2 | P < 0.001 |
| T0 vs T2 | P < 0.001 | T1 vs T3 | P < 0.001 | T0 vs T2 | P < 0.001 | T1 vs T3 | NS | |
| T0 vs T3 | P < 0.001 | T2 vs T3 | P < 0.001 | T0 vs T3 | P < 0.001 | T2 vs T3 | P < 0.001 | |
| Mean airway pressure | T0 vs T1 | P < 0.001 | T1 vs T2 | NS | T0 vs T1 | NS | T1 vs T2 | NS |
| T0 vs T2 | P < 0.001 | T1 vs T3 | NS | T0 vs T2 | P < 0.001 | T1 vs T3 | P < 0.001 | |
| T0 vs T3 | P < 0.001 | T2 vs T3 | NS | T0 vs T3 | P < 0.05 | T2 vs T3 | NS | |
| Dynamic pulmonary compliance | T0 vs T1 | P < 0.001 | T1 vs T2 | NS | T0 vs T1 | P < 0.001 | T1 vs T2 | NS |
| T0 vs T2 | P < 0.001 | T1 vs T3 | NS | T0 vs T2 | P < 0.001 | T1 vs T3 | P < 0.001 | |
| T0 vs T3 | P < 0.001 | T2 vs T3 | P < 0.001 | T0 vs T3 | P < 0.001 | T2 vs T3 | P < 0.001 | |
We realize that in an original study, such statistics will be performed using the row data.
Analysis of the hemodynamic parameters in Table 6 using appropriate statistical tests supported by a proper study design would have safeguarded the authors against erroneous presentation of their findings. In order to demonstrate the dynamic changes in the respiratory and hemodynamic parameters and their subsequent impact on early postsurgical inflammatory reactions, the remaining study results should have been analyzed and described accordingly.
Unfortunately, this study presents even more shortcomings [1]: It provides no information on the number of gastric or colon cancers in these groups, nor on the type of surgical access: laparotomy (LT) or laparoscopy (LS) or conversions from LS to LT, given that surgery extension, when lymphatic nodules are to be removed, or other simultaneous operations might increase surgical trauma and postsurgical inflammatory responses.
Judging by the anesthesiology management of this study, mainly LS surgeries are supposed to be involved here, resulting in lung ventilation, maintaining the end-tidal carbon dioxide (ETpCO2) at 35-45 mmHg during operation at a maximum airway pressure peak of no more than 25 cm of water. During LS surgery with CO2 pneumoperitoneum, there should have been increased carbon dioxide partial pressure (pCO2) and decreased pH with subsequent respiratory, blood gas, and acid-base balance disturbances due to the long-lasting operation time of 216.3 ± 20.5 and 212.0 ± 22.7 minutes in groups A and B, respectively. Most patients were classified as American Society of Anesthesiologists (ASA) II, but since an equal number of patients were in ASA stages I and III, all respiratory and hemodynamic disorders and postsurgical inflammatory responses should have been adjusted in accordance with the ASA classification.
It surprised us that no reference was made to obvious patient obesity with body weights 125.1 ± 9.7 and 126.4 ± 7.5 kg with height 165.0 ± 6.1 and 163.9 ± 5.5 cm in ages 69.6 ± 5.3 and 70.3 ± 5.7 years in groups A and B, respectively.
On the plus side, this is a well-organized study presenting a balanced number of patients in two groups based on accurately performed pre- and post-surgery measurements. However, questionable study design and poor statistical analysis resulted in shortcomings in describing the findings. We hope the authors will provide answers to our questions and discussion.
We sincerely thank Veronique Alice M.J.G. Berkein (M.A.) from Leuven (Belgium) for her help preparing this manuscript.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Kazakhstan
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Basson MD, United States; Sultana N, Bangladesh; Tan JK, Malaysia S-Editor: Liu JH L-Editor: A P-Editor: Zhang XD
| 1. | Wang Y, Yang Y, Wang DM, Li J, Bao QT, Wang BB, Zhu SJ, Zou L. Different positive end expiratory pressure and tidal volume controls on lung protection and inflammatory factors during surgical anesthesia. World J Clin Cases. 2022;10:12146-12155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |