Published online Jun 6, 2023. doi: 10.12998/wjcc.v11.i16.3852
Peer-review started: February 16, 2023
First decision: April 19, 2023
Revised: April 20, 2023
Accepted: May 6, 2023
Article in press: May 6, 2023
Published online: June 6, 2023
Processing time: 106 Days and 8.7 Hours
We report a case of ruptured ovarian teratoma mimicking pelvic inflammatory disease (PID) and ovarian malignancy. The case indicates the need for reviewing the information on ovarian teratomas, as the symptoms are vague, and, therefore, diagnosis and treatment had to be structured accordingly.
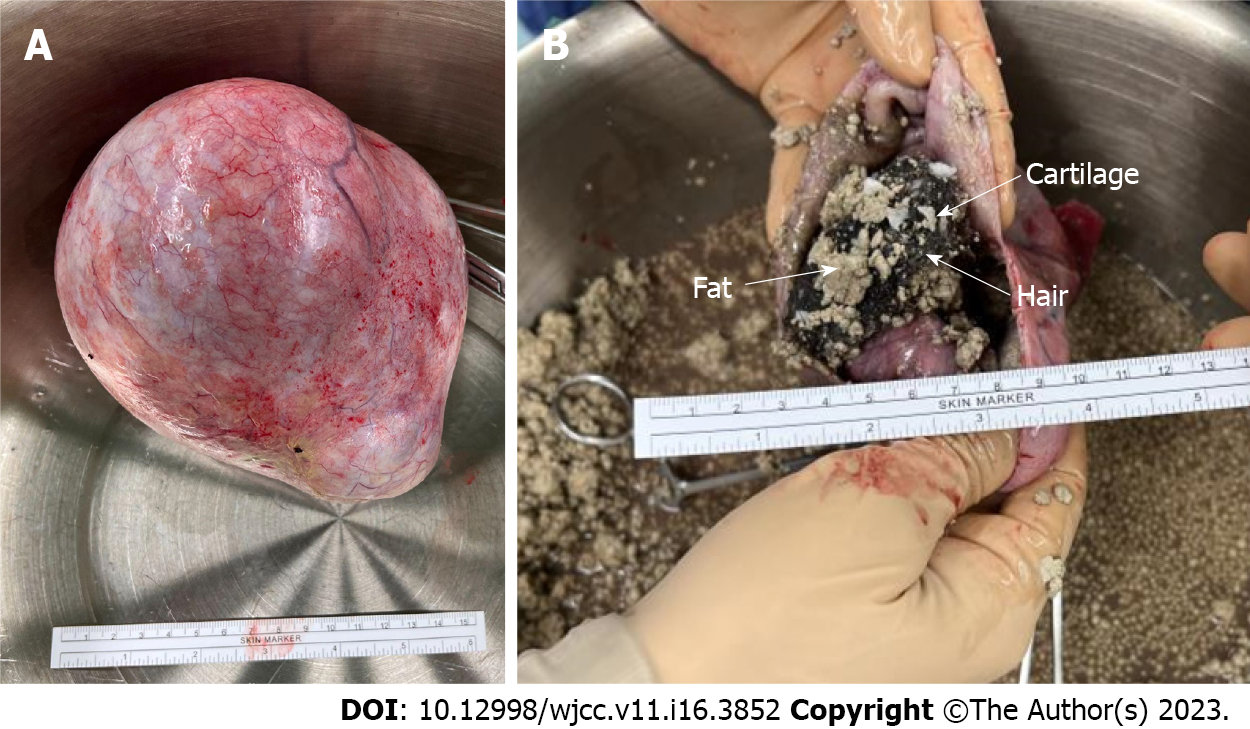
A 60-year-old woman was admitted to the emergency department with acute lower abdominal pain. She experienced weight loss and increased abdominal girth. Pelvic ultrasound and computed tomography revealed a 14-cm pelvic tumor. Laboratory examination revealed leukocytosis (white blood cell count: 12620/μL, segment: 87.7%) and high levels of C-reactive protein (18.2 mg/dL). Elevated levels of the tumor marker cancer antigen 19-9 (367.8 U/mL, normal value < 35 U/mL) were also noted. Due to the impression of a ruptured tubo-ovarian abscess or a tumor with malignancy, she immediately underwent an exploratory laparotomy. A ruptured ovarian tumor with fat balls, hair strands, cartilage, and yellowish fluid was observed on the right side. Right salpingo-oophorectomy was performed. A pathological examination revealed a mature cystic teratoma. The patient recovered after surgery and was discharged on post-operative day three. No antibiotics were administered.
This case illustrates the differential diagnosis of an ovarian tumor. Therefore, surgery is the mainstay for treating a ruptured teratoma.
Core Tip: We report a case of a ruptured ovarian teratoma mimicking pelvic inflammatory disease and malignancy. We updated the information on ovarian teratomas regarding symptoms, signs, diagnosis, and treatment. Because of the vague symptoms of ovarian teratoma, we provided a strategy to diagnose and treat this ovarian teratoma.
- Citation: Lai PH, Ding DC. Ruptured teratoma mimicking a pelvic inflammatory disease and ovarian malignancy: A case report. World J Clin Cases 2023; 11(16): 3852-3857
- URL: https://www.wjgnet.com/2307-8960/full/v11/i16/3852.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i16.3852
Mature cystic teratoma of the ovary constitutes 10%–20% of ovarian tumors[1]. Another report in Taiwan showed that the incidence of teratomas was 33%[2]. The most common symptom of teratomas is abdominal pain, which was observed in 48% of cases[2]. Other complications included torsion (9.2%), concurrent pregnancy (3.5%), and malignant transformation (0.7%)[2]. Abdominal pain is also a possible symptom following a ruptured teratoma[3].
We report a case of a 60-year-old woman with ruptured teratoma mimicking pelvic inflammatory disease (PID) and ovarian malignancy that was managed via an emergent right salpingo-oophorectomy (RSO).
A 60-year-old woman presented with aggravated abdominal pain and was admitted to the emergency department.
According to the patient’s statement, she had suffered from general abdominal bloating and distension since August 2022. Since October 2022, the discomfort had developed into non-remitting dull pain, accompanied by occasional stabbing pain in the right lower quadrant. The pain, initially eased by over-the-counter analgesics, progressed to become intolerable, and she could barely walk and sleep for days. She also suffered from lower urinary tract symptoms characterized by obstructive etiology, including intermittent urinary flow, hesitancy, need for straining, incomplete emptying, and frequency. Her body weight had decreased substantially from 59 kg in August to 54 kg at the time of recording, while the abdominal circumference increased. No fever or unstable vital signs were noted.
Her body mass index was 22.2 kg/m2 without remarkable gynecologic disorders or chronic illness. Menopause onset was at 54 years. Sexual activity and use of exogenous hormones were both ruled out.
Personal and family history was unremarkable.
A detailed physical examination revealed diffuse abdominal tenderness and equivocal rebound tenderness. An ovoid enlarged abdominal surface with a protruding mass on the right was observed.
The blood test yielded leukocytosis with left shift (white blood cell count: 12620/μL, segment: 87.7%) and a high C-reactive protein level (CRP 18.2 mg/dL), indicating an active systemic inflammatory status. The levels of tumor markers, including cancer antigen 125 (17.6 U/mL) and carcinoembryonic antigen (0.8 ng/mL), were within the normal ranges; however, cancer antigen 19-9 (CA 19-9 367.8 U/mL, normal value < 35 U/mL) was elevated. Post-operative cultures of the abdominal contents collected during surgery showed no microbial growth.
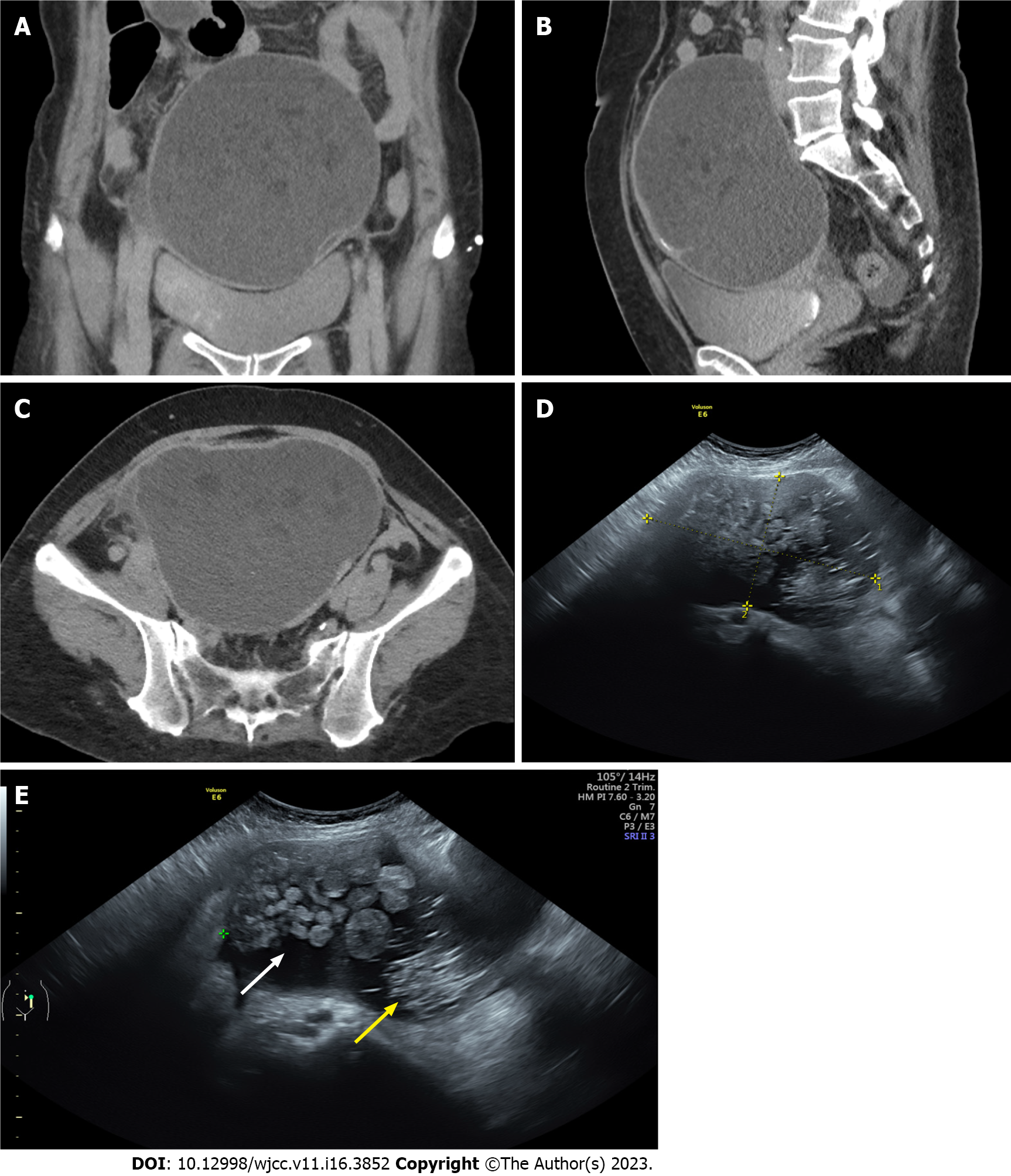
Contrast-enhanced computed tomography revealed a 14-cm cystic tumor occupying the pelvic cavity and lower abdomen (Figure 1A-C). The tumor probably originated from the adnexa, contained a few septations, had a mixed density of fluid and fat components, and lacked an enhancing mural nodule. Bilateral hydronephrosis might be a consequence of the compression effect of the tumor. Notably, a small amount of mildly turbid ascites was observed in the cul-de-sac. Based on the imaging findings, tubo-ovarian abscess was the primary impression, while ovarian torsion, ovarian tumor of either benign or malignant nature, or pyometra required differentiation. The computed tomography (CT) findings were echoed by the transabdominal ultrasound images, revealing a heterogeneous tumor with hyperechoic hair strand-like materials and papillary growth, which mimicked ovarian cancer (Figure 1D and E).
Due to absence of any sexual history, a diagnosis of the tubo-ovarian abscess was less likely. Considering the rapid growth of the tumor and the prominent symptoms, an exploratory laparotomy was performed the following day under the suspicion of adnexal malignancy.
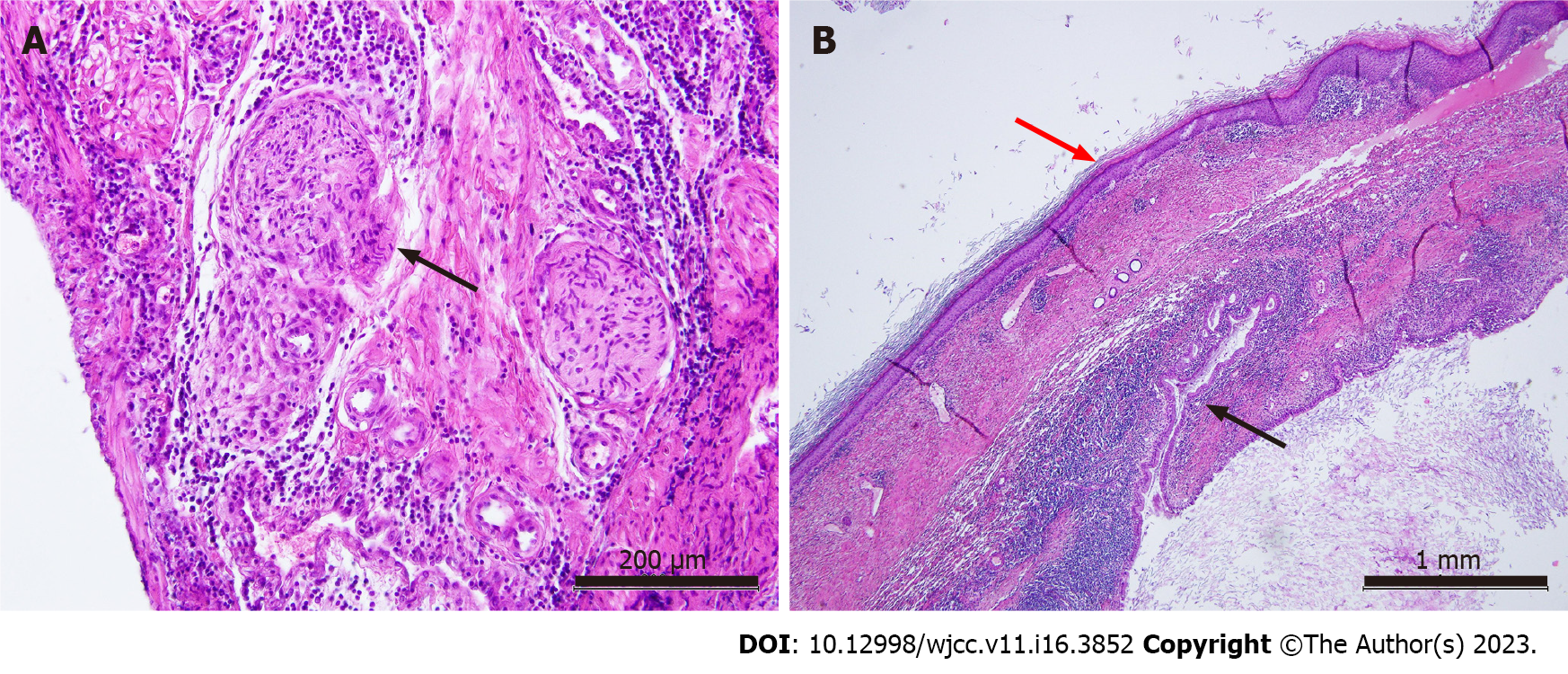
A right ovarian tumor with yellowish fluid accumulation and without a malodorous smell was found in the peritoneal cavity. Aerobic and anaerobic cultures were performed. RSO was performed. Grossly, the tumor contained hair strands, ball-like fat tissues, and cartilage within the tumor (Figure 2). Intraoperative frozen sections showed a teratoma. The histopathological study of paraffin-embedded tissue was found to be a mature cystic teratoma (Figure 3). As was expected, the diagnosis was revised to a mature cystic teratoma complicated with chemical peritonitis, which contributed to severe abdominal pain and inflammatory status.
After surgery, no antibiotics were administered for non-infectious pathogenesis. The surgical drain at the cul-de-sac drained only minimal serosanguinous fluid; therefore, it was removed. The patient recovered soon after the procedure and was discharged on postoperative day three. Follow-up at the outpatient department could have been more uneventful.
We report a case of a ruptured teratoma managed via emergent RSO. The presurgical impression of this teratoma mimicked pelvic inflammatory disease and ovarian malignancy. Peritoneal signs, leukocytosis, and left shift showed a high likelihood of PID. A complex tumor ultrasound and high CA 19-9 Levels led to the suspicion of ovarian malignancy. Finally, the teratoma was managed by RSO.
Diffuse abdominal pain, leukocytosis, and elevated CRP levels may be caused by a ruptured ovarian teratoma[3]. Other teratoma complications include torsion, infection, rupture, and malignant transformation[4]. The evaluated case also presented these symptoms and signs.
Spontaneous rupture of teratomas can occur, but are rare, due to thick cystic walls, with the possibility of occurrence ranging between 0.3%-0.7%. The cause of teratoma rupture is unknown. Torsion with infarction, direct trauma, prolonged pressure during pregnancy, malignant trans
Ultrasonography is an easy and effective tool for diagnosing ovarian teratomas[7]. The characteristics of ultrasound findings include dermoid mesh, tip of the iceberg sign, and Rokitansky nodule. Dermoid mesh indicates hyperechogenic lines reflecting that of hair[8]. Rokitansky nodule is a cystic lesion with echogenic tubercles projecting into the cystic lumen. To differentiate between benign and malignant tumors, the typical morphology for ovarian malignancy includes intratumor separation, papillary projection, vascular support to the lesion, heterogeneous echogenicity, and an ovarian volume of more than 20 cm3[9]. In the presented case, ultrasound showed a heterogeneous tumor with hyperechoic hair strand-like materials and papillary growth.
A teratoma, a heterogeneous adnexal mass with calcification and fatty components, can be noted on a CT scan[3]. Ruptured teratoma can be suspected when a CT scan shows a fatty nodule on the lesion and ascites with a peritoneal thickening layer[3]. The CT scan of ovarian cancer may show the size, location, and extent of primary ovarian carcinoma[10]. Ovarian cancer can show a cystic lesion with a portion of a solid tumor within it and may have a papillary projection[11]. The CT scan of the presented case showed a heterogeneous tumor with hyperechoic hair strand-like materials and papillary growth. Papillary growth may be similar to ovarian malignancy.
Teratomas are usually located in the ovaries. However, teratomas can occur anywhere in the body. Eight to fifteen percent of teratomas can occur bilaterally[12]. Multiple teratomas on the same side can also occur[13]. The most commonly observed side of teratoma occurrence varies in different studies[14].
Surgical treatment for ovarian teratomas includes cystectomy and oophorectomy[15]. Laparoscopic management is the gold standard. For young adults, cystectomy can be performed[16]. Ovarian teratoma can occur in pregnant women. For suspected malignancy or postmenopausal women, an oophorectomy could be performed[15]. When doing cystectomy, content spillage and possible chemical peritonitis may be encountered. However, this event can decrease complications through rigorous fluid flushing[16]. The presented case underwent an oophorectomy due to the suspicion of malignancy and to avoid content spillage. The choice of surgical method can be considered individually.
This report illustrates one case. The results of this report may not be applicable to another case of ruptured teratoma. Therefore, these results should be interpreted with caution.
We report a rare case of a ruptured teratoma causing symptoms, such as pelvic inflammatory disease and ovarian malignancy. Ultrasound and CT scan images cannot differentiate the actual tumor characteristics. After surgical exploration, a ruptured teratoma was diagnosed. This case illustrates the differential diagnosis of an ovarian tumor. Surgery is the mainstay for treating a ruptured teratoma.
We thank Dr. Ming-Hsun Li for his assistance with the pathological pictures.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Exbrayat JM, France; Martín Del Olmo JC, Spain S-Editor: Li L L-Editor: A P-Editor: Li L
| 1. | Prueksaritanond N, Mahiphun K, Insin P. Incidence and Associated Risk Factors of Patients with Malignant Transformation Arising in Mature Cystic Teratoma of the Ovary in Rajavithi Hospital. Asian Pac J Cancer Prev.. 2020;5:179-185. |
| 2. | Wu RT, Torng PL, Chang DY, Chen CK, Chen RJ, Lin MC, Huang SC. Mature cystic teratoma of the ovary: a clinicopathologic study of 283 cases. Zhonghua Yi Xue Za Zhi (Taipei). 1996;58:269-274. [PubMed] |
| 3. | El Moussaoui M, Médart L, Goffin F. Ruptured Teratoma and Chemical Peritonitis. J Belg Soc Radiol. 2019;103:8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Bužinskienė D, Mongirdas M, Mikėnas S, Drąsutienė G, Andreika L, Sakalauskaitė I. Chemical peritonitis resulting from spontaneous rupture of a mature ovarian cystic teratoma: a case report. Acta Med Litu. 2019;26:217-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Tanaka Y, Hori H, Gorai I. Chemical peritonitis caused by an iatrogenic rupture of mature cystic teratoma of the ovary during labor: a report of a case didactic to all the maternity health care workers. J Matern Fetal Neonatal Med. 2011;24:388-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (1)] |
| 6. | Eisman LE, Stull C, Barmat LI. Prolonged Chemical Peritonitis Following Intraperitoneal Rupture of a Dermoid Cyst. J Gynecol Surg. 2017;33:68-70. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Sahin H, Abdullazade S, Sanci M. Mature cystic teratoma of the ovary: a cutting edge overview on imaging features. Insights Imaging. 2017;8:227-241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 57] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 8. | Li X, Zhu D, Lv LI, Yu J. An uncommon recurrence of an immature teratoma: A case report. Oncol Lett. 2016;11:2453-2456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Jung SI. Ultrasonography of ovarian masses using a pattern recognition approach. Ultrasonography. 2015;34:173-182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Sahdev A. CT in ovarian cancer staging: how to review and report with emphasis on abdominal and pelvic disease for surgical planning. Cancer Imaging. 2016;16:19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 11. | Jung SE, Lee JM, Rha SE, Byun JY, Jung JI, Hahn ST. CT and MR imaging of ovarian tumors with emphasis on differential diagnosis. Radiographics. 2002;22:1305-1325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 349] [Cited by in RCA: 265] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 12. | de la Blanca EP, Fernandez-Perez MF, Martin-Diaz EDM, Lozano M, Garcia-Sanchez M, Monedero C. Ultrasound-guided Ex-vivo Retrieval of Mature Oocytes for Fertility Preservation During Laparoscopic Oophorectomy: A Case Report. J Reprod Infertil. 2018;19:174-181. [PubMed] |
| 13. | Fayez I, Khreisat B, Athamneh T, Omoosh R, Daibes MA. Multiple Bilateral Ovarian Mature Cystic Teratomas with Ovarian Torsion: A Case Report. Oman Med J. 2018;33:163-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Rathore R, Sharma S, Agarwal S. Malignant transformation in mature cystic teratoma of the ovary: a retrospective study of eight cases and review of literature. Prz Menopauzalny. 2018;17:63-68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Sinha A, Ewies AA. Ovarian Mature Cystic Teratoma: Challenges of Surgical Management. Obstet Gynecol Int. 2016;2016:2390178. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 16. | Ding DC, Chen SS. Conservative laparoscopic management of ovarian teratoma torsion in a young woman. J Chin Med Assoc. 2005;68:37-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |