Published online Jun 26, 2023. doi: 10.12998/wjcc.v11.i18.4412
Peer-review started: April 5, 2023
First decision: April 20, 2023
Revised: May 7, 2023
Accepted: May 30, 2023
Article in press: May 30, 2023
Published online: June 26, 2023
Processing time: 82 Days and 5.9 Hours
Pancreatitis, panniculitis, and polyarthritis (PPP) syndrome is a rare form of pancreatic disease. It is characterized by bullous erythematous skin lesions and arthritis, and both are triggered by pancreatic malfunction. Few cases have been described in the literature thus far. Due to the inconsistency in its clinical pre
A 66-year-old polymorbid male patient presented with several superficial abscesses on both lower legs and painful swelling in the knee. Treatment for septic arthritis and septic skin infection over several weeks failed. His general condition deteriorated gradually and worsened with sudden onset of abdominal pain. A diagnosis of necrotizing pancreatitis was made. He subsequently underwent a laparotomy and drainage of the pancreas. Eventually, our patient improved, and his abdominal complaints, knee pain, and dermal lesions resolved.
PPP syndrome is rare and easily misdiagnosed, as abdominal symptoms may be delayed or absent. Clinicians should consider PPP syndrome if they encounter refractory panniculitis in combination with joint infection.
Core Tip: Pancreatitis, panniculitis, and polyarthritis (PPP) syndrome is a rare disease. The combination of joint inflammation and abscess-like skin lesions suggests an infectious cause. However, these symptoms are triggered by pancreatic disease. As abdominal symptoms may be delayed or absent, PPP syndrome may be challenging to diagnose and treat. We present our experience in treating a 66-year-old patient with PPP syndrome. In conclusion, PPP syndrome should be considered in cases of hard-to-treat or atypical joint and tissue infections.
- Citation: Pichler H, Stumpner T, Schiller D, Bischofreiter M, Ortmaier R. Pancreatitis, panniculitis and polyarthritis syndrome: A case report. World J Clin Cases 2023; 11(18): 4412-4418
- URL: https://www.wjgnet.com/2307-8960/full/v11/i18/4412.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i18.4412
Patients with pancreatitis usually present with abdominal pain, nausea, and vomiting. Atypical symptoms such as osteomyelitis, intra-abdominal abscesses, arthritis, panniculitis, and peripheral fat necrosis may occur[1,2]. Pancreatitis, panniculitis, and polyarthritis (PPP) syndrome is a disorder characterized by the eponymous triad of pancreatitis, polyarthritis, and panniculitis. Due to the rarity of the disease, only 59 cases have been reported in the literature by 2020[3], and its inconsistent clinical presentation and the lack of therapy guidelines make it difficult to diagnose and treat.
In February 2021, a 66-year-old male patient presented to our orthopedic department because of multiple erythematous skin nodules on both lower legs and painful swelling in the right knee (Figure 1).
The dermal lesions first appeared 4 wk before without any history of trauma. Antibiotic therapy was started 3 wk before by the dermatology department with intravenous (IV) clindamycin 600 mg three times daily for three weeks. This was effective, and the patient was ultimately discharged. One week after discharge, the skin lesions worsened, and he was readmitted to the dermatology department. Antibiotic therapy was broadened to IV clindamycin 600 mg and IV fosfomycin 8 g three times daily.
Due to a spontaneous, painful swelling in his right knee, he was transferred to our orthopedic department, and septic arthritis was suspected. Eighty milliliters (ml) of pus were obtained after intraarticular puncture and were sent for culture. His abdominal pain did not occur until approximately two months after the onset of the first dermal lesions.
The patient had multiple comorbidities, including arterial hypertension, hyperlipidemia, diabetic neuropathy, chronic obstructive pulmonary disease, aortic bifurcation graft, ilio-femoral bypass on the right leg, iliac artery stent on the left side, and a double stroke. He reported recurrent ulceration on both feet and lower legs associated with his peripheral arterial disease and type 2 diabetes, which were never treated surgically. He was suffering from chronic pancreatitis caused by alcohol abuse and had a smoking history of approximately 40 packyears.
The patient had no history of previous joint infections. His family history for similar symptoms was negative.
The patient was in good overall condition, had no fever and was free of pain. There was swelling with marked effusion, warming, and reddening in the right knee. On both lower legs, he had multiple erythematous subcutaneous nodules.
The C-reactive protein (CRP) level was 27 mg/dL (norm < 1 mg/dL), and the leukocyte count was 16.1 G/L (norm 4-9 G/L). Serum levels of lipase, amylase, triglycerides, calcium, parathormone and immunoglobulin G4 were found to be normal. The aspirate from the right knee showed growth of Staphylococcus aureus in culture. Further infection diagnostics, such as a QuantiFERON test and screening for human immunodeficiency virus, LUES, and Francisella tularensis, all remained negative.
Radiographic X-ray imaging showed osteoarthritis of both knees without signs of osteodestruction. Magnetic resonance imaging showed an extensive bone lesion in the right femur and tibia extending approximately 15 cm craniocaudally. There were also several smaller bone lesions in the left tibia with a maximum size of 3.6 cm, indicating chronic osteomyelitis (Figure 2).
Following the positive detection of Staphylococcus aureus in the knee joint aspirate, arthroscopy with extensive irrigation and debridement was completed, and suction-irrigation drainage was applied. Due to persistent putrid secretion from the arthroscopic wounds, arthroscopy was repeated one week later. Several superficial abscesses were incised (Figure 3), and a biopsy of suspicious bone tissue was taken from the right tibia. The antibiotic therapy was changed to IV cefazolin 2 g three times daily and oral fusidic acid 500 mg three times daily. The inflammatory markers declined, with the CRP level decreasing to 2.9 mg/dL, and the leukocyte count had decreased to 11.1 G/L.
Despite extensive multimodal therapy, the skin lesions and swelling in the knee remained. The patient’s general condition deteriorated a few days later, and he complained of progressive abdominal pain. His CRP levels increased to 41.3 mg/dL with a leukocyte count of 26.7 G/L. The levels of lipase and amylase peaked at 582 U/L (norm 5-60 U/L) and 267 U/L (norm 30-120 U/L), respectively.
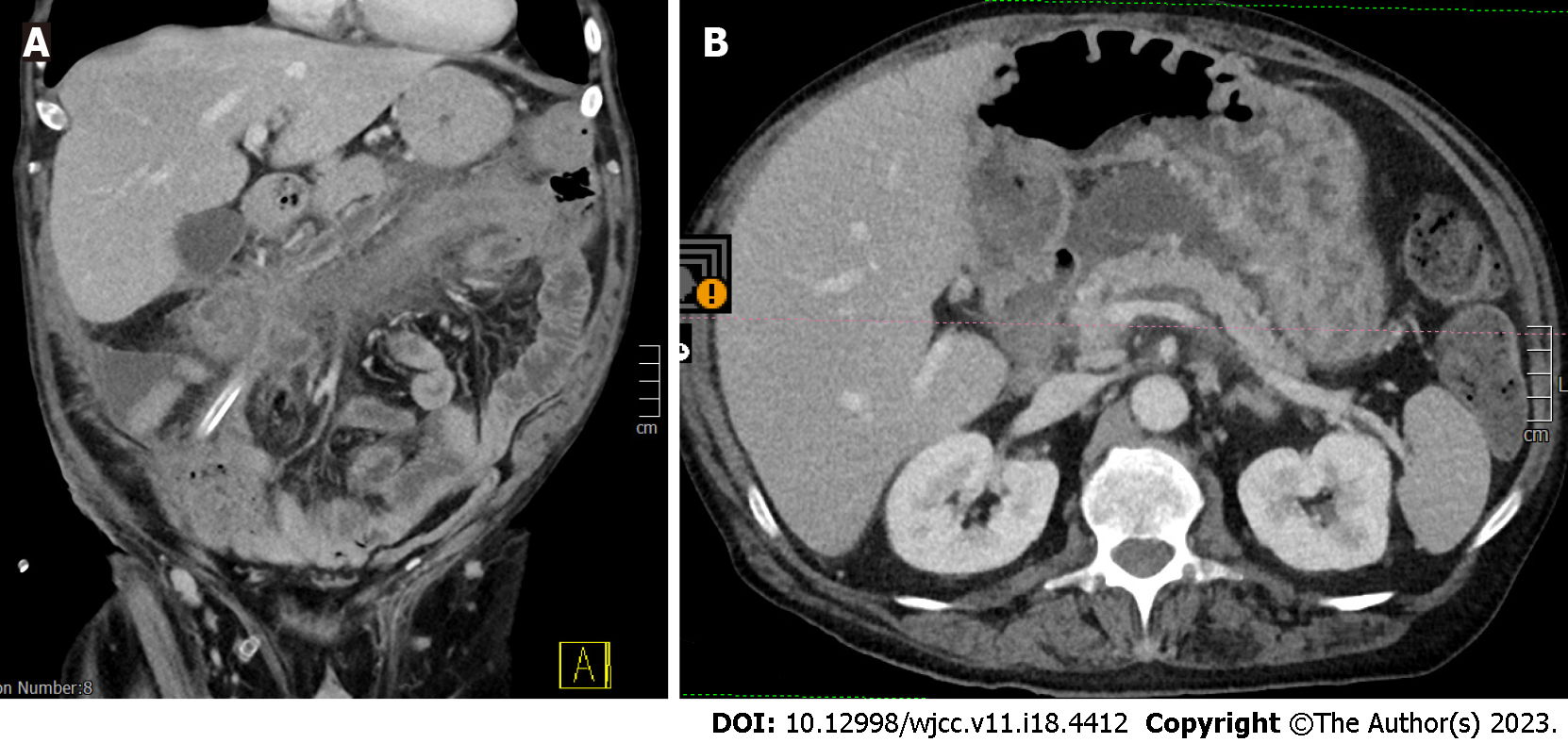
A computed tomography scan of the abdomen showed a stenotic transverse colon as well as massive inflammatory changes of the entire colon and peripancreatic acute necrotic collections (Revised Atlanta classification) in the sense of an incipient abscess indicating necrotizing pancreatitis (Figure 4). In addition, there was a cystic lesion around the uncinate process of the pancreas with a diameter of approx. 2.2 cm. There were no signs of malignant tumors.
The material obtained from the right tibia histologically showed fat tissue necrosis without florid inflammation, and microbiologic culture was negative. The onset of acute pancreatitis in combination with the existing skin lesions and knee infection finally provided decisive clues for the actual diagnosis.
The final diagnosis was PPP syndrome.
Due to the findings and the patient's poor general condition with an APACHE II score of 14, exploratory laparotomy was performed the same day. It showed a severe necrotizing pancreatitis with traces of debris extending into the transverse colon. A pancreatic drain was inserted, and a double-barreled ileostomy was performed to relieve the cecum. Histological findings of intraoperative tissue samples confirmed acute necrotizing pancreatitis. Microbiologic culture of drainage revealed Pseudomonas aeruginosa.
The antibiotic treatment was changed to IV meropenem 1 g three times daily and oral linezolid 600 mg twice daily.
Finally, the patient's condition slowly improved, and after almost three months of therapy, he was discharged from the hospital.
Four weeks after discharge, the patient presented in good general condition. Skin examination showed no lesions, and the pain in his knee and abdomen had resolved (Table 1).
| Date | Event |
| 2021-01-25 | First dermal lesions appeared |
| 2021-02-23 | CRP of 27 mg/dL (norm < 1 mg/dL), leukocyte count of 16.1 G/l (norm 4-9 G/l) |
| 2021-02-23 | Aspiration of 80 mL pus from the right knee |
| 2021-02-23 | First arthroscopic lavage of the right knee |
| 2021-02-24 | MRI scan of both legs |
| 2021-03-04 | Rearthroscopy and lavage of the right knee |
| 2021-03-15 | CRP of 5.4 mg/dL, lipase of 32 U/l (norm 5-60 U/l), amylase of 99 U/l (norm 30-120 U/l) |
| 2021-03-17 | Onset of abdominal pain |
| 2021-03-23 | CT scan of the abdomen indicated necrotizing pancreatitis |
| 2021-03-23 | CRP of 41.3 mg/dL, lipase of 582 U/l, amylase of 267 U/l |
| 2021-03-23 | Exploratory laparotomy |
| 2021-04-12 | CRP of 2.5 mg/dL, leukocyte count of 15.4 G/l |
| 2021-04-12 | Discharge from the hospital |
| 2021-05-19 | Last follow up |
Pancreatitis is usually characterized by gastrointestinal symptoms and high serum levels of pancreatic enzymes. However, it may be associated with extra-abdominal symptoms, such as pancreatic panniculitis, which occurs in 2%-3% of patients[4]. PPP syndrome, describing the triad of PPP, is rare, and only 59 documented cases of patients with PPP syndrome have been described thus far[3]. Most of the patients are middle-aged men, and 64% have a history of alcohol abuse[5].
The exact pathomechanism for PPP syndrome is still unclear. It is assumed that the release of pancreatic enzymes (such as amylase, lipase, trypsin, and phospholipase A) into the bloodstream leads to lipolysis and subsequent fat tissue necrosis in soft tissue and the bone marrow[6-9].
In 2021, Betrains et al[3] evaluated the underlying pancreatic disease that causes PPP syndrome. They found acute pancreatitis in 54.2% of the patients, chronic pancreatitis in 30.5%, pancreatic malignancy in 11.9%, and acute on chronic pancreatitis in 3.4%. In nearly half of the patients, such as ours, pancreatic pseudocysts were reported. Most patients were male (74.6%), and the median age was 49 reaching from 4 to 88 years old[3].
Pancreatic panniculitis occurs on the lower limbs in nearly 100% of patients. Upper limbs were affected in 25.4%, and the trunk was affected in 13.6%. The material discharged from these lesions showed areas of fat necrosis on histological examination, and this was also the case in our patient[3].
Arthritis is typically oligoarticular, and in two-thirds of cases, it is symmetrical. There seems to be no predilection for a particular joint, as the distribution of affected joints involved the ankles in 64.4%, knees in 57.6%, hands in 54.2%, wrists in 47.5%, feet in 25.4%, elbows in 22.0%, and shoulders in 3.4% of patients[3].
Only approximately half of patients with PPP syndrome were found to have gastrointestinal symptoms[3]. Absence or delayed onset of abdominal malaise may lead to a misdiagnosis of PPP syndrome as an infectious disease, as occurred in our case.
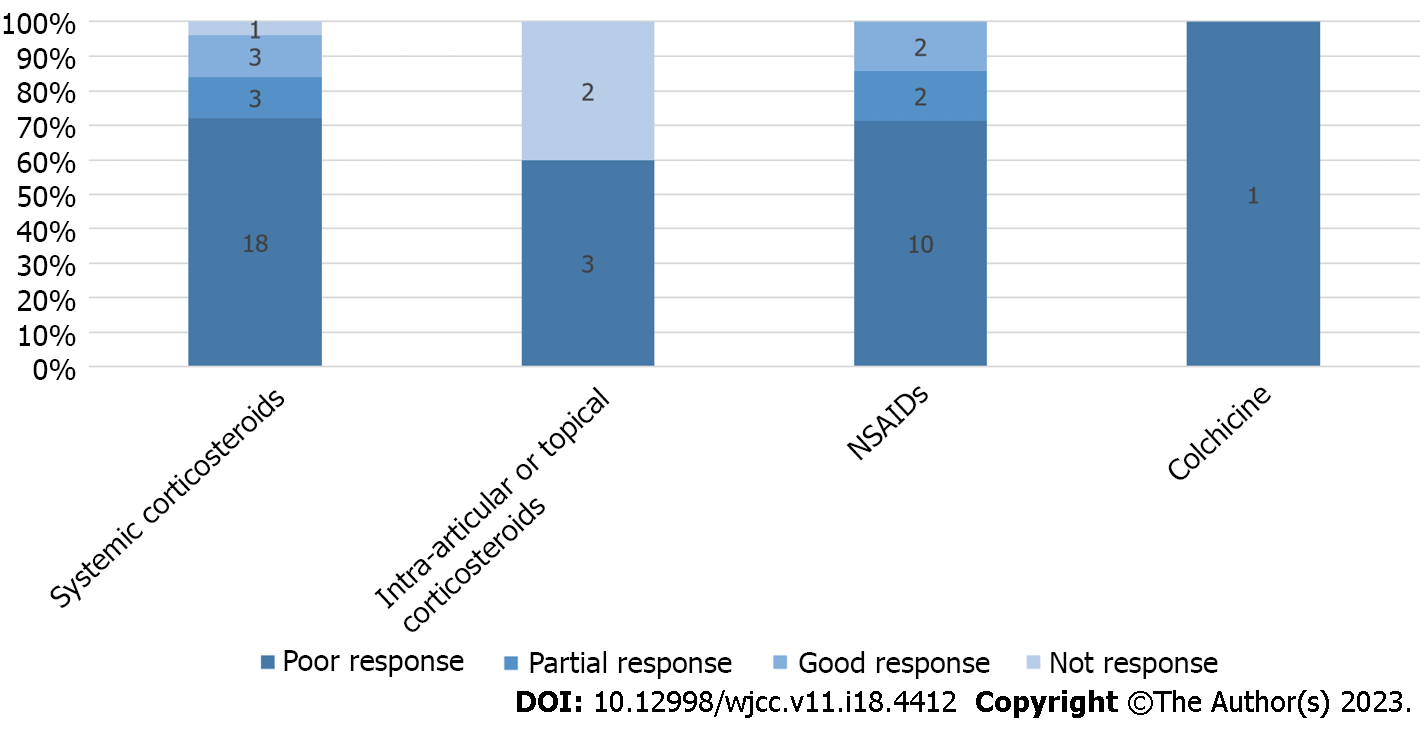
To date, no uniform treatment concept for PPP syndrome exists. Only 12% of patients treated with systemic steroids show a partial or good response, while a poor response is reported in 72%. Other therapeutic options reported are nonsteroidal anti-inflammatory drugs, topical or intra-articular corticosteroids, and colchicine. Overall, pharmacological treatment for PPP-syndrome shows poor response in 79% of patients (Figure 5)[6-10].
The key to successful treatment lies in the therapy of the underlying pancreatic disease[6,10]. As shown in our case, the patient´s condition improved substantially after surgical pancreas drainage stopped the release of pancreatic enzymes into the blood stream. Treatment for septic arthritis and peripheral abscesses alone only brought short-term success.
The outcome of PPP syndrome is generally poor. Of the 59 patients analyzed, 27.1% died after a median of 8 wk, and 10.2% had persistent disease. However, 55.9% of the patients achieved resolution of the disease. The mortality of patients with chronic pancreatitis was higher (25%) compared with patients with acute pancreatitis (15.6%)[3].
PPP syndrome is a rare disease that is difficult to diagnose and treat. The effects on multiple organ systems require an interdisciplinary therapeutic approach including abdominal surgeons, gastroenterologists, and orthopedic surgeons. As mortality is high, early diagnosis and therapy of underlying pancreatic disease is crucial. Therefore, we recommend that clinicians consider PPP syndrome even in the absence of gastrointestinal symptoms when they encounter a combination of atypical joint infection and erythematous, bullous dermal lesions resistant to therapy.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Austria
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D, D, D
Grade E (Poor): 0
P-Reviewer: Aslam M, India; Kitamura K, Japan S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Kamble PM, Patil A, Jadhav S, Rao SA. Anterior abdominal wall abscess with epididymo-orchitis: an unusual presentation of acute pancreatitis. J Postgrad Med. 2011;57:335-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Langenhan R, Reimers N, Probst A. Osteomyelitis: A rare complication of pancreatitis and PPP-syndrome. Joint Bone Spine. 2016;83:221-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Betrains A, Rosseels W, Van Mieghem E, Vanderschueren S, Nijs J. Clinical characteristics, treatment, and outcome of pancreatitis, panniculitis, and polyarthritis syndrome: a case-based review. Clin Rheumatol. 2021;40:1625-1633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 4. | Laureano A, Mestre T, Ricardo L, Rodrigues AM, Cardoso J. Pancreatic panniculitis - a cutaneous manifestation of acute pancreatitis. J Dermatol Case Rep. 2014;8:35-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Graham PM, Altman DA, Gildenberg SR. Panniculitis, pancreatitis, and polyarthritis: a rare clinical syndrome. Cutis. 2018;101:E34-E37. [PubMed] |
| 6. | Narváez J, Bianchi MM, Santo P, de la Fuente D, Ríos-Rodriguez V, Bolao F, Narváez JA, Nolla JM. Pancreatitis, panniculitis, and polyarthritis. Semin Arthritis Rheum. 2010;39:417-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 77] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 7. | Ferri V, Ielpo B, Duran H, Diaz E, Fabra I, Caruso R, Malave L, Plaza C, Rodriguez S, Garcia L, Perez V, Quijano Y, Vicente E. Pancreatic disease, panniculitis, polyarthrtitis syndrome successfully treated with total pancreatectomy: Case report and literature review. Int J Surg Case Rep. 2016;28:223-226. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 8. | Simkin PA, Brunzell JD, Wisner D, Fiechtner JJ, Carlin JS, Willkens RF. Free fatty acids in the pancreatitic arthritis syndrome. Arthritis Rheum. 1983;26:127-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 41] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Loverdos I, Swan MC, Shekherdimian S, Al-Rasheed AA, Schneider R, Fish JS, Ngan BY, Adeli K, Lowe ME, Singh VP, Sevilla WM, Langer JC, Gonska T. A case of pancreatitis, panniculitis and polyarthritis syndrome: Elucidating the pathophysiologic mechanisms of a rare condition. J Pediatr Surg Case Rep. 2015;3:223-226. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 10. | Dong E, Attam R, Wu BU. Board Review Vignette: PPP Syndrome: Pancreatitis, Panniculitis, Polyarthritis. Am J Gastroenterol. 2017;112:1215-1216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |