Published online Jun 6, 2023. doi: 10.12998/wjcc.v11.i16.3885
Peer-review started: March 7, 2023
First decision: March 24, 2023
Revised: March 27, 2023
Accepted: April 24, 2023
Article in press: April 24, 2023
Published online: June 6, 2023
Processing time: 87 Days and 5.5 Hours
Traumatic pancreatic injury is relatively rare in children, accounting for approximately 3%-12% of blunt abdominal trauma cases. Most traumatic pancreatic injuries in boys are related to bicycle handlebars. Traumatic pancreatic injuries often result in delayed presentation and treatment, leading to high morbidity and mortality. The management of children with traumatic main pancreatic duct injuries is still under debate.
We report the case of a 9-year-old boy who was presented at our institution with epigastric pain after being stuck with his bicycle handlebar at the upper abdomen and then treated with endoscopic stenting because of a pancreatic ductal injury.
We believe that endoscopic stenting of pancreatic ductal injuries may be a feasible technique in certain cases of children with traumatic pancreatic duct injuries to avoid unnecessary operations.
Core Tip: Traumatic pancreatic injuries often result in delayed presentation and treatment, leading to high morbidity and mortality. The management of children with traumatic main pancreatic duct injuries is still under debate. We report the case of a 9-year-old boy who was presented at our institution with epigastric pain after being stuck with his bicycle handlebar at the upper abdomen and then treated with endoscopic stenting because of a pancreatic ductal injury. We believe that endoscopic stenting of pancreatic ductal injuries may be a feasible technique in certain cases of children with traumatic pancreatic duct injuries to avoid unnecessary operations.
- Citation: Kwon HJ, Jung MK, Park J. Traumatic pancreatic ductal injury treated by endoscopic stenting in a 9-year-old boy: A case report. World J Clin Cases 2023; 11(16): 3885-3890
- URL: https://www.wjgnet.com/2307-8960/full/v11/i16/3885.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i16.3885
Traumatic pancreatic injuries in children are relatively rare because the pancreas is anatomically fixed at the retroperitoneal location, and it accounts for approximately 0.3%-0.7% of all pediatric trauma cases[1-3] and 3%-12% of children with blunt abdominal trauma[4]. Traumatic pancreatic injuries often result in delayed presentation and treatment, leading to high morbidity and mortality. The optimal management of traumatic pancreatic injuries in children has remained a challenge. Herein, we report the case of a 9-year-old boy who was presented at our institution with epigastric pain after being stuck with his bicycle handlebar at the upper abdomen and then treated with endoscopic stenting because of a pancreatic ductal injury.
A 9-year-old boy was admitted to our trauma center with epigastric pain after being stuck with his bicycle handlebar in the upper abdomen.
He complained of mild pain in the epigastric area.
He had a no previous medical history.
His personal and family history were unremarkable.
His vital signs were as follows: Blood pressure, 120/80 mmHg; heart rate, 86 beats per min; respiratory rate, 20 breaths per min; and body temperature, 36.5 °C at the time of arrival. The abdominal physical examination revealed mild tenderness in the epigastrium.
Initial laboratory values revealed normal values for his hemoglobin, platelet, erythrocyte sedimentation rate, and C-reactive protein, however, the white blood cell count was elevated to 13.13 × 109/L (normal range, 4.8-10.8). Renal and hepatic function tests were also within normal limits. Serum amylase and lipase levels were elevated to 841 (normal range, 28-110) U/L and 1159 (normal range, 13-60) U/L, respectively.
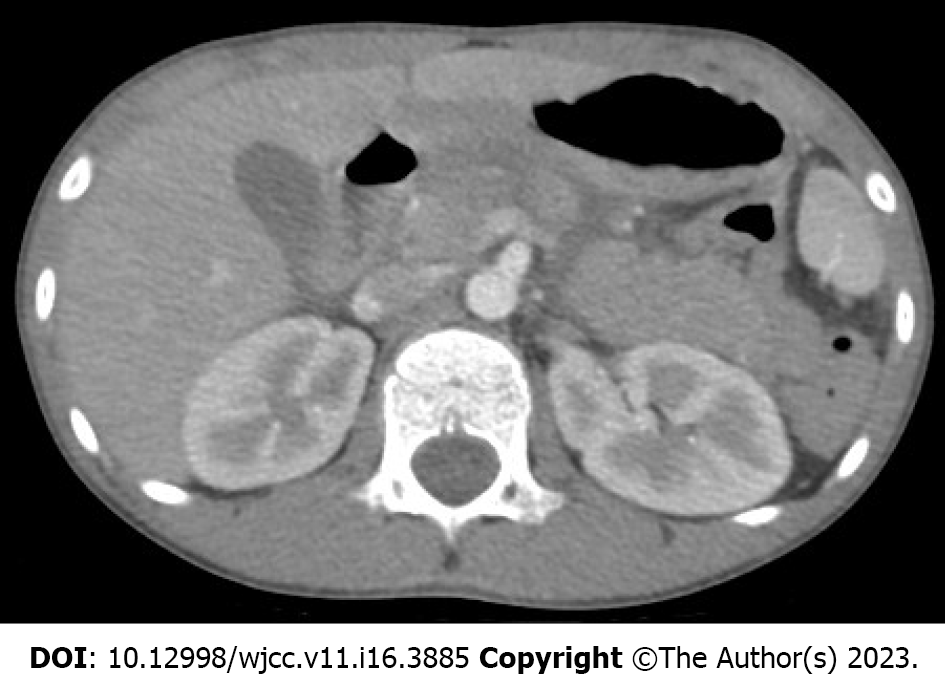
The initial abdominal computed tomography (CT) showed a low attenuation line indicating the transection across the neck of the pancreas with mild fat infiltration into the transverse mesocolon (Figure 1). The pancreatic injury was classified as grade III (distal transection or parenchymal injury with duct injury) according to the American Association for the Surgery of Trauma guidelines. On day 2 after the injury, the serum amylase and lipase levels were 1251 and 1033 U/L, respectively. The follow-up abdominal CT showed progression of the pancreatic disruption and an increase in the amounts of fluid around the pancreas.
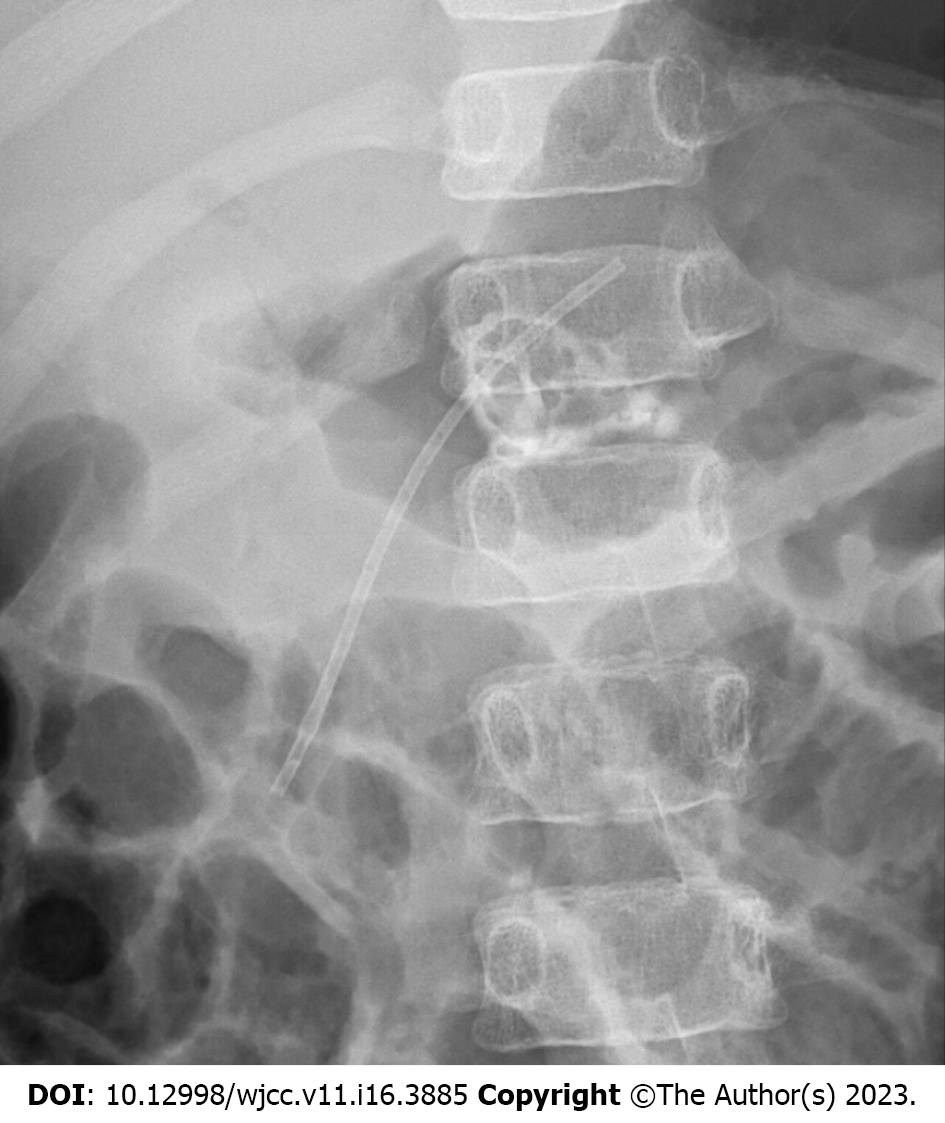
Endoscopic retrograde cholangiopancreatography (ERCP) was performed and revealed a major pancreatic duct disruption with contrast extravasation at the neck of the pancreas (Figure 2).
Endoscopic pancreatic stenting to the distal pancreatic duct was performed. A 5-French pancreatic stent of 7 cm length was placed successfully into the distal pancreatic duct across the injury site of the pancreatic duct (Figure 3). For 2 wk after the injury, the patient was managed conservatively with fasting and total parenteral nutrition. The postprocedural course after stent placement was uneventful. Serum amylase and lipase levels were normalized. He was discharged from the hospital without complications on day 35 after the injury. The pancreatic stent was removed endoscopically without complications 2 mo after the injury.
Pancreatic duct stricture, pseudocyst, or pancreatic atrophy did not appear on a follow-up abdominal CT 10 mo after the injury. The patient has done well without further symptoms or complications at a follow-up of 4 years.
Traumatic pancreatic injuries are relatively rare in children because the pancreas is anatomically fixed at the retroperitoneal location, and they account for approximately 0.3%-0.7% of all pediatric trauma cases[1-3] and 3%-12% of children with blunt abdominal trauma[4]. Most traumatic pancreatic injuries in boys are related to bicycle handlebars[2]. In children, the mechanism of trauma is usually related to the direct compression of the pancreas against the underlying lumbar vertebrae, with a high rate of injury at the pancreatic neck. Traumatic pancreatic injuries often result in delayed presentation and treatment, leading to high morbidity and mortality.
Serum amylase is considered a valuable screening test for traumatic pancreatic injuries. However, the change in serum amylase level by serial estimation must be measured because the serum amylase level may be normal within 48 h after the traumatic injury[5,6].
Abdominal CT remains the most effective and widely available imaging modality to assess the traumatic pancreatic injury in children. However, several reports have mentioned the limitations of CT in detecting pancreatic ductal injuries[6-9]. It may be unreliable in the first 24 h after the traumatic injury because of early tissue edema and the relative lack of retroperitoneal fat planes in children. In addition, the transection of the pancreas may not be apparent until the tissue edema subsides to demonstrate parenchymal disruption[7].
Defining the integrity of the pancreatic duct is critical in making a treatment decision for operative vs nonoperative management in a patient with a traumatic pancreatic injury. Compared with CT, magnetic resonance cholangiopancreatography (MRCP) is often performed to gain supplementary information about the integrity of the pancreatic duct. MRCP can distinctly visualize the pancreatic duct injury and other signs of pancreatic injuries, such as laceration, fluid, and hematoma. However, in a multi-institutional analysis, MRCP was more useful than CT for identifying the pancreatic duct but may not be superior for confirmation of the pancreatic duct integrity in children with blunt traumatic pancreatic injuries[8]. They suggested that ERCP may be necessary to confirm pancreatic duct disruption when considering pancreatic resection[8].
The effectiveness of ERCP to delineate the pancreatic duct anatomy in traumatic pancreatic injuries has been well documented in adults. ERCP accurately demonstrates the location and degree of pancreatic duct disruption and guides treatment decisions based on the degree of the pancreatic duct injury. Furthermore, the pancreatic ductal injury may be stented with ERCP to facilitate nonoperative management. Endoscopic pancreatic stenting can also ameliorate the patient’s clinical condition and resolve pancreatic fistula or pseudocyst. However, its application in children remains poorly described because of technical difficulty in cannulating the small ampulla of Vater, infection, and post-ERCP pancreatitis. Since the first description by Hall et al[10], several studies have suggested the safety and effectiveness of ERCP in children[11-13]. Rescorla et al[13] conducted ERCP in six children with major pancreatic ductal transection without serious adverse effects related to ERCP.
The optimal management of traumatic pancreatic injuries in children remains challenging. The advantages and safety of operative vs nonoperative management, especially in cases of traumatic pancreatic ductal injuries, are still being debated[14-18]. The nonoperative treatment of a minor pancreatic injury without a ductal injury (grade I) is generally recognized because they usually resolve spontaneously after conservative treatment[19-21]. However, there have been controversies regarding the most suitable management for children (grade II, III, or IV) with more serious pancreatic injuries or main pancreatic duct injuries. Early operative treatment might shorten the length of hospital stay and reduce the incidence of pseudocyst formation and total parenteral nutrition-associated complications. Nevertheless, there would be surgery-related complications, such as pancreatic fistula, small bowel obstruction, and incidental splenectomy[2]. Meier et al[17] reported that early surgical pancreatic resection restores the child’s health and lessens the inconvenience and emotional stress associated with longer hospitalization than nonoperative management. Jobst et al[18] mentioned that distal pancreatic duct injuries were best treated by prompt spleen-sparing distal pancreatectomy. However, since most reports are retrospective studies that analyzed a small number of cases and injuries and management vary, a clear treatment guideline on how to treat pediatric patients with traumatic pancreatic injuries is not easy to establish.
In summary, we believe that endoscopic stenting of pancreatic ductal injuries may be a feasible technique in certain cases of children with traumatic pancreatic duct injuries to avoid unnecessary operations.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Giacomelli L, Italy; Rocha R, Brazil S-Editor: Li L L-Editor: A P-Editor: Fan JR
| 1. | Englum BR, Gulack BC, Rice HE, Scarborough JE, Adibe OO. Management of blunt pancreatic trauma in children: Review of the National Trauma Data Bank. J Pediatr Surg. 2016;51:1526-1531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 48] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 2. | Houben CH, Ade-Ajayi N, Patel S, Kane P, Karani J, Devlin J, Harrison P, Davenport M. Traumatic pancreatic duct injury in children: minimally invasive approach to management. J Pediatr Surg. 2007;42:629-635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 77] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 3. | Ishikawa M, Shimojima N, Koyama T, Miyaguni K, Tsukizaki A, Mizuno Y, Hashimoto M, Ishihama H, Tomita H, Shimotakahara A, Hirobe S. Efficacy of early endoscopic intervention in pediatric pancreatic duct injury management. Pediatr Surg Int. 2021;37:1711-1718. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 4. | Iqbal CW, St Peter SD, Tsao K, Cullinane DC, Gourlay DM, Ponsky TA, Wulkan ML, Adibe OO; Pancreatic Trauma in Children (PATCH) Study Group. Operative vs nonoperative management for blunt pancreatic transection in children: multi-institutional outcomes. J Am Coll Surg. 2014;218:157-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 52] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 5. | Shilyansky J, Sena LM, Kreller M, Chait P, Babyn PS, Filler RM, Pearl RH. Nonoperative management of pancreatic injuries in children. J Pediatr Surg. 1998;33:343-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 78] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Firstenberg MS, Volsko TA, Sivit C, Stallion A, Dudgeon DL, Grisoni ER. Selective management of pediatric pancreatic injuries. J Pediatr Surg. 1999;34:1142-1147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 28] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Wales PW, Shuckett B, Kim PC. Long-term outcome after nonoperative management of complete traumatic pancreatic transection in children. J Pediatr Surg. 2001;36:823-827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 81] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 8. | Rosenfeld EH, Vogel A, Russell RT, Maizlin I, Klinkner DB, Polites S, Gaines B, Leeper C, Anthony S, Waddell M, St Peter S, Juang D, Thakkar R, Drews J, Behrens B, Jafri M, Burd RS, Beaudin M, Carmant L, Falcone RA Jr, Moody S, Naik-Mathuria BJ. Comparison of diagnostic imaging modalities for the evaluation of pancreatic duct injury in children: a multi-institutional analysis from the Pancreatic Trauma Study Group. Pediatr Surg Int. 2018;34:961-966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 9. | Lin BC, Wong YC, Chen RJ, Liu NJ, Wu CH, Hwang TL, Hsu YP. Major pancreatic duct continuity is the crucial determinant in the management of blunt pancreatic injury: a pancreatographic classification. Surg Endosc. 2017;31:4201-4210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Hall RI, Lavelle MI, Venables CW. Use of ERCP to identify the site of traumatic injuries of the main pancreatic duct in children. Br J Surg. 1986;73:411-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 50] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Rosenfeld EH, Vogel AM, Klinkner DB, Escobar M, Gaines B, Russell R, Campbell B, Wills H, Stallion A, Juang D, Thakkar RK, Upperman J, Jafri M, Burd R, Naik-Mathuria BJ; Pancreatic Trauma Study Group. The utility of ERCP in pediatric pancreatic trauma. J Pediatr Surg. 2017;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Garvey EM, Haakinson DJ, McOmber M, Notrica DM. Role of ERCP in pediatric blunt abdominal trauma: a case series at a level one pediatric trauma center. J Pediatr Surg. 2015;50:335-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Rescorla FJ, Plumley DA, Sherman S, Scherer LR 3rd, West KW, Grosfeld JL. The efficacy of early ERCP in pediatric pancreatic trauma. J Pediatr Surg. 1995;30:336-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 62] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 14. | Kawahara I, Maeda K, Ono S, Kawashima H, Deie R, Yanagisawa S, Baba K, Usui Y, Tsuji Y, Fukuta A, Sekine S. Surgical reconstruction and endoscopic pancreatic stent for traumatic pancreatic duct disruption. Pediatr Surg Int. 2014;30:951-956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Wood JH, Partrick DA, Bruny JL, Sauaia A, Moulton SL. Operative vs nonoperative management of blunt pancreatic trauma in children. J Pediatr Surg. 2010;45:401-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 60] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 16. | Mora MC, Wong KE, Friderici J, Bittner K, Moriarty KP, Patterson LA, Gross RI, Tirabassi MV, Tashjian DB. Operative vs Nonoperative Management of Pediatric Blunt Pancreatic Trauma: Evaluation of the National Trauma Data Bank. J Am Coll Surg. 2016;222:977-982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 17. | Meier DE, Coln CD, Hicks BA, Guzzetta PC. Early operation in children with pancreas transection. J Pediatr Surg. 2001;36:341-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 65] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 18. | Jobst MA, Canty TG Sr, Lynch FP. Management of pancreatic injury in pediatric blunt abdominal trauma. J Pediatr Surg. 1999;34:818-23; discussion 823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 91] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 19. | Koh EY, van Poll D, Goslings JC, Busch OR, Rauws EA, Oomen MW, Besselink MG. Operative Versus Nonoperative Management of Blunt Pancreatic Trauma in Children: A Systematic Review. Pancreas. 2017;46:1091-1097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 20. | Paul MD, Mooney DP. The management of pancreatic injuries in children: operate or observe. J Pediatr Surg. 2011;46:1140-1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 21. | Maeda K, Ono S, Baba K, Kawahara I. Management of blunt pancreatic trauma in children. Pediatr Surg Int. 2013;29:1019-1022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |