Published online Jun 6, 2023. doi: 10.12998/wjcc.v11.i16.3858
Peer-review started: February 20, 2023
First decision: March 24, 2023
Revised: April 3, 2023
Accepted: May 6, 2023
Article in press: May 6, 2023
Published online: June 6, 2023
Processing time: 102 Days and 7.9 Hours
Purpura annularis telangiectodes of Majocchi (PATM), also known as Majocchi, is a rare subclass of pigmented purpuric dermatoses. The etiology of PATM is unknown, but it seems more common in children and young women. The skin lesions are mostly symmetrical ring-shaped reddish-brown macules on the lower limbs.
A 9-year-old girl, who has received treated in our department, presented with reddish-brown ring-shaped rash on both lower limbs that had been present for 6 mo. These lesions, red brownish annular or petaloid patches, were mostly found on ankles and lower limber, which do not fade when adding pressure and no feel of infiltration and no atrophy when touching those lesions. Pathological examination showed deposition of hemosiderin in papillary dermis. However, dermoscopy showed the pigmentation in the center as well as the lavender patches on the edge of lesion. The child was thus diagnosed with PATM. After diagnosis, we suggested the patient avoid strenuous exercise. she was given vitamin C tablets for oral and mometasone furoate cream for external use. Follow-up examinations and treatment continue to support the clinical diagnosis to date.
This is the first report of investigating PATM using dermoscopy, which can differentiate PATM from other diseases due to its unique microscopic feature under dermoscopy. Although PATM is harmless, it still requires long-term follow-up. Moreover, dermoscopy technique can be applied for observation of multi-site lesions and correlated with histopathology. Thus, we believe this approach could be generalized for future diagnosis of PATM.
Core Tip: Purpura annularis telangiectodes of Majocchi (PATM) also known as Majocchi's disease, is a rare subclass of pigmented purpuric dermatoses. The skin lesions are mostly symmetrical ring-shaped reddish-brown macules on the lower limbs. This disease is more commonly found among children and young women and the etiology is unknown. Currently, the diagnosis of PATM mainly depends on clinical and histopathological features. Dermoscopy, a non-invasive detection technique, could be a promising technique for future PATM diagnosis owing to its good correlation with histopathology, and multi-site observation.
- Citation: Pu YJ, Jiang HJ, Zhang L. Purpura annularis telangiectodes of Majocchi: A case report. World J Clin Cases 2023; 11(16): 3858-3863
- URL: https://www.wjgnet.com/2307-8960/full/v11/i16/3858.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i16.3858
Purpura annularis telangiectodes of Majocchi (PATM), also known as Majocchi disease, is a rare subclass of pigmented purpuric dermatoses (PPD). The etiology of PATM is unknown, but it seems more common among children and young women[1]. The skin lesions are mostly symmetrical ring-shaped reddish-brown macules on the lower limbs[2,3]. Thus, some researchers believe that gravity and venous hypertension may be the inducing factors of this disease[4]. The diagnosis of PATM usually depends mainly on the clinical findings and histopathological features. However, different sampling sites or time may affect the pathological diagnosis. Moreover, histopathological examination is an invasive method, which is not conducive to long-term follow-up. Dermoscopy, a non-invasive detection method, has a good corresponding relationship with histopathology and multi-site observation is more beneficial to diagnose the disease. Herein, we applied the dermoscopy to observe a girl who suffered from PATM.
A 9-year-old girl admitted to Kunming Children’s Hospital, Kunming City, Yunnan Province, China in November 2021 due to the "repeated reddish-brown ring-shaped rash on both lower limbs for 6 mo".
In the beginning, the lesions were erythematous, where most of them are annular patches, appear on both insteps and ankles. Subsequently, the lesions evolved to both ankles, with sporadic itches. It recurs after topical glucocorticoids. They spread to both legs, with occasional itching. No clinic symptoms of hematuresis, hematocheiza, joint pain or hypodynamia observed during this period of time.
The patient had no history of systemic symptoms, allergies and no specific history of past illness.
Normal.
Physical examination revealed good general condition. Dermatological examination results showed that these lesions are red brownish annular or petaloid patches with various size, 1-3 cm in diameters can be observed on both insteps, ankles and lower limber. And they do not fade when adding pressure. During this process, light brownish pigmentation can be observed central of these macules. No feel of infiltration and no atrophy when touching those lesions. Such lesions on instep are shown in Figure 1.
Blood routine, urine routine, liver function, kidney function, antinuclear antibody, coagulation function and erythrocyte sedimentation rate tests were normal.
Dermoscopy showed a large number of reticular or honeycomb pigmentation in the center of the lesion, and lavender patches and a few focally distributed punctate blood vessels were seen on the edge of lesion (Figure 2).
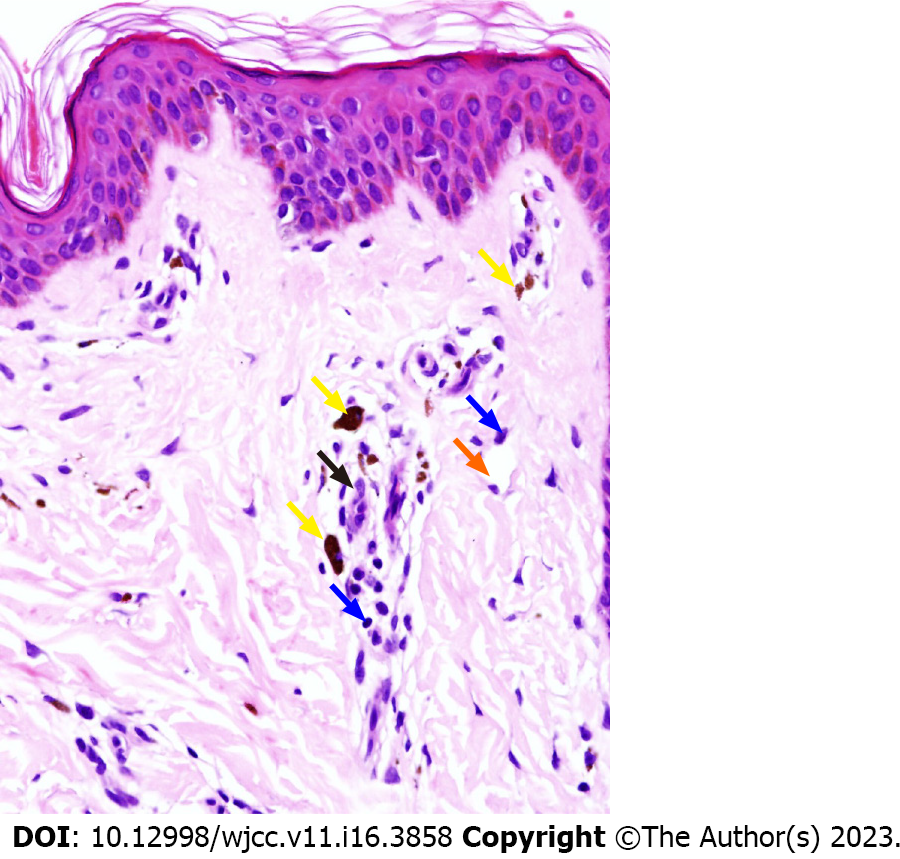
Pathological examination showed scattered vacuolar endothelial cells, infiltration of lymphocytes and histocytes around blood vessels, and deposition of hemosiderin in papillary dermis (Figure 3).
Combining with relevant examinations, the patient was diagnosed as PATM.
The patient was given orally dipyridamole tablets 25 mg/bid, vitamin C tablets 0.1 g/bid, and topical mometasone furoate cream and mucopolysaccharide polysulfonate cream bid for external use.
The patient was given orally vitamin C tablets 0.1 g/bid, and topical mometasone furoate cream for external use. We suggested that the girl avoid prolonged stand, as well as strenuous exercises. The skin lesions subsided after 2 wk of treatment. In December 2022, the patient's disease recurred again after intense exercise, and the lesions gradually subsided one month after external medication. Follow-up is ongoing.
In this case, dermoscopy data showed a large number of reticular or honeycomb-shaped pigmentations in the center of the lesion, some lavender patches, and a few focally distributed punctate blood vessels at the edge of the lesion. These structures are often observed in lichen sclerosus and pigmented purpuric dermatosis[5]. The purplish red patches under dermoscopy correspond to red blood cell overflow in the histopathological picture, while the pigmentation corresponds to hemosiderin deposition. It is well known that overflowing red blood cells are engulfed to form hemosiderin[1], and pigmentation is the final form of purplish-red patches. The histopathology results for the early rash of PATM shows swollen vascular endothelial cells in the upper dermis and dermal papilla, with a large number of lymphocytes and histiocytes around the lumen, extravasation of red blood cells, and occasional neutrophil infiltration. However, the inflammatory infiltration of old lesions is not as obvious as in the early stages, with reduction in extravasation of red blood cells, and deposition of hemosiderin. Although the pathological manifestations of this patient were consistent with those of old lesions, the active margin could be clearly observed under dermoscopy.
Differentiating PATM from lichen aureus (LA) and purpuric mycosis fungoides (PMF) could be challenging. LA is another subtype of PPD while PMF is a cutaneous lymphoma with purpuric eruptions as the clinical manifestation[6,7]. PATM and LA can be differentiated by the distribution pattern of pigments and purplish red patches using dermoscopy. PATM shows a ring-like distribution, while LA shows a diffuse distribution[8]. Neither of them has a special vessel structure under dermoscopy, but PMF has its unique vessels such as spermatozoa-like vessels[9]. Therefore, the differences between PATM, LA and PMF on dermoscopy are clear. In addition, we could distinguish the three diseases.
Due to the detection of epidermotropism or monoclonality in inflammatory infiltrates, other hypotheses believed that PPDs represent a type of T lymphocyte, occult and metaepithelial change[10]. There are even some described cases of progression to mycosis fungoides[11,12]. To sum up, although PATM is harmless, cutaneous T-cell lymphoma needs to be ruled out in some cases[2,11,12]. Thus, long-term follow-up of PATM is necessary.
PATM, a rare subclass of PPD, also known as Majocchi's disease. The skin lesions are mostly symmetrical ring-shaped reddish-brown macules on the lower limbs and more commonly found among children and young women. The purplish red patches under dermoscopy correspond to red blood cell overflow in the histopathological picture, while the pigmentation corresponds to hemosiderin deposition. Overflowing red blood cells are engulfed to form hemosiderin. Pigmentation is the final form of purplish-red patches. According to the histopathology results, the early rash of PATM shows swollen vascular endothelial cells in the upper dermis and dermal papilla, with a large number of lymphocytes and histiocytes around the lumen, extravasation of red blood cells, and occasional neutrophil infiltration. However, the inflammatory infiltration of old lesions is not as obvious as in the early stages, with reduction in extravasation of red blood cells, and deposition of hemosiderin. Although the pathological manifestations of this patient were consistent with those of old lesions, the active margin could be clearly observed under dermoscopy. It is challenging to differentiate PATM from LA and PMF but dermoscopy enables us to visualize the special vascular structure and pigment distribution pattern and distinguish these three diseases. Although PATM is harmless, the disease is prone to relapse and may resemble the early clinical feature of T-cell lymphoma. Thus, long-term follow-up of PATM is crucial. As a non-invasive detection method, Dermoscopy enables us multi-site observation and to correlates the obtained images with histopathology, which could be a promising approach for future PATM.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Exbrayat JM, France; Nazzaro G, Italy S-Editor: Li L L-Editor: A P-Editor: Li L
| 1. | Spigariolo CB, Giacalone S, Nazzaro G. Pigmented Purpuric Dermatoses: A Complete Narrative Review. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 2. | Hoesly FJ, Huerter CJ, Shehan JM. Purpura annularis telangiectodes of Majocchi: case report and review of the literature. Int J Dermatol. 2009;48:1129-1133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Fathy H, Abdelgaber S. Treatment of pigmented purpuric dermatoses with narrow-band UVB: a report of six cases. J Eur Acad Dermatol Venereol. 2011;25:603-606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Mansur AT, Koç MK, Ramadan S. Purpura annularis telangiectodes of Majocchi: an atypical presentation. Eur J Dermatol. 2019;29:546-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Borghi A, Corazza M, Minghetti S, Toni G, Virgili A. Clinical and dermoscopic changes of vulvar lichen sclerosus after topical corticosteroid treatment. J Dermatol. 2016;43:1078-1082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Kaufman AE, Patel K, Goyal K, O'Leary D, Rubin N, Pearson D, Bohjanen K, Goyal A. Mycosis fungoides: developments in incidence, treatment and survival. J Eur Acad Dermatol Venereol. 2020;34:2288-2294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 7. | Hanna S, Walsh N, D'Intino Y, Langley RG. Mycosis fungoides presenting as pigmented purpuric dermatitis. Pediatr Dermatol. 2006;23:350-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Portela PS, Melo DF, Ormiga P, Oliveira FJ, Freitas NC, Bastos Júnior CS. Dermoscopy of lichen aureus. An Bras Dermatol. 2013;88:253-255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Nasimi M, Bonabiyan M, Lajevardi V, Azizpour A, Nejat A, Dasdar S, Kianfar N. Pigmented purpuric dermatoses vs purpuric mycosis fungoides: Clinicopathologic similarities and new insights into dermoscopic features. Australas J Dermatol. 2022;63:81-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 10. | Georgala S, Katoulis AC, Symeonidou S, Georgala C, Vayopoulos G. Persistent pigmented purpuric eruption associated with mycosis fungoides: a case report and review of the literature. J Eur Acad Dermatol Venereol. 2001;15:62-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 33] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Guitart J, Magro C. Cutaneous T-cell lymphoid dyscrasia: a unifying term for idiopathic chronic dermatoses with persistent T-cell clones. Arch Dermatol. 2007;143:921-932. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 58] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Viseux V, Schoenlaub P, Cnudde F, Le Roux P, Leroy JP, Plantin P. Pigmented purpuric dermatitis preceding the diagnosis of mycosis fungoides by 24 years. Dermatology. 2003;207:331-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |