Published online Jun 6, 2023. doi: 10.12998/wjcc.v11.i16.3864
Peer-review started: February 21, 2023
First decision: March 28, 2023
Revised: April 4, 2023
Accepted: May 6, 2023
Article in press: May 6, 2023
Published online: June 6, 2023
Processing time: 100 Days and 20.7 Hours
The coexistence of a heterotopic pregnancy with a giant ovarian cyst is an incredibly rare abnormal pregnancy in cases of natural conception. The incidence of this condition has increased significantly as a result of the continuous development of assisted reproductive technologies. When this type of pregnancy occurs, both the continuation of intrauterine pregnancy and the life of the pregnant woman are severely threatened. Early diagnosis and treatment using safe and effective methods are paramount in this situation.
A 30-year-old primigravida at a gestation age determined as 8 wk 4 d by scan was admitted to the hospital with heterotopic pregnancy and a right ovarian cyst. Laparoscopic resection of the ectopic pregnancy was performed, but the intrauterine pregnancy and ovarian cyst were preserved.
The approach to a patient with heterotopic pregnancy and a giant ovarian cyst is individualized base on the fertility requirements. We recommend the following: (1) If the patient satisfies parity and has no fertility requirement, a laparoscopic salpingectomy should be performed and the giant ovarian cyst and intrauterine pregnancy removed; (2) If the patient has fertility requirements wishes to have more children in the future, laparoscopic salpingectomy or salpingostomy should be performed and the intrauterine pregnancy preserved. Serial ovarian cyst aspiration can be performed under ultrasound and resection can be done after delivery; and (3) Heterotopic pregnancy should be diagnosed early by active surveillance during antenatal visits using ultra sound as this is important for the avoidance of catastrophic complications.
Core Tip: Heterotopic pregnancy with a giant ovarian cyst is an unusual and abnormal pregnancy after natural conception, which can threaten the continuation of intrauterine pregnancy and life of the pregnant woman. Thus, early diagnosis and treatment are essential. This paper reports a rare case of heterotopic pregnancy complicated by a giant ovarian cyst. We recommend that if the patient has satisfied parity, a laparoscopic salpingectomy should be performed and the giant ovarian cyst and intrauterine pregnancy be removed; and if the patient wishes to have more children, laparoscopic salpingectomy or salpingostomy should be performed and the intrauterine pregnancy preserved.
- Citation: Kong YY, Chanda K, Ying XY. Giant cyst in heterotopic pregnancy: A case report. World J Clin Cases 2023; 11(16): 3864-3869
- URL: https://www.wjgnet.com/2307-8960/full/v11/i16/3864.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i16.3864
The coexistence of intrauterine and ectopic pregnancy is known as heterotopic pregnancy and has an incidence of 1/100000[1]. The rapid development of artificial reproduction technologies has resulted in increased incidence of heterotopic pregnancies and theca lutein ovarian cysts[2]. A theca lutein ovarian cyst, also called hyperreactive xanthinization, was previously believed to occur in multiple pregnancies, hypertensive disorders of pregnancy, blood group incompatibility, trophoblastic disorders, oral administration of large amounts of estrogen, and in ovulation induced by gonadotropins. This paper retrospectively analyzed a recent case of heterotopic pregnancy with a large theca lutein ovarian cyst. Early diagnosis and treatment is essential in such a situation for increasing the chance of a favorable pregnancy outcome.
No menstruation for more than 3 mo, vaginal bleeding for 1 d.
A 30-year-old female, primigravida, post-assisted reproductive technology (ART), 8 wk 4 d gestational age by scan, Chinese, Han tribe women presented with vaginal bleeding for 1 d. She had no previous history of headache, dizziness, abdominal pain, vaginal discharge, dysuria, diarrhea, coughing, or fever.
The patient’s history of past illness was found to be non-revealing.
The patient had no reproductive history and denied a family history of hereditary diseases or malignancies.
The patient was conscious, mobile, cooperative during the physical examination, and all vital signs were normal. The physical examination of the vagina resulted in blood on a gloved finger. The uterus was approximately the size of that of a woman during the 2nd month of pregnancy. The bilateral adnexal area was thickened and no tenderness was observed.
The carbohydrate antigen 125 was 187 U/mL. Other routine blood and urine tests and tumor markers indicated no abnormalities.
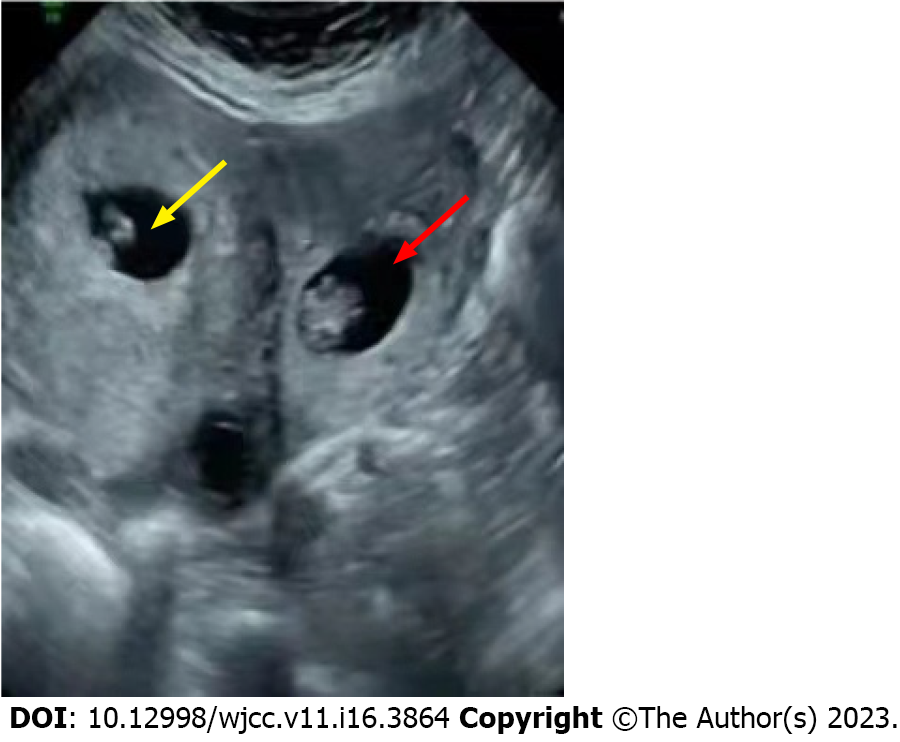
A B-scan performed on admission revealed an intrauterine pregnancy at gestation age of 8 wk and 4 d with a heartbeat, enlarged left fallopian tube with a mixed mass of 3.6 cm × 3.4 cm with active blood flow (Figure 1), and a right ovarian mass of 4.9 cm × 4.3 cm.
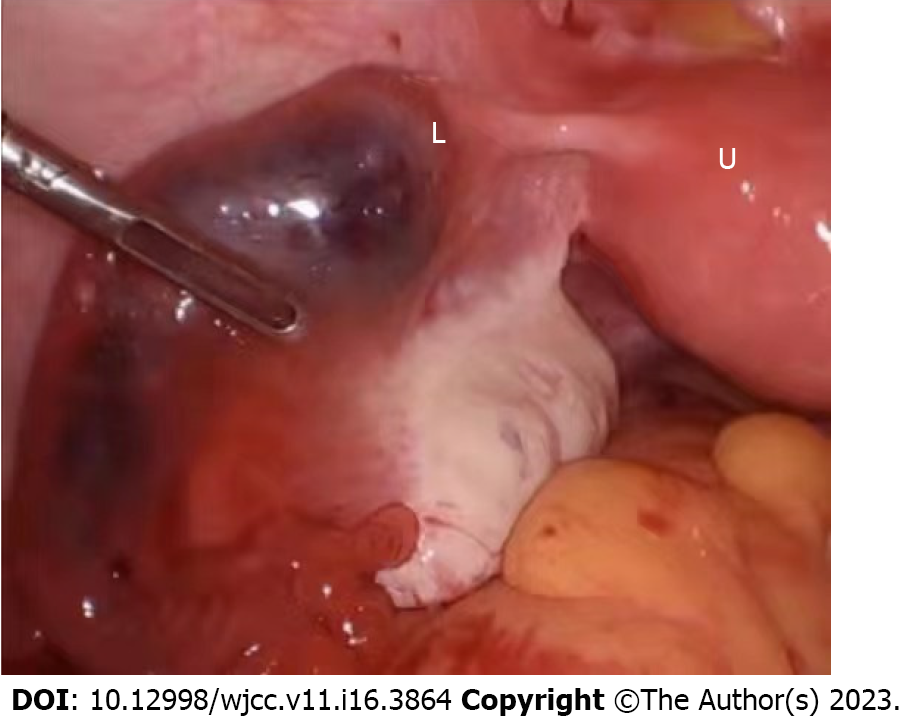
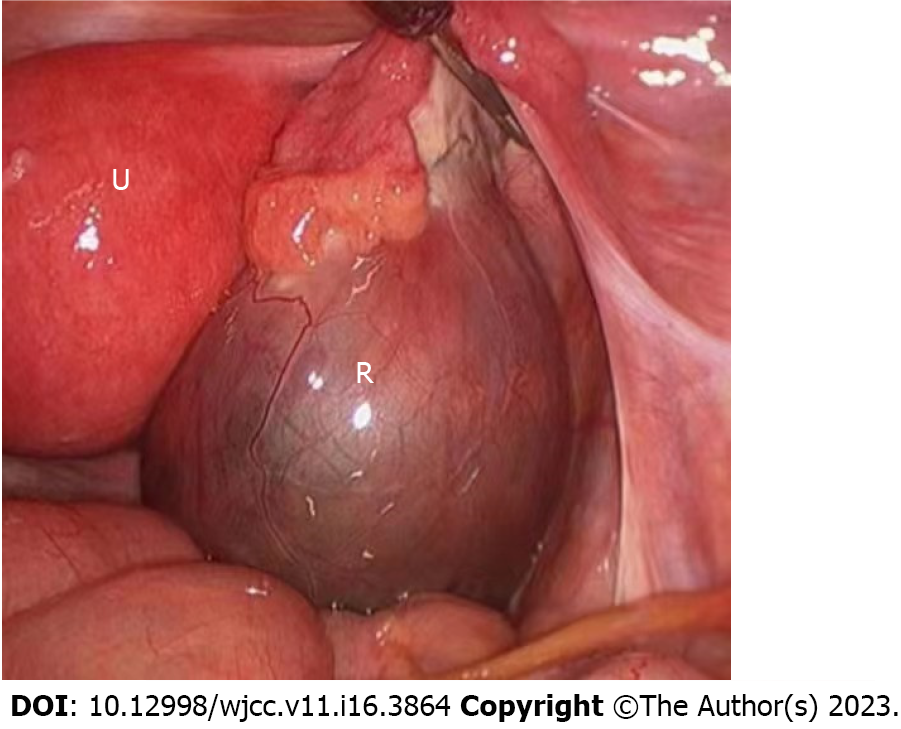
The patient was treated with magnesium sulfate and progesterone for fetal preservation. A reexamination after 4 d revealed the left fallopian tube had an uneven echo mass of 9.2 cm × 5.7 cm and a right ovarian mass of 11.6 cm × 7.1 cm. Close monitoring of the patient was essential considering the abnormal tumor markers, rapidly growing ectopic pregnancy in case of spontaneous rupture, and the possibility of the ovarian mass being malignant, all of which may affect the prognosis of a pregnant woman. After counseling the patient and her relatives, the decision to perform a laparoscopic exploration was taken. Intraoperatively, the uterus was enlarged, the left fallopian tube was enlarged by approximately 5 cm × 8 cm (Figure 2), and a right ovarian cystic mass of approximately 12 cm × 7 cm was recorded (Figure 3). The left ovary and right oviduct were both normal. The patient underwent left salpingectomy for the removal of ectopic pregnancy and the intrauterine pregnancy was preserved. A large theca lutein cyst was found on the right ovary during the procedure and resection was not performed as a means of avoiding a decrease in progesterone, which could have potentially led to intra-abdominal pregnancy abortion. Pathology following the left salpingectomy confirmed tubal pregnancy. The patient developed severe pain in the right lower quadrant 1 wk after surgery, and torsion of the right ovarian cyst pedicle was not excluded. Rather than opting for a second laparotomy for ovarian cystectomy, the patient underwent right ovarian cyst fluid aspiration via the abdomen under ultrasound guidance, and 300 mL yellow liquid was aspirated. The pain of the patient was relieved as a result.
From a combination of the medical history of the patient, the physical examination, and related examinations, the final medical diagnosis was determined as left tubal pregnancy complicated by a giant theca lutein right ovarian cyst and intrauterine pregnancy.
Three weeks after the operation, the patient was generally in good condition and was recovering well. There was no complaint of discomfort and she was discharged. The gestation age upon discharge was 12 wk 3 d, the fetus was visible, and the size of the right ovarian cyst had been reduced.
The patient has since successfully delivered a baby.
The clinical symptoms of an ectopic pregnancy are identical to those of an intrauterine pregnancy before rupture, but if the ectopic pregnancy ruptures, the presentation is similar to that of a simple ectopic pregnancy. However, without typical acute abdominal symptoms, the presentation may potentially be limited to vaginal bleeding and mild abdominal pain, and this is often misdiagnosed as preterm abortion, which results in treatment delay. Serum β-human chorionic gonadotropin (HCG) is one of the main tools for ectopic pregnancy diagnosis, but the time of multiplication of HCG in intrauterine pregnancy together with ectopic pregnancy is not significantly different to that of intrauterine pregnancy alone, particularly after the second trimester, which lacks diagnostic significance. Ultrasound has a certain amount of value for diagnosing this disease[3]. In this case, a mixed echogenic mass was observed outside the uterus, so ultrasound should not neglect the examination of the fetus during intrauterine pregnancy, particularly in the bilateral adnexal area, so the potential to miss the combined ectopic pregnancy can be avoided. The most common ovarian tumor type that is found during pregnancy is benign teratoma, which is generally detected before pregnancy and shows as a high-density signal on ultrasound. They are generally cystic or solid with indistinct borders, and often combined with a large amount of ascites and elevated carbohydrate antigen 125 and human epididymis protein 4, so a full evaluation of the clinical situation is required to facilitate the diagnosis and differentiation of theca lutein ovarian cysts during pregnancy[4]. Theca lutein ovarian cysts are physiological ovarian cysts and hormone-related cysts and they, can spontaneously disappear if the hormonal stimulation disappears. They also have the characteristic of self-generation[5]. Therefore, surgery is not recommended for theca lutein ovarian cyst during pregnancy, but if the ovarian cysts are twisted or have severe bleeding which leads to ovarian rupture or shock, or if ovarian enlargement results in obstructed labor, surgery is recommended, particularly if malignant tumors are highly suspected[6,7]. However, it is recommended that patients with ovarian cysts in combination with pregnancy be treated conservatively, but if a tumor is suspected, early detection and elective surgery should be performed as a means of excluding potential malignant tumors or benign tumors with complications such as torsion of the ovarian cyst that could have a negative impact on pregnancy outcome.
Following the diagnosis of heterotopic pregnancy, treatment plan choice should be based on a combination of factors, including the number of weeks of pregnancy or whether the patient wishes to keep the intrauterine pregnancy. For patients who wish to continue intrauterine pregnancy, laparoscopic technique is considered a safe and effective treatment method that, serves as a replacement for traditional open surgery due to its advantages of early diagnosis and treatment, less injury, faster recovery time, fewer postoperative complications, and less interference with intrauterine pregnancy[8]. However, during laparoscopic salpingectomy or salpingostomy, uterine irritation is inevitable, and this can lead to intrauterine miscarriage. At the same time, there is the possibility of some products of conception remaining with salpingotomy, which can lead to persistent ectopic pregnancy. In addition, patients who are treated with salpingectomy have a lower clinical pregnancy rate than those who are treated with salpingostomy or managed expectantly[9]. Patients and their families must be made fully aware of these risks. In this case, the patient firmly requested fetal preservation. As a means of ensuring intrauterine pregnancy continuation and the complete removal of the extra uterine pregnancy, operation time was minimized and uterus stimulation was minimal. A low transverse incision close to the base of the uterus was chosen for opening the abdomen to ensure mechanical stimulation of the uterus was reduced while exposing the adnexa[10]. Intraoperative mechanical stimulation of the uterus and destruction of the corpus luteum of pregnancy should be minimized to the greatest possible extent. Postoperative pain is also known cause of miscarriage, so postoperative analgesics can be given to pregnant women, in addition to magnesium sulfate, as a means of inhibiting contractions and progesterone, which can help prevent miscarriage. Therefore, for heterotopic pregnancy that is complicated by a giant ovarian cyst, individualized treatment based on the fertility requirements of the patient is recommended. If the intrauterine embryo is well developed, laparoscopic surgery is feasible for the removal of the affected fallopian tube and preservation of the intrauterine embryo, enabling the intrauterine pregnancy to continue. Normal pregnancy with ovarian flavin cysts can be diagnosed based on clinical manifestations in combination with ultrasound examination. If complications such as ovarian torsion do not occur, they can be observed until 6 mo after the end of pregnancy, when most will spontaneously disappear. If ovarian torsion occurs and surgery is necessary, conservative surgery can be performed in order to minimize ovarian damage and to ensure the pregnancy continues before full term[11]. In this reported case, theca lutein ovarian cyst with pedicle torsion could not be ruled out by ultrasound, but guided needle ovarian cyst aspiration could be performed on the patient to relieve symptoms. The key factors for treating this disease are early diagnosis, early treatment and correct differential diagnosis of various ovarian tumors. This can help prevent ectopic pregnancy mass rupture, hemorrhage, or ovarian tumor torsion, which can lead to tissue ischemia and necrosis, resulting in serious risk to the life of the pregnant woman and intrauterine embryo. Attention should be paid, to damage during surgery, avoiding affecting uterine and ovarian blood circulation, avoiding unnecessary surgical interventions following surgery, and cooperating with drug therapy, which can improve the success rate of a continued pregnancy.
The approach patients with heterotopic pregnancy and a giant ovarian cyst should be individualized based on their fertility requirements. We recommend the following: (1) If the patient has satisfied parity and has no fertility requirements, laparoscopic salpingectomy should be performed and the giant ovarian cyst and intrauterine pregnancy removed; (2) If the patient has the fertility requirement of wanting to have more children in the future, laparoscopic salpingectomy or salpingostomy can be performed to preserve the intrauterine pregnancy. Serial ovarian cyst aspiration can be performed under ultrasound and resection can be performed after delivery; and (3) Heterotopic pregnancy should be diagnosed early by active surveillance during antenatal visits using ultrasound to avoid any catastrophic complications.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Naem AA, Germany; Tolunay HE, Turkey S-Editor: Li L L-Editor: Filipodia P-Editor: Li L
| 1. | Wang X, Ma D, Zhang Y, Chen Y, Liu Z, Bi X, Wu X, Fan J. Rare heterotopic pregnancy after frozen embryo transfer: a case report and literature review. BMC Pregnancy Childbirth. 2020;20:542. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Reece EA, Petrie RH, Sirmans MF, Finster M, Todd WD. Combined intrauterine and extrauterine gestations: a review. Am J Obstet Gynecol. 1983;146:323-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 184] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 3. | Bromley B, Benacerraf B. Adnexal masses during pregnancy: accuracy of sonographic diagnosis and outcome. J Ultrasound Med. 1997;16:447-52; quiz 453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 81] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Timor-Tritsch LE, Lerner JP, Monteagudo A, Santos R. Transvaginal ultrasonographic characterization of ovarian masses by means of color flow-directed Doppler measurements and a morphologic scoring system. Am J Obstet Gynecol. 1993;168:909-913. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 82] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Ghezzi F, Cromi A, Fasola M, Bolis P. One-trocar salpingectomy for the treatment of tubal pregnancy: a 'marionette-like' technique. BJOG. 2005;112:1417-1419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 80] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Goh W, Bohrer J, Zalud I. Management of the adnexal mass in pregnancy. Curr Opin Obstet Gynecol. 2014;26:49-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Koay EJ, Teh BS, Paulino AC, Butler EB. A Surveillance, Epidemiology, and End Results analysis of small cell carcinoma of the bladder: epidemiology, prognostic variables, and treatment trends. Cancer. 2011;117:5325-5333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 73] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 8. | Yang C, Wang H, Zou Y, Cui W, Yang J, Li T, Li C, Jiang J. Hyperreactio luteinalis after delivery: a case report and literature review. Int J Clin Exp Med. 2015;8:6346-6348. [PubMed] |
| 9. | Török P, Naem A, Csehely S, Chiantera V, Sleiman Z, Laganà AS. Reproductive outcomes after expectant and surgical management for tubal pregnancy: a retrospective study. Minim Invasive Ther Allied Technol. 2023;1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Soper NJ. SAGES' guidelines for diagnosis, treatment, and use of laparoscopy for surgical problems during pregnancy. Surg Endosc. 2011;25:3477-3478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Sakae C, Sato Y, Taga A, Satake Y, Emoto I, Maruyama S, Kim T. Ultrasound-guided percutaneous aspiration of hyperreactio luteinalis avoids laparoscopic untwisting of ovarian torsion. Ultrasound Obstet Gynecol. 2015;46:243-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |