Published online May 26, 2023. doi: 10.12998/wjcc.v11.i15.3631
Peer-review started: February 2, 2023
First decision: February 17, 2023
Revised: February 27, 2023
Accepted: March 23, 2023
Article in press: March 23, 2023
Published online: May 26, 2023
Processing time: 112 Days and 7 Hours
Hysteromyoma is not a rare tumor among pregnant women. During pregnancy, the symptoms caused by hysteromyoma can be improved through conservative treatment in most cases. However, in order to ensure the safety of mothers and children, surgeries are necessary in some special cases.
We report a case of pregnancy complicated with hysteromyoma red degeneration. The patient had peritonitis after sudden abdominal pain during the 20th week of pregnancy. Laparoscopic exploration suggested rupture and bleeding of hysteromyoma, which were improved after drainage and an anti-inflammatory treatment. A cesarean section was performed after full term. This case shows the complications of rupture after red degeneration of hysteromyoma during pregnancy.
We should be alert to rupture of hysteromyoma during pregnancy, and active laparoscopic exploration is essential to improve the prognosis of such patients.
Core Tip: We report a case of pregnancy complicated with rupture and bleeding of hysteromyoma and review the diagnosis and treatment strategies for acute abdominal conditions associated with hysteromyoma in pregnancy with a view to providing a reference for clinical practice.
- Citation: Xu Y, Shen X, Pan XY, Gao S. Acute abdomen caused by spontaneous rupture of degenerative hysteromyoma during pregnancy: A case report. World J Clin Cases 2023; 11(15): 3631-3636
- URL: https://www.wjgnet.com/2307-8960/full/v11/i15/3631.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i15.3631
The incidence of hysteromyoma combined with pregnancy accounts for 0.09%-3.9% of all patients with hysteromyoma[1], which often causes degeneration due to an insufficient blood supply, including vitreous change, cystic change, red change, calcification, sarcomatoid change, and so on[2]. Especially during pregnancy, red degeneration often develops in hysteromyoma due to rapid growth, and erythroid degeneration is a special form of myoma necrosis, which is more common in a single large intramural myoma, often occurring among pregnant or lactating patients[3,4]. Pain caused by degenerative uterine fibroids is the most common clinical symptom of women with uterine fibroids during pregnancy[3]. The symptoms caused by hysteromyoma degeneration can be improved through conservative treatments in most cases, while surgical treatments are rarely needed[5]. Here, we report a case of pregnancy with hysteromyoma complicated with rupture and bleeding. The diagnosis and treatment strategies for pregnancy complicated with hysteromyoma-related acute abdomen are also reviewed, with an aim to provide a reference for clinical practice.
A 25-year-old primipara in 20th week of gestation presented with acute abdominal pain and signs of acute abdomen.
The patient developed left upper quadrant pain at rest, which progressed to severe diffuse abdominal pain. On admission, she appeared pale and distressed, complaining about severe abdominal pain and vomiting several times.
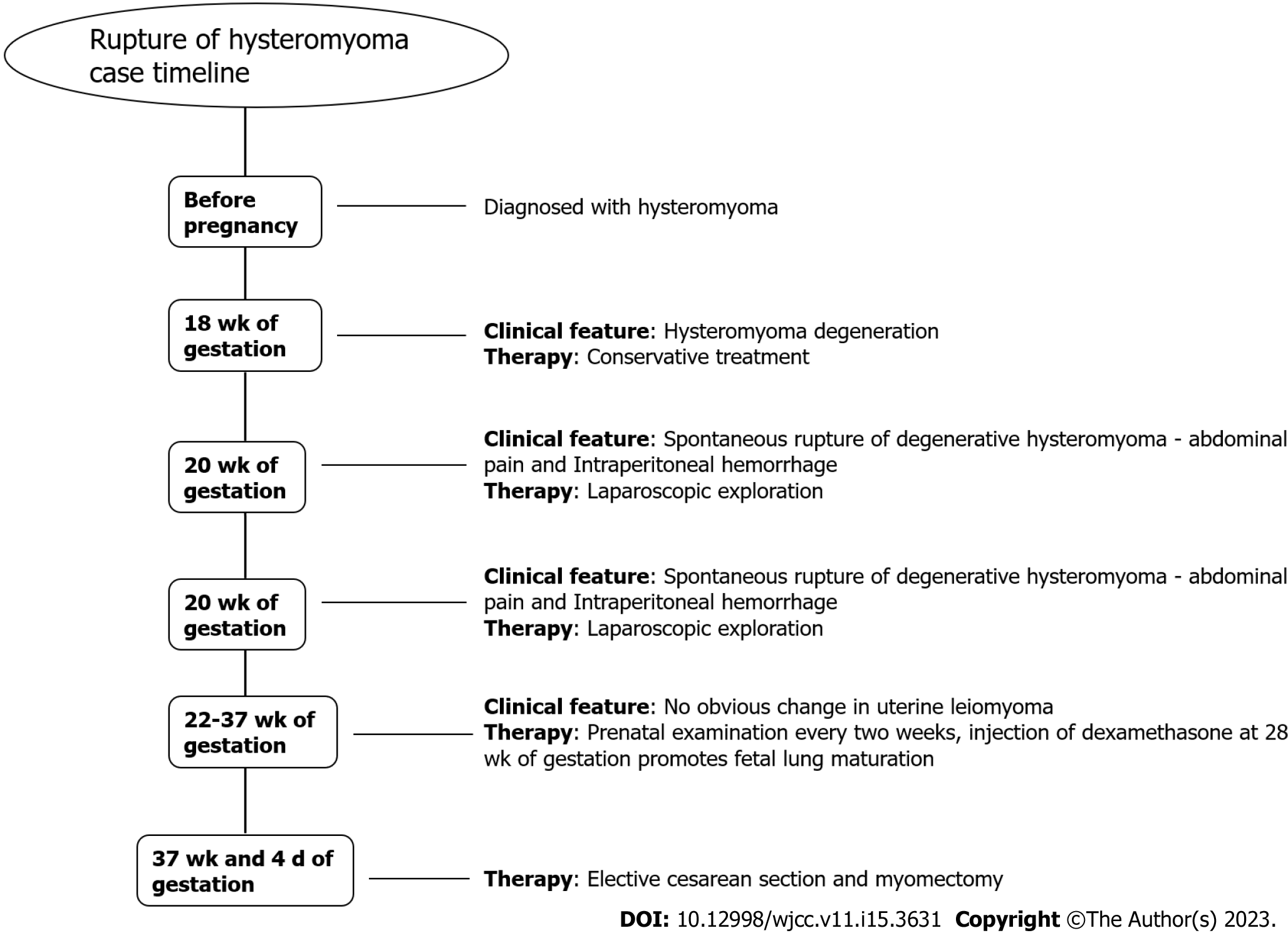
The patient was diagnosed with hysteromyoma before pregnancy, with no history of uterine or abdominal surgeries. At 18 wk of gestation, she had lower abdominal pain and threatened abortion, which were considered to be caused by hysteromyoma degeneration. Then the patient received a conservative treatment in our hospital and was discharged after symptom relief.
The patient’s pulse rate was 98 per minute, blood pressure was 97/74 mmHg, and body temperature was 37 °C. In addition to the peritoneal irritation sign, a goose-egg-sized mass was palpated in her right upper abdomen, and severe tenderness was observed at the same site.
Laboratory data included white blood cell count 21400/mm3, hemoglobin 8.9 g/dL, and C-reactive protein 12.4 mg/dL (normal, 0.2 mg/dL).
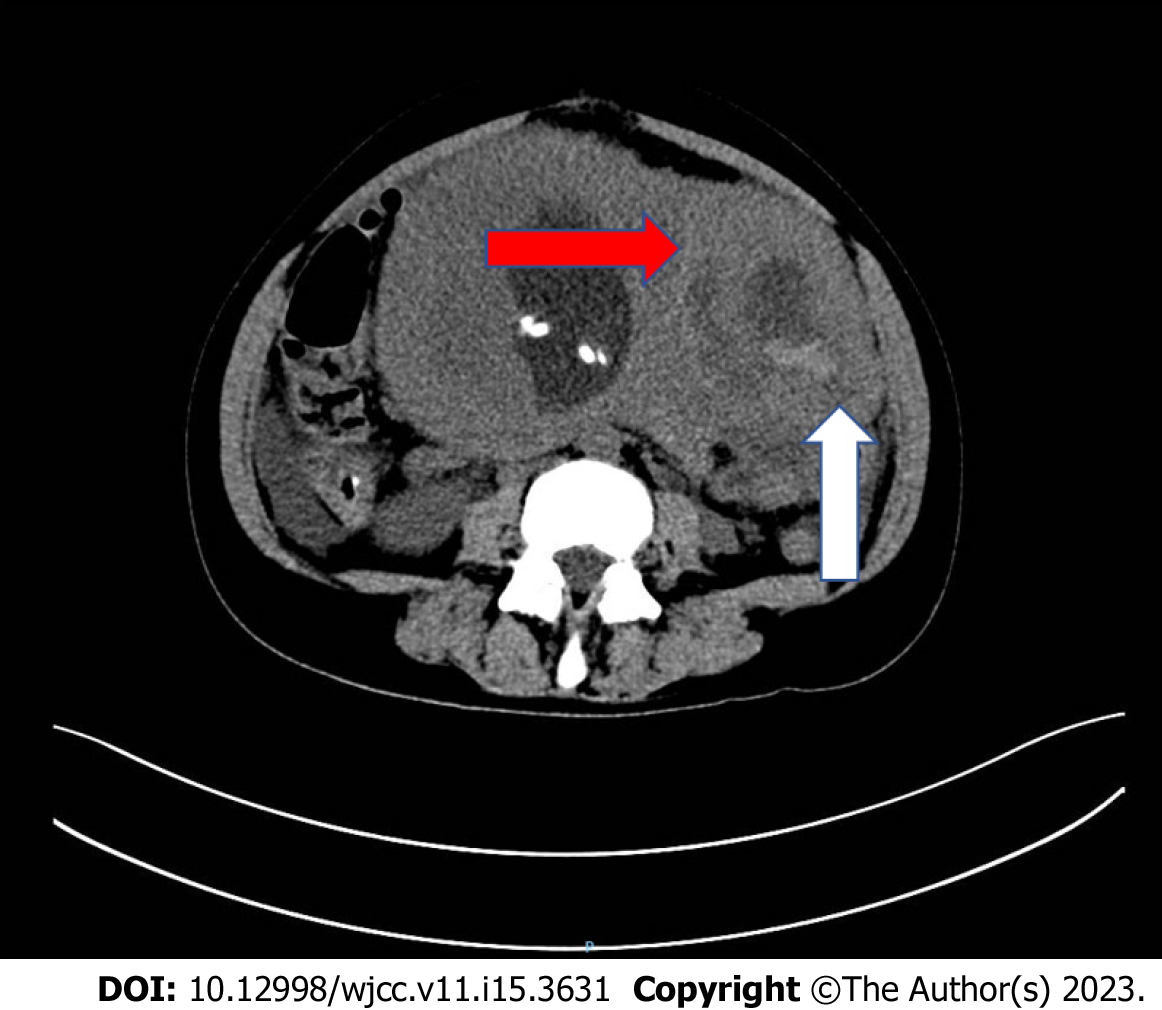
Abdominal sonogram confirmed an intrauterine live fetus after 20 wk of gestation and a 10-cm degenerative hysteromyoma. Combined with the patient's medical history and clinical symptoms, hysteromyoma degeneration was clinically suspected. In addition, the abdominal sonogram showed that there was a large amount of free fluid in her upper abdomen, indicating intra-abdominal hemorrhage. Computed tomography (CT) revealed a hysteromyoma situated in the left fundus of uterus, with a rupture (Figure 1).
Intra-abdominal hemorrhage was suspected, which was confirmed by the extraction of non-coagulable blood from the abdominal cavity under ultrasound guidance.
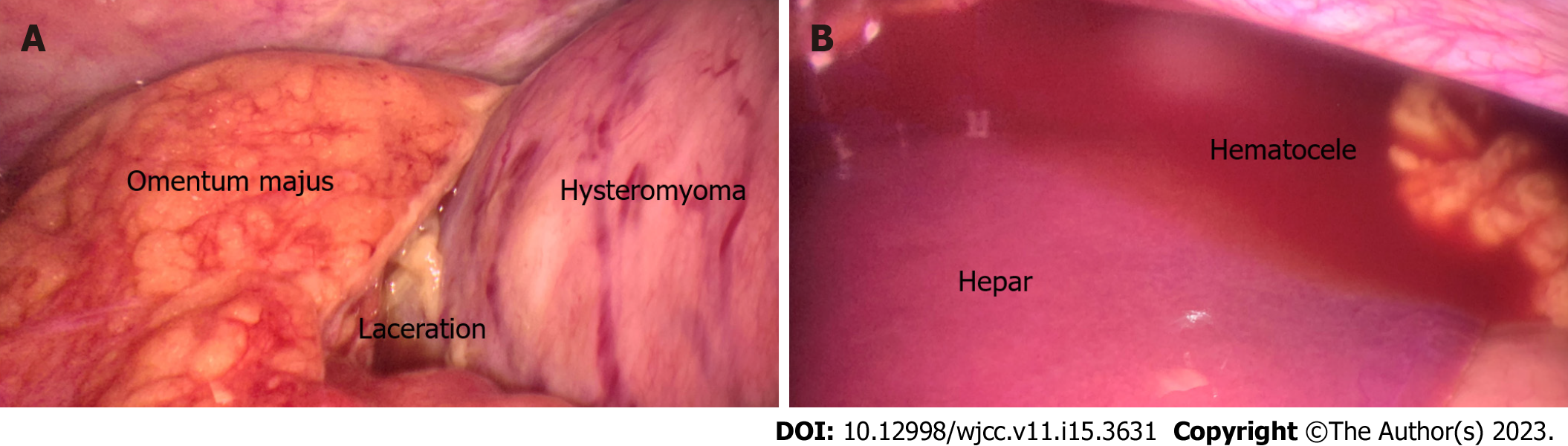
The patient underwent an immediate laparoscopic exploration with general anesthesia, through which rupture of the hysteromyoma and massive hemoperitoneum were revealed. We can see a huge subserous myoma in the fundus of her uterus with a 2 cm perforation at the top, oozing necrotic fluid and tissues into her abdominal cavity. The omentum was slightly adherent to perforation, and the adjacent peritoneum showed fibrinous reactions. About 200 mL of perihepatic and perisplenic hemoperitoneum could be seen, but no active bleeding point was found (Figure 2). Then hemoperitoneum was cleared and adhesion was released, and her abdomen was closed after copious irrigation. Two abdominal drainage tubes were placed. Anti-inflammatory and fetal protection treatments (ritodrine hydrochloride for inhibiting uterine contraction) were continued after operation.
After confirming that there was no intraperitoneal hemorrhage, the two abdominal drainage tubes were removed on the 3rd and 7th day after operation, respectively. The patient was discharged on the 7th day after operation. The subsequent antenatal period was uneventful (Figure 3). After 37 wk and 4 d of pregnancy, the patient delivered a healthy male infant with a birth weight of 3450g through an elective cesarean section and underwent myomectomy at the same time (Figure 4). The operation was successful with a total bleeding volume of about 600 mL.
Most female patients with uterine fibroids during pregnancy have no or only mild clinical symptoms, which can be relieved after conservative treatments (anti-inflammatory and inhibiting uterine contraction)[3,5]. In this report, we describe a case of degeneration, necrosis, and rupture of hysteromyoma during pregnancy, resulting in intraperitoneal hemorrhage and acute peritonitis, which could not be relieved through conservative treatments. It has been previously reported that the rupture of blood vessels on the surface of hysteromyoma during pregnancy or after delivery leads to acute abdomen (intraperitoneal hemorrhage)[6,7]. There are also reports on acute peritonitis caused by the degeneration, necrosis, liquefaction, and rupture of uterine hysteromyoma during pregnancy[5]. Our patient initially developed a degeneration and necrosis of hysteromyoma with vascular rupture during the progression of peritonitis, resulting in intraperitoneal hemorrhage.
Limited data can be used to guide clinicians to choose diagnoses and treatments for pregnant women complicated with hysteromyoma-related acute abdomen. In 1989, Makar et al[8] first reported that a female patient had peritonitis caused by the perforation and rupture of uterine fibroids during the 15th week of pregnancy, whose initial symptom was abdominal pain, and then there were aggravated peritonitis symptoms. The degeneration of hysteromyoma was shown via ultrasound. The necrotic perforation of hysteromyoma was confirmed by an open exploration, and only abdominal flushing was carried out to alleviate the symptoms of peritonitis. Unfortunately, the fetus eventually failed to survive[8]. For the selection of auxiliary examinations, CT and magnetic resonance imaging (MRI) are of great value for the diagnosis of uterine myoma rupture, which are helpful for preoperative diagnoses and the timely formulation as well as optimization of surgical plans[9]. In this case, the preoperative CT image of hysteromyoma perforation provides great value for making an operation plan in time. In addition to acute abdomen caused by the degeneration and perforation of hysteromyoma, the increase of blood vessels and venous congestion on the surface of uterine fibroids, as well as the increase of surface tension of uterine fibroids caused by the mechanical compression of uterine fibroids, are all high-risk factors for myoma-related acute abdomen during pregnancy. The vein tear on the surface of hysteromyoma leads to intraperitoneal bleeding, endangering the safety of mothers and children, which often occurs in large subserosal hysteromyoma. In terms of auxiliary examinations, both CT scan and MRI can be used to accurately identify the rupture of a degenerated hysteromyoma[9]. When there is intra-abdominal hemorrhage caused by uterine rupture, free fluid in the abdominal cavity can be shown through ultrasound and CT (while it is important to expose only the fetus to radiation if necessary, a dose is not typically delivered through routine CT performed in a single session at which serious biologic effect occurs[10]), and blood routine examinations show that the hemoglobin of the patient continues declining. If no definite hemoperitoneum is found through an imaging examination, it is important to monitor the changes of hemoglobin. For unexplained intra-abdominal hemorrhage, a diagnosis can be made only after laparoscopy. In this case, since it was impossible to rule out whether the acute abdomen was caused by gastrointestinal perforation at the early stage of diagnosis, we chose to use CT to make a clear diagnosis. We performed an abdominal puncture to confirm intra-abdominal hemorrhage, and then performed a surgery in time. During pregnancy, surgeries are often delayed to avoid unnecessary effect of anesthesia and surgical stimulation on the fetus. However, for acute abdomen caused by hysteromyoma during pregnancy, surgical treatments are necessary. The condition may be delayed due to delayed surgeries, causing adverse maternal and fetal outcomes. For the choice of surgical methods, although there is some previous literature reporting that open exploration and successful myomectomy have been carried out during pregnancy, after which the patients have delivered at full term with good maternal and fetal outcomes achieved[5,11], myomectomy during pregnancy leads to a greater risk of postoperative fetal loss and uncontrolled bleeding after hysterectomy. Conservative treatments and careful myomectomy during pregnancy are generally recommended in the medical literature[12].
In this report, the patient underwent laparoscopic exploration, whose abdominal cavity was thoroughly washed and an abdominal drainage tube was placed, through which good results were achieved.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Obstetrics and gynecology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Alao AI, Nigeria; Cooper KM, United States; Jovandaric MZ, Serbia S-Editor: Yan JP L-Editor: Wang TQ P-Editor: Chen YX
| 1. | De Vivo A, Mancuso A, Giacobbe A, Savasta LM, De Dominici R, Dugo N, Dugo C, Vaiarelli A. Uterine myomas during pregnancy: a longitudinal sonographic study. Ultrasound Obstet Gynecol. 2011;37:361-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 47] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 2. | Murase E, Siegelman ES, Outwater EK, Perez-Jaffe LA, Tureck RW. Uterine leiomyomas: histopathologic features, MR imaging findings, differential diagnosis, and treatment. Radiographics. 1999;19:1179-1197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 310] [Cited by in RCA: 247] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 3. | Kawakami S, Togashi K, Konishi I, Kimura I, Fukuoka M, Mori T, Konishi J. Red degeneration of uterine leiomyoma: MR appearance. J Comput Assist Tomogr. 1994;18:925-928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 61] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Takeuchi M, Matsuzaki K, Bando Y, Harada M. Evaluation of Red Degeneration of Uterine Leiomyoma with Susceptibility-weighted MR Imaging. Magn Reson Med Sci. 2019;18:158-162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 5. | Kobayashi F, Kondoh E, Hamanishi J, Kawamura Y, Tatsumi K, Konishi I. Pyomayoma during pregnancy: a case report and review of the literature. J Obstet Gynaecol Res. 2013;39:383-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Kasum M. Hemoperitoneum caused by a bleeding myoma in pregnancy. Acta Clin Croat. 2010;49:197-200. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Wong L, Ching TW, Kok TL, Koon TH. Spontaneous hemoperitoneum from a uterine leiomyoma in pregnancy. Acta Obstet Gynecol Scand. 2005;84:1208-1209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Makar AP, Meulyzer PR, Vergote IB, Schatteman EA, Huyghe ML, Meeuwis LA. A case report of unusual complication of myomatous uterus in pregnancy: spontaneous perforation of myoma after red degeneration. Eur J Obstet Gynecol Reprod Biol. 1989;31:289-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Kamat NV, Telkar HB, Ramani SK, Thakker AP. Ruptured degenerated uterine fibroid diagnosed by imaging. Obstet Gynecol. 2001;98:961-963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Sensakovic WF, Royall I, Hough M, Potrebko P, Grekoski V, Vicenti R. Fetal Dosimetry at CT: A Primer. Radiographics. 2020;40:1061-1070. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 11. | Odagami M, Makino M, Miyagi E, Aoki S. Spontaneous rupture of a degenerated leiomyoma causing peritonitis and ileus during pregnancy: A case report. Clin Case Rep. 2021;9:491-493. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 12. | Yu CH, Weng SF, Ho CH, Chen YC, Chen JY, Chang YJ, Wang JJ, Wu MP, Chu CC. Pregnancy outcomes following nonobstetric surgery during gestation: a nationwide population-based case-control study in Taiwan. BMC Pregnancy Childbirth. 2018;18:460. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |