Published online Jun 26, 2023. doi: 10.12998/wjcc.v11.i18.4433
Peer-review started: April 5, 2023
First decision: May 8, 2023
Revised: May 17, 2023
Accepted: May 22, 2023
Article in press: May 22, 2023
Published online: June 26, 2023
Processing time: 81 Days and 12.2 Hours
Herpes zoster is caused by reactivation of latent varicella-zoster virus infection within the sensory nerve ganglion of the spinal or cranial nerves. Laryngeal herpes zoster is rare and involves superior laryngeal nerve, which leads to several complications such as throat pain, and cough.
Patient concerns: A 52-year old woman presented with a 70 d history of throat pain and a 67 d history of non-productive cough. Three days after onset of pain, she was diagnosed with laryngeal herpes zoster. Flexible nasolaryngoscopy revealed multiple white ulcerated lesions on the left hemi epiglottis and the left supraglottic area. She was prescribed with 750 mg famciclovir a day for 7 d, and 150 mg pregabalin, 100 mg tramadol and 10 mg nortriptyline a day for 67 d. However, despite of these medications, she complained of pain and persistent cough. Therefore, superior laryngeal nerve block under ultrasound guidance was performed. Three days after the intervention, the throat pain and cough disappeared. The patient remained symptom-free at 3 mo follow-up.
A superior laryngeal nerve block can be an effective option for treatment of pain and cough following laryngeal herpes zoster.
Core Tip: Laryngeal herpes zoster is rare, leading to several complications such as throat pain, and cough. A superior laryngeal nerve block can be an effective option for treatment of pain and cough following laryngeal herpes zoster.
- Citation: Oh J, Park Y, Choi J, Jeon Y. Superior laryngeal nerve block for treatment of throat pain and cough following laryngeal herpes zoster: A case report. World J Clin Cases 2023; 11(18): 4433-4437
- URL: https://www.wjgnet.com/2307-8960/full/v11/i18/4433.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i18.4433
Herpes zoster is caused by reactivation of latent varicella-zoster virus infection within the sensory nerve ganglion of the spinal or cranial nerves[1]. Herpes zoster is characterized by acute pain and erythematous maculopapular rash in the affected dermatome and most commonly involves the thoracic dermatome. Laryngeal herpes zoster is rare and involves superior laryngeal nerve, which leads to several complications such as throat pain, and cough[2]. Here, we present a case of a 52-year-old woman with a 70-d history of throat pain and a 67 d history of non-productive cough following herpes zoster on the left hemi-epiglottis and the left supraglottic area. The pain and cough were successfully treated with left superior laryngeal nerve block with lidocaine and triamcinolone under ultrasonography guidance.
A 52-year-old female with throat pain and non-productive cough was referred to the pain management center from otolaryngology department.
Her throat pain occurred 70 d prior to presentation. Three days after onset of pain, she noticed non-productive cough.
She was diagnosed with laryngeal herpes zoster by an otolaryngologist 67 d prior to presentation.
She had no significant medical history and family history.
Three days after onset of pain, a flexible nasolaryngoscopy revealed multiple mucosal eruptions and swelling on the left hemi-epiglottis and the left supraglottic area (Figure 1). The vocal movements were bilaterally normal.
Blood laboratory tests including leukocyte count, C-reactive protein, and erythrocyte sedimentation rate showed no abnormalities.
Chest radiography showed no abnormalities.
She was diagnosed with throat pain and cough following laryngeal herpes zoster.
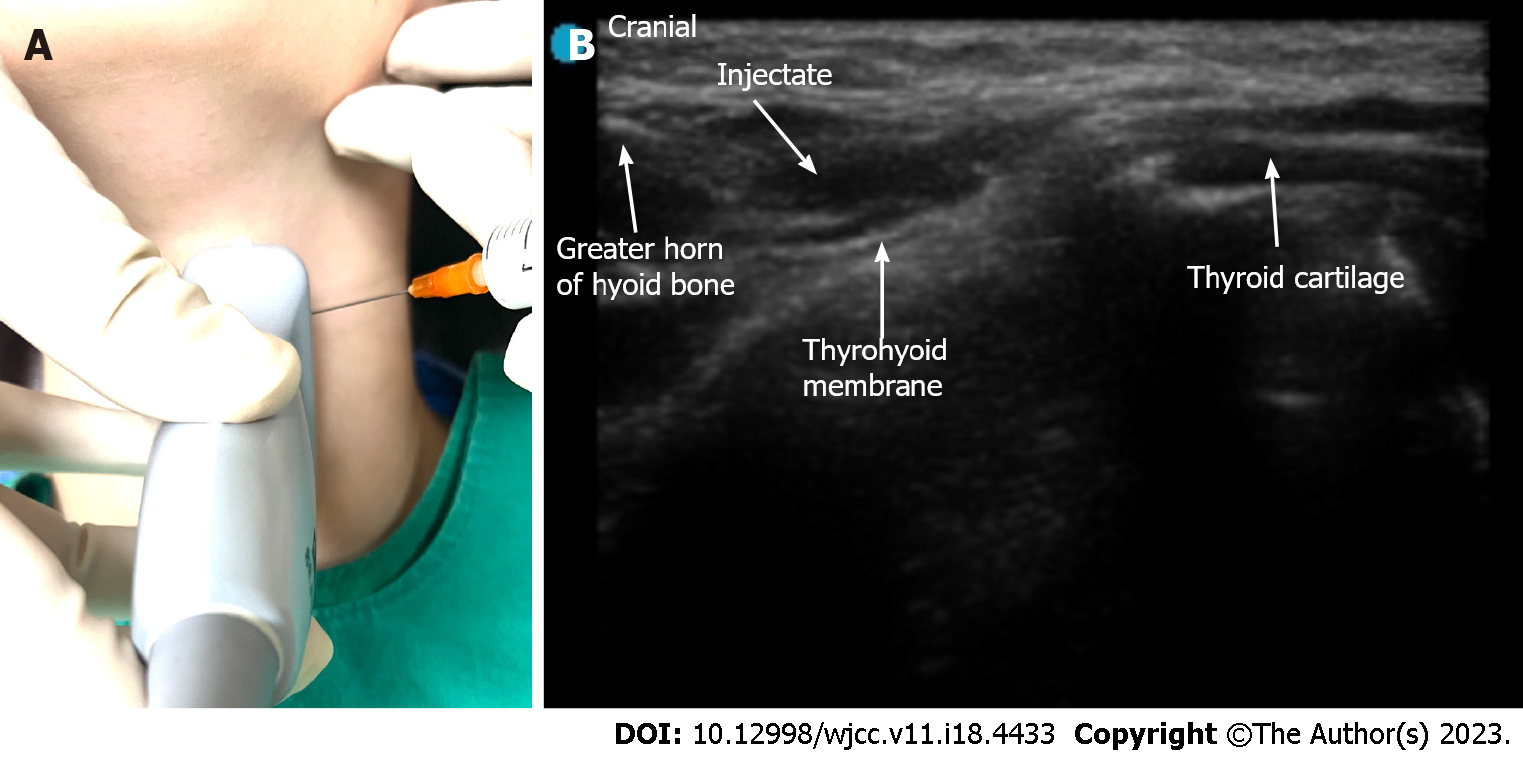
The patient was diagnosed with laryngeal herpes zoster by an otolaryngologist 67 d prior to presentation and 750 mg famciclovir once daily for 7 d was initially prescribed. In addition, she suffered from throat pain of 8 using the numerical analog scale (NRS) from 0 (no pain) to 10 (worst pain imaginable) and therefore, was treated with 75 mg pregabalin twice daily, 50 mg tramadol twice daily and 10 mg nortriptyline once at bedtime for 67 d. However, despite of these medications, the throat pain was 4 on the NRS. In addition, she complained of no improvement of cough. The patient suffered from mild constipation and dizziness due to medications and was reluctant to increase the dose. Her herpetic lesion was on the left supraglottic area, which are innervated by the internal branch of superior laryngeal nerve. Therefore, we decided to perform superior laryngeal nerve block under ultrasound guidance (Sonosite Edge 2, Fujifilm sonosite, Bothell, United States). The patient was placed in a supine position with the neck extension. The high frequency linear probe was placed over submandibular area in a longitudinal orientation. The greater horn of hyoid bone and thyroid cartilage were hyperechoic signals on sonography. Thyrohyoid muscle and thyrohyoid muscle were identified between two structures (Figure 2). Using out of plane approach, 2 mL of 50:50 mixture of 1% lidocaine and triamcinolone (40 mg/mL) was injected into the area of the posterior thyrohyoid membrane. After the procedure, the throat pain decreased to 1 on the NRS score, and the cough was greatly improved. Consent for publication of this case report was obtained from the patient.
Three days after the intervention, the pain and cough had completely disappeared. The patient remained symptom-free at a 3 mo follow-up.
Herpes zoster involves the sensory ganglion of spinal or cranial nerve, which subsequently, spreads along the peripheral nerves to the skin, leading to several complications such as rash, acute pain and postherpetic neuralgia (PHN)[1]. The diagnosis of herpes zoster is usually made on the history and examination findings. In this case, antibody titer to varicella zoster virus was not measured and the patient was diagnosed with laryngeal herpes zoster on the basis of the clinical presentation. The herpes zoster most commonly affects the thoracic region, followed by the ophthalmic branch of the trigeminal nerve[1]. Laryngeal herpes zoster is rare, involving the sensory of vagus nerve[2]. The sensory distribution of the vagus nerve includes superior laryngeal nerve and auricular nerve. The internal branch of the superior laryngeal nerve enters the thyrohyoid membrane and provides sensation of supraglottis above the vocal cord whereas the auricular branch of the vagus supplies part of the external auditory meatus[3]. In the present case, herpes zoster involved the left side of supraglottic region including the epiglottis, and vallecular, leading to unilateral throat pain.
Generally, the herpes zoster rash resolves within 2-4 wk. Administration of antiviral agents including acyclovir and famciclovir within 72 h after onset of herpes zoster effectively decreases acute pain, promotes lesion healing and prevents PHN[1,4]. However, PHN can occur due to nerve tissue injury during an outbreak of herpes zoster. Several inflammatory materials were released from the injured tissue including substance P, histamine and bradykinin, resulting in peripheral sensitization[5,6]. These excitatory materials increase ectopic discharge of C fibers and lead to spontaneous pain, allodynia, and hyperalgesia[7].
In the present case, three days after onset of throat pain, the patient noticed non-productive cough, easily triggered by speaking, which mildly affected the patient’s daily life.
When cough lasts more than 8 wk without clear external stimuli to the chough mechanism, neurogenic cough is conserved, which is associated with hypersensitivity of the superior laryngeal nerve[8]. It was reported that chronic cough occurs as a sequala to sensory nerve damage during laryngeal herpes zoster[2,8].
The anti-convulsant such as gabapentin or pregabalin and anti-depressant including tricyclic antidepressants represent first-line treatment options for neuropathic pain[1,9]. Postherpetic cough is associated with neurogenic hypersensitivity and is analogue to PHN. Therefore, medical treatment with pregabalin and amitriptyline can be considered to be effective to treat pain and cough following herpes zoster[2,8]. However, such complications associated with herpes zoster are often resistant to medical treatments[1,2,8]. In the present case, the patient complained of throat pain at a 4 on the NRS and cough despite medication with pregabalin, nortriptyline and tramadol.
Administration of local anesthetic plus steroid around nerve affected by herpes zoster is effective in treating zoster pain and preventing PHN[1,10,11]. It was reported that the superior laryngeal nerve with local anesthetic and steroid was effective to treat chronic neurogenic cough after post-viral neuropathy[12,13]. Steroids, a strong anti-inflammatory agent, can decrease the perineural inflammatory response and reduce ectopic discharge in the involved nerve[14,15]. In addition, it can help hasten recovery of the injured nerve[14]. In the present case, the pain and cough following herpes zoster was completely resolved with superior laryngeal nerve block under ultrasonography guidance.
In conclusion, laryngeal herpes zoster is a rare form of herpes zoster. It can cause several complications such as throat pain and cough. A superior laryngeal nerve block with steroid can be an effective option for treatment of persistent pain and cough following laryngeal herpes zoster. Clinicians should be aware of this entity to provide appropriate treatments.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Otorhinolaryngology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Higa K, Japan; Melek L, Egypt S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Jeon YH. Herpes Zoster and Postherpetic Neuralgia: Practical Consideration for Prevention and Treatment. Korean J Pain. 2015;28:177-184. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 90] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 2. | Ling B, Novakovic D, Sulica L. Cough after laryngeal herpes zoster: a new aspect of post-herpetic sensory disturbance. J Laryngol Otol. 2014;128:209-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Monkhouse S. Clinical anatomy: a core text with self-assessment: Elsevier Health Sciences, 2001. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Lilie HM, Wassilew S. The role of antivirals in the management of neuropathic pain in the older patient with herpes zoster. Drugs Aging. 2003;20:561-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Truini A, Galeotti F, Haanpaa M, Zucchi R, Albanesi A, Biasiotta A, Gatti A, Cruccu G. Pathophysiology of pain in postherpetic neuralgia: a clinical and neurophysiological study. Pain. 2008;140:405-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 85] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 6. | Mannion RJ, Costigan M, Decosterd I, Amaya F, Ma QP, Holstege JC, Ji RR, Acheson A, Lindsay RM, Wilkinson GA, Woolf CJ. Neurotrophins: peripherally and centrally acting modulators of tactile stimulus-induced inflammatory pain hypersensitivity. Proc Natl Acad Sci U S A. 1999;96:9385-9390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 331] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 7. | Fields HL, Rowbotham M, Baron R. Postherpetic neuralgia: irritable nociceptors and deafferentation. Neurobiol Dis. 1998;5:209-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 393] [Cited by in RCA: 372] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 8. | Altman KW, Noordzij JP, Rosen CA, Cohen S, Sulica L. Neurogenic cough. Laryngoscope. 2015;125:1675-1681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 53] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 9. | Gierthmühlen J, Baron R. Neuropathic Pain. Semin Neurol. 2016;36:462-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 88] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 10. | Kim HJ, Ahn HS, Lee JY, Choi SS, Cheong YS, Kwon K, Yoon SH, Leem JG. Effects of applying nerve blocks to prevent postherpetic neuralgia in patients with acute herpes zoster: a systematic review and meta-analysis. Korean J Pain. 2017;30:3-17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 71] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 11. | Lee H, Jeon Y. Treatment of herpes zoster with ultrasound-guided superficial cervical plexus block. J Dent Anesth Pain Med. 2015;15:247-249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Simpson CB, Tibbetts KM, Loochtan MJ, Dominguez LM. Treatment of chronic neurogenic cough with in-office superior laryngeal nerve block. Laryngoscope. 2018;128:1898-1903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 13. | Amin MR, Koufman JA. Vagal neuropathy after upper respiratory infection: a viral etiology? Am J Otolaryngol. 2001;22:251-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 84] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 14. | Johansson A, Bennett GJ. Effect of local methylprednisolone on pain in a nerve injury model. A pilot study. Reg Anesth. 1997;22:59-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 94] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 15. | Devor M, Govrin-Lippmann R, Raber P. Corticosteroids suppress ectopic neural discharge originating in experimental neuromas. Pain. 1985;22:127-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 187] [Article Influence: 4.7] [Reference Citation Analysis (0)] |