Published online Jun 26, 2023. doi: 10.12998/wjcc.v11.i18.4392
Peer-review started: March 10, 2023
First decision: April 11, 2023
Revised: May 15, 2023
Accepted: May 25, 2023
Article in press: May 25, 2023
Published online: June 26, 2023
Processing time: 108 Days and 9 Hours
The diagnosis and therapy during surgery depend largely on a full account of anatomic characteristics. Apart from regular structures, the common, less common or even uncommon anatomic variations are critical for procedural planning. This is especially true during craniocerebral microsurgery, where small vascular variations can affect the final surgical results and patient prognosis.
Herein, two rare variations concerning the A1 (horizontal) segment of anterior cerebral artery (ACA1) were introduced. One enabled the communication between perforating branch of ACA1 and dural artery of anterior skull base, which was discovered during autopsy. The other was ophthalmic artery (OA) originating from ACA1, shown on digital angiography.
In this study, we found two rare anatomical variations. One was an abnormal OA originated from the anterior communicating artery. The other was a perforating branch of the A1 segment of the anterior cerebral artery, which communicated with meningeal vessels in the anterior skull base. This finding is of great significance for the treatment of anterior communicating artery aneurysm or in other anterior skull base surgery.
Core Tip: In the process of anatomy of human specimens and cerebral angiography of patients, we found the unusual abnormal anatomical structure, that is, the communication between the perforating branch of anterior cerebral artery (ACA1) and the dura mater vessels of the anterior skull base, and the abnormal ophthalmic artery originated from ACA1, which is very useful for us to understand the abnormal structure of cerebral vessels.
- Citation: Mo ZX, Li W, Wang DF. Perforating and ophthalmic artery variants from the anterior cerebral artery: Two case reports. World J Clin Cases 2023; 11(18): 4392-4396
- URL: https://www.wjgnet.com/2307-8960/full/v11/i18/4392.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i18.4392
Comprehensive anatomic realization constitutes a prerequisite for surgical interventions. In addition to the normal anatomical structures, rare variations should also be recognized, as unintentional omission may result in immeasurable losses. For craniocerebral microsurgery, minor variation in cerebral arteries informs operational procedures and outcomes. Some small perforating arteries begin at the A1 segment of the anterior cerebral artery (ACA1) to supply the anterior perforated substance, dorsal surface of optic nerve, chiasm, tract, and fissure of Sylvian[1]. Prior reports have identified the appearance of ophthalmic artery (OA) at the location where the internal carotid artery (ICA) penetrates the dura mater[2]. Approximately half of the ophthalmic arteries come from the anteromedial side of the ICA, about 33% from the upper medial side, 7% from the medial side, and less than 2% from the upper anterior side[2]. However, the perforating branch of the anterior communicating artery rarely communicates with the dural branch of the anterior skull base[2]. In this report, variation in the perforating artery connecting ACA1 and anterior skull base dural arteries, as well as OA deriving from ACA1 was presented and discussed.
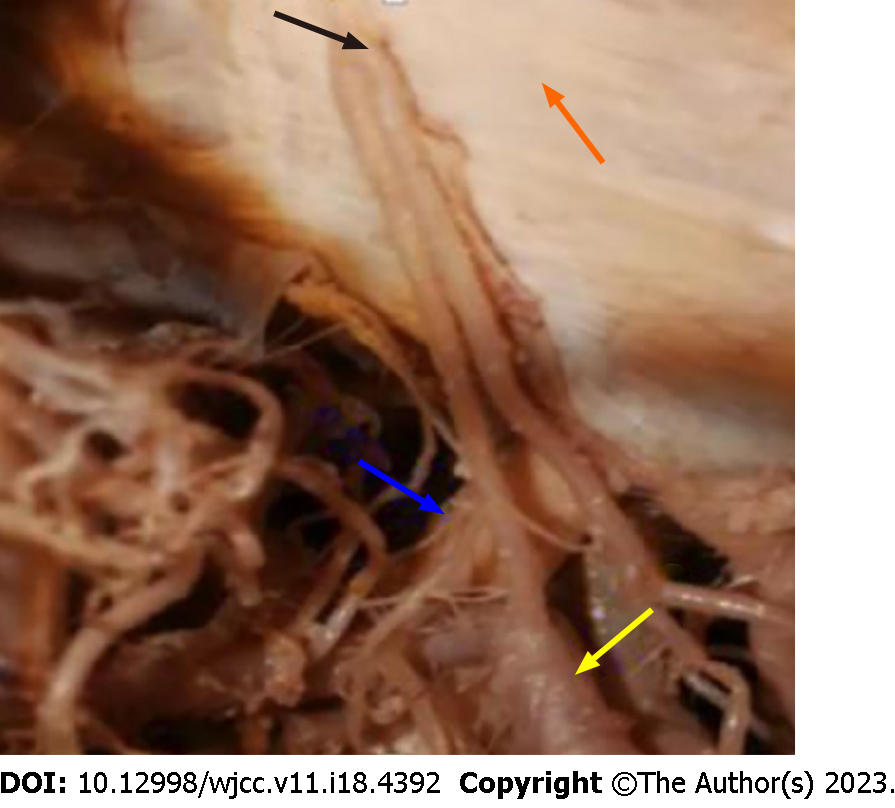
Case 1: A segmental right anterior cerebral artery was revealed in a cadaver specimen of an elderly male donor, whose cause of death was unknown. The autopsy was carried out in the Department of Anatomy, Medical College of Qinghai University. Upon dissection under a microscope, a variant ACA1 perforating artery was unveiled, which originated from the anterior superior wall of segment A1 and ended in the dura mater of the ipsilateral anterior skull base. Many of its small branches communicated with meningeal vessels (Figure 1).
Case 2: A 51-year-old female was admitted to the Qinghai Provincial People's Hospital for “sudden dizziness with intermittent nausea and vomiting for 8 h”.
Case 1: This was an autopsy and there was no current medical history.
Case 2: The patient had sudden dizziness with intermittent nausea and vomiting within the last 8 h.
Case 1: There was no past illness.
Case 2: The patient had a 3 year history of hypertension, which was managed using oral antihypertensive drugs.
Case 1: The patient has no family history.
Case 2: The patient denied any family history of malignant tumors.
Case 1: This was an autopsy and there was no physical examination.
Case 2: On physical examination, the vital signs were as follows: Body temperature, 36.5°C; blood pressure, 168/97 mmHg; heart rate, 82 beats per min; respiratory rate, 19 breaths per min; clear mind; stiff neck; normal limb movement.
Case 1: No examinations.
Case 2: No abnormality was found in routine blood test.
Case 1: Under the microscope, a variant ACA1 perforating artery was unveiled, which originated from the anterior superior wall of segment A1 and ended in the dura mater of the ipsilateral anterior skull base.
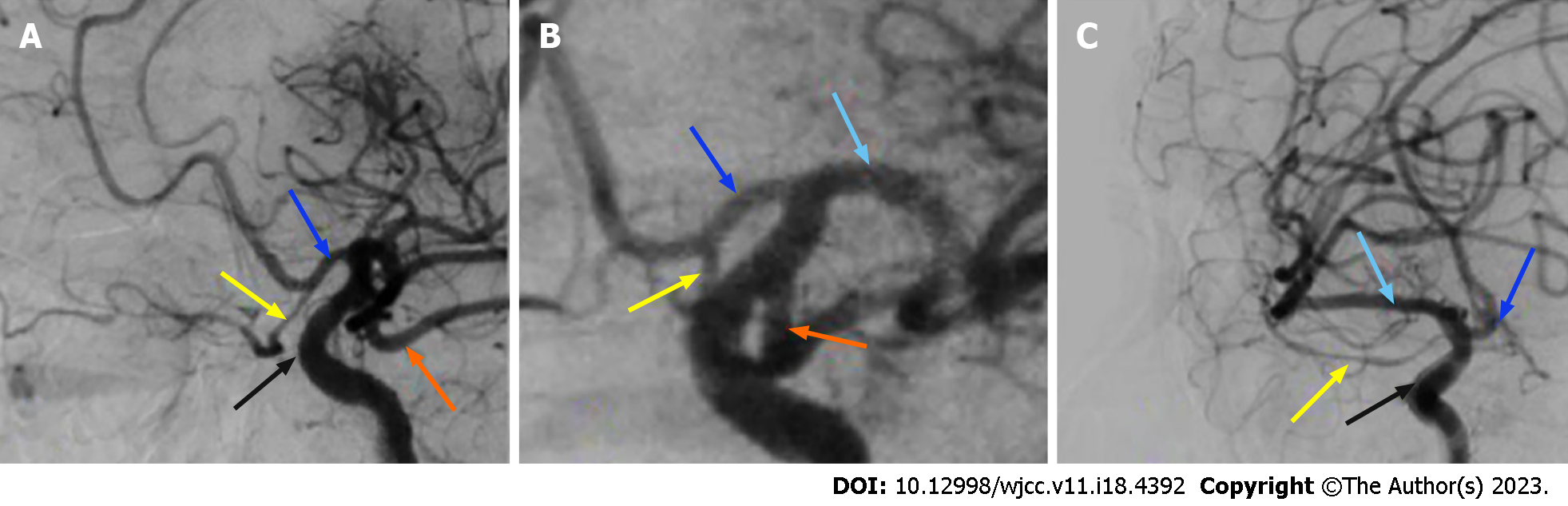
Case 2: Emergency head computed tomography showed a cerebellar hemorrhage broken into the fourth ventricle. Digital subtraction angiography (DSA) found a superior cerebellar artery aneurysm, ocular artery origin variation (bilateral OA originating from ACA1) and left embryonic posterior cerebral artery.
Case 1: Final diagnosis is unknow.
Case 2: Considering the patient’s medical history, the final diagnosis was superior cerebellar aneurysm.
Case 2: The superior cerebellar artery aneurysm was embolized using a simple coil. Other treatments included lumbar puncture and drainage, intracranial pressure reduction and analgesia.
Case 2: The patient recovered well without any complication.
At five week of embryonic gestation, the anterior cerebral artery appears as the secondary branch of the primitive olfactory artery. At six week, the plexiform anterior communicating artery converges with the contralateral anterior communicating artery. The primitive olfactory artery usually originates from the ICA, runs along the olfactory tract and supplies the distal region of ACA1[3].
The ACA1 emanates from ICA in medial segment of lateral fissure, lateral optic chiasma, and lower part of anterior perforating branch, which then moves forward in the basal frontal lobe and endplate cisterna. After arriving at the longitudinal fissure, it reaches the anterior communicating artery and proceeds as the ACA2 segment. The ACA1 segment sprouts out an average of eight perforating arteries, including the internal capsule and Heubner recurrent artery, which provide abundant blood supply to the cauda nucleus. Most of the perforating arteries stem from the posterior and superior wall of the ACA1 and primarily supply blood to the anterior parenchyma, dorsal side of the optic chiasmatic, dorsal side of the optic nerve, optic tract and upper part of the optic nerve in the hypothalamus. Recurrent injury of Heubner artery usually leads to hemiplegia, primarily in the upper arm, while injury to the perforating artery causes emotional disorders, personality changes, mental decline, anxiety, and mental disorders. In the present study, one of the ten autopsy specimens showed mutant perforating arteries (Figure 1), which originated from anterior superior wall of ACA1 and then forward to the dural artery of skull base. With multiple small branches communicating with the dural artery, it returned to the anterior perforated substance. Unfortunately, due to lack of cerebrovascular angiography in cadaver specimens, it is unclear whether there were traffic branches between varied perforating artery and branches of dural artery or ophthalmologic arteries. This kind of variation is relatively rare and should be noticed during embolization of vascular malformations at the anterior skull base in order to avoid the escape of embolization agent. When the embryo develops to 4-8 mm, the OA begins to develop[4]. The main variation of OA is from the spongy segment of the ICA[5]. Other less common variants are OA from ACA, or the origin of the middle meningeal artery[6]. A very unusual anomalous origin of OA from basal stem has been described previously[4]. With development of embryo, the ventral OA degenerates and forms the original OA, which is derived from ICA. In the second case presented in the current work, DSA of intracranial aneurysms detected another rare variation, showing the bilateral ocular artery originating from distal end of ACA1 segment (Figure 2).
OA forms the first branch of ICA, opening at the superior segment and serving as the main blood supply of orbital tissues. Generally, the OA may appear where the ICA penetrates the dura mater. About half of the OA comes from the anteromedial side of ICA, 33% from upper medial side, 7% from medial side, and less than 2% from upper anterior side[2]. The perforating branch of anterior communicating artery rarely communicates with dural branch of anterior skull base[2]. Few ophthalmic arteries originate from cavernous, bed processes and middle meningeal arteries of ICA while most (57%) are from anterior medial side of anterior knee. Other possible originations of OA involve superior medial (35%), medial (7%) or anterior superior (1%) of the ICA[7]. It is often reported that the OA or main branches of OA stems entirely from middle meningeal artery; however, the anterior cerebral artery or basilar artery is rarely mentioned. In traffic aneurysm clip craniotomy or interventional embolization, misidentification of OA may lead to blindness.
In conclusion, robust anatomic knowledge comes as a fundamental requirement for the surgeon, which includes not only the normal anatomic structures, but also potential abnormal features. In clinical practice, unanticipated anatomy could lead to procedural complications that contribute to adverse surgical outcomes.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Clinical neurology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Hegazy AA, Egypt; Kawabata H, Japan S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | Campero A, Baldoncini M, Martinez J, Villalonga JF, Lucifero AG, Luzzi S. Microneurosurgical management of aneurysms of the A1 segment of the anterior cerebral artery: Anatomy and surgical technique. Surg Neurol Int. 2022;13:310. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 2. | Parlato C, di Nuzzo G, Luongo M, Tortora F, Briganti F. Anatomical variant of origin of ophthalmic artery: case report. Surg Radiol Anat. 2011;33:275-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Ogawa Y, Soejima K, Kawahara I, Shiozaki E, Morofuji Y, Ono T, Haraguchi W, Tsutsumi K. A1 Segment Unruptured Aneurysm of Persistent Primitive Olfactory Artery Coexisted with Accessory Middle Cerebral Artery. J Stroke Cerebrovasc Dis. 2021;30:105758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Rivera R, Choi IS, Sordo JG, Giacaman P, Badilla L, Bravo E, Echeverria D. Unusual origin of the left ophthalmic artery from the basilar trunk. Surg Radiol Anat. 2015;37:399-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Bracard S, Liao L, Zhu F, Gory B, Anxionnat R, Braun M. The ophthalmic artery: a new variant involving two branches from the supracavernous internal carotid artery. Surg Radiol Anat. 2020;42:201-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Matsuura K, Uchino A, Saito N, Ishida J, Suzuki T. Carotid-anterior cerebral artery (ACA) anastomosis associated with azygos ACA and ophthalmic artery arising from the middle meningeal artery: a case report. Surg Radiol Anat. 2020;42:211-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Bonasia S, Smajda S, Ciccio G, Bojanowski MW, Robert T. Embryology of the anterior communicating artery complex: implications on possible adult variants. Surg Radiol Anat. 2022;44:737-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |