Published online Jun 26, 2023. doi: 10.12998/wjcc.v11.i18.4406
Peer-review started: March 27, 2023
First decision: May 8, 2023
Revised: May 10, 2023
Accepted: May 24, 2023
Article in press: May 24, 2023
Published online: June 26, 2023
Processing time: 91 Days and 7.5 Hours
Primary prostate Burkitt's lymphoma is a rare and aggressive condition with a poor prognosis. Its clinical presentation can be challenging to differentiate from benign prostatic hyperplasia. Given the rarity of primary prostate Burkitt's lymphoma, its diagnosis and treatment remain unclear.
This report presents a case of a 57-year-old male with primary prostate Burkitt's lymphoma, initially misdiagnosed as prostatic hyperplasia. This case's operative process, intraoperative findings and postoperative management are discussed in detail.
Primary prostate lymphoma is difficult to distinguish from other prostate diseases. Holmium laser enucleation of the prostate (HoLEP), a minimally invasive procedure, is crucial in diagnosing and treating this rare disease. Clinicians should remain vigilant and thoroughly combine physical examination, imaging and test results when encountering patients of younger age with small prostate size but a rapid progression of lower urinary tract symptoms. HoLEP is an essential diagnostic and therapeutic tool in managing primary prostate Burkitt's lymphoma.
Core Tip: Primary prostate Burkitt's lymphoma is a rare and aggressive condition with a poor prognosis. Combined with the analysis of the cases indexed in PubMed and RCA, Only three reports have previously documented Burkitt's lymphoma of the prostate. Holmium laser enucleation of the prostate (HoLEP) is an essential diagnostic and therapeutic tool in managing primary prostate Burkitt's lymphoma. Clinicians should remain vigilant and thoroughly combine physical examination, imaging and test results when encountering patients of younger age with small prostate size but a rapid progression of lower urinary tract symptoms.
- Citation: Wu YF, Li X, Ma J, Ma DY, Zeng XM, Yu QW, Chen WG. Primary prostate Burkitt's lymphoma resected with holmium laser enucleation of the prostate: A rare case report. World J Clin Cases 2023; 11(18): 4406-4411
- URL: https://www.wjgnet.com/2307-8960/full/v11/i18/4406.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i18.4406
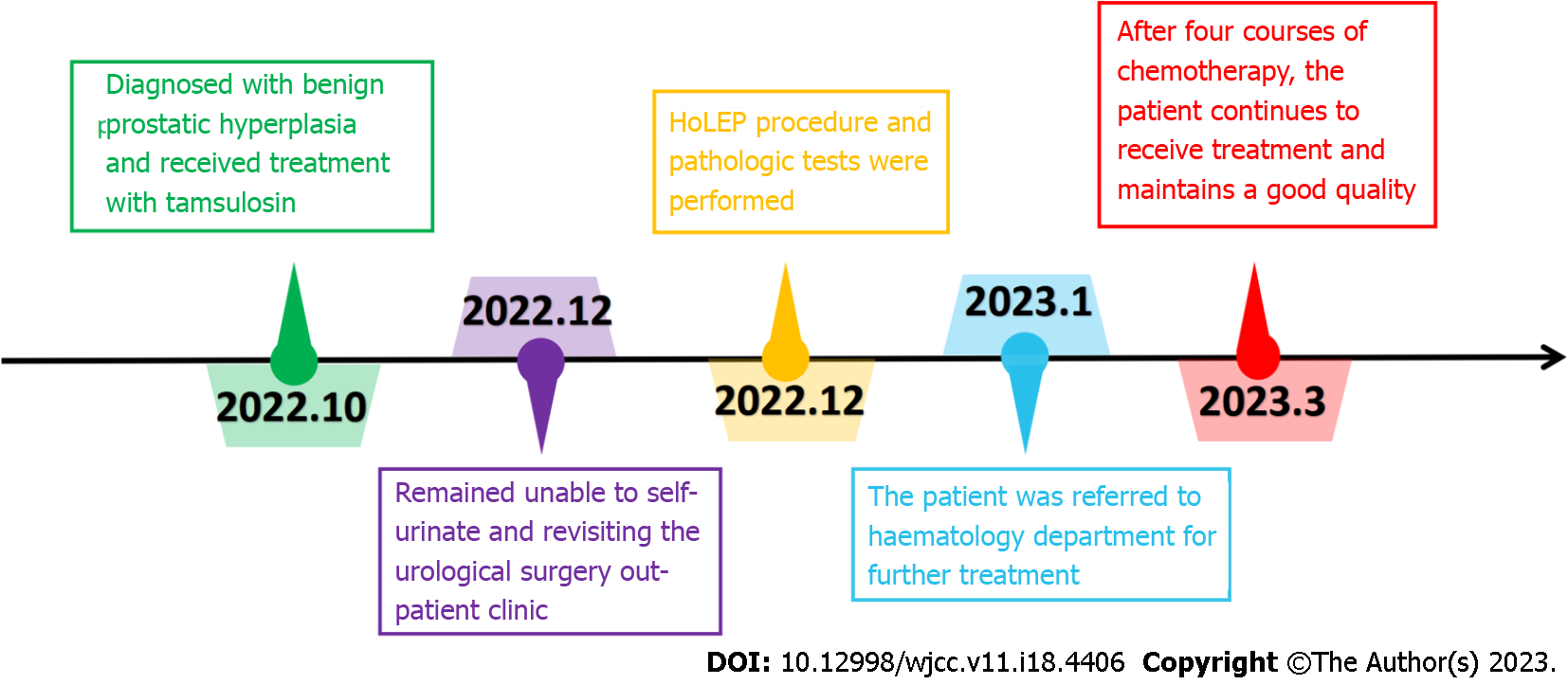
Primary malignant lymphoma of the prostate is exceedingly rare, accounting for a mere 0.09% of all prostate neoplasms and 0.1% of all non-Hodgkin's lymphomas[1]. In the majority of cases, patients are diagnosed with prostatic hyperplasia at the time of surgery, making preoperative diagnosis extremely challenging. While there have been several reports on primary malignant lymphomas of the prostate, most of these malignancies are diffuse large B-cell lymphomas[2]. Only three reports have previously documented Burkitt's lymphoma of the prostate, found through the electronic databases PubMed using the keywords 'Burkitt's lymphoma' and 'prostate'[3-5]. The details of these cases are provided as a supplementary document. Notably, all of the aforementioned patients were identified within the youth population. This report presents a case of primary prostate Burkitt's lymphoma in a middle-aged patient who initially presented with prostatic hyperplasia. The timeline of the case report was shown in Figure 1.
Holmium laser enucleation of the prostate (HoLEP), first introduced by Gilling et al[6] in 1998, has been established as a minimally invasive technique. HoLEP is now considered a reference technique for the surgical treatment of prostatic hyperplasia, offering the same curative effect as transurethral prostatectomy but with a reduced morbidity and complication rate[7].
A 57-year-old Chinese man presented to the urology clinic with unable to self-urinate for two weeks.
After two weeks of having the catheter in place and consistently taking tamsulosin, the patient remained unable to self-urinate.
A 57-year-old male initially visited an outpatient clinic specialising in urological surgery due to urinary urgency and frequency. In October 2022, the patient was diagnosed with benign prostatic hyperplasia (BPH). Despite treatment with tamsulosin, an α-blocker, his symptoms rapidly worsened within two months. Subsequently, he was admitted to the emergency department for acute urinary retention and received an indwelling catheter. After two weeks of having the catheter in place and consistently taking tamsulosin, the patient remained unable to self-urinate. He revisited the urological surgery outpatient clinic in December 2022 and was admitted for BPH. Over the previous two months, the patient experienced no other symptoms, such as fever or weight loss.
The patient denied any family history of malignant tumours.
The patient's physical examination revealed no apparent abnormalities. Digital rectal examination indicated a Grade II prostate, characterised by a firm texture, smooth surface, lack of tenderness and an absent central groove.
Blood routine examination and liver and kidney function test results were within normal limits. The serum total prostate-specific antigen measured 4.30 ng/mL (normal < 4 ng/mL), and the free prostate-specific antigen was 0.42 ng/mL. Routine urine analysis presented no significant abnormalities.
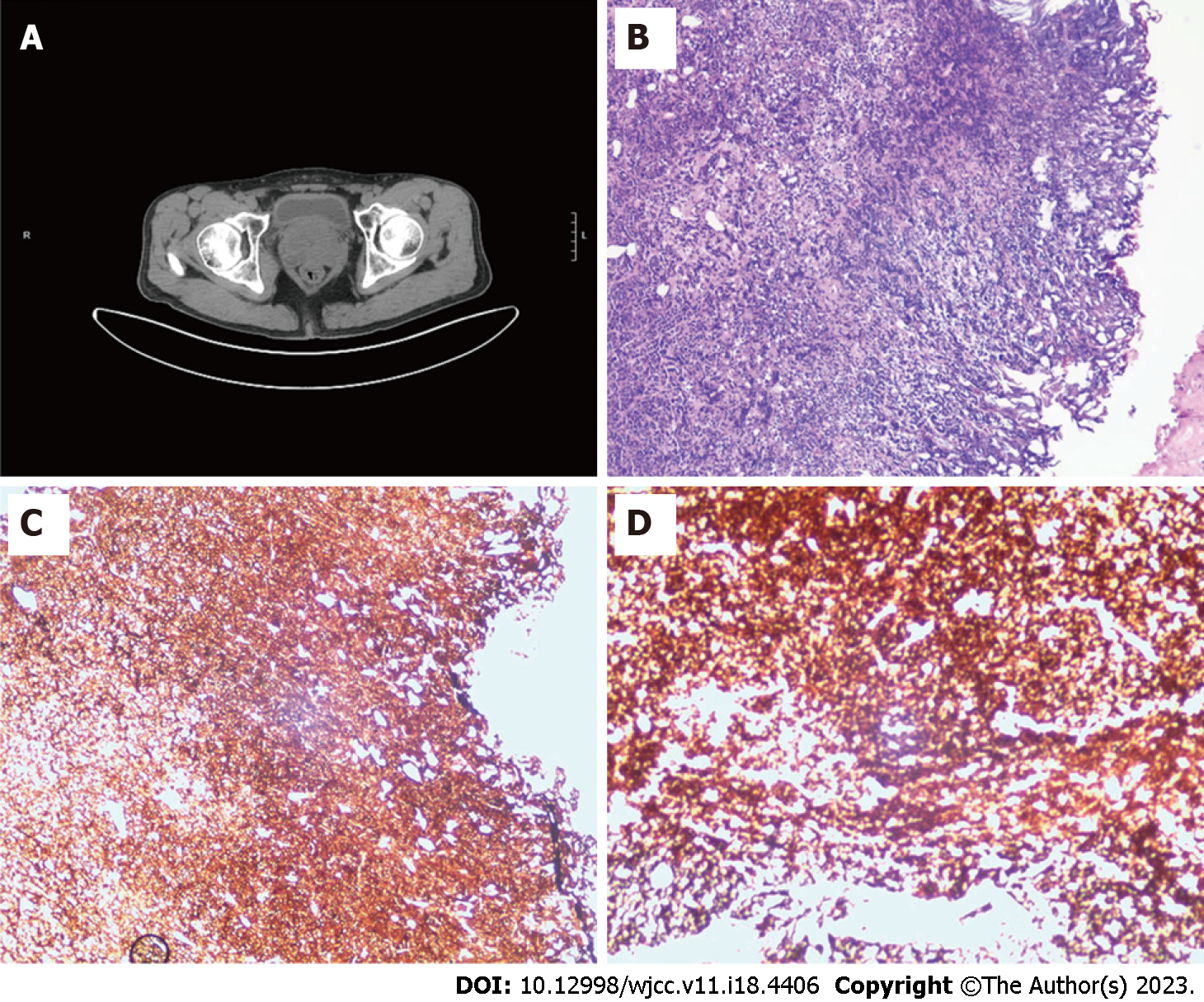
Ultrasound examination of the urinary system demonstrated normal left and right kidneys. Computerised tomography (CT) estimated the prostate size to be approximately 57 mm × 36 mm × 34 mm, with a volume of around 36 mL. The bladder's residual urine volume was approximately 552 mL, as illustrated in Figure 2A. The preoperative international prostate symptom score was 27, and the quality of life (QOL) score was 5. Urodynamic examination indicated a maximum urine flow rate of 6.4 mL/s and an average urine flow rate of 5.2 mL/s.
Based on the aforementioned examinations and tests, the patient was preliminarily diagnosed with prostatic hyperplasia. Upon conducting a physical examination, laboratory tests and imaging, a HoLEP procedure was performed on the patient in December 2022.
The surgeon observed that the patient's prostate tissue was notably swollen, with the left lobe of the prostate exhibiting significant oedema and protruding into the bladder. Additionally, extensive trabeculation was present within the bladder. The prostate tissue's texture was delicate, making it prone to bleeding upon contact. Once the bleeding from the prostate wound was controlled, the excised tissue was collected and submitted for examination. The patient experienced symptom regression following surgery.
Routine histological evaluation and immunohistochemical analysis of the postoperative specimens revealed a highly invasive malignant B-cell lymphoma, specifically Burkitt's lymphoma. The immunohistochemical assessment demonstrated positive CD20 and CD10 markers, while CD3, CD5, CD21 and CD23 were negative. In situ hybridisation for EBER was negative, and second-generation gene sequencing detected mutations in the MYC and TP53 genes (Figure 2B-D).
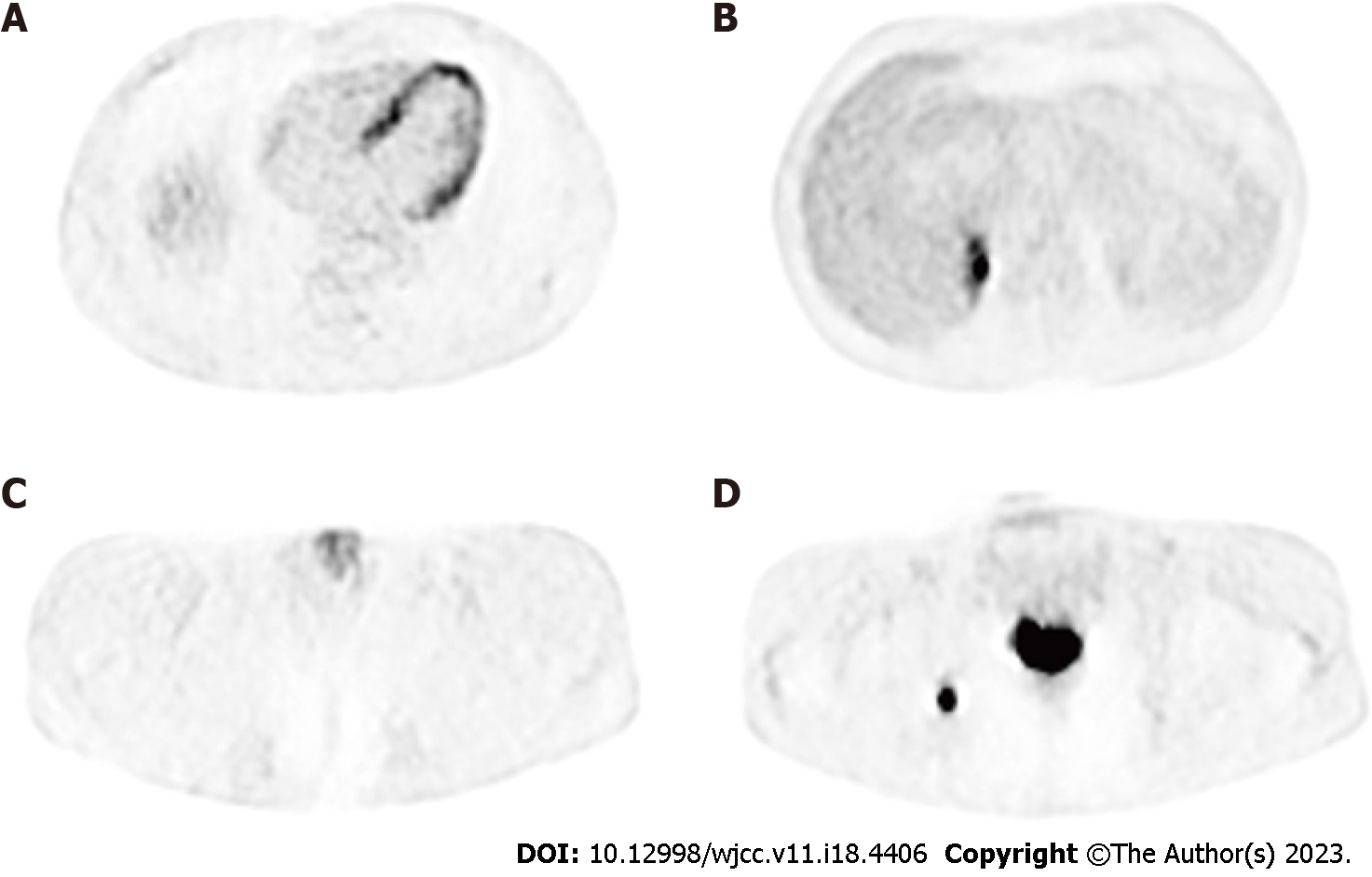
Following the primary prostate Burkitt's lymphoma diagnosis, the patient was immediately referred to our hospital's haematology department for further treatment. A whole-body PET-CT examination was conducted, revealing tumour invasion in the prostate, penis, gastric wall, right adrenal gland and bone marrow, consistent with lymphoma (Figure 3). The patient's Lugano stage was identified as stage IV. Subsequently, the patient underwent a lumbar puncture, with cerebrospinal fluid (CSF) analysis indicating no tumour involvement.
In consultation with our hospital's haematology department, and considering the high invasiveness of the disease, the patient's age, multiple lesions throughout the body, and high tumour load, the haematology experts opted for the COP regimen to reduce tumour load. The specific treatment plan included the following: cyclophosphamide 0.56 g D1, vinorelbine 4 mg D1, dexamethasone 10 mg D0-D6, mesna to prevent cyclophosphamide toxicity and intrathecal injections of methotrexate and cytarabine to prevent central infiltration during a lumbar puncture. Following the COP pre-treatment, the R-COPDAM1 chemotherapy protocol was initiated: rituximab 700 mg D1, vinpocetine 4 mg D2, methotrexate 3.8 g D2, doxorubicin 50 mg D3, cyclophosphamide 0.93 g D3-D5 and dexamethasone 10 mg D2-D6.
To date, the patient has undergone four courses of standard treatment and has exhibited tolerability. After these four courses of chemotherapy, a follow-up whole-body CT scan demonstrated complete remission in response to the therapy. The patient continues to receive treatment and maintains a good quality of life.
Primary malignant lymphoma of the prostate is a rare form of prostate malignancy, accounting for 0.09% of all prostate cancers[1]. In previous reports, most of these malignancies were documented as diffuse large B-cell lymphomas[2], with only three reports documenting Burkitt's lymphoma of the prostate[3-5]. This case presents several unique aspects compared to previous cases, enabling clinicians to better understand this rare disease.
First, patients with Burkitt's lymphoma are typically young people or minors, but in this case, a patient is a middle-aged man. This significant difference from previous literature reports increases the difficulty of preoperative diagnosis. Clinicians tend to misdiagnose such patients as having the more common condition of prostatic hyperplasia.
Furthermore, primary prostate lymphoma is difficult to distinguish from other prostate diseases. Symptoms, imaging and laboratory tests are not significantly different from BPH. To date, the only way to definitively diagnose this condition is through histopathological examination. In this case, the postoperative pathological results suggest Burkitt's lymphoma. A large-diameter core needle or surgical biopsy is necessary to distinguish Burkitt's lymphoma from other invasive lymphomas[8]. We believe that obtaining a large number of tissue samples through minimally invasive surgery, such as HoLEP with minimal trauma, plays a vital role in diagnosis. Our approach has also greatly improved the patient's lower urinary tract symptoms and quality of life. However, radical surgical tumour reduction is unnecessary for patients with Burkitt's lymphoma, as postoperative recovery may delay the start of systemic treatment, ultimately affecting disease management.
Regarding treatment, a consensus on the treatment plan for primary prostate lymphoma has not been reached. The conventional non-Hodgkin lymphoma chemotherapy plan is usually the mainstream method. In this case, the PET/CT of the patient showed multiple extranodal invasions, while bone marrow and CSF examinations were negative. Considering the high invasiveness of Burkitt's lym
In conclusion, early diagnosis and appropriate treatment can increase survival time and improve patients' QOL with prostate lymphoma. In this case, the patient's lower urinary tract obstruction symptoms were improved while obtaining pathological specimens via the HoLEP[9,10] minimally invasive method. Despite misdiagnosis before the operation, the patient achieved satisfactory results through multidisciplinary consultation and reasonable treatment. Clinicians should be vigilant and thoroughly combine physical examination, imaging and test results when encountering patients of a younger age with a small prostate but with a rapid progression of lower urinary tract symptoms.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Urology and nephrology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gaman MA, Romania; Sarier M, Turkey S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Warrick JI, Owens SR, Tomlins SA. Diffuse large B-cell lymphoma of the prostate. Arch Pathol Lab Med. 2014;138:1286-1289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Hu S, Wang Y, Yang L, Yi L, Nian Y. Primary non-Hodgkin's lymphoma of the prostate with intractable hematuria: A case report and review of the literature. Oncol Lett. 2015;9:1187-1190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Chavarriaga J, Arenas J, Medina M, Meek E, Perez J, Fernandez N. Do not Forget Burkitt´s Lymphoma! Unusual Case of Primary Malignant Lymphoma of the Prostate in a Young Patient. Urology. 2020;138:152-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Derigs M, Pehl A, Riera-Knorrenschild J, Hofmann R, Hegele A. Burkitt's lymphoma of the prostate presenting as acute urinary retention: a case report. BMC Urol. 2020;20:53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Sinclair N, Babyn P, Kinloch M, Sinha R. A Rare and Unusual Case of Burkitt's Lymphoma Presenting with a Prostate Mass in a 12-Year-Old Boy. Case Rep Radiol. 2014;2014:106176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Gilling PJ, Kennett K, Das AK, Thompson D, Fraundorfer MR. Holmium laser enucleation of the prostate (HoLEP) combined with transurethral tissue morcellation: an update on the early clinical experience. J Endourol. 1998;12:457-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 237] [Cited by in RCA: 249] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 7. | Vincent MW, Gilling PJ. HoLEP has come of age. World J Urol. 2015;33:487-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 86] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 8. | Olszewski AJ, Jakobsen LH, Collins GP, Cwynarski K, Bachanova V, Blum KA, Boughan KM, Bower M, Dalla Pria A, Danilov A, David KA, Diefenbach C, Ellin F, Epperla N, Farooq U, Feldman TA, Gerrie AS, Jagadeesh D, Kamdar M, Karmali R, Kassam S, Kenkre VP, Khan N, Kim SH, Klein AK, Lossos IS, Lunning MA, Martin P, Martinez-Calle N, Montoto S, Naik S, Palmisiano N, Peace D, Phillips EH, Phillips TJ, Portell CA, Reddy N, Santarsieri A, Sarraf Yazdy M, Smeland KB, Smith SE, Smith SD, Sundaram S, Zayac AS, Zhang XY, Zhu C, Cheah CY, El-Galaly TC, Evens AM. Burkitt Lymphoma International Prognostic Index. J Clin Oncol. 2021;39:1129-1138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 43] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 9. | Ramadhani MZ, Kloping YP, Rahman IA, Yogiswara N, Renaldo J, Wirjopranoto S. Comparative efficacy and safety of holmium laser enucleation of the prostate (HoLEP) using moses technology and standard HoLEP: A systematic review, meta-analysis, and meta-regression. Ann Med Surg (Lond). 2022;81:104280. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Large T, Krambeck AE. Evidence-based outcomes of holmium laser enucleation of the prostate. Curr Opin Urol. 2018;28:301-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |