Published online Jun 6, 2023. doi: 10.12998/wjcc.v11.i16.3802
First decision: January 30, 2023
Revised: February 19, 2023
Accepted: April 19, 2023
Article in press: April 19, 2023
Published online: June 6, 2023
Processing time: 173 Days and 8.5 Hours
The coaxial radiography-guided puncture technique (CR-PT) is a novel technique for endoscopic lumbar discectomy. As the X-ray beam and the puncturing needle are maintained in a parallel and coaxial direction, the X-ray beam can be used to guide the trajectory angle, facilitating the choice of the puncture site and providing real-time guidance. This puncture technique offers numerous advan
To confirm whether CR-PT is a superior approach to percutaneous transforaminal endoscopic lumbar discectomy compared to AP-PT.
In this parallel, controlled, randomized clinical trial, herniated lumbar disc patients appointed to receive percutaneous endoscopic lumbar discectomy treatment were recruited from the Pain Management Department of the Affiliated Hospital of Xuzhou Medical University and Nantong Hospital of Traditional Chinese Medicine. Sixty-five participants were enrolled and divided into either a CR-PT group or an AP-PT group. The CR-PT group underwent CR-PT, and the AP-PT group underwent AP-PT. The number of fluoroscopies during puncturing, puncture duration (min), surgery duration (min), VAS score during puncturing, and puncture success rate were recorded.
Sixty-five participants were included, with 31 participants in the CR-PT group and 34 in the AP-PT group. One participant in the AP-PT group dropped out due to unsuccessful puncturing. The number of fluoroscopies [median (P25, P75)] was 12 (11, 14) in the CR-PT group vs 16 (12, 23) in the AP-PT group, while the puncture duration (mean ± SD) was 20.42 ± 5.78 vs 25.06 ± 5.46, respectively. The VAS score was 3 (2, 4) in the CR-PT group vs 3 (3, 4) in the AP-PT group. Further subgroup analysis was performed, considering only the participants with L5/S1 segment herniation: 9 patients underwent CR-PT, and 9 underwent AP-PT. The number of fluoroscopies was 11.56 ± 0.88 vs 25.22 ± 5.33; the puncture duration was 13.89 ± 1.45 vs 28.89 ± 3.76; the surgery duration was 105 (99.5, 120) vs 149 (125, 157.5); and the VAS score was 2.11 ± 0.93 vs 3.89 ± 0.6, respectively. All the above outcomes demonstrated statistical significance (P < 0.05), favoring the CR-PT treatment.
CR-PT is a novel and effective technique. As opposed to conventional AP-PT, this technique significantly improves puncture accuracy, shortens puncture time and operation time, and reduces pain intensity during puncturing.
Core Tip: Puncturing is the first step for percutaneous endoscopic lumbar discectomy. Compared with the anterior-posterior and lateral radiography-guided puncture technique (AP-PT), the coaxial radiography-guided puncture technique (CR-PT) has the advantage of guiding the trajectory angle, facilitating the choice of the puncture site, and also providing real-time guidance for puncturing. This study aimed to compare the two techniques. In this randomized controlled trial, the CR-PT technique demonstrated significantly better puncture accuracy, and shorter puncturing and operation duration. We argue that the CR-PT technique is an advisable option in percutaneous endoscopic lumbar discectomy, especially for unusual cases.
- Citation: Chen LP, Wen BS, Xu H, Lu Z, Yan LJ, Deng H, Fu HB, Yuan HJ, Hu PP. Coaxial radiography guided puncture technique for percutaneous transforaminal endoscopic lumbar discectomy: A randomized control trial. World J Clin Cases 2023; 11(16): 3802-3812
- URL: https://www.wjgnet.com/2307-8960/full/v11/i16/3802.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i16.3802
Percutaneous endoscopic lumbar discectomy (PELD) is a promising treatment for herniated lumbar disc (HLD). Its advantages over conventional surgery include less intraoperative bleeding, minimal para-spinal muscle injury, high clinical efficacy, and rapid functional recovery. Therefore, PELD has become a popular surgical method[1-8]. Furthermore, in PELD surgery, only a tiny part of the bone tissue is removed, which does not compromise spinal stability[9,10].
Despite its numerous advantages, PELD is technically challenging and has a steep learning curve[11,12]. Accurate puncturing and working channel intubation are required to create favorable conditions for endoscopic surgery[13,14]. However, the puncture technique is relatively difficult, especially in percutaneous transforaminal endoscopic lumbar discectomy (PTELD), which requires specific puncture angles to certain parts of the intervertebral foramen. In addition, for a L5/S1 segment HLD case with a hypertrophied L5 transverse process and articular process, high iliac crest, and narrowed intervertebral foramen, the puncturing is more difficult[15,16].
Conventionally, intermittent anteroposterior and lateral radiography is used for accurate puncturing. However, this process relies on the surgeon’s experience to determine and adjust the trajectory angle and depth of the needle. Occasionally, an inappropriate puncture angle leads to failure of the endoscopic surgery[17,18]. Repeated puncturing results in a prolonged operation and increased exposure to radiation[19,20]. Moreover, repeated puncturing increases the patient’s pain perception.
This paper describes a novel coaxial radiography-guided puncture technique (CR-PT) that we developed in our clinical practice. This technique focuses on maintaining the X-ray beam and the puncturing needle in a parallel and coaxial direction[21,22]. With the coaxial technique, the X-ray beam can be used to facilitate puncture site selection and guide the trajectory angle while providing real-time guidance. We hypothesized that this new technique reduces the difficulty of the puncture process, reduces the number of Xray fluoroscopies, shortens the puncture duration, and increases the puncture accuracy. Therefore, the new puncture technique was compared with the conventional anterior-posterior and lateral radiography-guided puncture technique (AP-PT) in order to confirm its superiority.
This is a parallel, controlled, single-blinded, randomized clinical trial. The participants were recruited from the Pain Management Department of the Affiliated Hospital of Xuzhou Medical University and Nantong Hospital of Traditional Chinese Medicine and were assigned to two parallel groups: CR-PT group and AP-PT group. The CR-PT group underwent CR-PT, and the AP-PT group underwent AP-PT. This study complied with The Declaration of Helsinki, and the trial was approved by the Institutional Ethics Committee of Clinical Research of Nantong Hospital of Traditional Chinese Medicine. The clinical trial was registered on the Chinese Clinical Trial Registry website (Registration number ChiCTR2200058894) and written informed consent was obtained from all the participants. No external funding was available for the trial.
Inclusion criterion: HLD patients appointed to receive PELD treatment.
Exclusion criteria: Patients with verbal communication disorders; patients with mental disorders; patients who underwent percutaneous inter-laminar endoscopic lumbar discectomy.
One researcher was in charge of the enrollment and allocation. The participants were allocated according to their year of birth. Participants with an odd-numbered birth year were assigned to the CR-PT group, while participants with an even-numbered birth year were assigned to the AP-PT Group. The participants were blinded to which group they were assigned.
Another researcher was assigned to evaluate the outcomes. The operations were performed by two surgeons in the two respective hospitals. They were not blinded to the allocation. Data processing and statistical analysis were performed by another researcher who was blinded to the allocation. The allocation method was revealed after the completion of the statistical analysis.
The primary outcomes included the number of fluoroscopies during puncturing and the puncture duration (min). The puncture duration was defined as the time taken from setting the operation position to the needle tip reaching the correct target. The secondary outcome was the surgery duration (min), which was defined as the time taken from setting the operation position to suturing. The VAS score during puncturing and the puncture success rate were also evaluated as secondary outcomes. Successful puncturing was defined as the needle tip reaching the correct target; otherwise, the puncture was deemed unsuccessful. The outcomes were recorded during and after the surgeries by a separate researcher.
The sample size was set based on the number of fluoroscopies. According to the previous literature, the effect size was set to be 4 and the standard deviation was set to be 4.6, with α = 0.05 and beta = 0.1. The sample size was 32 for each group. As no follow-up work was needed in the study, no dropout rate was considered. The sample size was calculated to be 64.
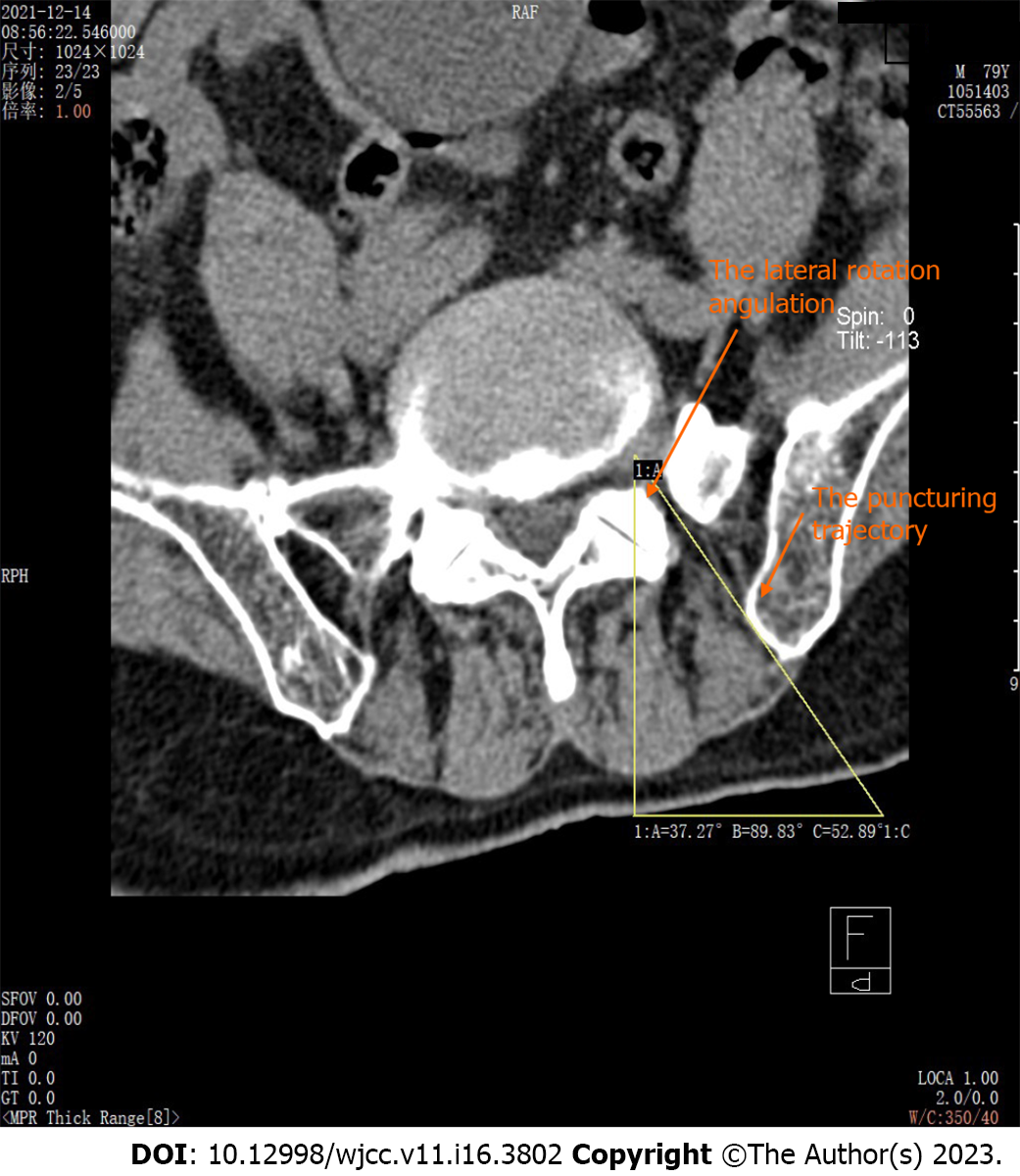
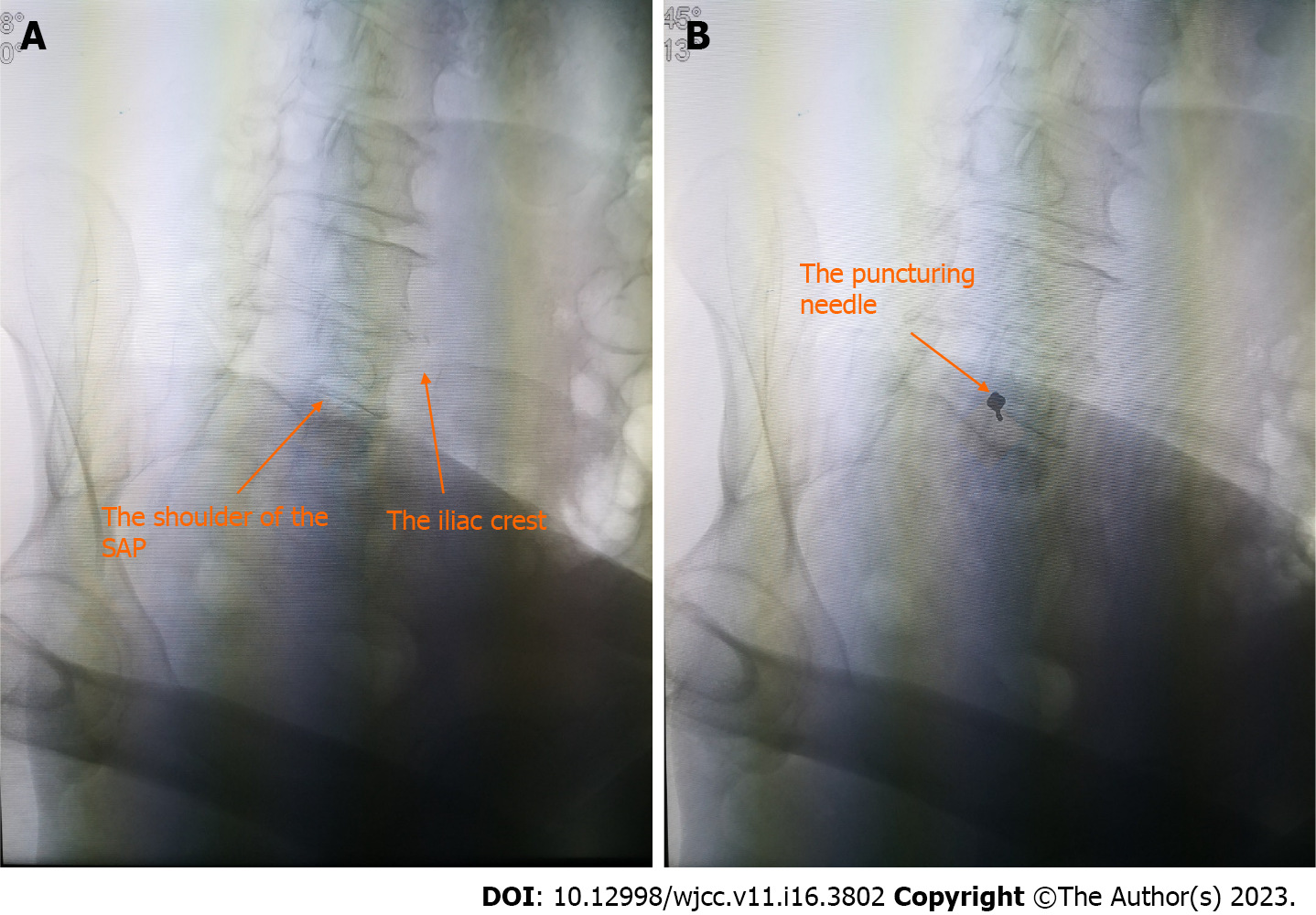
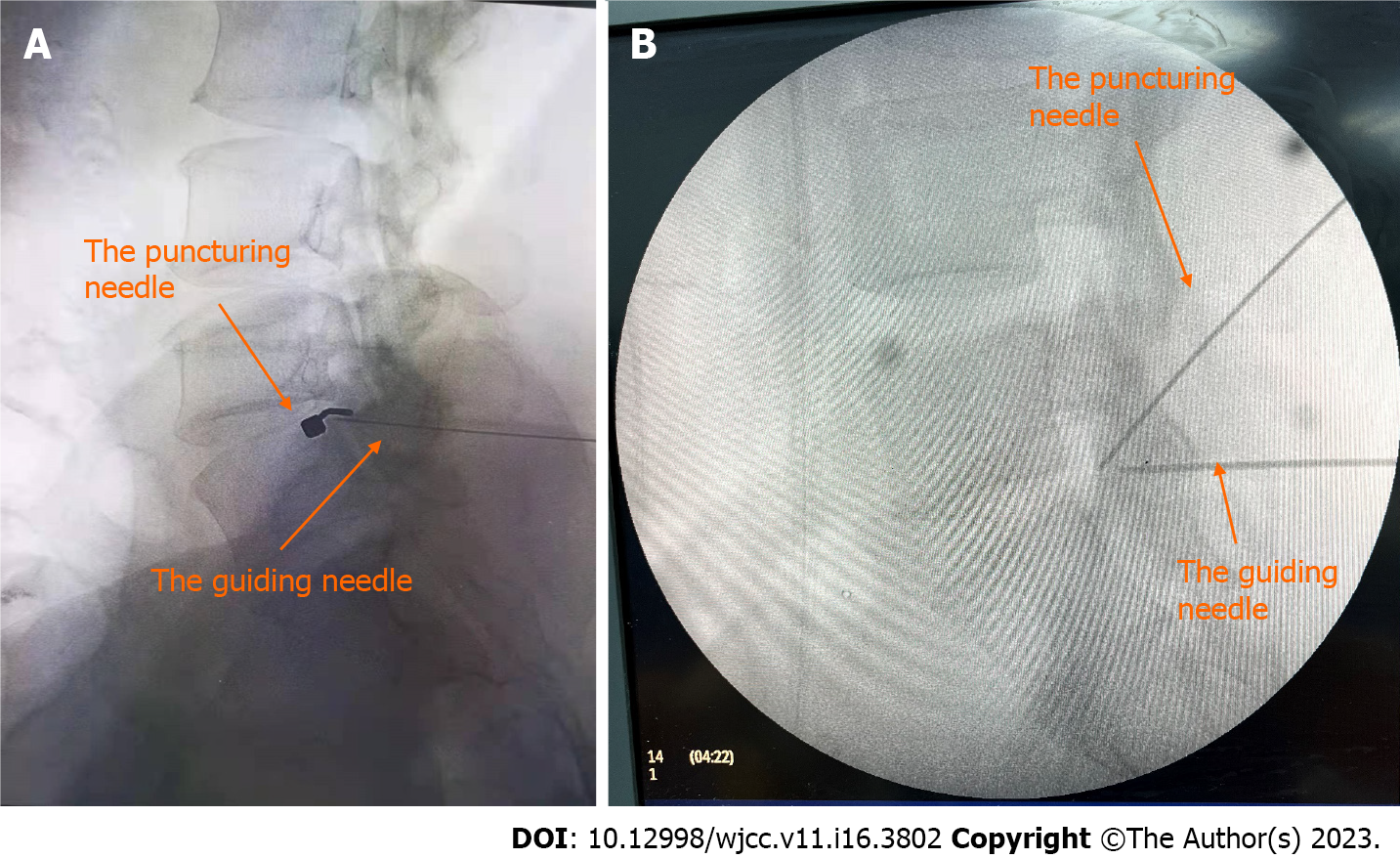
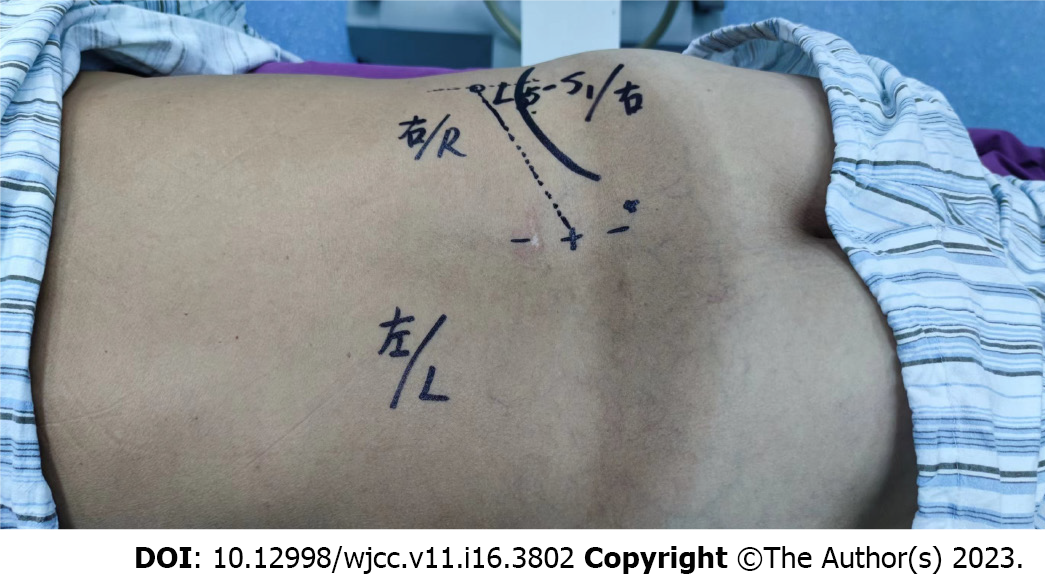
CR-PT procedure: MRI or CT was performed before surgery, and the proper lateral and cranial tilt angle of the trajectory was measured (Figure 1). The participant was placed in the prone position, and a cushion was placed under the abdomen to reduce lumbar lordosis. Then, the C-arm was tilted to the predetermined lateral and cranial oblique angulation, and the superior part of the lateral border of the superior articular process (SAP), also known as the shoulder of the SAP, was identified as the target. In some circumstances, some modifications were made to the target selection. In L5/S1 segment cases, if the intervertebral foramina and the SAP were obstructed by the iliac crest, the C-arm was tilted cranially and slightly medially until the intervertebral foramina and the SAP could be visualized. The radiopaque marker was then placed on the skin superimposing the target, which was marked, disinfected, and draped. Subsequently, the marked skin and subcutaneous tissues were anesthetized. A needle (17G, 15 cm) was inserted a short distance until it was seated in the subcutaneous tissues overlying the target, and the angle of the needle was adjusted until it was parallel to the X-ray axis. In this instance, the needle hub projected directly over the tip and was aligned with the target, as displayed in Figure 2. The needle was advanced while maintaining a parallel direction to the X-ray axis until contact with the shoulder of the SAP was made. Then, anteroposterior and lateral radiography was performed to confirm the needle placement.
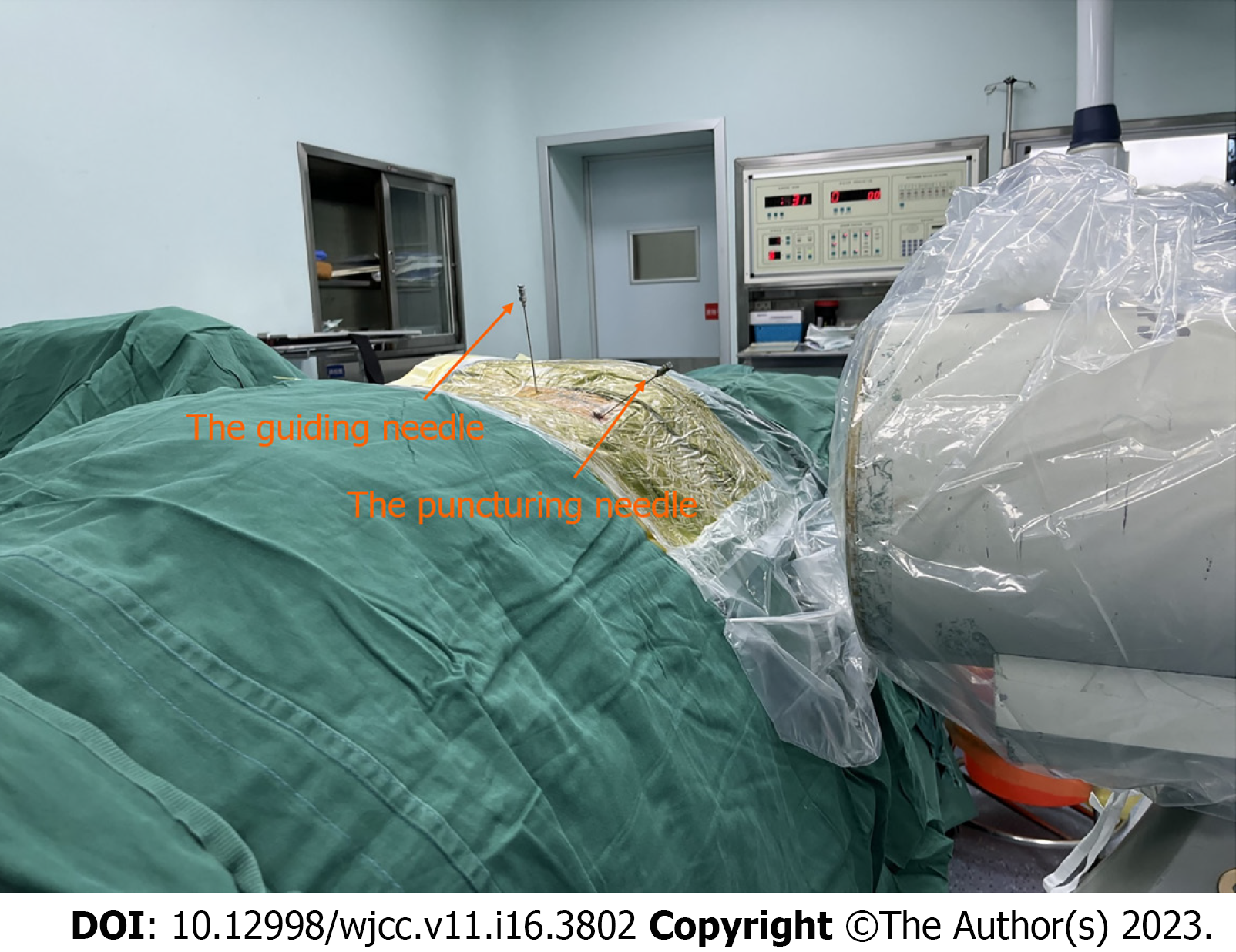
In some cases, the SAP could not be visualized clearly despite setting the C-arm to the predetermined angulation, and mild angulation adjustments were made to allow for proper visualization. This situation occurred when the lateral oblique angle of the C-arm was very large. In such cases, a guiding needle was utilized in addition to the puncturing needle (Figure 3).
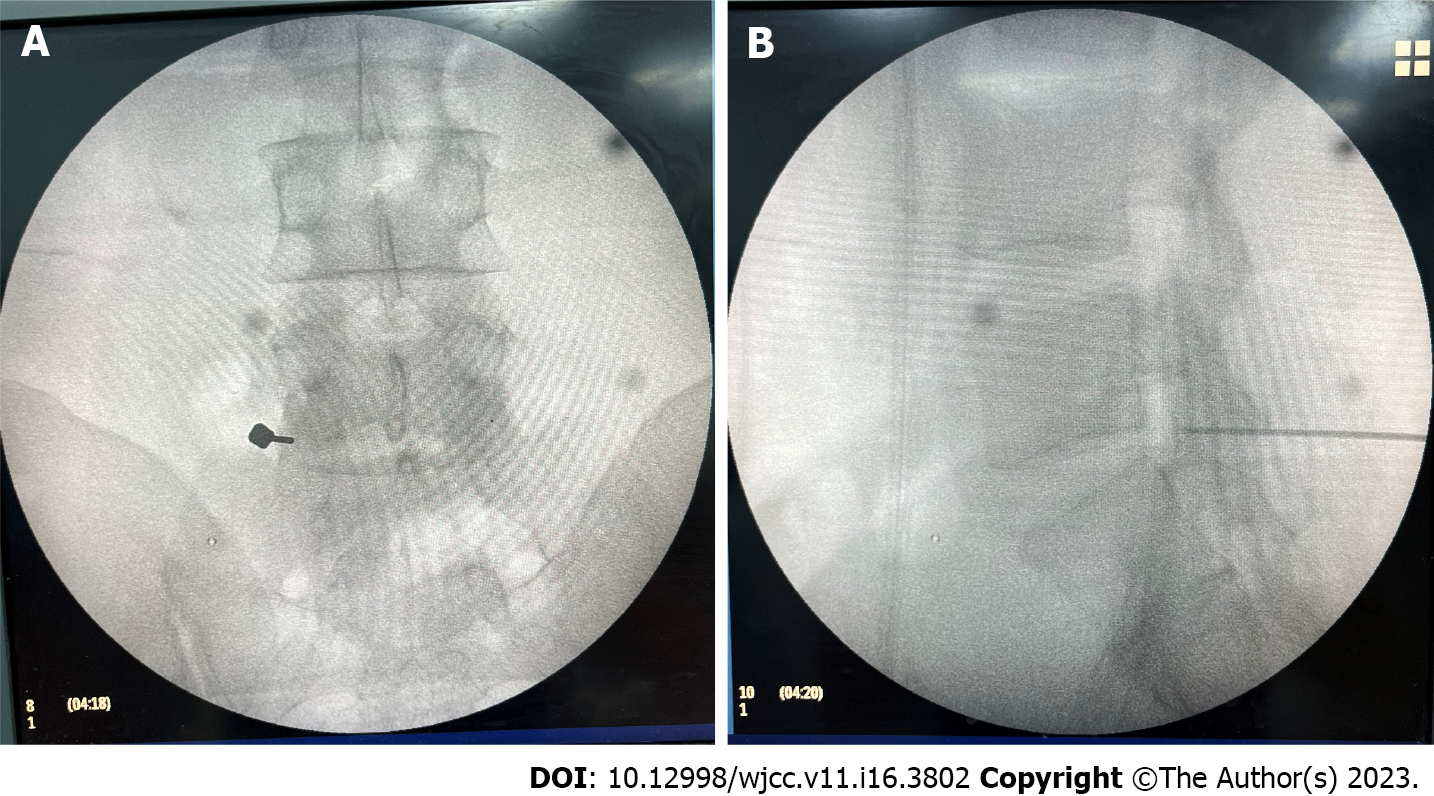
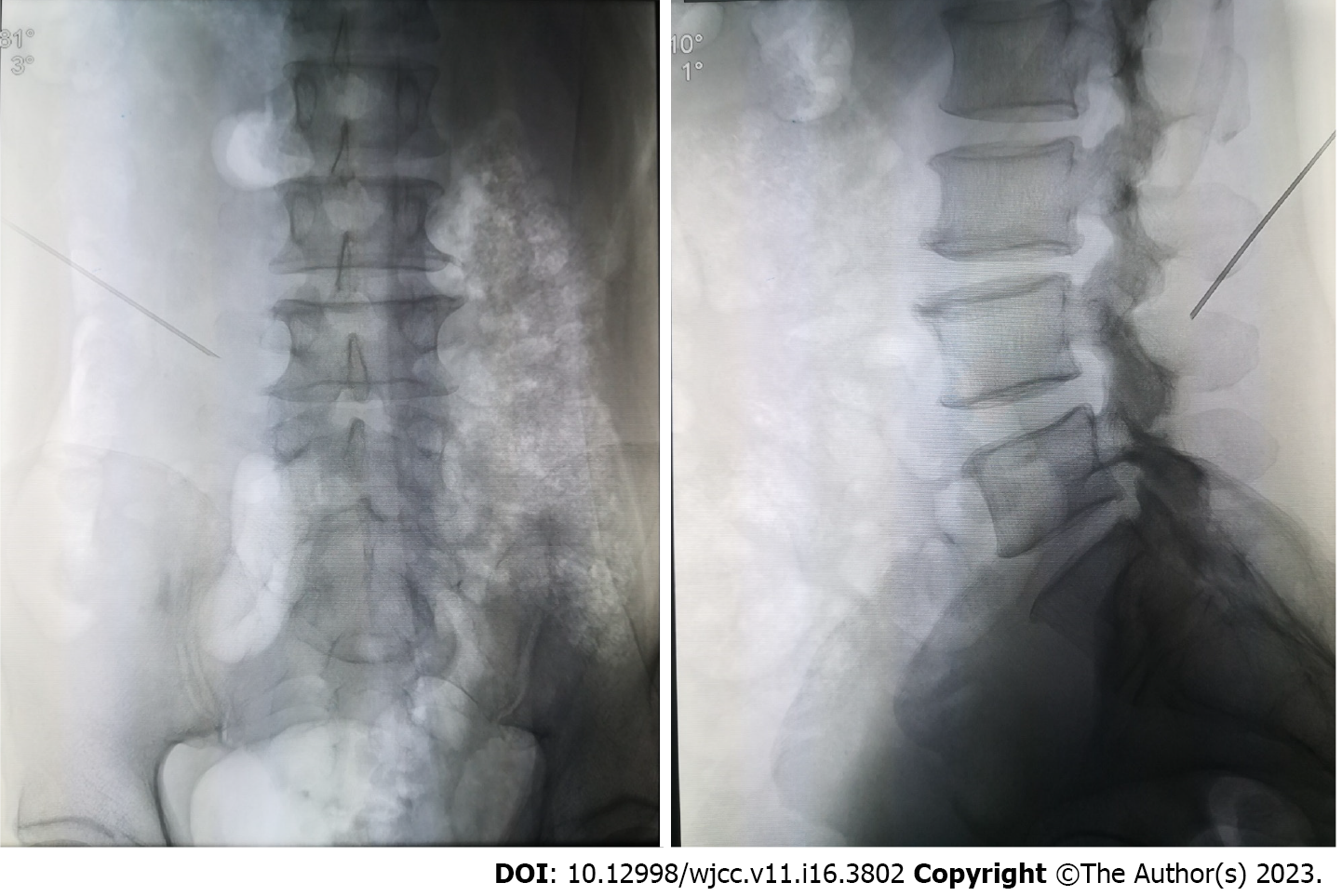
First, the radiopaque marker was placed and the skin was prepared for puncture as described above. The guiding needle (20G, 15 cm) was inserted sagittally under X-ray guidance until contact was made with the SAP, and the needle was repositioned and advanced slightly along the lateral border of the SAP. The needle was further advanced slightly to ensure that the needle tip was situated near the ventral margin of the SAP, and the anteroposterior and lateral view was taken to confirm the position (Figure 4). Then, the tip of the guiding needle was set as the puncturing target, and the coaxial technique was performed as described above (Figure 5).
The C-arm was set at the correct alignment to achieve a standard lumbar anteroposterior radiography. This process ensured that the X-ray beam was parallel to the disc and that the endplate was displayed as a straight line. Subsequently, the center longitudinal line of the lumbar spine and an oblique line passing through the shoulder of the SAP were marked. For the L5/S1 Lumbar disc, the oblique line should reach above the peak point of the iliac crest. Then, a longitudinal line parallel and 10-14 cm lateral to the center line was drawn. The intersection of the lateral longitudinal line and the oblique line was defined as the puncture point (Figure 6). After disinfection, draping, and anesthesia, a needle was inserted. During the procedure, anteroposterior and lateral views were taken every 1 cm of needle advancement, confirming that the needle was oriented to the shoulder of the SAP (Figure 7). Slight modifications in direction were performed as necessary. When the needle tip touched the SAP, anteroposterior and lateral radiographs were taken to confirm the needle position.
Quantitative variables with a normal distribution are presented as the mean ± SD, while non-normally distributed variables are reported as the median (P25, P75). An independent t-test was performed to analyze normally distributed data with homogeneity of variance. A separate variance estimated t-test was performed to analyze normally distributed data without homogeneity of variance. The remaining quantitative data were statistically analyzed by the Wilcoxon rank sum test. For qualitative variables, Fisher's exact test and Pearson chi-square test were applied. In this study, P < 0.05 was considered statistically significant. SPSS version 26 was utilized for statistical analyses. Moreover, a subgroup analysis of the patients with L5/S1 HLD was performed using the same statistical methodology.
In total, 86 participants were evaluated from April 2022 to May 2023, and 65 participants were enrolled in the trial. Among the enrolled participants, 16 were from the Nantong Hospital of Traditional Hospital, and 49 were from the Affiliated Hospital of Xuzhou Medical University. One participant in the AP-PT group dropped out due to AP-PT failure and eventually underwent CR-PT. Therefore, statistical analysis was performed for 64 participants, with 31 participants in the CR-PT group and 33 in the AP-PT group.
The demographic characteristics of the patients showed no statistically significant difference between the two groups, as displayed in Table 1.
| CR-PT group (31) | AP-PT group (34) | P value | |
| Sex (male:female) | 19:12 | 18:16 | 0.5 |
| Height (cm) | 168.29 ± 7.99 | 167.53 ± 8.18 | 0.71 |
| Weight (kg) | 66 (62, 75) | 69 (60, 80) | 0.17 |
| BMI (kg/cm2) | 25.3 (22.63, 28.04) | 27.25 (23.19, 33.35) | 0.15 |
| Age | 55 (41, 65) | 58 (38, 66) | 0.5 |
| Surgical segment | |||
| L1/L2 | 0 | 2 | 0.57 |
| L2/L3 | 1 | 0 | |
| L3/L4 | 1 | 3 | |
| L4/L5 | 20 | 19 | |
| L5/S1 | 9 | 10 | |
| Laterality (left:right) | 18:13 | 12:22 | 0.07 |
| Pain duration (mo) | 6 (1, 24) | 6 (2, 24) | 0.64 |
The number of fluoroscopies [median (P25, P75)] was 12 (11, 14) in the CR-PT group vs 16 (12, 23) in the AP-PT group, while the puncture duration (mean ± SD) was 20.42 ± 5.78 vs 25.06 ± 5.46, respectively. All the variables demonstrated statistically significant differences (P < 0.05), as displayed in Table 2.
| CR-PT group (31) | AP-PT group (33) | P value | |
| Number of fluoroscopies | 12 (11, 14) | 16 (12, 23) | 0.002 |
| Puncture duration | 20.42 ± 5.78 | 25.06 ± 5.46 | 0.002 |
| Surgery duration | 115 (107, 124) | 123 (92, 148.5) | 0.173 |
| VAS score during puncturing | 3 (2, 4) | 3 (3, 4) | 0.021 |
| Puncture success rate (34 participants included for AP-PT group) | 100% | 97.06% | 1 |
Furthermore, a subgroup analysis of the clinical outcomes was performed on the participants who underwent L5/S1 segment surgery. In total, 15 participants were included in the subgroup analysis, with 7 patients from the CR-PT subgroup and 8 from the AP-PT subgroup. The number of fluoroscopies was 11.56 ± 0.88 vs 25.22 ± 5.33, and the puncture duration was 13.89 ± 1.45 vs 28.89 ± 3.76, respectively. All the variables demonstrated statistically significant differences (P < 0.05), as displayed in Table 3.
| CR-PT subgroup (9) | AP-PT subgroup (9) | P value | |
| Number of fluoroscopies | 11.56 ± 0.88 | 25.22 ± 5.33 | 0 |
| Puncture duration | 13.89 ± 1.45 | 28.89 ± 3.76 | 0 |
| Surgery duration | 105 (99.5, 120) | 149 (125, 157.5) | 0 |
| VAS score during puncturing | 2.11 ± 0.93 | 3.89 ± 0.6 | 0 |
No complications were reported in the trial.
This clinical trial was carried out to compare the two puncturing techniques. The aim of the study was to confirm whether CR-PT is a superior approach to percutaneous transforaminal endoscopic lumbar discectomy compared to AP-PT. The number of fluoroscopies during puncturing, puncture duration, surgery duration, VAS score during puncturing, and puncture success rate were recorded.
One participant with L5/S1 segment HLD dropped out due to an unsuccessful AP-PT procedure. All the clinical outcomes demonstrated superiority with statistical significance favoring the CR-PT group except the surgery duration. Additionally, a subgroup analysis was performed, focusing on L5/S1 segment participants. All the clinical outcomes demonstrated statistically significant superiority in the CR-PT subgroup compared to the AP-PT subgroup. The superiority was more obvious in the subgroup analysis.
The superiority of CR-PT over AP-PT may be attributed to the following points. In the coaxial puncturing technique, the puncturing needle and X-ray beam share a common axis, which is easier to observe on radiography and allows for less needle repositioning. Additionally, as opposed to AP-PT, this novel puncturing technique does not require shifting the C-arm machine between the lateral position and the anteroposterior position repeatedly. The working cannula tilt angulation is crucial for PTELD, as it should be accurate and individualized. For example, a central-type disc herniation requires a larger lateral oblique angulation, whereas a small lateral oblique angulation is warranted in a foraminal type or far lateral type HLD case. Similarly, caudal hernia prolapses require a larger cranial tilt angulation, otherwise minor cranial tilt angulation is necessary. In the coaxial technique, the individualized puncturing angle and the individualized puncturing spot can be predetermined and guaranteed by setting the C-arm angulation beforehand. Hence, the angulation of the working cannula intubation can be optimized, which facilitates subsequent endoscopic surgery. However, for AP-PT, selecting the optimal puncture point and puncturing angulation depends on the surgeon’s expertise, which is much less accurate.
Our research demonstrated a more obvious superiority of CR-PT in HLD of the L5/S1 segment, which may be due to the following reasons. First, L5/S1 segments typically require a smaller lateral rotation angle, allowing easy visualization of the SAP. Therefore no guiding needle is required, which shortens puncturing time. Second, in the coaxial technique, the iliac crest is relatively easily avoided due to the more accurate angulation. Therefore, we believe that CR-PT is far more advantageous in L5/S1 cases.
Other innovative puncturing techniques have been reported for PELD. Zeng et al[14] reported a novel targeted puncture technique using a lumbar disc herniation target collimator, indicating superiority over the conventional free-hand injection method. Fan et al[23] applied a so-called HELLO system, which consisted of a self-made surface locator and a puncture-assisted device to guide the percutaneous puncturing process. The report also indicated improved puncturing accuracy and reduced fluoroscopic duration, as well as preoperative location duration. Moreover, C-arm navigation and 3D printing technologies have been applied in multiple studies. Qin et al[13] reported that using the C-arm navigation system could dramatically reduce the number of fluoroscopies and puncture attempts compared with the conventional method. Erken et al[24] reported the use of a collimation device to facilitate puncturing in PELD. However, all these methods require additional equipment and could increase the cost of the procedure. In contrast, our method requires no additional device and provides a more convenient and practical approach.
Nevertheless, the limitations of this study should be acknowledged. The sample size was small. Thus, further clinical research with a larger sample size is required. Second, the puncturing technique relies on personal expertise and surgeons have their personal preferences, and our result can only provide an alternative reference.
CR-PT in PTELD is a novel and effective technique. It enables individualized cranial and lateral tilt angulation during puncturing, accurate identification of the puncturing location, fewer needle direction adjustments, and no need for repeated C-arm angulation shifting. This technique significantly improves puncture accuracy, shortens puncture time and operation time, and reduces pain during puncturing. Therefore, CR-PT could be an advisable option in PTELD.
As a conventional puncture technique in endoscopic discectomy, anterior-posterior and lateral radiography-guided puncture technique (AP-PT) has limitations, such as repeated intermittent radiographs and inaccurate needle angulation. Although some innovative puncturing techniques have been reported, most of them require additional equipment. This paper describes an innovative coaxial radiography-guided puncture technique (CR-PT) and verifies its feasibility and superiority compared to the traditional AP-PT technique.
The coaxial radiography-guided puncture technique (CR-PT) is commonly applied in conventional procedures; however, we applied this technique in endoscopic lumbar discectomies. For some difficult cases, a guiding needle was used and the tip of the guiding needle was set as the target, which subsequently enabled the coaxial puncture technique to be performed.
The aim of the research was to verify the superiority of CR-PT over AP-PT in endoscopic lumbar discectomies.
This is an RCT trial. The participants were assigned to either a CR-PT group or an AP-PT group. The number of fluoroscopies during puncturing, puncture duration (min), surgery duration (min), VAS score during puncturing, and puncture success rate were recorded and compared.
The trial verified the superiority of CR-PT over AP-PT in terms of puncture duration, puncture accuracy, and VAS score during puncturing.
The CR-PT technique is a novel and effective technique. This technique significantly improves puncture accuracy and shortens puncture duration. Therefore, CR-PT could be an advisable option in endoscopic discectomy.
This study lays a foundation for further research on the CR-PT technique in trans-interlaminar endoscopic lumbar discectomies and endoscopic cervical discectomies.
Provenance and peer review: Invited article; Externally peer-reviewed.
Peer-review model: Single-blind
Peer review started: December 11, 2022
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bakır M, Turkey; Xu B, China S-Editor: Liu JH L-Editor: Wang TQ P-Editor: Wu RR
| 1. | Li Z, Zhang C, Chen W, Li S, Yu B, Zhao H, Shen J, Zhang J, Wang Y, Yu K. Percutaneous Endoscopic Transforaminal Discectomy versus Conventional Open Lumbar Discectomy for Upper Lumbar Disc Herniation: A Comparative Cohort Study. Biomed Res Int. 2020;2020:1852070. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 2. | Choi KC, Kim JS, Park CK. Percutaneous Endoscopic Lumbar Discectomy as an Alternative to Open Lumbar Microdiscectomy for Large Lumbar Disc Herniation. Pain Physician. 2016;19:E291-E300. [PubMed] |
| 3. | Li WS, Yan Q, Cong L. Comparison of Endoscopic Discectomy Versus Non-Endoscopic Discectomy for Symptomatic Lumbar Disc Herniation: A Systematic Review and Meta-Analysis. Global Spine J. 2022;12:1012-1026. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 33] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 4. | Perez-Roman RJ, Gaztanaga W, Lu VM, Wang MY. Endoscopic decompression for the treatment of lumbar spinal stenosis: an updated systematic review and meta-analysis. J Neurosurg Spine. 2022;36:549-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 28] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 5. | Qin R, Liu B, Hao J, Zhou P, Yao Y, Zhang F, Chen X. Percutaneous Endoscopic Lumbar Discectomy Versus Posterior Open Lumbar Microdiscectomy for the Treatment of Symptomatic Lumbar Disc Herniation: A Systemic Review and Meta-Analysis. World Neurosurg. 2018;120:352-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 74] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 6. | Pan M, Li Q, Li S, Mao H, Meng B, Zhou F, Yang H. Percutaneous Endoscopic Lumbar Discectomy: Indications and Complications. Pain Physician. 2020;23:49-56. [PubMed] |
| 7. | Gadjradj PS, Harhangi BS, Amelink J, van Susante J, Kamper S, van Tulder M, Peul WC, Vleggeert-Lankamp C, Rubinstein SM. Percutaneous Transforaminal Endoscopic Discectomy Versus Open Microdiscectomy for Lumbar Disc Herniation: A Systematic Review and Meta-analysis. Spine (Phila Pa 1976). 2021;46:538-549. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 88] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 8. | Kapetanakis S, Gkantsinikoudis N, Charitoudis G. Implementation of Percutaneous Transforaminal Endoscopic Discectomy in Competitive Elite Athletes With Lumbar Disc Herniation: Original Study and Review of the Literature. Am J Sports Med. 2021;49:3234-3241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Ahn Y, Lee SH, Park WM, Lee HY, Shin SW, Kang HY. Percutaneous endoscopic lumbar discectomy for recurrent disc herniation: surgical technique, outcome, and prognostic factors of 43 consecutive cases. Spine (Phila Pa 1976). 2004;29:E326-E332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 199] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 10. | Jarebi M, Awaf A, Lefranc M, Peltier J. A matched comparison of outcomes between percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for the treatment of lumbar disc herniation: a 2-year retrospective cohort study. Spine J. 2021;21:114-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 47] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 11. | Lee SG, Ahn Y. Transforaminal Endoscopic Lumbar Discectomy: Basic Concepts and Technical Keys to Clinical Success. Int J Spine Surg. 2021;15:S38-S46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 12. | Hsu HT, Chang SJ, Yang SS, Chai CL. Learning curve of full-endoscopic lumbar discectomy. Eur Spine J. 2013;22:727-733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 172] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 13. | Qin H, Deng L, Xu L, Mu Q, Luo X, Huang S, Wang M, Luo C, Huang C, Huang W. Puncture and localization for percutaneous endoscopic lumbar discectomy with C-arm navigation: a randomized controlled cadaver trial. Ann Transl Med. 2021;9:1730. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Zeng Y, Bao J, Su J, Tan P, Xie W, Huang Z, Xia H. Novel targeted puncture technique for percutaneous transforaminal endoscopic lumbar discectomy reduces X-ray exposure. Exp Ther Med. 2017;14:2960-2968. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Yan Y, Zhu M, Cao X, Zhang Y, Zhang X, Xu M, Zhang D. Different approaches to percutaneous endoscopic lumbar discectomy for L5/S1 lumbar disc herniation: a retrospective study. Br J Neurosurg. 2020;1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 1] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Choi KC, Park CK. Percutaneous Endoscopic Lumbar Discectomy for L5-S1 Disc Herniation: Consideration of the Relation between the Iliac Crest and L5-S1 Disc. Pain Physician. 2016;19:E301-E308. [PubMed] |
| 17. | Fan G, Gu X, Liu Y, Wu X, Zhang H, Gu G, Guan X, He S. Lower Learning Difficulty and Fluoroscopy Reduction of Transforaminal Percutaneous Endoscopic Lumbar Discectomy with an Accurate Preoperative Location Method. Pain Physician. 2016;19:E1123-E1134. [PubMed] |
| 18. | Zheng C, Li J, Zeng G, Ye W, Sun J, Hong J, Li C. Development of a Virtual Reality Preoperative Planning System for Postlateral Endoscopic Lumbar Discectomy Surgery and Its Clinical Application. World Neurosurg. 2019;123:e1-e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 19. | Mariscalco MW, Yamashita T, Steinmetz MP, Krishnaney AA, Lieberman IH, Mroz TE. Radiation exposure to the surgeon during open lumbar microdiscectomy and minimally invasive microdiscectomy: a prospective, controlled trial. Spine (Phila Pa 1976). 2011;36:255-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 84] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 20. | Ahn Y, Kim CH, Lee JH, Lee SH, Kim JS. Radiation exposure to the surgeon during percutaneous endoscopic lumbar discectomy: a prospective study. Spine (Phila Pa 1976). 2013;38:617-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 123] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 21. | Lavy C. Variations in selective nerve root block technique. Ann R Coll Surg Engl. 2015;97:245. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Ko S, Kwon J, Lee Y, Chae S, Choi W. Comparison of Pain-reducing Effect After Selective Nerve Root Block According to the Type of Lumbar Foraminal Stenosis. Clin Spine Surg. 2019;32:E60-E64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 23. | Fan G, Guan X, Zhang H, Wu X, Gu X, Gu G, Fan Y, He S. Significant Improvement of Puncture Accuracy and Fluoroscopy Reduction in Percutaneous Transforaminal Endoscopic Discectomy With Novel Lumbar Location System: Preliminary Report of Prospective Hello Study. Medicine (Baltimore). 2015;94:e2189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 24. | Erken HY, Yilmaz O. Collimation Reduces Radiation Exposure to the Surgeon in Endoscopic Spine Surgery: A Prospective Study. J Neurol Surg A Cent Eur Neurosurg. 2022;83:6-12. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |