Published online Jun 26, 2023. doi: 10.12998/wjcc.v11.i18.4313
Peer-review started: February 11, 2023
First decision: March 24, 2023
Revised: April 3, 2023
Accepted: May 16, 2023
Article in press: May 16, 2023
Published online: June 26, 2023
Processing time: 135 Days and 9.2 Hours
Among the various types of aortic dissection, multichanneled aortic dissection (MCAD) differs from classic double-channeled aortic dissection and involves the formation of an additional false lumen in the aortic wall or the flaps. It is considered a relatively rare condition with high perioperative mortality and morbidity. However, the morphological characteristic and the optimal therapeutic strategy for MCAD has not been fully determined.
A 64-year-old man presented to our hospital with severe epigastric abdominal pain radiating to the back that was associated with nausea without emesis. A computed tomography angiogram was performed that revealed a type B aortic dissection with multiple channels extending from the level of the left subclavian artery to the bilateral femoral arteries. We used a medical three-dimensional modeling (3D) modeling system to identify the location and extension of multiple lumens from different angles. It also precisely located the two primary entries leading to the false lumens, which helped us to exclude the two false lumens with one stent-graft.
By applying medical 3D modeling system, we discover the fragility of aortic wall and the collapse of true lumen caused by the multiple false lumens are the two morphological features of MCAD.
Core Tip: Multichanneled aortic dissection usually causes the formation of more than two false lumens in the aortic wall. We used medical three-dimensional modeling (3D) modeling system preoperatively to help identify the location and extension of multiple lumens from different angles. It also precisely located the two primary entries leading to the false lumens, which helped us to exclude the two false lumens with one stent-graft. The 3D modeling system has a potential new role in clinical assessment and operative project planning for complicated aortic dissection.
- Citation: Lu WF, Chen G, Wang LX. Morphological features and endovascular repair for type B multichanneled aortic dissection: A case report. World J Clin Cases 2023; 11(18): 4313-4317
- URL: https://www.wjgnet.com/2307-8960/full/v11/i18/4313.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i18.4313
Among the various types of aortic dissection, multichanneled aortic dissection (MCAD) differs from classic double-channeled aortic dissection and involves the formation of an additional false lumen in the aortic wall or the flaps. It is considered a relatively rare condition with high perioperative mortality and morbidity[1]. However, the morphological characteristic and the optimal therapeutic strategy for MCAD has not been fully determined.
Severe epigastric abdominal pain radiating to the back for 1 wk.
A 64-year-old man presented to our hospital with severe epigastric abdominal pain radiating to the back that was associated with nausea without emesis for 1 wk.
Hypertension and stroke.
Hypertension.
A physical examination revealed significant tenderness in the abdomen and a palpable pulse throughout his distal extremities.
Normal.
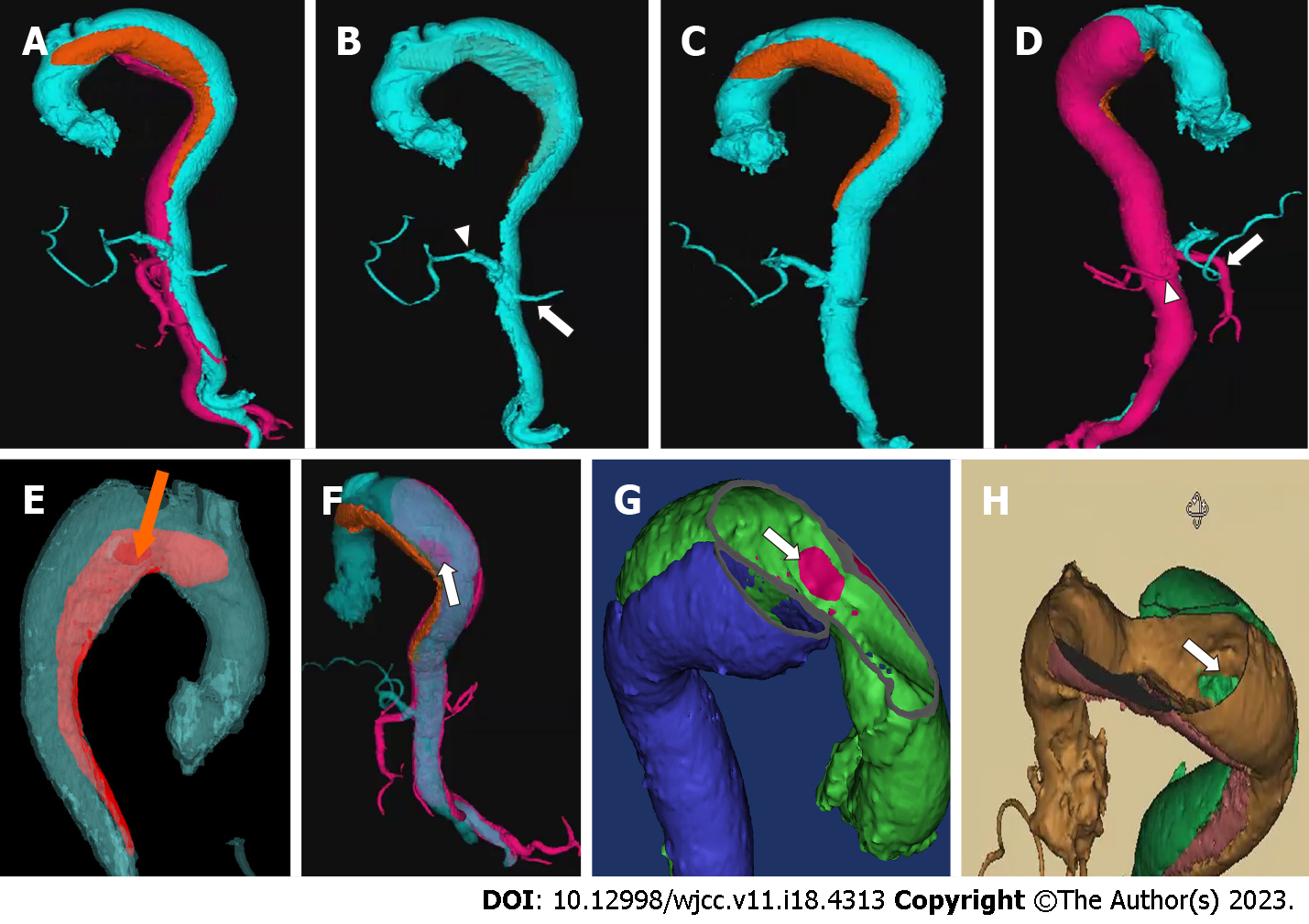
A computed tomography (CT) angiogram was performed that revealed a type B aortic dissection with multiple channels extending from the level of the left subclavian artery to the bilateral femoral arteries. To identify the specific location of entry tears and the origin of abdominal branches, we used a medical three-dimensional (3D) modeling system to reconstruct and create an omnidirectional image by analyzing and integrating CT angiographic images. It confirmed a typical three-channeled aortic dissection, and the location of the primary entry tears of two different false lumens could be clearly recognized. The superior mesentery artery and the right renal artery originated from one of the false lumens (Figure 1 and Video), which suggested the complexity and potential risk of organ malperfusion of the MCAD.
Type B aortic dissection.
Because this patient was resistant to open chest and abdominal surgery, we performed thoracic endovascular aortic repair (TEVAR) with a debranching technique. We made a longitudinal incision on both sides of the neck to expose the left and right common carotid artery, then the end-to-side anastomosis was made from the artificial graft to the left common carotid artery. After the graft was tunneled from the left side to the right side, the end-to-side anastomosis was performed on the right common carotid artery. Then we made a left carotid to left subclavian artery bypass. After successful anastomosis, the left common carotid artery was ligated and TEVAR was performed with the help of an intravascular ultrasound to guide the wire through the true lumen from the right femoral artery to the aortic arch. Then the stent-graft (Zenith Alpha Thoracic Endograft, Cook Medical, Bloomington, IN) was precisely deployed within the aortic arch just adjacent to the innominate artery distally. The complete angiograph showed that the primary entries of both two false lumens were sealed without type I endoleaks (Figure 2), and the true lumen was enlarged with good blood flow perfusion to visceral organs.
After the operation, the patient had a thoracic duct injury with increased drainage from the incision, which was managed with percutaneous coil embolization. He was discharged one week later after a successful recovery.
MCAD was first reported in 1978 by McReynolds et al[1]. The incidence of MCAD ranges from 4.9% to 9% with higher observed rates in patients with Marfan syndrome[2-4]. Due to the difference and complexity of its flow patterns and hemodynamics, conventional CT imaging has difficulty in clearly depicting the morphological configuration of MCAD. An important morphological feature of MCAD, as shown in our case by the medical 3D modeling system, is a relatively greater risk of collapse of true lumen compressed by the false lumens on both sides. This morphology may often cause a potential risk of organ malperfusion. Another important feature is the fragility of the aortic wall when the second false lumen develops laterally on the wall of the first false lumen in the acute dissection. The false lumens usually have no re-entry formation which increases the pressure in the false lumens and causes rupture[3].
Due to its hemodynamic instability and potential risk of organ malperfusion, early surgical or endovascular intervention such as TEVAR is recommended[3]. However, the relevant literature is limited. Generally, for debranching technique, if the aortic dissection involves the innominate artery, graft from the ascending aorta to the neck vessels is performed. In our case, the innominate artery was not involved by the aortic dissection, so we performed the right common carotid - left common carotid artery bypass and left carotid to left subclavian artery bypass before TEVAR procedure. During the TEVAR procedure of MCAD, it is challenging to identify the configuration of multiple lumens and their relationship with aortic branches. Preoperative evaluation is crucial to the success of TEVAR. In our case, a medical 3D modeling system was used preoperatively to help identify the location and extension of multiple lumens from different angles. It also precisely located the two primary entries leading to the false lumens, which helped us to exclude the two false lumens with one stent-graft. Additionally, an intravascular ultrasound was also used to guide the wire and assure the precise deployment of the stent graft within the true lumen. Our results showed that the MCAD with complex configuration could be managed with endovascular repair with the help of 3D modeling system and intravascular ultrasound.
The fragility of the aortic wall and the collapse of the true lumen caused by the multiple false lumens are the two morphological features of MCAD. Notably a 3D modeling system has a potential new role in clinical assessment and operative project planning for complicated aortic dissection such as MCAD. More in-depth studies are required.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Schoenhagen P, United States; Shuhaiber JH, United States S-Editor: Li L L-Editor: A P-Editor: Li L
| 1. | McReynolds RA, Shin MS, Sims RD. Three-channeled aortic dissection. AJR Am J Roentgenol. 1978;130:549-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Sueyoshi E, Nagayama H, Hayashida T, Sakamoto I, Uetani M. Comparison of outcome in aortic dissection with single false lumen vs multiple false lumens: CT assessment. Radiology. 2013;267:368-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Ando M, Okita Y, Tagusari O, Kitamura S, Matsuo H. Surgery in three-channeled aortic dissection. A 31-patient review. Jpn J Thorac Cardiovasc Surg. 2000;48:339-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Guo B, Hou K, Guo D, Xu X, Shi Z, Shan Y, Lv P, Fu W. Outcomes of thoracic endovascular repair for type B aortic dissection with multichanneled morphology. J Vasc Surg. 2017;66:1007-1017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |