Published online Jun 26, 2023. doi: 10.12998/wjcc.v11.i18.4384
Peer-review started: March 22, 2023
First decision: April 10, 2023
Revised: April 18, 2023
Accepted: May 12, 2023
Article in press: May 12, 2023
Published online: June 26, 2023
Processing time: 96 Days and 10.4 Hours
Fibromatosis-like metaplastic carcinoma is classified as a rare type of metaplastic carcinoma of the breast by the 2012 WHO pathological and genetic classification criteria for breast tumors, which takes hyperplastic spindle cells as the main component and is often misdiagnosed as benign stromal proliferative lesions or benign mesenchymal tumors of the breast because of its mild morphology. Here, we collected the clinical data of 2 cases of fibromatosis-like metaplastic carcinoma of the breast and performed pathomorphological observation and immunohistochemical staining of the surgically resected specimens. According to the clinical features, imaging features, immunophenotype, diagnosis and differential diagnosis of 2 cases of fibromatosis-like metaplastic carcinoma of the breast, it was further differentiated.
Case 1: A 56-year-old postmenopausal female was admitted due to "right breast mass for over 1 year and local ulceration for over 1 mo". Physical examination showed a mass with a diameter of 4.5 cm × 5.5 cm palpable at 2.5 cm from the nipple at 1 o'clock in the right breast. The skin on the surface of the mass ruptured about 3 cm, with a small amount of exudation and bleeding, less clear boundary, hard texture, fair activity, without obvious tenderness. No obvious abnormality was palpable in the left breast. No enlarged lymph nodes were palpable in the bilateral axillae and bilateral supraclavicular region. After removing the mass tissue, it was promptly sent to the pathology department for examination. Case 2: Female, 52-years-old, premenopausal, admitted due to "right breast mass for more than 3 mo". Physical examination showed a 4.0 cm × 4.0 cm diameter mass palpable at 2.0 cm of the nipple in the lower outer 7 o'clock direction of the right breast, with less clear boundary, hard texture, fair activity, no significant tenderness, no palpable significant abnormalities in the left breast, and no palpable enlarged lymph nodes in the bilateral axillae and bilateral supraclavicular region. The mass was resected and sent for pathological examination. Postoperative pathological examination revealed fibromatosis-like metaplastic carcinoma of the breast in both patient 1 and patient 2. No systemic therapy and local radiotherapy were performed after surgery, and no tumor recurrence or metastasis was observed.
Fibromatosis-like metaplastic carcinoma of the breast is a rare subtype of metaplastic carcinoma that is often misdiagnosed, and the diagnosis relies on medical history collection, complete sampling, and full use of immunohistochemical assessment. The risk of lymph node and distant metastasis is low, and the current treatment is based on complete surgical resection. The efficacy of systemic radiotherapy and chemotherapy is not clear.
Core Tip: Fibromatosis-like metaplastic carcinoma is a rare type of metaplastic carcinoma of the breast with proliferating spindle cells as the main component, which is often misdiagnosed as low-grade mesenchymal tumors or proliferative lesions because of its mild morphology. Two cases of fibromatosis-like metaplastic carcinoma of the breast were reported and the literatures were reviewed. The pathological features were observed to ensure the correct diagnosis.
- Citation: Bao WY, Zhou JH, Luo Y, Lu Y. Fibromatosis-like metaplastic carcinoma of the breast: Two case reports. World J Clin Cases 2023; 11(18): 4384-4391
- URL: https://www.wjgnet.com/2307-8960/full/v11/i18/4384.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i18.4384
Metaplastic carcinoma of the breast (MBC) is a rare but aggressive form of breast cancer that accounts for less than 0.5% of all breast cancers. It has been recognized as a distinct pathological entity by the World Health Organization. Morphologically, it is characterized by differentiation of the neoplastic epithelium into squamous cells and/or mesenchymal elements (squamous cells, spindle cells, cartilage or bone, etc.)[1,2]. Fibromatosis-like metaplastic carcinoma (FLMCa), a subtype of MBC, is a very rare metaplastic carcinoma[3]. FLMCa is a locally aggressive tumor with low likelihood of lymph node and distant metastasis, but tends to recur after resection[4]. Therefore, understanding the histological features of FLMCa may be important for the treatment of FLMCa.
FLMCa is a low-grade tumor formed by spindle cells with mild or absent nuclear atypia. The tumor is dominated by spindle cells, which may be mixed with a small proportion of ductal or lobular carcinoma components of the breast[5,6]. Gobbi et al[7] found that low-grade spindle cells accounted for more than 95% of the total tumor area, and epithelial cells or low-grade carcinomas accounted for less than 5% of cases in 30 breast swelling samples. One of the main features of FLMCa is low-grade spindle cell proliferation, which is mainly characterized by infiltrative, focal mild atypia, and focal epithelioid differentiation[8]. Accurate diagnosis of FLMCa is very difficult due to morphological overlap with other low-grade spindle cell lesions and is often misdiagnosed as benign stromal proliferative lesions or benign mesenchymal tumors of the breast because of its mild morphology[9]. Understanding different morphologic, immunohistochemical, and molecular features is therefore important for diagnosis. In this study, we report on 2 cases of FLMCa that provide insights regarding the histological aspects.
Case 1: A 56-year-old postmenopausal female patient was admitted due to "right breast mass for more than 1 year and local ulceration for over 1 mo".
Case 2: Patient 2 was a 52-year-old premenopausal woman who was admitted to our hospital due to a right breast mass for more than 3 mo.
Case 1: The patient was found to have a mass in the right breast for more than 1 year. The tumor gradually increased in size, with hard texture, poor activity, no tenderness and nipple discharge, and no treatment was performed. One month ago, local ulceration of the right breast was found, and a mass with a diameter of 4.5 cm × 5.5 cm was palpable 2.5 cm from the nipple at 1 o'clock in the right breast. The skin on the surface of the mass ruptured about 3 cm, with a small amount of exudation and bleeding, less clear borders, hard texture, fair activity, and no significant tenderness. There was no remission in recent days, and the patient visited our hospital for further treatment.
Case 2: The patient found a mass in the right breast for more than 3 mo, which was located at 7 o'clock outside and below the right breast, and a mass with a diameter of 4.0 cm × 4.0 cm could be palpated 2.0 cm from the nipple, with less clear boundary, hard texture, fair activity, and no obvious tenderness. No treatment was performed during this period. The patient came to our hospital today for diagnosis and treatment.
Case 1: The patient had good physical fitness, denied the medical history of "hypertension and diabetes” and infectious diseases history such as "hepatitis and tuberculosis". There was no history of surgery, trauma, blood transfusion, poisoning, food or drug allergy, and the vaccination history was unknown.
Case 2: The patient denied any history of hepatitis, tuberculosis, malaria, hypertension, heart disease, diabetes, cerebrovascular disease, mental illness, surgery, trauma, blood transfusion, food or drug allergy, and had received the hepatitis B vaccination.
Case 1: The patient was born in her native country, and had not been to other places for a long time; had no history of exposure to schistosomiasis infected water; no history of exposure to poisons, with regular daily life, no bad habits, and no history of major mental trauma. All family members were healthy and denied any genetic history of family diseases.
Case 2: The patient was born in her native country, and had not been to other places for a long time; had no history of exposure to schistosomiasis-infected water; no history of exposure to poisons, with regular daily life, no bad habits, and no history of major mental trauma. All family members were healthy and denied any genetic history of family diseases.
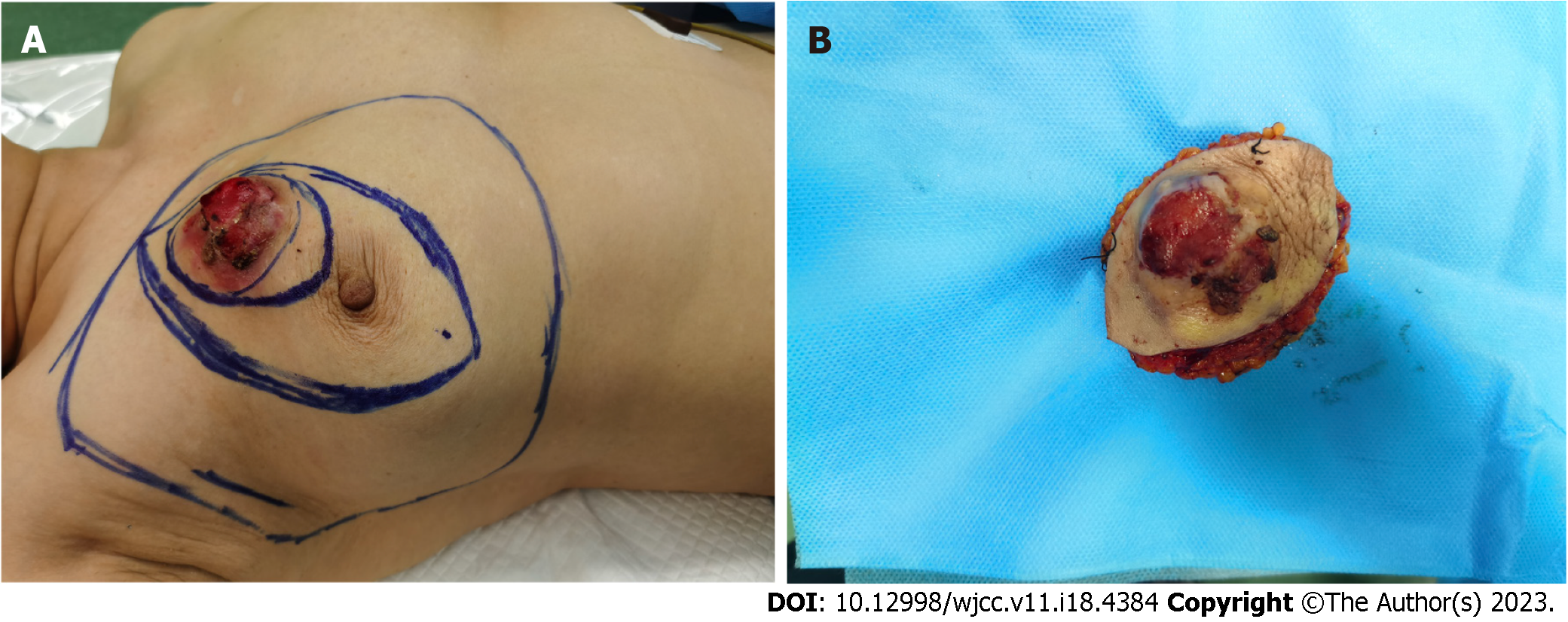
Case 1: A mass with a diameter of 4.5 cm × 5.5 cm was palpable 2.5 cm from the nipple at 1 o'clock in the right breast, and the skin on the surface of the mass had ruptured about 3 cm, with a small amount of exudation and bleeding, less clear borders, hard texture, fair activity, no significant tenderness, no significant abnormalities palpable in the left breast, and no palpable enlarged lymph nodes in the bilateral axillae and bilateral supraclavicular regions (Figure 1A and B).
Case 2: Physical examination showed a 4.0 cm × 4.0 cm diameter mass palpable at 2.0 cm of the nipple in the lower outer 7 o'clock direction of the right breast, with less clear boundary, hard texture, fair activity, no significant tenderness, no palpable significant abnormalities in the left breast, and no palpable enlarged lymph nodes in the bilateral axillae and bilateral supraclavicular region.
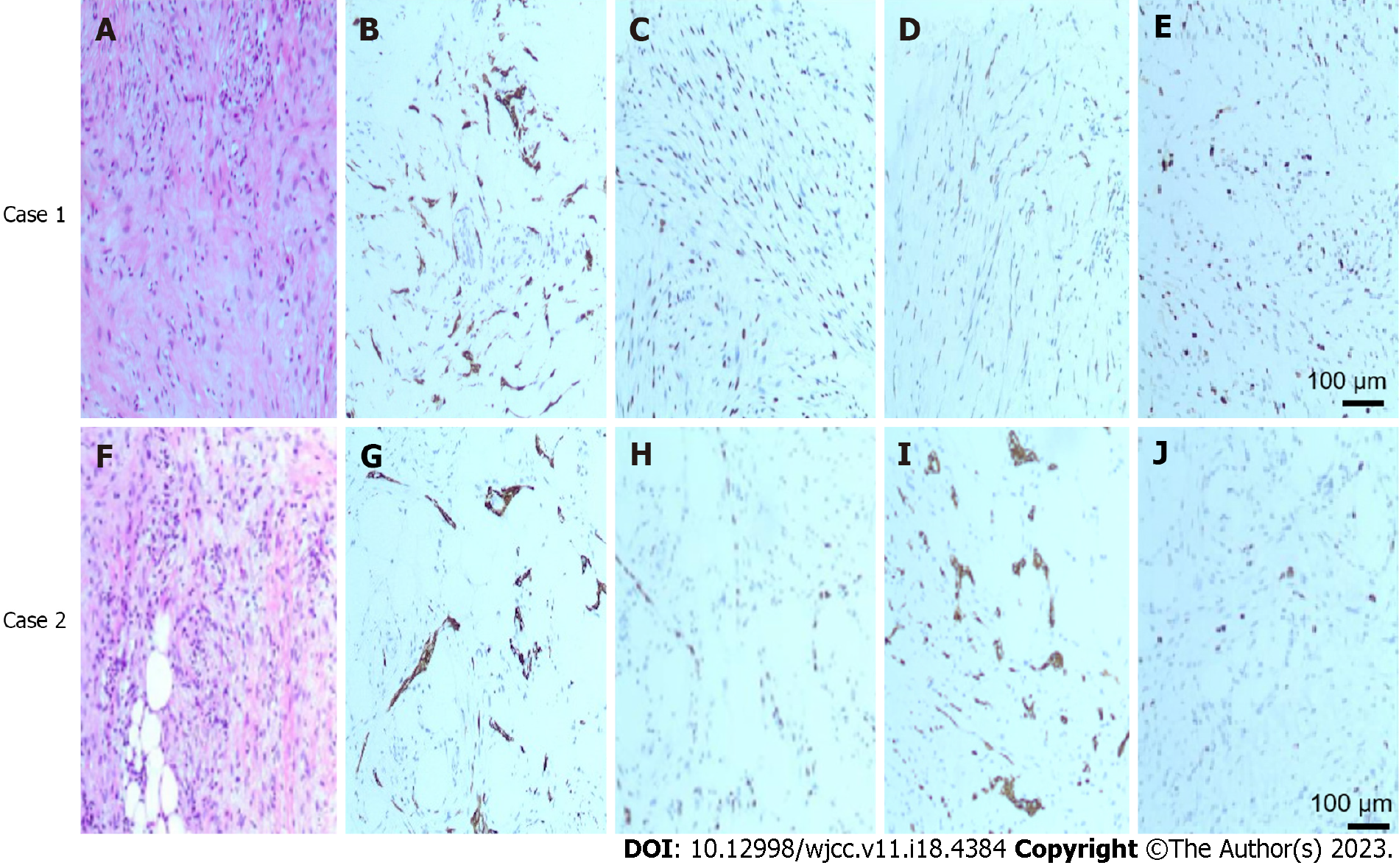
Case 1: The tumor puncture tissue was sent for pathological examination to consider sclerosing adenopathy, and the mass was sent for pathological examination after complete resection. Immunohistochemical examination revealed that the tumor was composed of spindle cells with mild morphology and mild atypia of the tumor cells. Envision was used to detect CKPan, P63 and CK5/6 positive in tumor cells, and the Ki-67 positive index was about 15% (Figure 2A and E). Diagnosis of fibromatosis-like MBC was confirmed.
Case 2: Tumor puncture was performed, and pathology showed puncture tissue, followed by pathological examination, considering fibromatosis-like MBC. The tumor was composed of spindle cells with mild morphology, and the tumor cells were mildly atypical. Envision assay showed that CKPan, P63 and CK5/6 were positive in tumor cells, and the Ki-67 positive index was about 20% (Figure 2F and J).
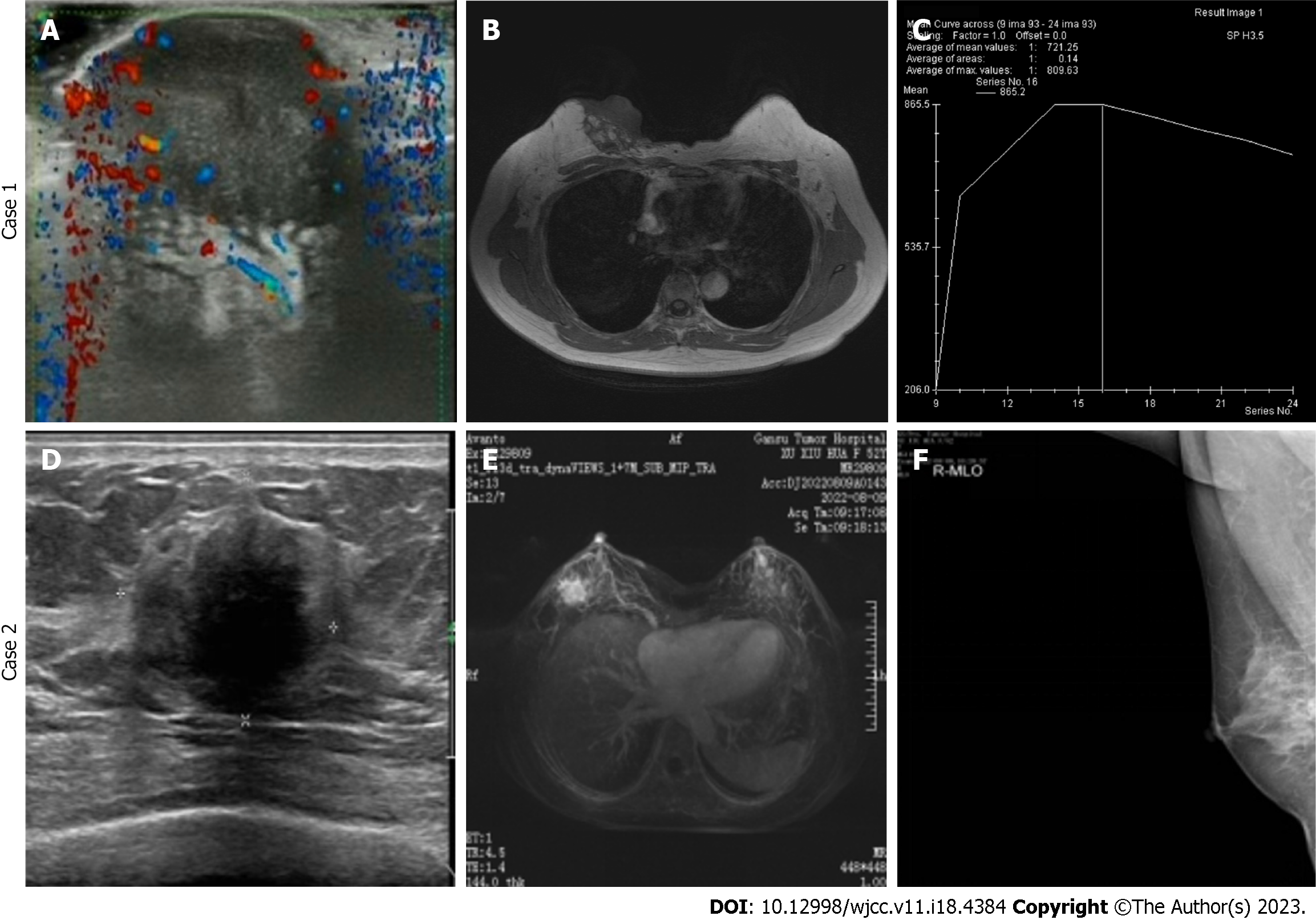
Case 1: After admission, ultrasound and magnetic resonance imaging (MRI) were performed, which revealed breast imaging reporting and data system (BI-RADS) grade V (Figure 3A and C). Computed tomography showed a right breast mass and was considered a malignancy. Breast tumor markers were unremarkable.
Case 2: After admission, breast ultrasound and MRI were performed, and revealed breast cancer BI-RADS grade IVc (Figure 3C and D), and molybdenum target examination revealed breast cancer BI-RADS grade IVb (Figure 3E), both of which suggested the possibility of malignant tumors in the right breast.
Cases 1 and 2: FLMCa of the right breast.
Case 1: The patient was given a simple mastectomy of the right breast + axillary sentinel lymph node biopsy after complete resection of the right breast mass.
Case 2: Complete resection of the right breast mass was followed by simple mastectomy of the right breast + axillary sentinel lymph node biopsy.
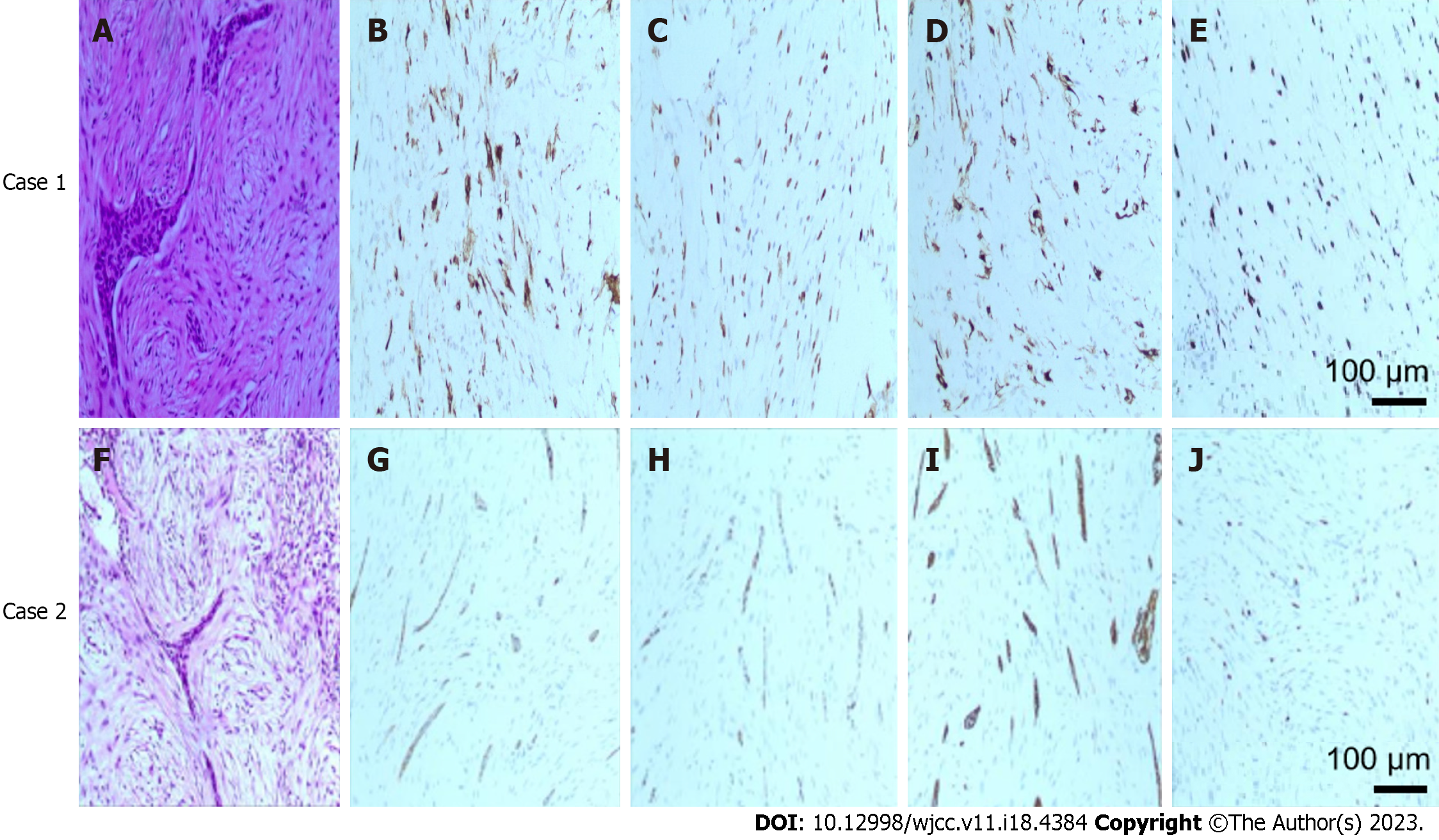
Postoperative pathology showed FLMCa of the right breast (3 cm × 4.5 cm) with ulceration of the skin surface. Pathological examination showed that the tumor was composed of spindle cells with mild morphology, and in immunohistochemical staining, the tumor cells were ER (−), PR (−), HER-2 (0), Ki-67 (+ 10%), CK5/6 (+), P63 (+), calponin (+), B-Catenin (+), S-100 (local +), CK8/18 (+), CD34 (vascular +), BcL-2 (−), SMA (+), Desmin (−), Caldesmon (−), and CD10 (+) (Figure 4A and E).
No systemic therapy and local radiotherapy were performed after surgery, and no tumor recurrence or metastasis was observed 11 mo after follow-up.
Postoperative pathology revealed a right breast mass size (2.0 cm × 1.7 cm), FLMCa of the right breast, cancer tissue invading the surrounding adipose tissue, and atypical hyperplasia of the ductal epithelium around the cancer. Under the original incision, hyperplasia of mammary glands, sclerosing adenopathy, common hyperplasia of ductal epithelium, massive angiectasia, congestion, foreign body granuloma and fat necrosis formation were observed, without clear residual tissue. Pathological examination revealed that the tumor was composed of spindle cells with mild morphology and mild atypia of the tumor cells. Immunohistochemistry showed tumor cells ER (-), PR (-), HER-2 (0), Ki-67 (+ 20%), E-caherin (-), P120 (plasma +), CKpan (+), CK5/6 (+), P63 (+), SMA (+), CKH (partial +), P40 (partial +), calponin (-), AR (-), GATA-3 (-), SOX-10 (-), B-Catenin (partial plasma +), CK8/18 (-), CK7 (-), CD31 (vascular endothelium +), CD34 (vascular endothelium +), S-100 (local +) (Figure 4F and J). No systemic therapy and local radiotherapy were performed after surgery, and no tumor recurrence or metastasis was observed 15 mo after surgery.
FLMCa of the breast, a very rare variant of breast tumors, is a newly described metaplastic tumor in the 2012 WHO classification of breast tumors (4th edition). Low-grade fibromatosis-like spindle cell carcinoma is a very rare breast cancer, accounting for < 0.5% of all breast cancers[10,11]. It is a low grade tumor formed by spindle cells with mild or absent nuclear atypia embedded in collagenized stroma, and only < 5% of tumor cells exhibit epithelial traits[12,13]. Because its biological behavior is superior to that of spindle cell metaplastic carcinoma in general, this cancer type was added to the new WHO classification[14]. Because of its mild morphology, FLMCa is frequently misdiagnosed as benign stromal proliferative lesions or benign mesenchymal tumors, and usually requires conservative treatment because of its favorable clinical outcome[15]. Accurate diagnosis is therefore a challenging task, particularly in core biopsies.
Histopathologically, FLMCa is a spindle cell metaplastic carcinoma with mild morphology characterized histologically by spindle cells with mild morphology arranged in wavy, fascicular, and woven patterns. Also, the cellular stroma was collagenized to varying degrees, resembling fibromatosis of soft tissue, and showed finger-like infiltration into the surrounding mammary stroma, as studied by Kinkor et al[16]. Immunohistologically, tumor cells consistently express p63 and CK, but sometimes CK is focally expressed and rarely confined to obese spindle and epithelioid cells. Other antibodies ER, PgR and HER2 are generally negative, resembling normalised metaplastic carcinoma. As in our case, Rekhi et al[17], Nozoe et al[18], Rito et al[19] and others also found by immunohistochemical examination that FLMCa did not express estrogen receptors, progesterone receptors, and HER2 receptors, but mainly vimentin and basal cytokeratin. In addition, immunohistochemical expression of AE1/3 and CAM5.2 was also observed, and positive expression of epithelial and mesenchymal markers in these cells may be considered indicative of the "epithelial-mesenchymal" transformation observed in these tumors.
In the differential diagnosis, the diagnoses considered were nodular fasciitis, inflammatory myofibroblastic tumor, pseudoangiomatous stromal hyperplasia (PASH), myoblastoma, low-grade fibrosarcoma, and of course fibromatosis, which are very difficult to differentiate[20]. However, the development of immunohistochemistry has led to a better understanding of this histological type and allows for a better differential diagnosis. In our pathological examination, due to the lack of significant lymphoplasmacytic infiltration and myxoid background, we excluded nodular fasciitis and inflammatory myofibroblastic tumors[21,22]. Furthermore, PASH is less likely to be diagnosed because there is no slit-like space lined by fibroblasts[23]. Finally, there is a lack of fascicular arrangement and single row fibroblasts, which help to exclude fibrosarcomas and pleomorphic sarcomas[9].
In conclusion, due to the small number of previously reported cases, morphological features often do not reflect the nature of the lesion, and its lack of understanding is often misdiagnosed as proliferative breast lesions or low-grade soft tissue tumors, which may make the diagnosis and surgical treatment challenging. Given the small amount of published data, each reported clinical case may be important to improve the understanding of the argument. We therefore describe in detail the clinical, diagnostic, histopathological and therapeutic information observed in patients and compare it with information obtained from literature reviews. It was found that immunohistochemical analysis may be helpful in the diagnosis. Because local recurrence rates are high and can only be detected by resection, understanding the role of surgical margins in reducing or eliminating local recurrence is particularly important to assign appropriate strategies for assessing early detection of local recurrence or distant metastasis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gilmore N, United States; Janelsins M, United States S-Editor: Gong ZM L-Editor: Filipodia P-Editor: Zhang XD
| 1. | McKinnon E, Xiao P. Metaplastic carcinoma of the breast. Arch Pathol Lab Med. 2015;139:819-822. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 45] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 2. | Surenkok S, Tahberer E, Cinkaya A, Kodaz H, Deger A. Metaplastic breast cancer: A case report. J Pak Med Assoc. 2018;68:466-468. [PubMed] |
| 3. | Takatsuka D, Ogura H, Asano Y, Nakamura A, Koizumi K, Shiiya N, Baba S. A difficult-to-diagnose fibromatosis-like metaplastic carcinoma of the breast: a case report. Surg Case Rep. 2021;7:16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Victoor J, Bourgain C, Vander Borght S, Vanden Bempt I, De Rop C, Floris G. Fibromatosis-like metaplastic carcinoma: a case report and review of the literature. Diagn Pathol. 2020;15:20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 5. | Zhou X, Wu X, Wang L, Guo J, Wu Q, Song W, Zhao Y, Feng Z, Wu S, Zhang L, Gong X. Metaplastic breast carcinoma: a retrospective study of 26 cases. Int J Clin Exp Pathol. 2021;14:355-362. [PubMed] |
| 6. | Zhao Y, Gong X, Li N, Zhu B, Yu D, Jin X. Fibromatosis-like metaplastic carcinoma of breast: a challenge for clinicopathologic diagnosis. Int J Clin Exp Pathol. 2018;11:3691-3696. [PubMed] |
| 7. | Gobbi H, Simpson JF, Borowsky A, Jensen RA, Page DL. Metaplastic breast tumors with a dominant fibromatosis-like phenotype have a high risk of local recurrence. Cancer. 1999;85:2170-2182. [PubMed] [DOI] [Full Text] |
| 8. | Rakha EA, Brogi E, Castellano I, Quinn C. Spindle cell lesions of the breast: a diagnostic approach. Virchows Arch. 2022;480:127-145. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 9. | Dwyer JB, Clark BZ. Low-grade fibromatosis-like spindle cell carcinoma of the breast. Arch Pathol Lab Med. 2015;139:552-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 10. | Nonnis R, Paliogiannis P, Giangrande D, Marras V, Trignano M. Low-grade fibromatosis-like spindle cell metaplastic carcinoma of the breast: a case report and literature review. Clin Breast Cancer. 2012;12:147-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Tang F, Gu DH, Bao Y, Wang H, Zhu HG, Xu ZD, Hu XQ. [Low-grade (fibromatosis-like) spindle cell carcinoma of the breast: case report and review of the literature]. Zhonghua Bing Li Xue Za Zhi. 2005;34:444-445. [PubMed] |
| 12. | Nahleh Z, Ebrahim V, Guerrero R, Gaur S, Ayyappan A, Padilla O. Spindle cell carcinoma of the breast: a case report and discussion. Breast Dis. 2011;33:115-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Takano EA, Hunter SM, Campbell IG, Fox SB. Low-grade fibromatosis-like spindle cell carcinomas of the breast are molecularly exiguous. J Clin Pathol. 2015;68:362-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Sneige N, Yaziji H, Mandavilli SR, Perez ER, Ordonez NG, Gown AM, Ayala A. Low-grade (fibromatosis-like) spindle cell carcinoma of the breast. Am J Surg Pathol. 2001;25:1009-1016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 102] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 15. | Podetta M, D'Ambrosio G, Ferrari A, Sgarella A, Dal Bello B, Fossati GS, Zonta S, Silini E, Dionigi P. Low-grade fibromatosis-like spindle cell metaplastic carcinoma: a basal-like tumor with a favorable clinical outcome. Report of two cases. Tumori. 2009;95:264-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Kinkor Z, Svitáková I, Ryska A, Kodet R, Hrabal P. [Metaplastic spindle-cell (fibromatosis-like) carcinoma of the breast--report of 4 cases]. Cesk Patol. 2002;38:164-168. [PubMed] |
| 17. | Rekhi B, Shet TM, Badwe RA, Chinoy RF. Fibromatosis-like carcinoma-an unusual phenotype of a metaplastic breast tumor associated with a micropapilloma. World J Surg Oncol. 2007;5:24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Nozoe E, Nozoe T, Tanaka J, Ohga T, Fujita A, Sueishi K. Spindle cell carcinoma of the breast - A case report. J Med Invest. 2020;67:365-367. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 19. | Rito M, Schmitt F, Pinto AE, André S. Fibromatosis-like metaplastic carcinoma of the breast has a claudin-low immunohistochemical phenotype. Virchows Arch. 2014;465:185-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Dunne B, Lee AH, Pinder SE, Bell JA, Ellis IO. An immunohistochemical study of metaplastic spindle cell carcinoma, phyllodes tumor and fibromatosis of the breast. Hum Pathol. 2003;34:1009-1015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 106] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 21. | Lin W, Bao L. Nodular fasciitis of the breast: the report of three cases. BMC Womens Health. 2022;22:54. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 22. | Coffin CM, Dehner LP, Meis-Kindblom JM. Inflammatory myofibroblastic tumor, inflammatory fibrosarcoma, and related lesions: an historical review with differential diagnostic considerations. Semin Diagn Pathol. 1998;15:102-110. [PubMed] |