Published online Jun 26, 2023. doi: 10.12998/wjcc.v11.i18.4267
Peer-review started: April 11, 2023
First decision: April 26, 2023
Revised: May 4, 2023
Accepted: May 19, 2023
Article in press: May 19, 2023
Published online: June 26, 2023
Processing time: 76 Days and 19.6 Hours
Attention-deficit/hyperactivity disorder (ADHD) is one of the most common disorders in child and adolescent psychiatry, with a prevalence of more than 5%. Despite extensive research on ADHD in the last 10 to 20 years, effective treat-ments are still lacking. Instead, the concept of ADHD seems to have become broader and more heterogeneous. Therefore, the diagnosis and treatment of ADHD remains challenging for clinicians.
To investigate the effects of a multimodal integrated intervention for children with ADHD.
Between March 2019 and September 2020, a total of 100 children with ADHD who were diagnosed and treated at our hospital were assessed for eligibility, two of whom revoked their consent. A case-control study was conducted in which the children were equally assigned, using a randomized number table, to either a medication group (methylphenidate hydrochloride extended-release tablets and atomoxetine hydrochloride tablets) or a multimodal integrated intervention group (medication + parent training + behavior modification + sensory integration therapy + sand tray therapy), with 49 patients in each group. The clinical endpoint was the efficacy of the different intervention modalities.
The two groups of children with ADHD had comparable patient characteristics (P > 0.05). Multimodal integrated intervention resulted in a significantly higher treatment efficacy (91.84%) than medication alone (75.51%) (P < 0.05). Children who received the multimodal integrated intervention showed lower scores in the Conners Parent Symptom Questionnaire and the Weiss Functional Impairment Rating Scale than those treated with medication alone (P < 0.05). The Sensory Integration Scale scores of children in the multimodal integrated intervention group were higher than those of children in the medication group (P < 0.05). Children who received the multimodal integrated intervention had higher compliance and family satisfaction and a lower incidence of adverse events than those treated with medication alone (P < 0.05).
Multimodal integrated intervention effectively alleviated symptoms associated with ADHD in children. It enhanced their memory and attention with high safety and parental satisfaction, demonstrating good potential for clinical promotion.
Core Tip: Multimodal integrated intervention, including medication, parent training, behavior modification, sensory integration therapy, and sand tray therapy, has been shown to effectively alleviate symptoms of attention-deficit/hyperactivity disorder (ADHD) in children. This intervention resulted in higher treatment efficacy compared to medication alone, with lower scores in symptom questionnaires and functional impairment scales. Children who received this approach also had higher compliance and family satisfaction and a lower incidence of adverse events. Such a multimodal integrated intervention shows promising potential for clinical promotion in ADHD treatment.
- Citation: Lv YB, Cheng W, Wang MH, Wang XM, Hu YL, Lv LQ. Multimodal integrated intervention for children with attention-deficit/hyperactivity disorder. World J Clin Cases 2023; 11(18): 4267-4276
- URL: https://www.wjgnet.com/2307-8960/full/v11/i18/4267.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i18.4267
Attention-deficit/hyperactivity disorder (ADHD) is the most common neurobehavioral disorder in children, with a prevalence of 7%-9% among children aged < 14 years[1]. It is characterized by inattention, hyperactivity, and impulsive behavior. Although most children with ADHD have normal intelligence, their learning performance, well-being, and social interactions can be compromised to varying degrees[2,3]. Relevant epidemiological data show that the global prevalence of ADHD has remained stable over the past 3 years, and a related meta-analysis revealed that the prevalence of ADHD in children in China is 5.7%, with approximately twice the prevalence in boys than in girls[4]. Clinical treatment of ADHD aims to alleviate symptoms and reduce behavioral issues, with pharmacological and non-pharmacological interventions being the main treatment options[5]. The American Academy of Child and Adolescent Psychiatry guidelines suggest that pharmacological interventions are more effective than behavioral treatments, whereas the American Academy of Pediatrics recommends behavioral interventions, especially for preschool children. Despite the slightly stronger evidence for pharmacotherapy than for non-pharmacotherapy, recent guidelines for the diagnosis and treatment of ADHD in China have reinforced the recommendation for a multimodal approach, supporting attempts to combine pharmacological, behavioral, psychotherapeutic, and medical-educational approaches, with greater emphasis on the use of behavioral interventions, especially before the age of 12 years[6].
However, in multimodal approaches, the balance of weights between pharmacological and non-pharmacological therapeutic interventions varies, and the optimal treatment effect relies on the coordination of different intervention options. Their effectiveness for behavioral interventions in preschool children merits further investigation[7]. Owing to the paucity of national studies on multimodal approaches for the treatment of ADHD in China, the present study was undertaken to investigate the effects of a multimodal integrated intervention for children with ADHD.
Between March 2019 and September 2020, a total of 100 children with ADHD who were diagnosed and treated at our hospital were assessed for eligibility and recruited for this study. Two patients revoked their consent, and 98 children were finally included. A case-control study was conducted in which the children were equally assigned, using a randomized number table, to either a medication group (methylphenidate hydrochloride extended-release tablets and atomoxetine hydrochloride tablets) or a multimodal integrated intervention group (medication + parent training + behavior modification + sensory integration therapy + sand tray therapy), with 49 patients in each group. The family members of the children signed the informed consent form before treatment. The ethics committee of Ningbo Women & Children’s Hospital approved this study.
Inclusion criteria: Children who met the diagnostic criteria established by the Diagnostic and Statistical Manual of Mental Disorders 5th edition, were of Han ethnicity, were < 14 years old, were not using other psychiatric drugs such as methylphenidate (Ritalin) within 1 wk before enrollment, and had no allergic reactions to the study-related drugs or had no history of allergy were included.
Exclusion criteria: Children with mental retardation, conduct disorders, mood disorders, tic disorders, childhood autism, schizophrenia, severe liver and kidney abnormalities, a history of acute and chronic somatic infections, or global developmental disorders were excluded.
The children received methylphenidate hydrochloride extended-release tablets and atomoxetine hydrochloride tablets, which were administered as a single dose each morning before and after meals, depending on the severity of their attention deficit[8,9].
(1) Medication: The medication regimen was the same as that in the medication group; (2) Parent training: Parent training, which included disease awareness, advantages and disadvantages of medications, parent-child relationship, and improving attention in children, was conducted for a total of four sessions; (3) Behavior modification: Behavior modification included positive reinforcement, temporary isolation, abatement, demonstration, cognitive behavioral therapy, and applied behavioral analysis; (4) Sensory integration: Sensory integration training consisted of seven activities, namely, warming up (singing nursery songs, story reading), vestibular sensory training (spinning, moving, scooting, going over obstacles), proprioception training (holding, lifting, pushing, pulling heavy objects), balance training (crossing a balance beam, walking along a hula hoop, playing single-legged games, balancing on a balance board), hand-eye coordination training (throwing balloons, throwing sandbags, hitting target objects, throwing things to partners), relaxation training (partaking in relaxation activities, singing simple children’s songs, playing finger rhymes, storytelling), and fine motor training (making snacks, cutting and pasting, partaking in art activities, coloring)[10]. Each session lasted for 45-60 min, for a total treatment duration of 3-6 mo depending on the child’s condition; (5) Sand tray game: The course was conducted by a sand tray therapist on a one-to-one basis, and the process included guidance provision, familiarization with the environment, feeling the sand, making the sand tray, experiencing the work, dialogue and communication, dismantling the work, and discussion and analysis with the parents. The game required approximately 40-60 min for each session, with a total of 10-12 sessions; and (6) Appointment system: An appointment system was established to ensure timely appointment for children with ADHD. A personal file was established for each child to ensure good follow-up compliance.
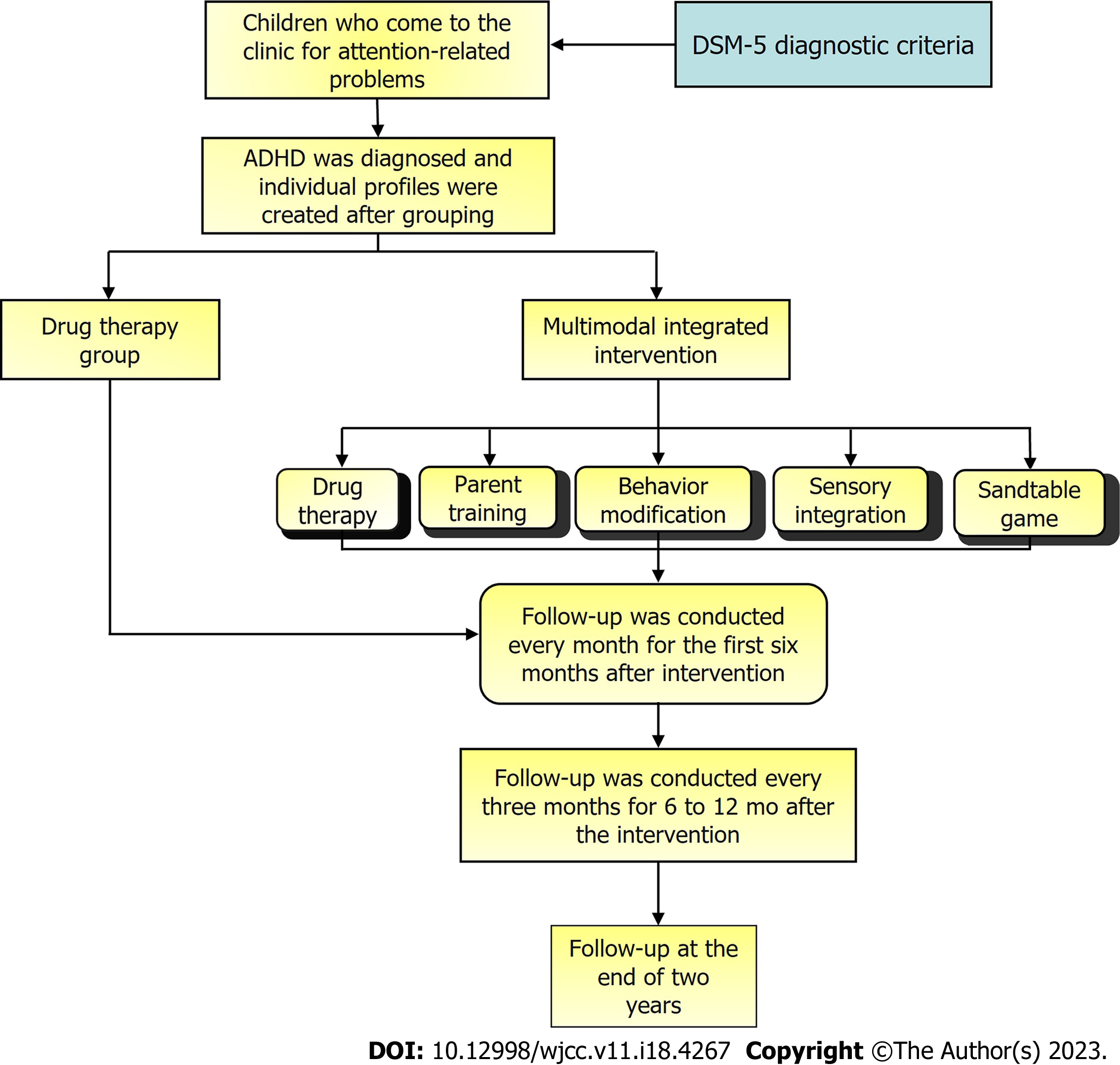
The research route is shown in Figure 1.
Every year, our department sees approximately 500 children with various psychological problems, including approximately 300 children with ADHD. The sensory integration therapists, rehabilitation therapists, and sand tray therapy consultants in our department are professionally trained and qualified. To date, parent training and behavior modification have been conducted for > 1 year with > 200 participants. Active classes on Triple P parenting have been conducted for more than half a year. The department has conducted > 100 sessions of sensory integration training and nearly 90 sessions of sand tray therapy and has achieved certain expected results. Our department has also conducted or participated in research on related topics. In addition, we have established different clinics for child psychological counseling, child language intervention, high-risk child follow-up, child rehabilitation, child eugenics counseling, and child nutrition counseling. All these clinics are manned by doctors with senior titles, rich clinical experience, and strong teaching and clinical guidance abilities.
Clinical efficacy was divided into four levels: clinical control [≥ 90% decrease in the Swanson, Nolan, and Pelham, version IV (SNAP-IV) scores after treatment; recovery of normal adaptive and social functioning; significantly improved academic performance; hyperactivity index < 1.1], markedly effective (≥ 60% decrease in the SNAP-IV scores after treatment, near-normal recovery of adaptive and social functioning, improved academic performance, and hyperactivity index < 1.5), effective (≥ 35% decrease in the SNAP-IV scores after treatment; improved, but not stable, adaptive and social functioning and academic performance; decreased hyperactivity index but still > 1.5), and ineffective (the above criteria were not met). Total efficacy was calculated as follows: (number of clinical control cases + number of markedly effective cases + number of effective cases)/total number of cases.
The Conners Parent Symptom Questionnaire (PSQ) and Weiss Functional Impairment Rating Scale (WFIRS) were used for evaluation. The PSQ scale includes six factors: character problems, learning problems, psychosomatic problems, impulsivity-hyperactivity, anxiety, and hyperactivity index. The higher the score, the more severe the problem. The WFIRS includes six items rated on a scale of 0-4: family, learning/school, life skills, self-concept, social activities, and adventure activities. The lower the score, the better the social functioning.
The scale consists of 58 questions, each rated on a five-point scale with a maximum score of 5 and a minimum score of 1. It includes four items: vestibular balance, tactile defense, proprioceptive function, and learning ability.
Child compliance, family satisfaction, and the incidence of adverse events were recorded and compared between the groups.
SPSS software (version 26.0) was used to organize and statistically analyze the data. Measurement data were expressed as mean ± SD and analyzed using the t-test. Count data were expressed as number and percentage and were analyzed using the χ2 test. Statistical significance was set at P < 0.05.
Patients in the medication group were aged 6-14 (9.21 ± 1.69) years. The group included 36 boys and 13 girls with a disease duration of 11-37 (23.68 ± 1.84) months and a Wechsler IQ score of ≥ 85 (92.11 ± 2.74). Of these patients, 27 had either the inattentive or hyperactive-impulsive type of ADHD and 22 had mixed-type ADHD. Meanwhile, patients in the multimodal integrated intervention group were aged 6-14 (9.08 ± 1.88) years. The group included 38 boys and 11 girls with a disease duration of 11-38 (24.01 ± 1.59) months and a Wechsler IQ score of ≥ 85 (92.23 ± 2.69). Of these patients, 31 had inattentive or hyperactive-impulsive ADHD, and 18 had mixed ADHD. The patient characteristics were comparable between the two groups (P < 0.05) (Table 1).
| Medication group (n = 49) | Multimodal integrated intervention group (n = 49) | t value | P value | ||
| Age (yr) | Range | 6-14 | 6-14 | - | - |
| mean | 9.21 ± 1.69 | 9.08 ± 1.88 | 0.360 | 0.720 | |
| Sex | Male | 36 | 38 | - | - |
| Female | 13 | 11 | - | - | |
| Duration of disease (mo) | Range | 11-37 | 11-38 | - | - |
| mean | 23.68 ± 1.84 | 24.01 ± 1.59 | 0.950 | 0.344 | |
| Wechsler intelligence score (points) | Range | ≥ 85 | ≥ 85 | - | - |
| mean | 92.11 ± 2.74 | 92.23 ± 2.69 | 0.219 | 0.827 | |
| ADHD subtype | Dispersion | 27 | 31 | - | - |
| Mixed | 22 | 18 | - | - | |
| Place of residence | Local | 37 | 39 | - | - |
| Non-local | 12 | 10 | - | - | |
In the medication group, clinical efficacy was judged as follows: clinical control in 19 cases, markedly effective in 10 cases, effective in 8 cases, and ineffective in 12 cases. In the multimodal integrated intervention group, clinical efficacy was judged as follows: clinical control in 26 cases, markedly effective in 13 cases, effective in 6 cases, and ineffective in 4 cases. Multimodal integrated intervention resulted in a significantly higher treatment efficacy (91.84%) than medication alone (75.51%) (P < 0.05) (Table 2).
| Group | n | Clinical control | Markedly effective | Effective | Ineffective | Total efficacy |
| Medication | 49 | 19 (38.78) | 10 (20.41) | 8 (16.33) | 12 (24.50) | 37 (75.51) |
| Multimodal integrated intervention | 49 | 26 (53.06) | 13 (26.53) | 6 (12.24) | 4 (8.17) | 45 (91.84) |
| χ2 value | - | - | - | - | - | 7.127 |
| P value | - | - | - | - | - | 0.008 |
In the medication group, the scores for the six factors in the PSQ scale were 0.69 ± 0.18, 0.94 ± 0.33, 3.45 ± 1.05, 1.11 ± 0.53, 2.03 ± 1.23, and 0.98 ± 0.32, and the scores for the six items in the WFIRS were 0.59 ± 0.48, 0.63 ± 0.48, 0.92 ± 0.42, 0.94 ± 0.65, 0.52 ± 0.49, and 0.29 ± 0.20. In the multimodal integrated intervention group, the PSQ scale scores were 0.58 ± 0.06, 0.73 ± 0.11, 2.87 ± 0.77, 0.85 ± 0.12, 1.23 ± 0.59, and 0.68 ± 0.32, and the WFIRS scores were 0.39 ± 0.23, 0.35 ± 0.24, 0.65 ± 0.24, 0.68 ± 0.31, 0.30 ± 0.18, and 0.18 ± 0.11. The PSQ and WFIRS scores of the multimodal integrated intervention group were significantly lower than those of the medication group, suggesting that children who received the multimodal integrated intervention had better outcomes (P < 0.05) (Table 3).
| Medication group (n = 49) | Multimodal integrated intervention group (n = 49) | t value | P value | ||
| PSQ | Character problems | 0.69 ± 0.18 | 0.58 ± 0.06 | 4.058 | < 0.001 |
| Learning problems | 0.94 ± 0.33 | 0.73 ± 0.11 | 4.226 | < 0.001 | |
| Psychosomatic problems | 3.45 ± 1.05 | 2.87 ± 0.77 | 3.118 | 0.002 | |
| Impulsivity-hyperactivity | 1.11 ± 0.53 | 0.85 ± 0.12 | 3.349 | 0.001 | |
| Anxiety | 2.03 ± 1.23 | 1.23 ± 0.59 | 4.105 | < 0.001 | |
| Hyperactivity index | 0.98 ± 0.32 | 0.68 ± 0.32 | 4.640 | < 0.001 | |
| WFIRS | Family | 0.59 ± 0.48 | 0.39 ± 0.23 | 2.630 | 0.010 |
| Learning/school | 0.63 ± 0.48 | 0.35 ± 0.24 | 3.652 | < 0.001 | |
| Life skills | 0.92 ± 0.42 | 0.65 ± 0.24 | 3.907 | < 0.001 | |
| Self-concept | 0.94 ± 0.65 | 0.68 ± 0.31 | 2.527 | 0.013 | |
| Social activities | 0.52 ± 0.49 | 0.30 ± 0.18 | 2.950 | 0.004 | |
| Adventure activities | 0.29 ± 0.20 | 0.18 ± 0.11 | 3.373 | 0.001 | |
Before the intervention, the Sensory Integration Scale scores did not significantly differ between the two groups (P > 0.05). After the intervention, the medication group had a vestibular balance score of 32.56 ± 4.15 points, tactile defense score of 33.86 ± 4.12 points, proprioceptive function score of 31.37 ± 3.95 points, and learning ability score of 26.94 ± 2.84 points. The multimodal integrated intervention group had a vestibular balance score of 39.88 ± 3.95 points, tactile defense score of 38.85 ± 4.23 points, proprioceptive function score of 35.75 ± 4.02 points, and learning ability score of 30.15 ± 2.58 points. The Sensory Integration Scale scores of children in the multimodal integrated intervention group were higher than those of children in the medication group (P < 0.05) (Table 4).
| Medication group (n = 49) | Multimodal integrated intervention group (n = 49) | t value | P value | ||
| Before the intervention | Vestibular balance | 23.56 ± 3.15 | 23.69 ± 3.14 | 0.205 | 0.838 |
| Tactile defense | 29.95 ± 3.45 | 29.87 ± 3.56 | 0.113 | 0.910 | |
| Proprioceptive function | 29.08 ± 3.14 | 28.94 ± 3.35 | 0.213 | 0.832 | |
| Learning ability | 22.91 ± 4.02 | 22.77 ± 3.85 | 0.176 | 0.861 | |
| After the intervention | Vestibular balance | 32.56 ± 4.15 | 39.88 ± 3.95 | 8.943 | < 0.001 |
| Tactile defense | 33.86 ± 4.12 | 38.85 ± 4.23 | 5.915 | < 0.001 | |
| Proprioceptive function | 31.37 ± 3.95 | 35.75 ± 4.02 | 5.440 | < 0.001 | |
| Learning ability | 26.94 ± 2.84 | 30.15 ± 2.58 | 5.856 | < 0.001 | |
The medication group had a compliance rate of 79.49%, family satisfaction rate of 71.43%, and an incidence of adverse events of 16.33%. The multimodal integrated intervention group had a compliance rate of 95.92%, family satisfaction rate of 97.96%, and an incidence of adverse events of 2.04%. Children who received the multimodal integrated intervention had higher compliance and family satisfaction and a lower incidence of adverse events than those treated with medication alone (P < 0.05) (Table 5).
| Group | n | Child compliance | Family satisfaction | Incidence of adverse events |
| Medication | 49 | 31 (79.49) | 35 (71.43) | 8 (16.33) |
| Multimodal integrated intervention | 49 | 47 (95.92) | 48 (97.96) | 1 (2.04) |
| χ2 value | - | 16.082 | 13.303 | 5.995 |
| P value | - | < 0.001 | < 0.001 | 0.014 |
The poor self-control of children with ADHD and the difficulty parents face in distinguishing between behavioral problems and symptoms of the disorder lead to intense parent-child conflicts[11]. Existing evidence suggests that ADHD in children is attributable to disruption of the metabolism of the central neurotransmitters dopamine and norepinephrine, resulting in mildly impaired brain function[12,13], and that improvements in the cognitive function of patients may alleviate psychiatric symptoms such as attention deficit, hyperactivity, and impulsivity[14].
In the present study, multimodal integrated interventions resulted in significantly higher treatment efficacy and C-factor scores than medication alone. Children who received the multimodal integrated intervention had lower PSQ and WFIRS scores than those treated with medication alone. Clinical studies suggest that, in addition to medication, long-term, individualized, and comprehensive treatment is required for patients with ADHD to alleviate symptoms, reduce comorbidities, and promote full recovery of social functioning. In this study, non-pharmacological treatments included parent training, behavior modification, sensory integration therapy, and sand tray therapy. Parent training is currently a common approach for the management of children with ADHD. Meanwhile, behavioral interventions for children with ADHD focus more on functional recovery than symptom mitigation. Previous studies have shown that correctional interventions are associated with a reduction in ADHD symptoms, which is consistent with the results of the current study. Moreover, the combination of medications provides a more pronounced effect and results in higher treatment compliance, leading to long-term alleviation of major ADHD symptoms. Some patients with ADHD experience perceptual problems and hand-eye coordination disorders. Sensorimotor training has been shown to alleviate hyperactivity, impulsivity, and attention deficits in patients with ADHD and to modulate sensory integration disorders[15]. It improves patients' visual acuity and proprioceptive and vestibular inputs through a series of targeted treatments, and oculomotor re-regulation and reintegration improve gaze stability, postural control, and balance owing to the reorganization of the brainstem and cerebellar pathways[16]. Moreover, the Sensory Integration Scale scores of children in the multimodal integrated intervention group were higher than those of children in the medication group, indicating that multimodal integrated interventions improve the spatial, motor, and visual perceptions; modulate the function of the ves-tibular system of the brain; and are safe, effective, and easy to implement in children. This helps alleviate anxiety and improves academic performance and efficiency[17], thereby increasing the persistence and stability of children’s attention, improving their auditory and visual attention levels, and mobilizing their motivation and initiative[18]. The brains of children are highly developmentally plastic[19], and behavioral therapy allows children with ADHD to adjust and control their behavioral patterns based on feedback from the external environment, facilitating coordination between different areas of the brain to generate new conditioned reflexes, improving the function of the prefrontal cortex and striatal norepinephrine pathways, and enhancing various aspects of cognitive function[20].
In addition, children who received the multimodal integrated intervention had higher compliance and family satisfaction and a lower incidence of adverse events than those treated with medication alone, suggesting that multimodal integrated interventions can restore learning ability, improve physical and mental health, facilitate family understanding of the disorder and its treatments, create a good atmosphere in the hospital, and avoid various emergency situations. Lv et al[21] used a non-pharmacological intervention for children with ADHD and observed positive effects on the cognitive function of children with different ADHD subtypes, similar to the findings of the present study.
This study had some limitations, including the small sample size and the lack of short-term follow-up. The setting of the treatment course and long-term efficacy in terms of cognitive function require further investigations to provide more reliable data.
Multimodal integrated intervention effectively alleviated the symptoms associated with ADHD in children. It enhanced their memory and attention with high safety and parental satisfaction, demonstrating good potential for clinical promotion.
In this study, the background discusses the prevalence of attention-deficit/hyperactivity disorder (ADHD) and the lack of effective treatments despite extensive research in the last decade or two. The concept of ADHD has also become broader and more heterogeneous, which adds to the challenge of diagnosis and treatment for clinicians. This sets the stage for the current research, which aims to investigate the effects of a multimodal integrated intervention for children with ADHD.
In this study, the motivation is to address the lack of effective treatments for ADHD despite extensive research and the broader and heterogeneous concept of ADHD that makes diagnosis and treatment challenging for clinicians. The study aims to investigate the effects of a multimodal integrated intervention that includes medication, parent training, behavior modification, sensory integration therapy, and sand tray therapy. The motivation behind the research is to find an effective intervention that can alleviate symptoms associated with ADHD in children and improve their memory and attention while ensuring high safety and parental satisfaction.
In this study, the primary objective is to investigate the effects of a multimodal integrated intervention on children with ADHD. More specifically, the study aims to compare the efficacy of a multidisciplinary intervention that includes medication, parent training, behavior modification, sensory integration therapy, and sand tray therapy vs medication alone in treating ADHD symptoms. The study also aims to assess and compare the compliance, family satisfaction, and incidence of adverse events between the two treatment groups. Ultimately, the research objectives are to identify an effective intervention to alleviate ADHD symptoms in children and improve their overall quality of life.
A total of 100 children with ADHD were assessed for eligibility, and 49 patients were assigned to each group using a randomized number table. The medication group received methylphenidate hydrochloride extended-release tablets and atomoxetine hydrochloride tablets, while the multimodal integrated intervention group received medication, parent training, behavior modification, sensory integration therapy, and sand tray therapy. The clinical endpoint was the efficacy of the different intervention modalities, which was evaluated through various measures such as symptom questionnaires, functional impairment scales, and sensory integration scales. Compliance, family satisfaction, and incidence of adverse events were also assessed.
The study found that the multimodal integrated intervention had a significantly higher treatment efficacy than medication alone in alleviating ADHD symptoms in children. The group receiving the integrated intervention also showed lower scores on symptom questionnaires and functional impairment scales, higher scores on sensory integration scales, higher compliance rates, and greater family satisfaction with fewer adverse events. These results indicate that a multidisciplinary approach to ADHD treatment can be more effective than medication alone, and that integrating parent training, behavior modification, sensory integration therapy, and sand tray therapy can enhance the treatment outcomes in children with ADHD, improving their memory and attention while ensuring high safety and parental satisfaction.
The study concludes that the multimodal integrated intervention, consisting of medication, parent training, behavior modification, sensory integration therapy, and sand tray therapy, is an effective treatment for children with ADHD. The research found a significantly higher treatment efficacy in the group receiving this multidisciplinary approach compared to the medication-alone group. The integrated intervention improved symptom relief, increased compliance rates, boosted family satisfaction, and resulted in fewer adverse events. This study supports the promotion of a comprehensive approach to treating ADHD, which can improve memory and attention, leading to better outcomes in children with the condition.
The study's findings suggest that a multimodal integrated intervention can significantly improve the treatment outcomes in children with ADHD. Further research is needed to explore the long-term effects of this intervention and its impact on cognitive and academic performance. Future studies can also examine the applicability of this approach to other populations or age groups. In addition, more research is necessary to determine the optimal combination of interventions, dosages, and duration of treatment. Finally, efforts should be made to disseminate the results of this study and promote the adoption of a comprehensive approach to treating ADHD in clinical practice.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, general and internal
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tsukasaki M, Japan; Zloto O, Israel S-Editor: Wang JL L-Editor: A P-Editor: Chen YX
| 1. | Sakakihara Y. More attention to ADHD. Dev Med Child Neurol. 2013;55:296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Panagiotidi M, Overton PG, Stafford T. The relationship between ADHD traits and sensory sensitivity in the general population. Compr Psychiatry. 2018;80:179-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 69] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 3. | Jensen PS, Mrazek D, Knapp PK, Steinberg L, Pfeffer C, Schowalter J, Shapiro T. Evolution and revolution in child psychiatry: ADHD as a disorder of adaptation. J Am Acad Child Adolesc Psychiatry. 1997;36:1672-9; discussion 1679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 124] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 4. | Schoenfelder EN, Kollins SH. Topical Review: ADHD and Health-Risk Behaviors: Toward Prevention and Health Promotion. J Pediatr Psychol. 2016;41:735-740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 42] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 5. | Kaisari P, Dourish CT, Higgs S. Attention Deficit Hyperactivity Disorder (ADHD) and disordered eating behaviour: A systematic review and a framework for future research. Clin Psychol Rev. 2017;53:109-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 80] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 6. | Terán Prieto A. [Attention-deficit/hyperactivity disorder and substance abuse. Scientific evidence]. Medicina (B Aires). 2020;80 Suppl 2:76-79. [PubMed] |
| 7. | Lange AM, Thomsen PH. [ADHD in preschoolers and early parent training interventions]. Ugeskr Laeger. 2019;181. [PubMed] |
| 8. | Smoot LC, Boothby LA, Gillett RC. Clinical assessment and treatment of ADHD in children. Int J Clin Pract. 2007;61:1730-1738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Leblanc N. [Attention deficit hyperactivity disorder (ADHD) in preschoolers: nature, assessment and treatment]. Sante Ment Que. 2009;34:199-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 10. | Coelho L, Chaves E, Vasconcelos S, Fonteles M, De Sousa F, Viana G. [Attention deficit hyperactivity disorder (ADHD) in children: neurobiological aspects, diagnosis and therapeutic approach]. Acta Med Port. 2010;23:689-696. [PubMed] |
| 11. | Giupponi G, Giordano G, Maniscalco I, Erbuto D, Berardelli I, Conca A, Lester D, Girardi P, Pompili M. Suicide risk in attention-deficit/hyperactivity disorder. Psychiatr Danub. 2018;30:2-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 12. | Hilger K, Sassenhagen J, Kühnhausen J, Reuter M, Schwarz U, Gawrilow C, Fiebach CJ. Neurophysiological markers of ADHD symptoms in typically-developing children. Sci Rep. 2020;10:22460. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Banaschewski T, Hollis C, Oosterlaan J, Roeyers H, Rubia K, Willcutt E, Taylor E. Towards an understanding of unique and shared pathways in the psychopathophysiology of ADHD. Dev Sci. 2005;8:132-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 87] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 14. | Salomonsson B. Interpreting the inner world of ADHD children: psychoanalytic perspectives. Int J Qual Stud Health Well-being. 2017;12:1298269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Høvik MF, Plessen KJ. [Emotional regulation and motivation in children with ADHD]. Tidsskr Nor Laegeforen. 2010;130:2349-2352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Konrad K, Eickhoff SB. Is the ADHD brain wired differently? A review on structural and functional connectivity in attention deficit hyperactivity disorder. Hum Brain Mapp. 2010;31:904-916. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 530] [Cited by in RCA: 452] [Article Influence: 30.1] [Reference Citation Analysis (0)] |
| 17. | Benzing V, Schmidt M. Cognitively and physically demanding exergaming to improve executive functions of children with attention deficit hyperactivity disorder: a randomised clinical trial. BMC Pediatr. 2017;17:8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Cordier R, Vilaysack B, Doma K, Wilkes-Gillan S, Speyer R. Peer Inclusion in Interventions for Children with ADHD: A Systematic Review and Meta-Analysis. Biomed Res Int. 2018;2018:7693479. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 19. | Shaw M, Hodgkins P, Caci H, Young S, Kahle J, Woods AG, Arnold LE. A systematic review and analysis of long-term outcomes in attention deficit hyperactivity disorder: effects of treatment and non-treatment. BMC Med. 2012;10:99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 533] [Cited by in RCA: 460] [Article Influence: 35.4] [Reference Citation Analysis (0)] |
| 20. | Song M, Lauseng D, Lee S, Nordstrom M, Katch V. Enhanced Physical Activity Improves Selected Outcomes in Children With ADHD: Systematic Review. West J Nurs Res. 2016;38:1155-1184. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Lv YB, Cheng W, Wang MH, Wang XM, Hu YL, Lv LQ. Effect of non-pharmacological treatment on the full recovery of social functioning in patients with attention deficit hyperactivity disorder. World J Clin Cases. 2023;11:3238-3247. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 1] [Article Influence: 0.5] [Reference Citation Analysis (5)] |