Published online Jun 26, 2023. doi: 10.12998/wjcc.v11.i18.4419
Peer-review started: March 25, 2023
First decision: May 8, 2023
Revised: May 11, 2023
Accepted: May 23, 2023
Article in press: May 23, 2023
Published online: June 26, 2023
Processing time: 93 Days and 13.5 Hours
Longus colli tendinitis (LCT) with dyspnea is a relatively less-reported condition in the literature, and physicians should be aware of its existence. Misdiagnosis of this condition may cause unnecessary treatment for dyspnea.
Herein, we report the case of a 40-year-old man with acute neck tendonitis. The patient presented to the pneumology department clinic with a complaint of acute neck tendonitis with dyspnea. An emergency cervical magnetic resonance examination was performed, and the preliminary diagnosis was “acute longus cervicalis tendinitis.” After aggressive medical treatment, the symptoms obviously improved.
LCT is a self-limiting disease that usually improves after three to seven days of conservative treatment following a definite diagnosis. However, owing to its insidious onset and complex clinical manifestations, most relevant personnel are not fully understood. The definite diagnosis of LCT is based on a comprehensive understanding of the triad, rare symptoms, and the clear identification of cervical 1 and 2 levels calcification and prevertebral edema by medical imaging examination, especially magnetic resonance imaging and computed tomography.
Core Tip: The diagnosis of longus colli tendinitis was established using computed tomography, magnetic resonance imaging, and clinical features. The purpose of this study is to describe my experience with this case, broaden our understanding, and avoid a misdiagnosis of this disease in the future.
- Citation: Wu H, Liu W, Mi L, Liu Q. Acute neck tendonitis with dyspnea: A case report. World J Clin Cases 2023; 11(18): 4419-4424
- URL: https://www.wjgnet.com/2307-8960/full/v11/i18/4419.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i18.4419
Dyspnea and dysphagia are some of the most common symptoms in patients visiting physicians. However, it can easily be misinterpreted as lung disease or pharyngeal disease; cervical spine dysfunction combined with deep neck flexors is a lesser-known disease[1]. Adjacent to the front of the cervical vertebrae and covered by the deep cervical fascia, the longus is the deepest neck flexor muscle, spanning all cervical vertebrae in a segmented manner. Bilateral contraction of the neck longus and anterior flexion of the head and neck can stabilize the front of neck flexion, prevent excessive head extension, and maintain normal cervical physiological curvature. The long cervical muscle is divided into three parts: Superior oblique, vertical, and inferior oblique bundles. The inferior oblique bundle starts from the front of the first to the third thoracic vertebra and ends at the anterior tubercle of the fifth and sixth cervical transverse processes, upward and forward. The vertical bundle starts from the front of the upper three thoracic vertebrae and the front of the transverse process of the lower three cervical vertebrae and ends in the front of the second to fourth cervical vertebrae. The superior oblique bundle originates from the anterior tubercle of the transverse process of the third to fifth cervical spine and ends at the anterior tubercle of the anterior arch of the atlas. The longus colli tendinitis (LCT) mainly occurs in the superior oblique bundle of the cervical longus muscle. It is mainly caused by the deposition of calcium salts in the fascicles of the cervical longus muscle, which induces aseptic inflammation. Most scholars believe that this abnormal deposition of calcium salt is caused by repeated injury, local ischemia, and hypoxia, which leads to degeneration with the classical symptoms of neck pain, limitation of cervical spine movement, and swallowing complaints or dyspnea[2]. Tendon calcification of the cervical longus muscle is generally divided into four stages: Stage 1, also known as pre-calcification, is characterized by fibrocartilage degeneration and pre-calcification of the tendon. There were no symptoms, and patients in the calcified phase of formation had no obvious symptoms or slight subacromial appearance. As a manifestation of impingement syndrome, patients with calcifications in the absorption phase may experience severe pain and limited vitality. One study demonstrated that conservative treatment is successful in 90% of cases. In cases with large calcifications, the integrity of the calcification can be preserved as much as possible during surgery[3,4]. In stage 2, the calcification enters a stationary phase. The third stage is the reabsorption stage. Clinically, pain and limitation of activity appear to be associated with the resorption period. When calcification is loose and amorphous, it may represent a reabsorption period. In the fourth stage, the final stage during the repair phase, fibroblasts regenerate collagen from the normal tendon[5].
The patient is a 40-year-old Chinese man presented to the pneumology department clinic with a complaint of acute neck tendonitis with dyspnea.
On Friday, October 28, 2022, at 21:00, he developed neck pain and limited movement without obvious cause and inducement. Not taking them seriously, the patient thought the symptoms were due to overwork and rested in bed. At 2:00 on October 29, 2022, he felt that the above symptoms had significantly aggravated. Slight dyspnea appeared, which was tolerable, but he could not sleep all night. Until 7:00 am on October 29, 2022, the symptoms continued to worsen, with obvious dyspnea and dysphagia. At 7:30 am, an emergency cervical magnetic resonance examination was performed, and the preliminary diagnosis was “acute longus cervicalis tendinitis.” Immediately, he took a nimesulide dispersible tablet orally. Twenty-four hours later, his symptoms gradually improved; however, his swallowing function was still very poor, and he could only consume a small amount of liquid food. He continued to take nimesulide dispersible tablets for further treatment. After 48 h, all the above symptoms significantly improved, and the swallowing function returned to nearly normal state. Now, he takes postprednisolne acetate tablets, 20 mg qd, and nimesulide dispersible tablets, 20 mg bid.
The patient had no previous history of infectious diseases, trauma, or bad habits (such as smoking or drinking).
The patient denied any family history of malignant tumours.
On physical examination, the vital signs were as follows: Body temperature, 36.6 ℃; blood pressure, 120/78 mmHg; heart rate, 85 beats per min; respiratory rate, 18 breaths per min. There was no obvious redness and swelling in the neck. Annual physical examinations (including various laboratory tests and imaging examinations) indicated that the patient was healthy.
White blood cell: 10.78 × 109/L, neutrophils: 7.27 × 109/L. C-reactive protein and erythrocyte sedimen
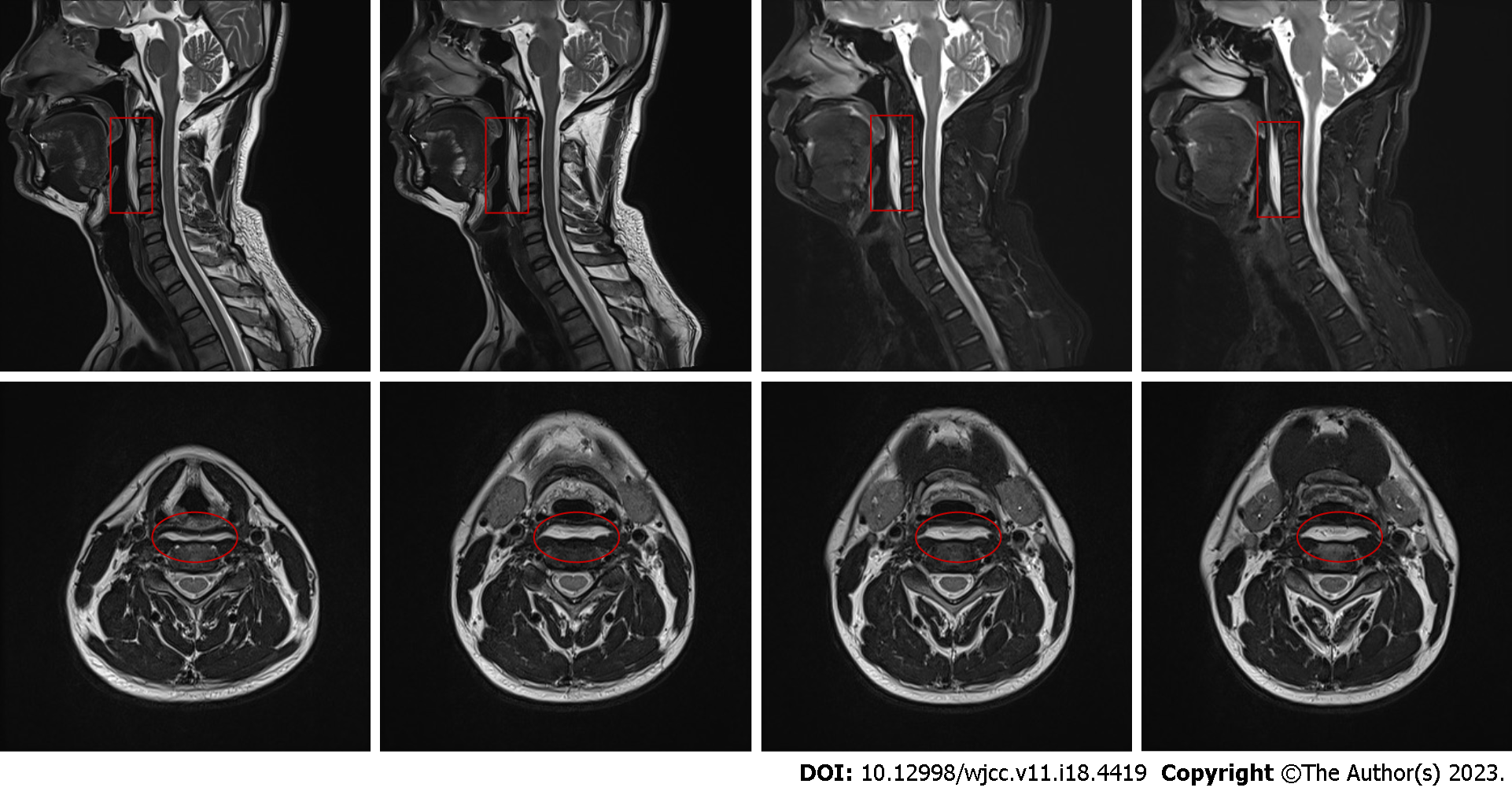
The magnetic resonance imaging (MRI) examination of the cervical region revealed T2-weighted localized slit-like areas in the prevertebral region, located at the level of cervical 1 to cervical 4, with long T2 changes (Figure 1). Computed tomography (CT) of the cervical spine showed no significant calcification (Figure 2).
Combined with the patient’s medical history, the final diagnosis was LCT.
Treatment with prednisolone acetate tablets and nimesulide dispersible tablets.
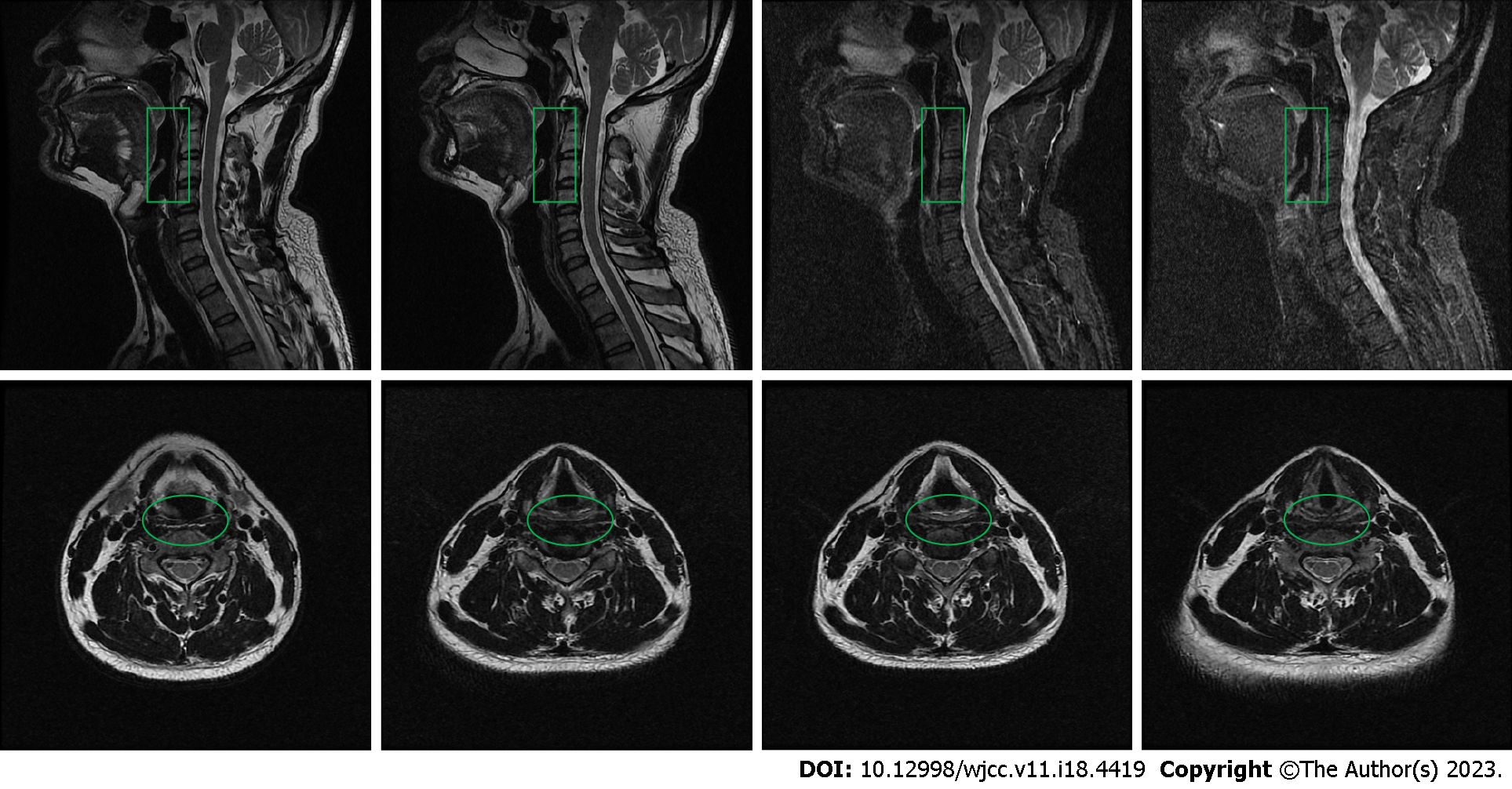
Symptoms were relieved immediately after treatment, and complete resolution of symptoms was observed after five days. Figure 3 presents the MRI of after treatment. Up to now, there has been no recurrence and the patient is doing well.
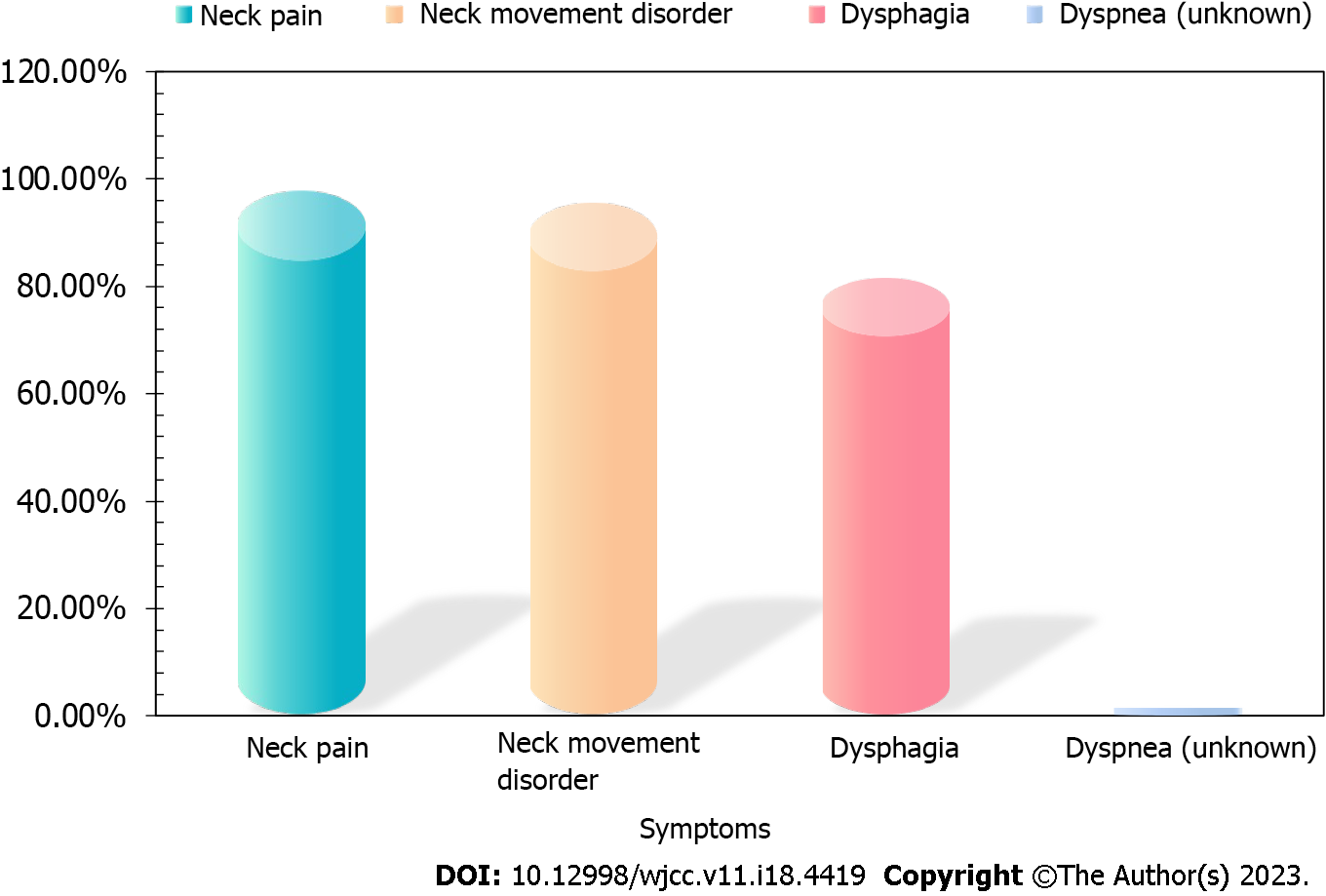
Typical clinical manifestations include acute and subacute neck pain, neck movement disorder, and dysphagia triad. Shen et al[6] conducted a retrospective analysis of relevant literature and found that among 278 LCT patients from 1964 to 2018, neck pain accounted for 97.8%, neck movement disorder accounted for 95.6%, and dysphagia for 81.6% (Figure 4). Other manifestations included neck stiffness, shoulder and upper limb pain, swallowing pain, pharyngeal discomfort, back pain, head pain, stiff pillow, vertigo, and so on. Most of them were without or accompanied by abnormal inflammatory indicators such as white blood cell count, erythrocyte sedimentation rate, and C protein. However, there are currently no clear statistics on acute neck tendonitis with dyspnea.
The high resolution of CT can identify small calcifications within tendons that are often not shown on X-ray and can identify calcifications rather than dense shadows of other skeletal sources. Calcification is generally located below the anterior arch of the atlas, and anterior to the odontoid process along the axis[7]. CT helps confirm the presence of prevertebral effusion and rule out other pathological findings, such as fractures or abscesses. MRI is sensitive to effusion and may help identify soft-tissue abnormalities to rule out retropharyngeal abscesses, spondylitis, or neoplastic lesions. MRI examination can clearly show changes in the morphology and signal of the supraspinatus tendon; however, small calcified deposits may be missed. T2-weighted localized fissure-like areas in the prevertebral area, mostly located at the level of neck 1 to 4, show long T2 changes, which are due to the effusion caused by inflammation. T2-weighted, fat-suppressed, and T1-weighted sequences are important for differentiating effusion from adipose tissue, fatty bone marrow, retropharyngeal infection, and spondylitis. MRI has shortcomings in the examination of calcification, which can be hyperintense or hypointense in T1-weighted calcification and hypointense in T2-weighted calcification, need to be combined with CT. In conclusion, the specific imaging findings of longus cervicalis tendinitis include the presence of anterior margin effusion of C1-C4 and calcified deposits below the anterior arch of C1. The combination of clinical and imaging findings will help distinguish this disease from other diseases[8].
LCT is a self-limiting disease that usually improves after three to seven days of conservative treatment following a definite diagnosis[9]. However, owing to its insidious onset and complex clinical manifestations, most relevant personnel are not fully understood. The definite diagnosis of LCT is based on a comprehensive understanding of the triad, rare symptoms, and the clear identification of cervical 1 and 2 Levels calcification and prevertebral edema by medical imaging examination, especially MRI and CT.
We thank the corresponding author Liu Q for his selfless dedication.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Neurosciences
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bernardes A, Portugal; Tanaka T, Japan S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Siag K, Mazzawi S, Paker M, Biener R, Ghanayim R, Lumelsky D. Acute longus colli tendinitis and otolaryngology. Braz J Otorhinolaryngol. 2022;88:351-357. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Guerroum H, Koubaa I, Benissad A. Calcific tendinitis of the longus colli: An uncommon cause of neck pain. Radiol Case Rep. 2022;17:1228-1230. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 3. | Darrieutort-Laffite C, Blanchard F, Le Goff B. Calcific tendonitis of the rotator cuff: From formation to resorption. Joint Bone Spine. 2018;85:687-692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 4. | Kang T, Park SY, Lee SH, Park JH. Acute Calcific Tendinitis of the Longus Colli. Pain Med. 2020;21:1706-1708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Ko-Keeney E, Fornelli R. Acute Calcific Tendinitis of the Longus Colli: Not All Retropharyngeal Fluid is an Abscess. Ear Nose Throat J. 2022;101:78-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Shen Y, Zhou Q, Zhu X, Qiu Z, Jia Y, Liu Z, Li S. Vertigo caused by longus colli tendonitis: A case report and literature review. Medicine (Baltimore). 2018;97:e13130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Qureshi PAAA, Bollason G, Ágústsson KL. Acute Calcific Tendinitis of the Longus Colli Muscles: An Entity That Should Be Known by Emergency Radiologists. Cureus. 2022;14:e25518. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 8. | Igami E, Fukae J, Kanazawa K, Fuse A, Nakajima A, Eguchi H, Hattori N, Shimo Y. Two rare diseases, acute calcific retropharyngeal tendinitis, and crowned dens syndrome, mimicking meningitis: A case report. Front Neurol. 2022;13:946222. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | Bannai T, Seki T, Shiio Y. A pain in the neck: calcific tendinitis of the longus colli muscle. Lancet. 2019;393:e40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |