Published online May 26, 2023. doi: 10.12998/wjcc.v11.i15.3583
Peer-review started: January 4, 2023
First decision: February 17, 2023
Revised: March 4, 2023
Accepted: April 18, 2023
Article in press: April 18, 2023
Published online: May 26, 2023
Processing time: 141 Days and 7.5 Hours
Pyogenic spondylitis is often manifested as atypical low back pain and fever, which makes it easy to be confused with other diseases. Here we report a case of pyogenic spondylitis and describe the diagnosis and treatment based on the related literature.
The reported case suffered from pyogenic spondylitis caused by Escherichia coli and complicated with bacteremia and psoas abscess. Acute pyelonephritis was initially diagnosed due to atypical symptoms. Symptoms were improved from antibiotic treatment while developing progressive lower limb dysfunction. One month post the admission, the patient underwent anterior lumbar debridement + autogenous iliac bone graft fusion + posterior percutaneous screw-rod internal fixation, and received 6 wk of antibiotic treatment after the operation. Reexamination 4 mo post the operation showed that the patient had no evident pain in the waist, and walked well with no evident dysfunction of lower limbs.
Here we describe the application value of several imaging examinations, such as X-ray, computed tomography and magnetic resonance imaging, and certain tests like erythrocyte sedimentation rate and C-reactive protein in the clinical treatment of pyogenic spondylitis. This disease requires early diagnosis and treatment. Sensitive antibiotics should be used in early stages and surgical intervention should be taken if necessary, which may help for a speedy recovery and prevent the occurrence of severe complications.
Core Tip: The reported case suffered from pyogenic spondylitis caused by Escherichia coli and complicated with bacteremia and psoas abscess. Acute pyelonephritis was initially diagnosed due to atypical symptoms. Symptoms were improved from antibiotic treatment while developing progressive lower limb dysfunction. One month post the admission, the patient underwent anterior lumbar debridement + autogenous iliac bone graft fusion + posterior percutaneous screw-rod internal fixation, and received 6 wk of antibiotic treatment after the operation. Reexamination 4 mo post the operation showed that the patient had no evident pain in the waist, and walked well with no evident dysfunction of lower limbs.
- Citation: Zou LC, Qian J, Bian ZY, Wang XP, Xie T. Pyogenic spondylitis caused by Escherichia coli: A case report and literature review. World J Clin Cases 2023; 11(15): 3583-3591
- URL: https://www.wjgnet.com/2307-8960/full/v11/i15/3583.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i15.3583
Pyogenic spondylitis (PS) is a type of non-specific spondylitis caused by bacterial infection mainly involving vertebral body and/or intervertebral disc, and can be clinically classified as discitis, vertebral osteomyelitis and epidural abscess[1,2]. Antibiotic treatment of septic spondylitis is a long-term process, and identification of the pathogenic microorganism by blood culture, tissue culture and nucleic acid amplification test is crucial[3]. Staphylococcus aureus is the most pathogenic, while Gram-negative bacilli cannot be negated, with the disease caused by relevant infections on the rise annually[4]. Due to the fact that the clinical symptoms of PS are lack of specificity, early diagnosis turns out a tough issue, which results in failure of timely and effective treatment. Besides, PS after recovery often comes with nerve injury and spinal deformity attributed to the long disease course and poor prognosis[5,6].
Escherichia coli (E. coli) is an opportunistic pathogen that is mainly responsible for cystitis and even pyelonephritis secondary to transurethral infection of the urinary system. Currently, there have been few case reports for the PS caused by E. coli[7]. We here report a 61-year-old male case of PS caused by E. coli infection, whose main manifestations are acute urethral syndrome and low back pain. We also review the relevant literature to elucidate related treatment strategies and experience for this rare disease.
Had bilateral low back pain (mainly manifested on the left) with prominent dysuria, urgency, and frequency.
While with no significant fever, the low back pain was gradually exacerbated in following days. One day prior to the admission, the patient suffered from chills and fever with a body temperature up to 39.5°C, and accompanied with gross hematuria.
The patient had pulmonary tuberculosis 30 years ago.
No special personal history, no familial genetic disease.
Physical examination showed bilateral lumbar tenderness prominent on the left, bilateral renal percussion pain manifested as positive and no signs of neurological disorders.
Laboratory examination revealed no increase in white blood cell (WBC) count (7.9 × 103/μL) at admission, including neutrophil count of 6.4 × 103/μL and lymphocyte count of 0.6 × 103/μL, as described in reported literature[8], while an increase of C-reactive protein (CRP) content (260 mg/L) and procalcitonin (5.34 ng/L). On the 1st day of the admission, flow urine sediment inspection presented red blood cell (2683/ul) and WBC (142/uL), with no WBC or pyocyte in stool routine. On the 4th day of the admission, E. coli were detected from blood by bacteria culture (piperacillin/tazobactam S: < 4), Acinetobacter baumannii and Aeromonas caviae were seen in urine with no bacilli detected, and no pathogens like Salmonella and Vibrio parahaemolyticus were detected in feces. On the 7th day of the admission, no acid-fast bacilli were detected from sputum smear.
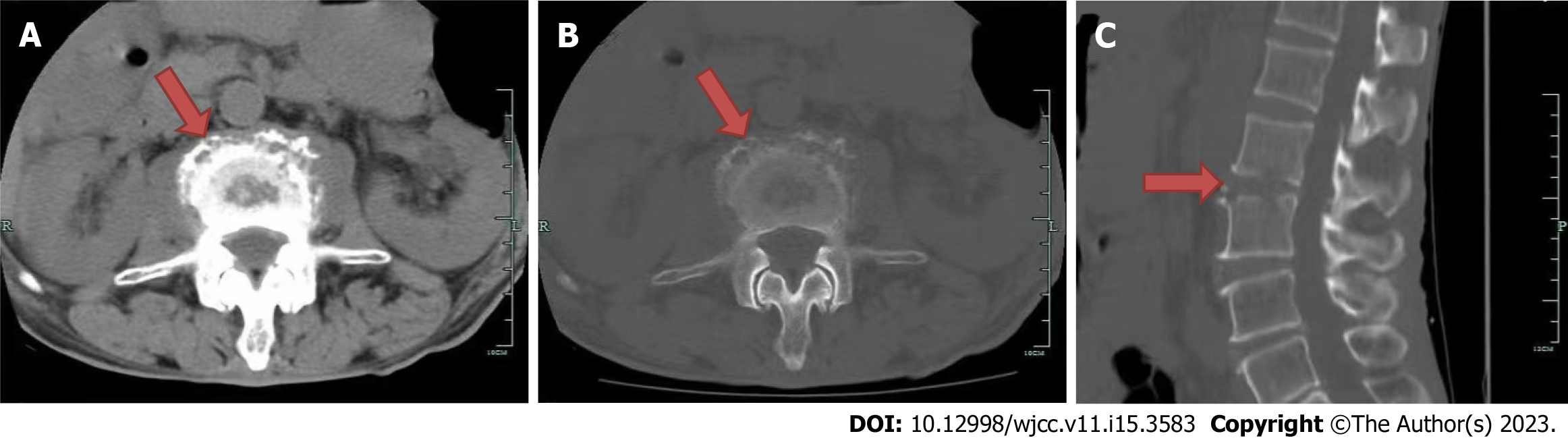
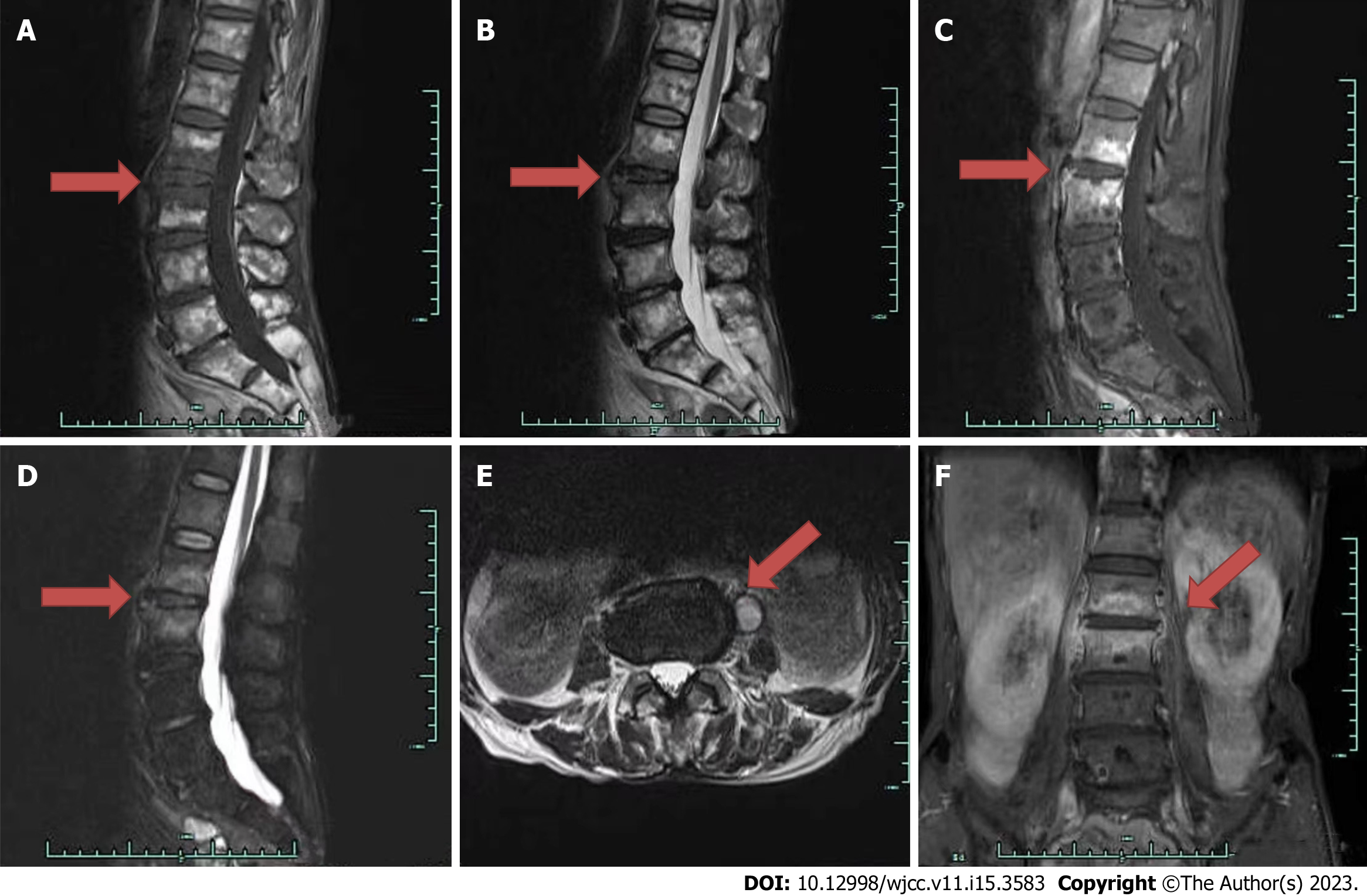
Lumbar computed tomography (CT) examination showed local bone defects at lower margin of L2 vertebral body and upper margin of L3 vertebral body, mass-like soft tissue density shadow around, left psoas enlargement with uneven density, and infection was suspected (Figure 1). Lumbar magnetic resonance imaging (MRI) examinations indicated that there are patchy hypo-intense signals in the L2-L3 vertebral bodies in T1 and T2 weighted images. MRI examinations also showed that the cortical bone of spine is incomplete and there are hyper-intense signals in the L2-3 vertebral bodies in images with fat suppression, and no obvious enhancement is seen after enhanced scan. There are long T1 and T2 signal shadows in the left psoas major muscle, and annular enhancement is observed from enhanced scan, which suggested abscess formation (Figure 2).
According to the clinical manifestation, laboratory test results and imaging findings, the patient was finally diagnosed with pyogenic spondylitis caused by E. coli.
The patient was diagnosed with acute pyelonephritis at admission. He initially went to the Department of Nephrology and received intravenous piperacillin/tazobactam (4.5 g) once every 8 h combined with intravenous moxifloxacin (0.4 g) once daily for anti-infection treatment. Intravenous aztreonam (2 g) once every 8 h was then taken according to the results of blood culture and drug test. Urinary irritation symptoms and fever were improved after treatment. The patient still had persistent pain in the waist, which gradually extended to the left thigh. Physical examination showed Grade 3 muscle strength of the left iliopsoas, Grade 4 muscle strength of the quadriceps, and weakened left knee and ankle reflexes. Lumbar CT and magnetic resonance imaging (MRI) examinations showed abnormal L2-3 vertebral bodies, and formation of paravertebraland left psoas abscess, and infection was suspected. Conservative treatment with intravenous antibiotics was continued, and no resolution of symptoms was observed. On the 34th day of admission, the patient received anterior lumbar debridement + autogenous iliac bone graft fusion + posterior percutaneous pedicle screw-rod internal fixation. During the operation, the abscesses around the psoas major muscle were removed, and the large amount of necrotic tissue in the L2-3 intervertebral space was cleaned and kept for culture. Autologous iliac bone of the patient was taken for structural bone grafting after trimming. Piperacillin/tazobactam (4.5 g) once every 8 h was given by intravenous drip for anti-infection treatment after the operation.
Fever, low back pain and radiating pain of the left lower limb were significantly alleviated, and the infection indexes in blood routine significantly recovered. Postoperative lumbar X-ray showed good L2-3 internal fixation and well positioned bone graft, and no paravertebral soft tissue swelling was found. The muscle strength of the left lower limb recovered significantly after 1 mo of the operation. Four months after the operation, imaging findings showed good lumbar internal fixation of the bone graft, and the patient had no prominent low back pain or dysfunction of lower limbs, and walked well by himself.
PS caused by E. coli infection is a rare disease that is commonly seen secondary to genitourinary diseases, such as urinary tract infection and pyelonephritis[9]. Common predisposing factors include diabetes, and complications from a history of spinal surgery or trauma[10-13]. Recent studies have shown that patients with PS caused by Gram-negative bacilli infection may have potential malignant tumors or are under immunosuppression[14]. PS caused by Gram-negative bacilli infection is a blood-borne disease. Microorganisms reach the spine through the vertebral nutrient arterioles or the paraspinal Baston venous plexus, which is similar to the metastasis of malignant tumors to the spine and is the main cause for the occurrence of PS[15,16].
The patient in this report had no diarrhea, and no WBCs or pyocyte in stool routine. Intestinal infection was excluded. The patient had no previous spinal trauma. Among the tumor indicators, prostate specific antigen was slightly increased to 4.436 μg/L. B-mode ultrasound of urinary system showed peri-renal abscesses, urine culture grew Acinetobacter baumannii and Aeromonas caviae. E. Coli was tested negative in urine culture, but detected positive in blood and intervertebral pus culture. E. Coli infection from the urinary system, therefore, cannot be ruled out as a cause of spinal involvement.
The diagnosis of PS requires a combination of clinical manifestations, imaging examination, laboratory examinations, etiologic examinations and drug sensitivity tests[17].
PS is characterized by atypical symptoms. For patients suffering from PS caused by Gram-negative bacilli infection, pain in the affected part is the most common symptom, though up to 15% of patients may feel no pain[4,13,18]. Persistent pain is a dangerous sign of PS and worsens at night[13,18]. Only 16.4% of the patients present with motor weakness. Lumbar spine involvement is the most common, and paravertebral abscesses develop in about half of the patients which is easy to be confused with peri-renal one[19]. Despite the low mortality, this disease often comes with sequelae like neurological deficits, which makes early diagnosis particularly important[10].
In this reported case, a delayed diagnosis was made, since the initial diagnosis by physicians in the Department of Nephrology was only based on the B-mode ultrasound for urinary system and blood culture, combining a difficulty in distinguishing lumbar percussion pain from bilateral renal percussion pain. High fever was relieved by taking sensitive antibiotics according to drug sensitivity test, but the body temperature still fluctuated repeatedly, finally resulting in the occurrence of symptoms of nerve dysfunction of lower limbs. Lumbar infection was then evidenced by lumbar CT scan and MRI examination.
Early PS shows few symptoms in early X-rays, and the normal appearance can usually be maintained for 2-8 wk[18]. Disc space narrowing, irregularity, or unclear vertebral endplates are the initial and most common manifestations[20]. Osteopetrosis may develop within 10-12 wk if no treatment is managed[18]. For the PS in early stages, radionuclide examination is more sensitive compared to X-ray examination with a diagnosis rate of at least 90%[21]. However, it has low specificity, which is especially seen in patients having tumor metastasis or degenerative spinal disease[21,22]. CT findings are similar to those in conventional X-rays but potentially more sensitive to early changes, including swelling of surrounding soft tissue, effusion and epidural abscess, which is suitable for patients with contraindications to MRI[22]. Currently, CT-guided needle biopsy is identified a helpful tool for early pathological and bacteriological diagnosis.
In 2015, Infectious Diseases Association recommended MRI as the first choice for PS inspection due to its sensitivity and specificity as high as 98% and 93%, respectively, and it was regarded as the most sensitive and specific detection method for PS[13,18,23]. In most cases, spinal osteomyelitis manifests as destructive and expansive lesions in MRI findings. Bone marrow edema may lead to increased fluid signals, manifested as hyper-intense signal on T2-weighted images, hypo-intense signal on T1-weighted images, and positive gadolinium enhancement[22]. MRI is superior in distinguishing tumors from degenerative diseases to other imaging examinations[6]. On T2-weighted images, the highest signal intensity for infectious lesions of PS is seen equal to or higher than that of cerebrospinal fluid, while the signal intensity of malignant lesions is lower[20]. Besides, epidural and soft tissue abscesses are also readily seen on T2-weighted images and contrast sequences[18]. Nevertheless, inflammatory repair and bone healing can be seen earlier in CT images, compared to MRI findings, which makes CT scan superior in curative effect monitoring and long-term follow-up[24].
More than 90% of patients with spinal infection have changes in certain inflammatory indicators, such as erythrocyte sedimentation rate (ESR) and CRP[25]. Rosahl et al[26] suggested that CRP and ESR should be used as monitoring indicators for the diagnosis and treatment of spinal infection. WBC count may not increase in patients with PS, and such increase is reported to occur in no more than 50% of cases[18]. It is recognized that WBC count is a routine examination indictor for the diagnosis of infection, but its specificity for spinal infection is relatively low.
Blood culture is the simplest method for identification of microorganisms, and with this way responsible pathogen can be identified in about half of patients with PS[27]. This method is recommended to complete in the peak period of fever or the period of the severe degree of chills, which helps improve the microbial positive rate[18]. In cases of negative results, percutaneous bone biopsy should be considered. Besides, open biopsy sampling is required if two or more cultures from CT-guided biopsy samples or blood fail to identify pathogens[28].
Treatment approaches for PS include antibiotic treatment, external fixation (cervical spine) or use of braces (thoracic and lumbar spine), and surgery[18,29], while the optimal treatment has not yet been determined.
The intervertebral disc is the largest structure devoid of blood vessels in the human body, and the penetration into tissues by antibiotics must be carefully considered when choosing the appropriate antibiotic regimen[4]. Fluoroquinolones, clindamycin, and rifapentine are recommended by some specialists for the PS caused by E. coli[30-32]. Some studies found that patients receiving a combination of multiple antibiotics have shorter treatment duration compared to patients with a single antibiotic[4]. Antibacterial agents should be delayed, unless disease progresses, until a microbiological diagnosis is established[18]. CT-guided biopsy is required in cases of the initial blood culture is negative. If the pathogen cannot be determined, empirical broad-spectrum antibiotics (e.g. third-generation cephalosporins) is recommended, which may cover most bacterial infections.
As for the duration of medication, a 6-wk antibiotic treatment has efficacy not inferior to a 12-wk antibiotic treatment, suggesting that standard antibiotic treatment for patients with the disease can be shortened to 6 wk[33]. Moreover, most studies suggest a medication time of 6-8 wk with intravenous injection of antibiotics, followed by a further treatment time of around 6 wk with oral antibiotics. Antibiotic discontinuation can be managed while following symptoms occur[34]: (1) Alleviation of spinal pain and disappearance of inflammation; (2) Normal body temperature; (3) Normal CRP and/or ESR; and (4) Stable and improved X-rays. For patients with severe sepsis, regular monitoring of liver and kidney function should be considered when antibiotics are used.
At the initial diagnosis, bed rest is recommended for about 3-4 mo until the pain is significantly relieved[13]. External fixation helps stabilize the spine, relieve pain, prevent deformity, and allow a small range of spinal movement[2]. The duration of fixation depends on the severity of bone destruction and deformity until bony ankylosis occurs[35,36].
Percutaneous drainage, which is a minimally invasive treatment combining etiological and histopathological diagnosis, has become the only effective treatment option for patients who cannot tolerate surgery and respond to long-term anti-infection treatment[37]. CT-guided percutaneous puncture or surgical treatment should be considered for abscess drainage and infection control in the presence of uncontrollable sepsis. Soft tissue is the best action site for microbiological diagnosis in PS patients with needle biopsy[38].
Surgical treatment is committed to removing infected foci to reduce the compression on the nerve as far as possible, which facilitates to alleviate symptoms, reconstruct the stability of spine and correct spinal deformity[36,39].
The surgical indications for PS are described as follows: (1) No clinical improvement after 2-3 wk of intravenous antibiotics, or the persistently increased inflammatory indicators, ESR and CRP[40]; (2) Spinal cord compression, no more than 36 h of paralysis time, or progressive neurological dysfunction[41]; and (3) Spinal instability and/or deformity[16]. When the disease progresses to chronic osteomyelitis, surgical removal of necrotic tissue also needs to be considered, which may result in reduction of bacterial biofilm formation and development of antibiotic resistance[42].
The surgery time for patients with PS should be scheduled comprehensively from two aspects: The effect of anti-infection treatment and the symptoms of spinal nerves[35]. Segreto et al[43]conducted a retrospective analysis covering the clinical information of PS cases, and found that patients who underwent surgery within 24 h of admission received better outcome than those who underwent conservative treatment or delayed surgery.
The surgical approaches for PS fall into posterior approach, anterior approach, combined anterior and posterior approach and lateral approach[44,45]. Among them, anterior approach is classic[36]. Since intervertebral infection is mostly seen in the anterior and middle column of spine, the anterior approach can make the infected site fully exposed, which directly and clearly displays the diseased tissue to help thoroughly remove the necrotic and infected tissue. In addition, full drainage of the complicated psoas or epidural abscesses can be achieved to avoid residual infectious foci and bacteria[46]. However, anterior internal fixation often results in surgical failure due to the insufficient fixation strength[44]. Besides, anterior approach is also associated with higher postoperative morbidity and mortality[45]. Simple posterior approach for focal debridement and bone grafting has a relatively narrowed operation field, which is prone to result in incomplete focal clearance, insufficient treatment of bone grafting surface of the upper and lower endplates, not fully recovered intervertebral height and other conditions, leading to uncontrollable foci and failed bone graft fusion[44]. Given these considerations, a combi
Minimally invasive techniques, such as percutaneous endoscopic debridement combined with percutaneous pedicle screw fixation, provide a better alternative to the treatment of PS. Percutaneous endoscopic-assisted surgery can keep the posterior structure intact, while minimally invasive pedicle screw rod system can achieve strong internal fixation[40].
Since most patients requiring a surgery are in severe disease conditions, which may lead to obvious bone loss of anterior column, bone graft fusion is required aiming to stabilize the anterior spine and prevent the posterior spinal kyphosis to further reduce the relevant damage of nervous system, while autologous bone grafting is the most traditional way. Bone graft fusion is generally performed with the iliac, rib, or fibula which is of a high fusion rate[16]. In recent years, the application of interbody fusion cages and titanium mesh cages also provides more options for intervertebral fusion[47,48].
Following bone fusion, nutritional support and bed rest are recommended, and ground activities are allowed under protection of braces. Broad-spectrum antibiotics should be taken one week after the operation, and sensitive antibiotics are used and adjusted according to the results of bacteria culture and drug sensitivity test for 6 wk. In following 6-8 wk, oral antibiotics are taken as alternative until the symptoms disappear, and ESR and CRP decrease to normal range[34].
In short, for patients suspected of PS, early diagnosis is essential. Once the results of bacteria culture have been identified, the corresponding antibiotics should be initiated for the treatment. It should be noted that active surgery for PS may improve the prognosis. On the basis of rational surgical indications, anterior focal debridement and bone graft fusion + posterior pedicle screw internal fixation + sensitive antibiotics for spinal infection is an effective treatment for PS, which can achieve reliable fixation and good therapeutic effect.
There are some deficiencies in the diagnosis and treatment of this case. For example, the patient was admitted to our hospital for non-specific symptoms, such as high fever and back pain, with a diagnosis of acute pyelonephritis, and treated with conservative treatment, while PS was delayed diagnosed in 2 wk. Atypical symptoms often lead to delay in diagnosis, which highlights the significance of early clinical detection and diagnosis. It is noteworthy that for patients with more high risk factors, such as non-mechanical new or aggravated low back pain, fever, elevated ESR and/or CRP, diabetes, or complicated genitourinary infections, necessary MRI examination can achieve early diagnosis and distinguish PS from malignant tumors, epidural or other abscesses. Blood, urine, sputum and throat swab culture should be managed at the same time to identify the source of infection. Bacterial culture result can guide the treatment. Although there is a lack of randomized controlled trial, the drug treatment time is generally recommended to be 6 wk, and patients with surgical indications still need to consider surgical treatment.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mohey NM, Egypt; Rotondo JC, Italy S-Editor: Liu JH L-Editor: A P-Editor: Chen YX
| 1. | Lazzeri E, Bozzao A, Cataldo MA, Petrosillo N, Manfrè L, Trampuz A, Signore A, Muto M. Joint EANM/ESNR and ESCMID-endorsed consensus document for the diagnosis of spine infection (spondylodiscitis) in adults. Eur J Nucl Med Mol Imaging. 2019;46:2464-2487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 53] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 2. | Cheung WY, Luk KD. Pyogenic spondylitis. Int Orthop. 2012;36:397-404. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 160] [Cited by in RCA: 189] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 3. | Kim NJ. Microbiologic Diagnosis of Pyogenic Spondylitis. Infect Chemother. 2021;53:238-246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Graham SM, Fishlock A, Millner P, Sandoe J. The management gram-negative bacterial haematogenous vertebral osteomyelitis: a case series of diagnosis, treatment and therapeutic outcomes. Eur Spine J. 2013;22:1845-1853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Gouliouris T, Aliyu SH, Brown NM. Spondylodiscitis: update on diagnosis and management. J Antimicrob Chemother. 2010;65 Suppl 3:iii11-iii24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 331] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 6. | Malaviya AN, Rawat R, Agrawal N, Patil NS. The Nonradiographic Axial Spondyloarthritis, the Radiographic Axial Spondyloarthritis, and Ankylosing Spondylitis: The Tangled Skein of Rheumatology. Int J Rheumatol. 2017;2017:1824794. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Jiang N, Ma YF, Jiang Y, Zhao XQ, Xie GP, Hu YJ, Qin CH, Yu B. Clinical Characteristics and Treatment of Extremity Chronic Osteomyelitis in Southern China: A Retrospective Analysis of 394 Consecutive Patients. Medicine (Baltimore). 2015;94:e1874. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 8. | Rotondo JC, Aquila G, Oton-Gonzalez L, Selvatici R, Rizzo P, De Mattei M, Pavasini R, Tognon M, Campo GC, Martini F. Methylation of SERPINA1 gene promoter may predict chronic obstructive pulmonary disease in patients affected by acute coronary syndrome. Clin Epigenetics. 2021;13:79. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 9. | Aragón-Sánchez J, Lipsky BA, Lázaro-Martínez JL. Gram-negative diabetic foot osteomyelitis: risk factors and clinical presentation. Int J Low Extrem Wounds. 2013;12:63-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Mylona E, Samarkos M, Kakalou E, Fanourgiakis P, Skoutelis A. Pyogenic vertebral osteomyelitis: a systematic review of clinical characteristics. Semin Arthritis Rheum. 2009;39:10-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 376] [Cited by in RCA: 391] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 11. | O'Neill SC, Baker JF, Ellanti P, Synnott K. Cervical epidural abscess following an Escherichia coli urinary tract infection. BMJ Case Rep. 2014;2014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Gaschignard J, Geslain G, Mallet C, Lorrot M, Blot N, Alison M, Bonacorsi S. Spondylodiscitis in a healthy 12-year-old girl with Extraintestinal pathogenic Escherichia coli (ExPEC) bacteraemia. BMC Infect Dis. 2017;17:380. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Del Pozo FJ, Alonso JV, Ruiz MÁ, Vythilingam S, Ruiz DL. Community Acquired Spondylodiscitis caused by Escherichia Coli; Case Report and Literature Review. Bull Emerg Trauma. 2016;4:174-179. [PubMed] |
| 14. | Park KH, Cho OH, Jung M, Suk KS, Lee JH, Park JS, Ryu KN, Kim SH, Lee SO, Choi SH, Bae IG, Kim YS, Woo JH, Lee MS. Clinical characteristics and outcomes of hematogenous vertebral osteomyelitis caused by gram-negative bacteria. J Infect. 2014;69:42-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 15. | Cahill DW, Love LC, Rechtine GR. Pyogenic osteomyelitis of the spine in the elderly. J Neurosurg. 1991;74:878-886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 82] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 16. | Hsieh PC, Wienecke RJ, O'Shaughnessy BA, Koski TR, Ondra SL. Surgical strategies for vertebral osteomyelitis and epidural abscess. Neurosurg Focus. 2004;17:E4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 63] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 17. | Zhang SC, Li YX, Mo L, Liang D, Yang ZD, Guo DQ, Feng PB, Mo GY, Li DX, Li YW, Tang YC. [Analysis of clinical characteristics of 20 patients with pyogenic spondylitis]. Zhongguo Gu Shang. 2016;29:923-927. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Cottle L, Riordan T. Infectious spondylodiscitis. J Infect. 2008;56:401-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 245] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 19. | Kang SJ, Jang HC, Jung SI, Choe PG, Park WB, Kim CJ, Song KH, Kim ES, Kim HB, Oh MD, Kim NJ, Park KH. Clinical characteristics and risk factors of pyogenic spondylitis caused by gram-negative bacteria. PLoS One. 2015;10:e0127126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 20. | Abe E, Yan K, Okada K. Pyogenic vertebral osteomyelitis presenting as single spinal compression fracture: a case report and review of the literature. Spinal Cord. 2000;38:639-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Rodiek SO. [Diagnostic methods in spinal infections]. Radiologe. 2001;41:976-986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Modic MT, Feiglin DH, Piraino DW, Boumphrey F, Weinstein MA, Duchesneau PM, Rehm S. Vertebral osteomyelitis: assessment using MR. Radiology. 1985;157:157-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 546] [Cited by in RCA: 408] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 23. | Berbari EF, Kanj SS, Kowalski TJ, Darouiche RO, Widmer AF, Schmitt SK, Hendershot EF, Holtom PD, Huddleston PM 3rd, Petermann GW, Osmon DR. Executive Summary: 2015 Infectious Diseases Society of America (IDSA) Clinical Practice Guidelines for the Diagnosis and Treatment of Native Vertebral Osteomyelitis in Adults. Clin Infect Dis. 2015;61:859-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 108] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 24. | Wirtz DC, Genius I, Wildberger JE, Adam G, Zilkens KW, Niethard FU. Diagnostic and therapeutic management of lumbar and thoracic spondylodiscitis--an evaluation of 59 cases. Arch Orthop Trauma Surg. 2000;120:245-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 52] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 25. | Kwon JW, Hyun SJ, Han SH, Kim KJ, Jahng TA. Pyogenic Vertebral Osteomyelitis: Clinical Features, Diagnosis, and Treatment. Korean J Spine. 2017;14:27-34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 26. | Rosahl SK, Gharabaghi A, Zink PM, Samii M. Monitoring of blood parameters following anterior cervical fusion. J Neurosurg. 2000;92:169-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 27. | Luzzati R, Giacomazzi D, Danzi MC, Tacconi L, Concia E, Vento S. Diagnosis, management and outcome of clinically- suspected spinal infection. J Infect. 2009;58:259-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 62] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 28. | Quiñones-Hinojosa A, Jun P, Jacobs R, Rosenberg WS, Weinstein PR. General principles in the medical and surgical management of spinal infections: a multidisciplinary approach. Neurosurg Focus. 2004;17:E1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 40] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 29. | Sakkas LI, Davas EM, Kapsalaki E, Boulbou M, Makaritsis K, Alexiou I, Tsikrikas T, Stathakis N. Hematogenous spinal infection in central Greece. Spine (Phila Pa 1976). 2009;34:E513-E518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 30. | Fraimow HS. Systemic antimicrobial therapy in osteomyelitis. Semin Plast Surg. 2009;23:90-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 99] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 31. | Stein GE. Pharmacokinetics and pharmacodynamics of newer fluoroquinolones. Clin Infect Dis. 1996;23 Suppl 1:S19-S24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 74] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 32. | Lazzarini L, Lipsky BA, Mader JT. Antibiotic treatment of osteomyelitis: what have we learned from 30 years of clinical trials? Int J Infect Dis. 2005;9:127-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 181] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 33. | Bernard L, Dinh A, Ghout I, Simo D, Zeller V, Issartel B, Le Moing V, Belmatoug N, Lesprit P, Bru JP, Therby A, Bouhour D, Dénes E, Debard A, Chirouze C, Fèvre K, Dupon M, Aegerter P, Mulleman D; Duration of Treatment for Spondylodiscitis (DTS) study group. Antibiotic treatment for 6 weeks versus 12 weeks in patients with pyogenic vertebral osteomyelitis: an open-label, non-inferiority, randomised, controlled trial. Lancet. 2015;385:875-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 266] [Cited by in RCA: 316] [Article Influence: 31.6] [Reference Citation Analysis (0)] |
| 34. | Legrand E, Flipo RM, Guggenbuhl P, Masson C, Maillefert JF, Soubrier M, Noël E, Saraux A, Di Fazano CS, Sibilia J, Goupille P, Chevalie X, Cantagrel A, Conrozier T, Ravaud P, Lioté F; Rheumatology Network Organization. Management of nontuberculous infectious discitis. treatments used in 110 patients admitted to 12 teaching hospitals in France. Joint Bone Spine. 2001;68:504-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 96] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 35. | Sato K, Yamada K, Yokosuka K, Yoshida T, Goto M, Matsubara T, Iwahashi S, Shimazaki T, Nagata K, Shiba N; RESEARCH GROUP FOR SPINE AND SPINAL CORD DISORDERS (HONNEKAI). Pyogenic Spondylitis: Clinical Features, Diagnosis and Treatment. Kurume Med J. 2019;65:83-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 36. | Hadjipavlou AG, Mader JT, Necessary JT, Muffoletto AJ. Hematogenous pyogenic spinal infections and their surgical management. Spine (Phila Pa 1976). 2000;25:1668-1679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 480] [Cited by in RCA: 439] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 37. | Ando N, Sato K, Mitsukawa M, Yamada K, Wakioka T, Nagata K. Surgical results of percutaneous suction aspiration and drainage for pyogenic spondylitis. Kurume Med J. 2010;57:43-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 38. | Kim CJ, Kang SJ, Choe PG, Park WB, Jang HC, Jung SI, Song KH, Kim ES, Kim HB, Oh MD, Park KH, Kim NJ. Which tissues are best for microbiological diagnosis in patients with pyogenic vertebral osteomyelitis undergoing needle biopsy? Clin Microbiol Infect. 2015;21:931-935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 39. | Lin Y, Chen WJ, Zhu WT, Li F, Fang H, Chen AM, Xiong W. Single-level lumbar pyogenic spondylodiscitis treated with minimally invasive anterior debridement and fusion combined with posterior fixation via Wiltse approach. J Huazhong Univ Sci Technolog Med Sci. 2013;33:707-712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 40. | Duan K, Qin Y, Ye J, Zhang W, Hu X, Zhou J, Gao L, Tang Y. Percutaneous endoscopic debridement with percutaneous pedicle screw fixation for lumbar pyogenic spondylodiscitis: a preliminary study. Int Orthop. 2020;44:495-502. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 41. | Canouï E, Zarrouk V, Canouï-Poitrine F, Desmoulin U, Leflon V, Allaham W, de Lastours V, Guigui P, Fantin B. Surgery is safe and effective when indicated in the acute phase of hematogenous pyogenic vertebral osteomyelitis. Infect Dis (Lond). 2019;51:268-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 42. | Anastasiadis P, Mojica KD, Allen JS, Matter ML. Detection and quantification of bacterial biofilms combining high-frequency acoustic microscopy and targeted lipid microparticles. J Nanobiotechnology. 2014;12:24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 43. | Segreto FA, Beyer GA, Grieco P, Horn SR, Bortz CA, Jalai CM, Passias PG, Paulino CB, Diebo BG. Vertebral Osteomyelitis: A Comparison of Associated Outcomes in Early Versus Delayed Surgical Treatment. Int J Spine Surg. 2018;12:703-712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 44. | Lin Y, Li F, Chen W, Zeng H, Chen A, Xiong W. Single-level lumbar pyogenic spondylodiscitis treated with mini-open anterior debridement and fusion in combination with posterior percutaneous fixation via a modified anterior lumbar interbody fusion approach. J Neurosurg Spine. 2015;23:747-753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 45. | Aljawadi A, Jahangir N, Jeelani A, Ferguson Z, Niazi N, Arnall F, Pillai A. Management of Pyogenic Spinal Infection, review of literature. J Orthop. 2019;16:508-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 46. | Dimar JR, Carreon LY, Glassman SD, Campbell MJ, Hartman MJ, Johnson JR. Treatment of pyogenic vertebral osteomyelitis with anterior debridement and fusion followed by delayed posterior spinal fusion. Spine (Phila Pa 1976). 2004;29:326-32; discussion 332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 131] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 47. | Hee HT, Majd ME, Holt RT, Pienkowski D. Better treatment of vertebral osteomyelitis using posterior stabilization and titanium mesh cages. J Spinal Disord Tech. 2002;15:149-56; discussion 156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 130] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 48. | Heyde CE, Boehm H, El Saghir H, Tschöke SK, Kayser R. Surgical treatment of spondylodiscitis in the cervical spine: a minimum 2-year follow-up. Eur Spine J. 2006;15:1380-1387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 69] [Article Influence: 3.6] [Reference Citation Analysis (0)] |