Published online Jun 6, 2023. doi: 10.12998/wjcc.v11.i16.3877
Peer-review started: March 10, 2023
First decision: April 10, 2023
Revised: April 18, 2023
Accepted: May 6, 2023
Article in press: May 6, 2023
Published online: June 6, 2023
Processing time: 83 Days and 19.9 Hours
Postpartum ovarian vein thrombosis (POVT) is a rare puerperal complication. It is easily missed or misdiagnosed due to its insidious onset and lack of specific clinical symptoms and signs. This paper reports two patients who developed right ovarian vein thrombosis after cesarean section and vaginal delivery, respectively.
Case 1 was a 32-year-old female who underwent a cesarean section in labor at 40 wk of gestation due to fetal distress. The patient was persistently febrile after the operation and escalated antibiotic treatment was ineffective. POVT was diagnosed by abdominal computed tomography (CT) and was treated by increasing the dose of low molecular weight heparin (LMWH). Case 2 was a 21-year-old female with a spontaneous vaginal delivery at 39 wk of gestation. The patient developed fever and abdominal pain 3 days after delivery. POVT was promptly identified by abdominal CT, and the condition was quickly controlled after treatment with LMWH and antibiotics.
These two cases occurred after cesarean section and vaginal delivery, respectively. The diagnosis was mainly based on imaging examination due to the unspecific clinical symptoms and signs, the CT scan provided an especially high diagnostic value. Comparing these two cases, escalating antibiotics alone did not provide significant therapeutic benefit, but the early escalation of anticoagulant dosage seemed to shorten the disease course. Therefore, early diagnosis by CT followed by aggressive anticoagulation might have a positive effect on improving the prognosis of the disease.
Core Tip: Postpartum ovarian vein thrombosis (POVT) is a rare puerperal complication. It is easily missed or misdiagnosed due to its insidious onset and lack of specific clinical symptoms and signs. Retrospective literature showed that anticoagulation and anti-infection agents constituted the main treatment modalities for this disease, and the definite diagnosis before treatment mainly depended on imaging diagnosis, especially computed tomography (CT) scans. This paper reports two cases in which early diagnosis and timely treatment likely led to a shorter disease course. Therefore, for patients in whom POVT is suspected, an early CT scan can assist in the early diagnosis. Of course, in view of radiation and other side effects, the clinical overuse of CT scans should still be avoided.
- Citation: Zhu HD, Shen W, Wu HL, Sang X, Chen Y, Geng LS, Zhou T. Postpartum ovarian vein thrombosis after cesarean section and vaginal delivery: Two case reports. World J Clin Cases 2023; 11(16): 3877-3884
- URL: https://www.wjgnet.com/2307-8960/full/v11/i16/3877.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i16.3877
Postpartum ovarian vein thrombosis (POVT) is a relatively rare puerperal complication with an incidence of 0.01%-0.18%[1-3], and is more common after cesarean delivery than vaginal delivery[4]. However, the condition is easily missed or misdiagnosed due to its unspecific clinical symptoms and signs. Delayed diagnosis and treatment may lead to serious complications such as inferior vena cava thrombosis and pulmonary embolism and even endanger maternal life. Therefore, prompt diagnosis and treatment are particularly important. This paper reports two cases of postpartum ovarian vein thrombosis and reviews the relevant literature to provide a reference for the clinical diagnosis and treatment of this condition.
Case 1: A 32-year-old G2P0 female who underwent a cesarean section in labor at 40 wk of gestation due to fetal distress. However, she developed persistent abdominal pain and fever after the operation.
Case 2: A 21-year-old G1P0 female with a spontaneous vaginal delivery at 39 wk of gestation. She also had symptoms such as abdominal pain and fever after delivery.
Case 1: The patient was hospitalized at 40 wk of gestation with possible fetal macrosomia. She had a height of 156 cm, a weight of 72 kg, and a body mass index (BMI) of 29.5 kg/m2. The patient was administered 0.5% oxytocin (2.5 IU oxytocin added to 500 mL 0.9% sodium chloride injection) by intravenous drip to induce labor. On the same day, frequent late fetal heart deceleration was observed. As the uterine orifice was dilated to only 7 cm, an emergency cesarean section (C-section) of the lower uterine section was performed due to fetal distress. A male newborn with a birthweight of 4130 g and an APGAR score of 10-10/1-5 min was delivered. The operation lasted 32 min and went smoothly, with 300 mL of intraoperative bleeding.
The patient was administered cefuroxime at 1.5 g q8h after the C-section. Referring to the Queensland Clinical Guidelines for Venous thromboembolism (VTE) in pregnancy and the puerperium[5], her risk score was 3 (cesarean section in labor). The patient was administered low molecular weight heparin (LMWH) at 4100 IU qd for standard prophylaxis 12 h after C-section and was informed to mobilize early and move frequently to reduce the risk of thrombosis.
On postoperative day 1, the patient had a fever with a body temperature of 38.2℃ and no abdominal pain. The white blood cell (WBC) count was 16.40 × 109/L with a neutrophil percentage (NEUT%) of 88.7%, and the high sensitive C-reactive protein (hs-CRP) level was 67.49 mg/L. On postoperative day 2, she developed right-sided abdominal pain, and the physical examination showed tenderness on the right edge of the uterus. The body temperature was 38.3℃, and the laboratory examinations were repeated, revealing a WBC count of 16.19 × 109/L, NEUT% of 91.5%, and hs-CRP of 174.52 mg/L. Therefore, she was diagnosed with a pelvic infection, and the antibiotic was changed to cefoperazone sulbactam at 2.0 g q8h. On postoperative day 4, the patient showed no improvement in abdominal pain, and the temperature was still 38.2℃, with a WBC count of 12.15 × 109/L, NEUT% of 83.4 %, and hs-CRP of 129.11 mg/L. However, the ultrasound of the lower abdomen and vascular ultrasound of both lower extremities showed no significant abnormalities. On postoperative day 6, the body temperature was 37.9℃, and the right-sided abdominal pain was still present. The WBC count was 12.90 × 109/L, with a NEUT% of 82.7%, and an hs-CRP level of 199.22 mg/L. Considering that the abdominal pain and fever had not subsided and the significant increase in hs-CRP, the antibiotic regimen was switched to linezolid at 0.6 g q12h and piperacillin-tazobactam at 4.5 g q8h.
Case 2: The patient was hospitalized for labor at 39 wk of gestation. Her height was 156 cm, her weight was 65 kg, and her BMI was 26.7 kg/m2. On the night of admission, a male newborn was delivered vaginally with a birth weight of 3450 g and an APGAR score of 10-10/1-5 min. The birth process went smoothly, with a total labor time of 16 h and 200 mL of hemorrhage.
Referring to the Queensland Clinical Guidelines for VTE in pregnancy and the puerperium[5], her risk score was 0. Therefore, the patient was not administered LMWH but was also informed to mobilize early and frequently move to reduce the risk of thrombosis. Two days after delivery, her body temperature was normal, and the recovery was smooth. The WBC count was 12.57 × 109/L, the NEUT% was 84.4%, and the hs-CRP level was 57.0 mg/L.
On postpartum day 3, the patient developed a fever of 38.3℃, accompanied by right-sided lower abdominal pain. The physical examination showed tenderness in the right lower abdomen. The WBC count was 12.04 × 109/L, the NEUT% was 84.5%, and the hs-CRP level was 167.91 mg/L. Her signs and symptoms were similar to those in case 1.
Case 1: In January 2019, the patient underwent curettage for hydatidiform mole, and the postoperative follow-up was uneventful. She had regular menstrual cycles.
Case 2: The patient had no previous medical history or any surgical interventions in the past.
Case 1 and Case 2: The personal and family history was unremarkable.
Not applicable.
Not applicable.
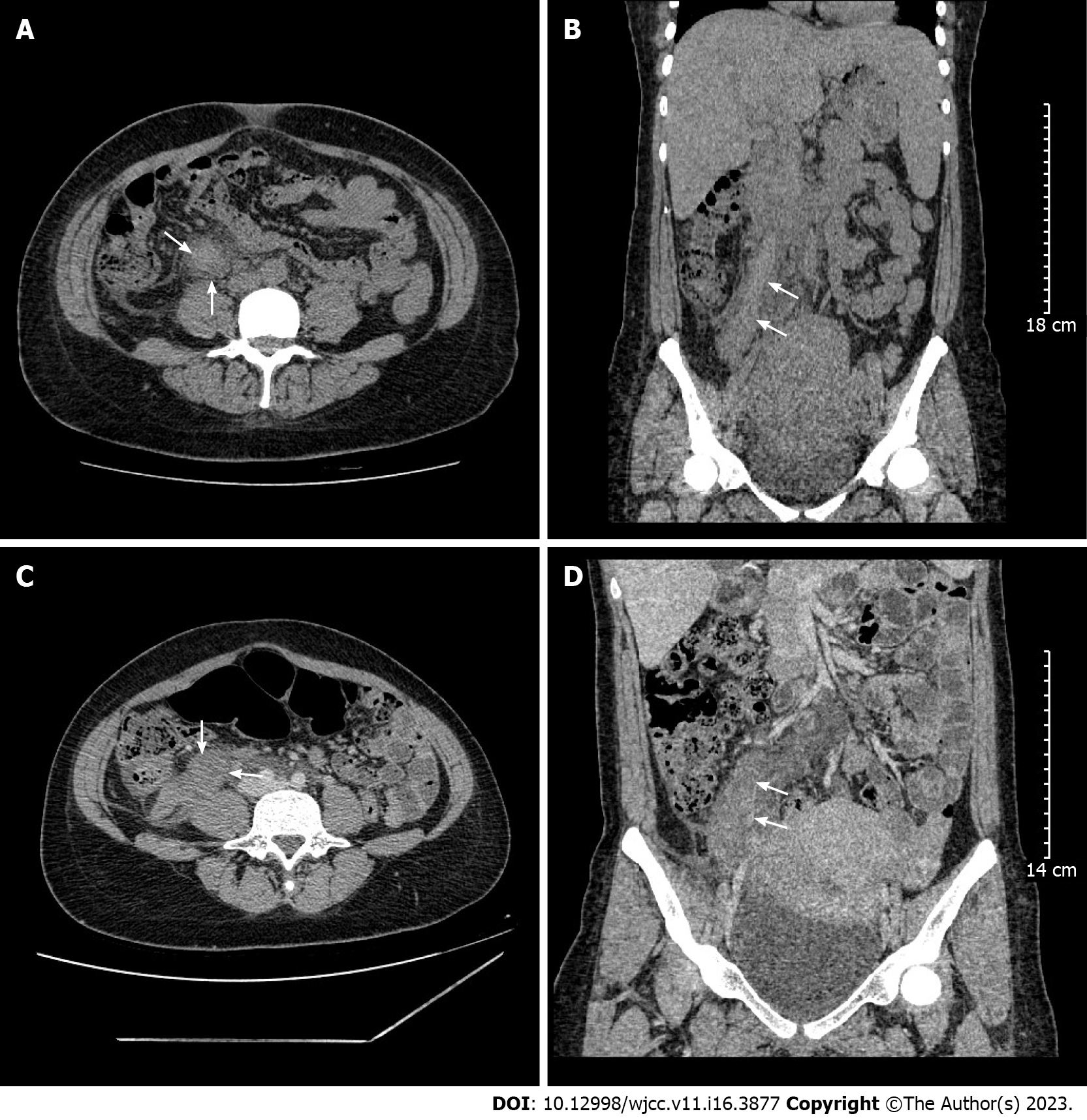
Case 1: On postoperative day 7, the body temperature was 37.8℃, and an abdominal computed tomography (CT) scan was performed, revealing a strip of high-density shadow in the meridian area of the right ovarian vein (Figure 1A and B), which was highly indicative of venous thrombosis.
Case 2: On postpartum day 3, an abdominal CT scan showed a twisted strip of shadow from the lower pole of the right kidney to the right side of the uterus, which raised suspicions of venous thrombosis. On the next day, a CT enhancement scan revealed a tortuous vascular shadow in the right adnexal area and confirmed the diagnosis of right ovarian vein thrombosis (OVT) (Figure 1C and D).
Based on CT scans, both patients were diagnosed with right OVT.
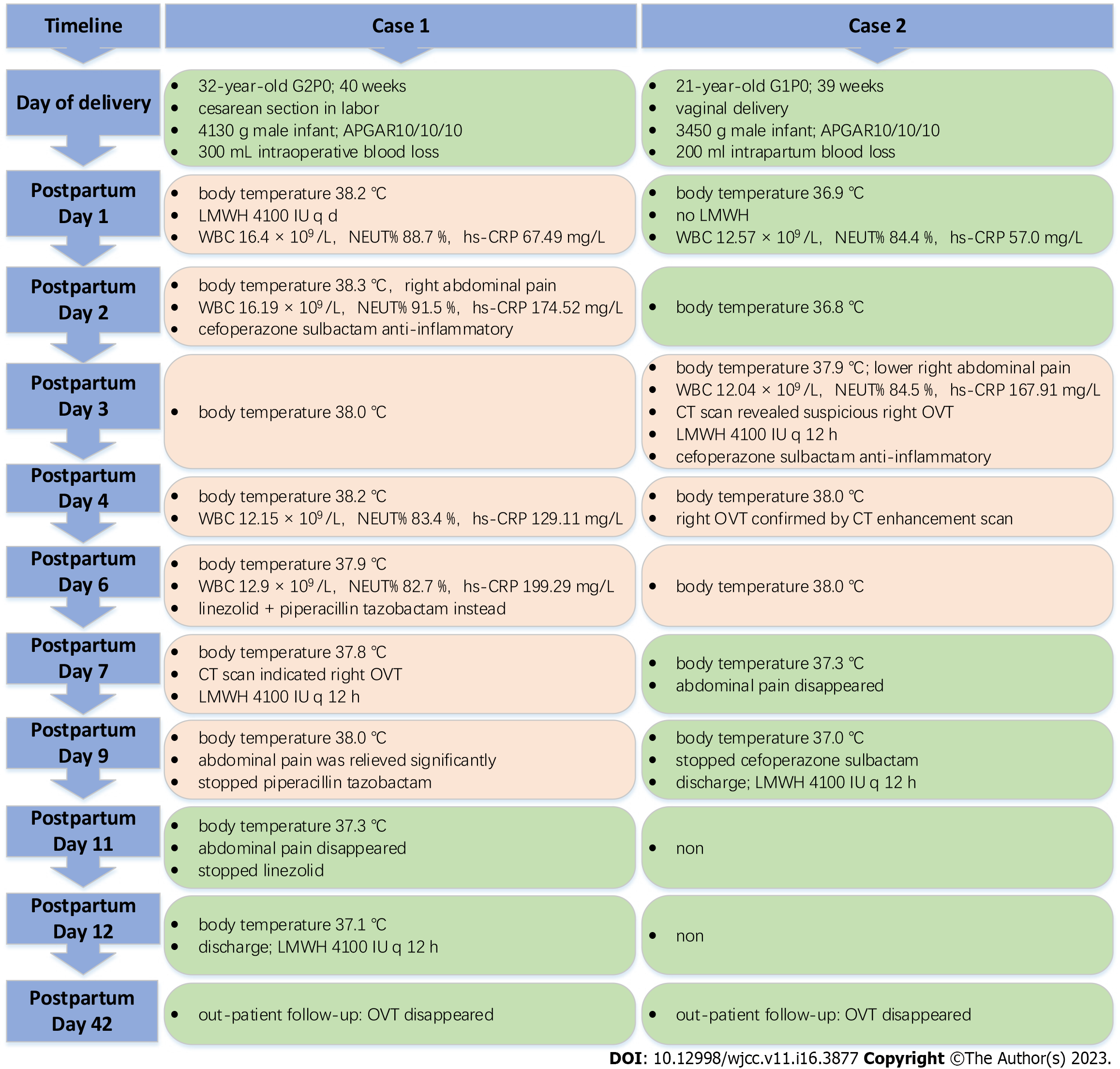
Case 1: After POVT was diagnosed, the anticoagulation treatment was immediately changed to LMWH 4100 IU q12h. On postoperative day 9, the abdominal pain was significantly relieved, and piperacillin-tazobactam was stopped. On postoperative day 11, the body temperature returned to normal, abdominal pain had disappeared, and linezolid was stopped. On postoperative day 12, she was discharged from the hospital and treated with LMWH at 4100 IU q12h for 3 mo.
Case 2: After right OVT was diagnosed, LMWH was administered at 4100 IU q12h for anticoagulation and cefoperazone sulbactam at 2.0 g q8h for anti-infection. With the above treatment, her abdominal pain was gradually relieved. On postpartum day 7, the body temperature returned to normal, with minimal abdominal pain. On postpartum day 9, the antibiotics were discontinued, and the patient was discharged. LMWH at 4100 IU q12h was administered for 3 mo.
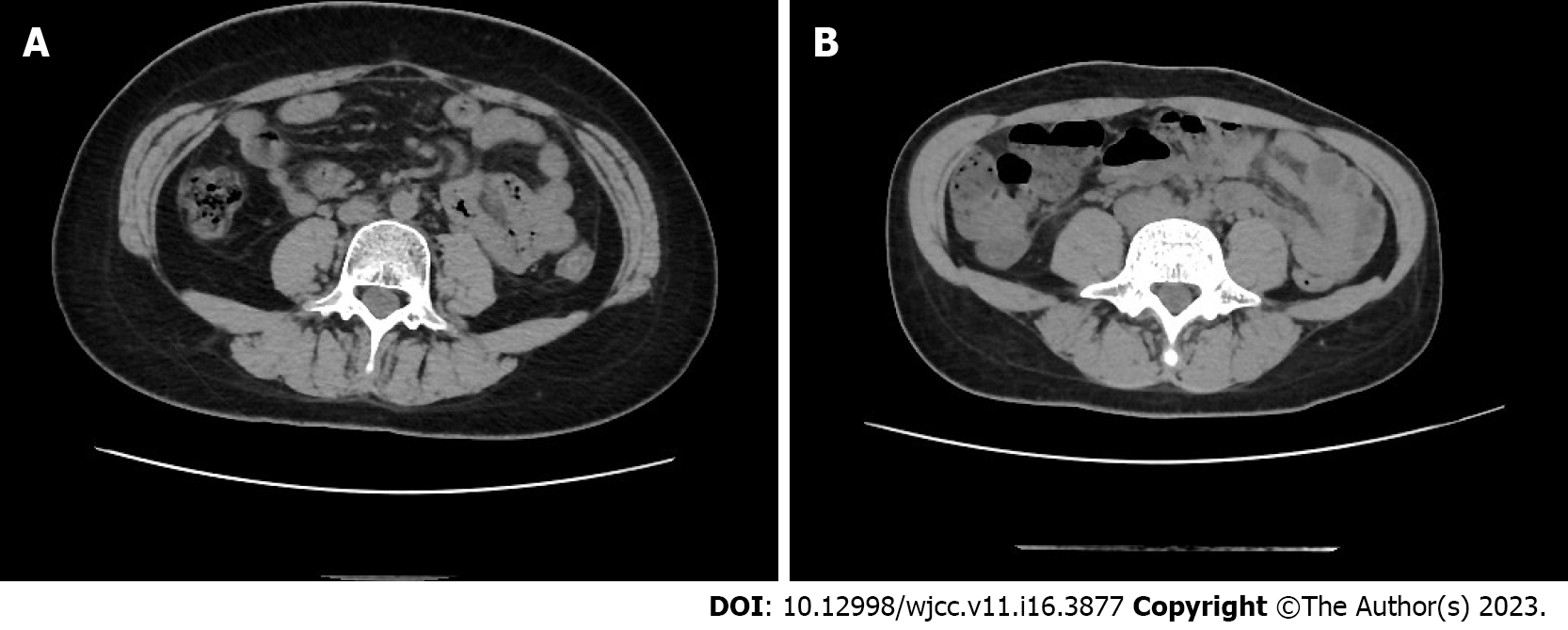
Case 1: The repeat CT scan 42 days after the C-section revealed that the right OVT had disappeared (Figure 2A).
Case 2: The CT scan 42 days after delivery also revealed that the right OVT had disappeared (Figure 2B).
This paper reports two patients with POVT (the timeline from diagnosis to treatment is displayed in Figure 3), one after C-section and the other after vaginal delivery. In case 1, the disease was initially misdiagnosed, which resulted in delayed treatment and slow recovery. Having learned from case 1, our team promptly diagnosed and treated case 2, leading to a quick recovery. Therefore, the literature related to this disease was reviewed and summarized.
A higher incidence has been reported after C-section than after vaginal delivery[2,6], and the right ovarian vein is also significantly more commonly affected than the left, with 80% to 90% of cases involving the right ovarian vein[7]. This finding may be attributed to the right ovarian vein being longer than the left, and the right ovarian vein is compressed by the right rotation of the enlarged uterus in late pregnancy. The two cases reported also developed thrombosis in the right ovarian vein.
POVT has an insidious onset and atypical clinical symptoms. Its most common symptom is lower quadrant abdominal pain, usually on the side of the thrombosed vein[3,8]. Other signs include fever and palpable abdominal mass[9,10]. As the ovarian veins have a deep anatomical location, positive signs on physical examination are also difficult to detect. Hence, the disease is easily missed and misdiagnosed and can lead to serious and fatal complications such as pulmonary embolism[11,12]. According to the literature[13], the peak onset of POVT is 2 d after delivery, and about 90% of cases occurred within 10 d of delivery. In the current study, the 2 cases both developed within 3 d of delivery, which is also consistent with relevant reports. The differential diagnoses include puerperal pelvic infections, ovarian tumor torsion, acute appendicitis, pyelonephritis, and renal calculi. Furthermore, both cases presented with fever and abdominal pain as the main symptoms, with no other specific manifestations. Due to the rarity of the disease and our lack of clinical experience, case 1 was misdiagnosed as a puerperal pelvic infection. However, we learned from the experience, and case 2 was diagnosed early.
The changes observed in the laboratory examination of POVT are also not specific, mostly characterized by an increase in infectious indicators such as WBC count, NEUT%, hs-CRP, and procalcitonin, while urine culture and blood culture are usually negative[14]. These are consistent with the cases reported in this paper.
Imaging examination is of great value in the diagnosis of POVT. Ultrasound has a sensitivity of 63% and a specificity of 78%, while CT has a sensitivity of 100% and a specificity of 90%, and magnetic resonance imaging (MRI) has a sensitivity of 92% and a specificity of 100%[11]. Although ultrasound is more economical and radiation-free, its application is limited by factors such as abdominal distention, resulting in low diagnostic sensitivity and specificity. MRI is radiation-free but costs much more than CT. Although CT involves radiation, it is still used as the preferred choice in diagnosing POVT due to its high sensitivity, specificity, and lower cost compared to MRI. The cases we reported confirmed that CT has higher sensitivity than ultrasound and also has high specificity.
Currently, there are no guidelines or treatment standards for POVT, and the main treatments include anticoagulation and anti-infection agents. However, the optimal treatment remains controversial.
Khishfe et al[15] suggested that POVT patients with fever and elevated WBC count be treated with broad-spectrum antibiotics for 7-10 d. Bannow et al[11] also recommended antibiotics for POVT patients with suspected infection but did not recommend a specific duration of treatment. Both cases showed signs of infection, such as fever, elevated WBC count, and hs-CRP levels, and both were treated with antibiotics.
POVT should be considered when antibiotics alone are ineffective, and the symptoms persist or even worsen[16]. In case 1, escalating antibiotics yielded unsatisfactory results, and the condition improved significantly after switching to LMWH q12h. In case 2, broad-spectrum antibiotics were administered after prompt diagnosis, with LMWH q12h, resulting in a significantly shorter disease duration than in case 1. Therefore, our cases support the majority of literature, demonstrating that anticoagulation is necessary for POVT patients, even though there are still no guidelines recommending specific anticoagulant drugs, dosage, and course[17]. In the two cases we reported, the anticoagulant treatment with LMWH at 4100 IU q12h was effective, but case 1 also reflected that the treatment with LMWH at 4100 IU qd was not effective. The duration of anticoagulation is inconclusive, and some literature suggested a mean duration of treatment of 3 mo[3,8,11]. Other authors suggested referring to the clinical management of thromboembolism in pregnancy in the absence of clear evidence[18]. Both cases reported in this study were anticoagulated for 3 mo, and the CT scan on postpartum day 42 revealed that the thrombus had disappeared.
In conclusion, POVT is a rare and insidious postpartum disease with non-specific symptoms and signs. However, early and definitive diagnosis and treatment are particularly important to shorten the course of the disease and reduce the occurrence of potentially serious complications, such as pulmonary embolism. POVT should be considered in postpartum women with unexplained fever and abdominal pain, especially when antibiotics alone are not effective. CT scan has a high diagnostic value and allows the early diagnosis of suspected POVT patients. Early aggressive anticoagulation and anti-infection agents should have a definite effect. However, in view of radiation and other side effects, the clinical overuse of CT scans should still be avoided.
We would like to thank these two patients for allowing us to share their cases and using their picture and we are also grateful to all of our team members who were involved in the management of the cases.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Obstetrics and gynecology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mohey NM, Egypt; Shariati MBH, Iran S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Brown TK, Munsick RA. Puerperal ovarian vein thrombophlebitis: a syndrome. Am J Obstet Gynecol. 1971;109:263-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 68] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Dunnihoo DR, Gallaspy JW, Wise RB, Otterson WN. Postpartum ovarian vein thrombophlebitis: a review. Obstet Gynecol Surv. 1991;46:415-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 113] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Rottenstreich A, Da'as N, Kleinstern G, Spectre G, Amsalem H, Kalish Y. Pregnancy and non-pregnancy related ovarian vein thrombosis: Clinical course and outcome. Thromb Res. 2016;146:84-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | Brown CE, Stettler RW, Twickler D, Cunningham FG. Puerperal septic pelvic thrombophlebitis: incidence and response to heparin therapy. Am J Obstet Gynecol. 1999;181:143-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 81] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 5. | Health Q. Queensland clinical guidelines (No.MN14.9-V5-R19): venous thromboembolism (VTE) in pregnancy and the puerperium [EB/OL]. 2020. [DOI] [Full Text] |
| 6. | Salomon O, Dulitzky M, Apter S. New observations in postpartum ovarian vein thrombosis: experience of single center. Blood Coagul Fibrinolysis. 2010;21:16-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Kodali N, Veytsman I, Martyr S, Lu K. Diagnosis and management of ovarian vein thrombosis in a healthy individual: a case report and a literature review. J Thromb Haemost. 2017;15:242-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 8. | Labropoulos N, Malgor RD, Comito M, Gasparis AP, Pappas PJ, Tassiopoulos AK. The natural history and treatment outcomes of symptomatic ovarian vein thrombosis. J Vasc Surg Venous Lymphat Disord. 2015;3:42-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 9. | Sinha D, Yasmin H, Samra JS. Postpartum inferior vena cava and ovarian vein thrombosis--a case report and literature review. J Obstet Gynaecol. 2005;25:312-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Akinbiyi AA, Nguyen R, Katz M. Postpartum ovarian vein thrombosis: two cases and review of literature. Case Rep Med. 2009;2009:101367. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Bannow BTS, Skeith L. Diagnosis and management of postpartum ovarian vein thrombosis. Hematology Am Soc Hematol Educ Program. 2017;2017:168-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Fei Z, Peng A, Wang L, Zhang L. Pulmonary embolism caused by postpartum ovarian vein thrombophlebitis after vaginal delivery: Case report and brief review of the literature. J Clin Ultrasound. 2020;48:291-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Klima DA, Snyder TE. Postpartum ovarian vein thrombosis. Obstet Gynecol. 2008;111:431-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Djakovic I, Mustapic M, Marleku F, Grgic O, Djakovic Z, Kosec V. Ovarian vein thrombosis--a case report. Acta Clin Belg. 2015;70:445-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Khishfe BF, Sankovsky A, Nasr I. Idiopathic ovarian vein thrombosis: a rare cause of abdominal pain. Am J Emerg Med. 2016;34:935.e1-935.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Salomon O, Apter S, Shaham D, Hiller N, Bar-Ziv J, Itzchak Y, Gitel S, Rosenberg N, Strauss S, Kaufman N, Seligsohn U. Risk factors associated with postpartum ovarian vein thrombosis. Thromb Haemost. 1999;82:1015-1019. [PubMed] |
| 17. | Cao W, Ni X, Wang Q, Li J, Li Y, Chen T, Wang X. Early diagnosis and precision treatment of right ovarian vein and inferior vena cava thrombosis following caesarean section: A case report. Exp Ther Med. 2020;19:2923-2926. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | American College of Obstetricians and Gynecologists' Committee on Practice Bulletins—Obstetrics. ACOG Practice Bulletin No. 196: Thromboembolism in Pregnancy. Obstet Gynecol. 2018;132:e1-e17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 274] [Article Influence: 45.7] [Reference Citation Analysis (0)] |