Published online May 26, 2023. doi: 10.12998/wjcc.v11.i15.3560
Peer-review started: January 29, 2023
First decision: March 14, 2023
Revised: March 23, 2023
Accepted: April 14, 2023
Article in press: April 14, 2023
Published online: May 26, 2023
Processing time: 116 Days and 13.9 Hours
Primary abdominal and retroperitoneal cavernous hemangioma is a vascular tumor and rarely seen in the clinic. Due to the lack of specific imaging features, retroperitoneal cavernous hemangioma cannot be diagnosed accurately. Some symptoms may develop with the enlargement of lesion volume or the occurrence of complications such as rupture or oppression. We report here a special case who was admitted with chronic abdominal pain. Admission examination suggested a retroperitoneal lymphatic duct cyst. Laparoscopic resection of the retroperitoneal mass was performed, and histological examination confirmed retroperitoneal cavernous hemangioma.
The patient was a 43-year-old Tibetan woman with intermittent left lower abdominal pain and discomfort 3 years ago. Ultrasonography revealed a cystic mass in the retroperitoneum with clear boundaries, internal septa, and no blood flow signal. Computed tomography (CT) and magnetic resonance imaging (MRI) showed an irregular space-occupying mass in the retroperitoneum, and retroperitoneal lymphatic cyst was considered. Plain CT scanning showed multiple cyst-like hypo-intense shadows in the retroperitoneum, partially fused into a mass, and no obvious enhancement was found on enhanced scanning. MRI showed multiple irregular clump-like long T1 and long T2 signal shadows above the pancreas, within which linear short T2 signal shadows were seen. Diffusion-weighted imaging sequence showed hypo-signal shadows, without obvious enhancement on enhanced scanning. Ultrasound, CT, and MRI all suggested the possibility of retroperitoneal lymphatic cyst. However, the patient was finally diagnosed with retroperitoneal cavernous hemangioma by pathological exa
Retroperitoneal cavernous hemangioma is a benign lesion, and it is difficult to make a diagnosis preoperatively. Surgical resection may be the only treatment, which not only allows histopathological confirmation as a diagnostic purpose and excludes any risk of malignancy, but also avoids invasion of adjacent tissues, oppression, and other complications as a therapeutic goal.
Core Tip: In this report, we describe a case of retroperitoneal cavernous hemangioma misdiagnosed as retroperitoneal lymphangioid cyst preoperatively.
- Citation: Hou XF, Zhao ZX, Liu LX, Zhang H. Retroperitoneal cavernous hemangioma misdiagnosed as lymphatic cyst: A case report and review of the literature. World J Clin Cases 2023; 11(15): 3560-3570
- URL: https://www.wjgnet.com/2307-8960/full/v11/i15/3560.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i15.3560
Cavernous hemangioma is a benign vascular neoplasm consisting of proliferative vascular endothelial cells characterized by abnormal angiogenesis[1], with a propensity for orbital region, liver, brain cadres, and skin involvement but rarely involving the retroperitoneum[2-6]. Cavernous hemangiomas can occur at any age[7] and grow rapidly in infancy, but may spontaneously degenerate late in life[8,9]. In the early stage, most patients tend to be asymptomatic, while as the tumor grows, patients require hospital management due to the presence of oppressive symptoms such as pain, nausea, and vomiting. Cavernous hemangioma has diverse imaging features. Ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) contribute to the initial identification and localization of pathological lesions. However, it is difficult to make a definitive diagnosis of retroperitoneal cavernous hemangioma by any non-surgical modality, and this disease is often misdiagnosed as adenocarcinoma, neuroendocrine tumors, or other solid pancreatic entities. In the case that we report here, the patient was preoperatively diagnosed with a retroperitoneal lymphatic duct cyst.
Despite the benign nature of cavernous hemangioma, the case that we report had suffered from long-term intermittent pain and discomfort. Hence, we chose to perform space-occupying lesion resection under laparoscopy. Here, we also performed a literature review of the diagnosis and treatment of retroperitoneal cavernous hemangioma and retroperitoneal lymphatic cyst in recent years and made a comparison between them.
A 43-year-old woman of Tibetan ethnicity was admitted to the hospital with a 3-year history of pain and discomfort in the left lower abdomen and aggravation in recent 1 year.
The pain was not obvious at the time of admission examination 3 years ago, so the patient did not receive further treatment.
The patient underwent tubal ligation 20 years ago, with no history of acute pancreatitis, abdominal trauma, chronic diseases, or infectious diseases.
The patient denied any family history of malignant tumours.
Admission physical examination revealed: Normal body temperature, respiration, and blood pressure, and a pulse rate of 65 beats/min; good nutritional status; flat abdomen, no intestinal pattern and peristaltic waves, and no varicose veins in the abdominal wall; soft abdomen, with left lower abdominal tenderness, no muscle tension and rebound pain, no palpable liver or spleen under the ribs, no abnormal masses palpated in the abdomen, and Murphys' sign negativity; no shifting dullness, with normal bowel sounds, and no air-over-water sounds or abnormal vascular murmurs.
Laboratory tests after admission indicated that routine blood indexes, tumor markers, and biochemical indicators were all within normal range.
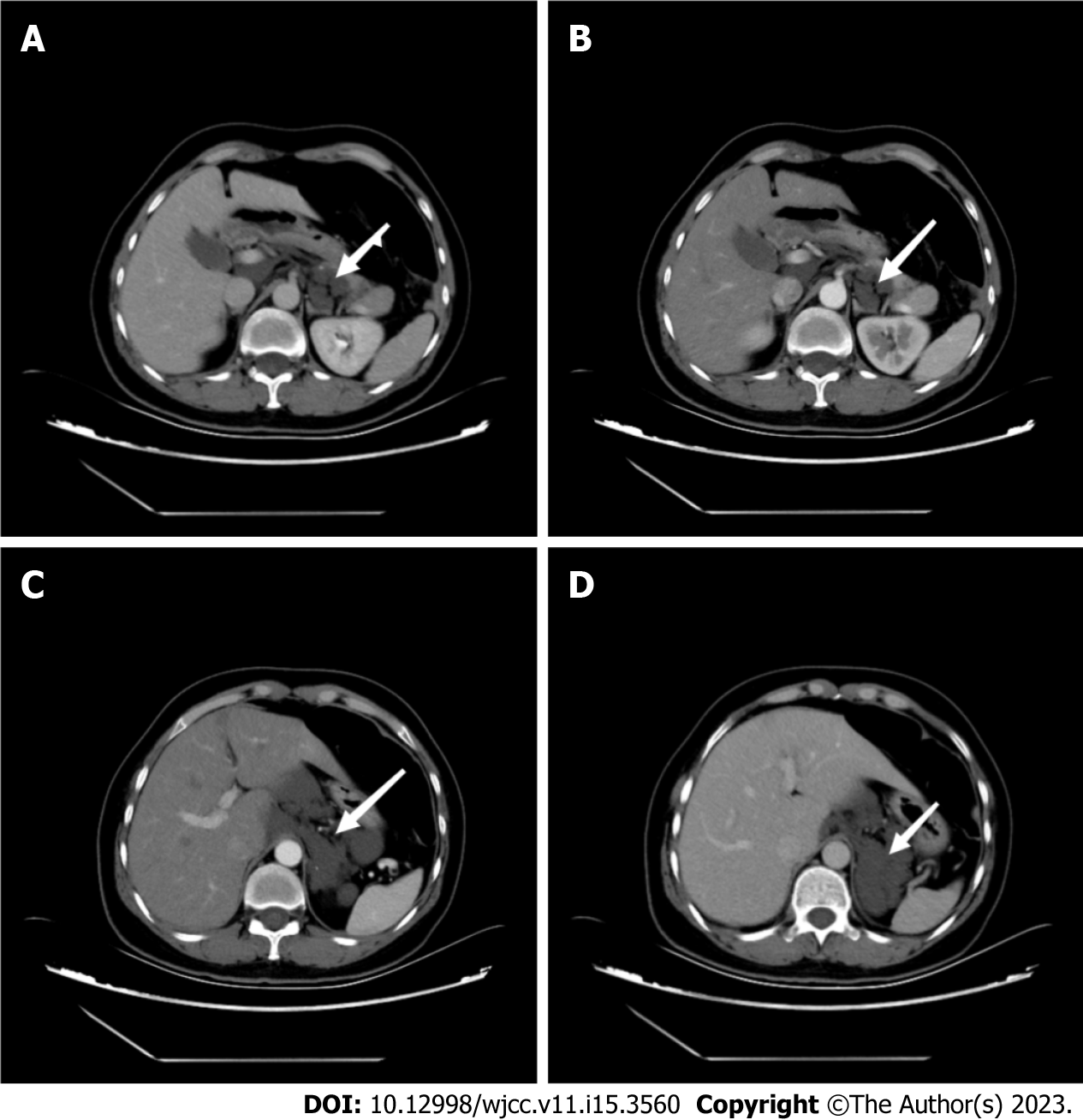
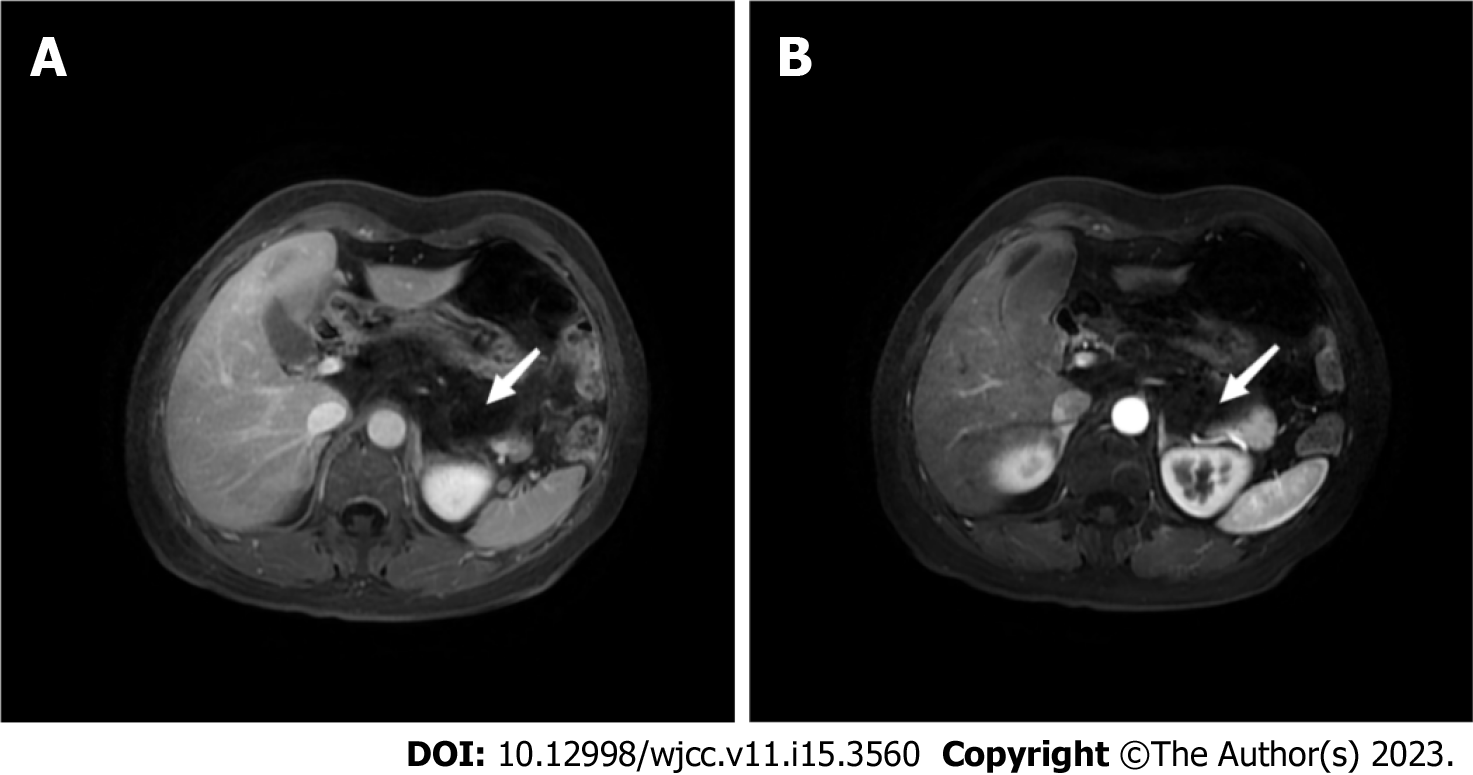
On ultrasonography, a retroperitoneal cystic mass with a size of 88 mm × 62 mm was seen, with clear borders and internal separation, and no significant blood flow signal was observed on color Doplor flow image. Enhanced CT showed multiple retroperitoneal cystic hypo-intense shadows, partially fused into a mass of approximately 46 mm × 35 mm in size, with no significant enhancement on enhancement (Figure 1). MRI showed multiple irregular masses of long T1 and long T2 signal shadows above the pancreas, within which linear short T2 signal shadows were seen. The diffusion-weighted imaging sequence showed hypo-signal shadows (Figure 2). The retroperitoneal layer was clear without obviously enlarged lymph nodes. These imaging findings did not suggest evidence of mass invading surrounding organs or retroperitoneal lymphadenopathy.
The preoperative diagnosis was retroperitoneal lymphatic duct cyst. Laparoscopic resection of the retroperitoneal mass was performed after surgical evaluation.
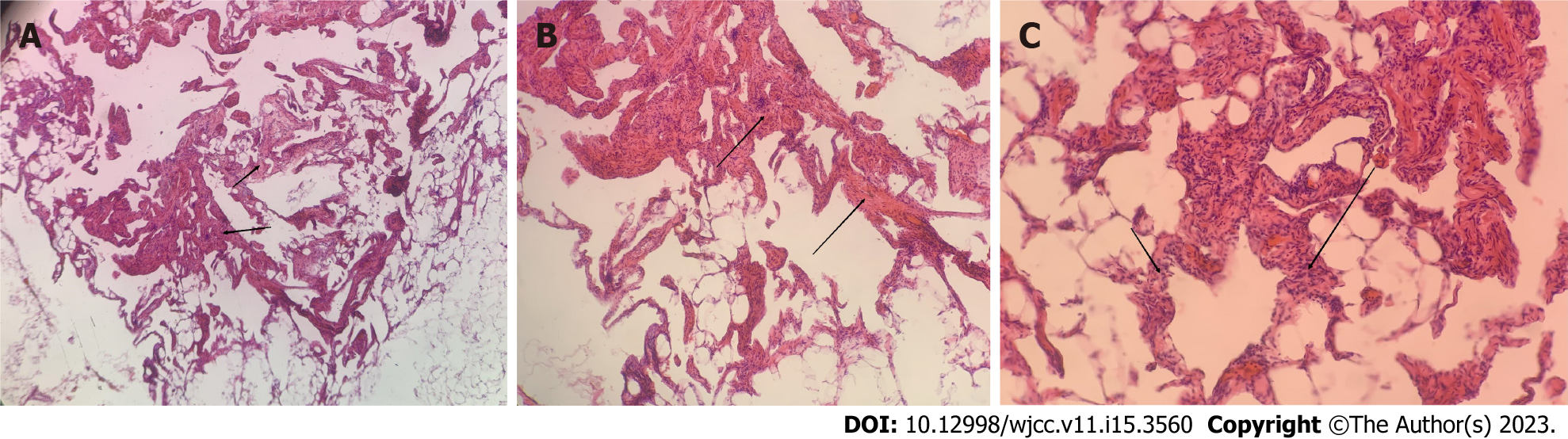
During the operation, a soft cystic tumor above and posterior to the pancreas was found, which was closely connected with the inferior vena cava. The size of the tumor was about 6 cm × 7 cm, and it was prone to bleeding when touched. Reddish fluid was seen in the cyst, and the tumor envelope was intact (Figure 3). Microscopically, blood vessels with different lumen sizes and uneven wall thickness were seen in the tissues, and coagulation was seen in some vessels, conforming to the morphology of cavernous hemangioma, and a small amount of adipose tissue was seen around (Figure 4). Immunohistochemistry revealed CD34 (+), CD31 (+), SMA (+), and Desmin (partially +).
The histopathology confirmed the diagnosis of retroperitoneal cavernous hemangioma.
In this report, we describe a case of retroperitoneal cavernous hemangioma misdiagnosed as retroperitoneal lymphangioid cyst preoperatively. Retroperitoneal tumors are extremely rare, accounting for less than 0.2% of all tumor types[10]. This disease mainly originates from the fat tissue, loose connective tissue, and fascia of the abdominal cavity. Hemangiomas located in the mesentery and gastrointestinal tract can invade outwardly the peritoneal cavity[11,12]. Liposarcoma is the most common tumor located in the retroperitoneal space. Among the malignant tumors of the retroperitoneum, liposarcoma and leiomyosarcoma are most frequently seen, while teratomas, cysts, and neuromas are the common benign tumors[3,13-14]. Vascular tumors include lymphangioleiomas, hemangiomas, lymphangioidomas, hemangiotheliomas, and hemangioblastomas, all of which are benign lesions with slow growth and few malignant changes. These lesions are commonly found in the skin, eyes, liver, brain, spleen, and other organs, while cavernous hemangioma is extremely rare[15].
The majority of cavernous hemangiomas often do not exhibit obvious clinical symptoms in the early stage due to the small volume of the space-occupying lesion. Non-specific symptoms, such as abdominal pain and anemia, present only when oppressive symptoms or invasion of adjacent tissues occur[16]. A few patients may be admitted due to lower back pain or gastrointestinal bleeding[17]. In the literature that we review, there are 6 cases of cavernous hemangiomas primarily originating from the adrenal gland[18-23], 12 cases of cavernous hemangiomas primarily originating from the pancreas[24-32], 3 cases of primary retroperitoneal cavernous hemangioma[33-35], 7 cases unspecified[14,36-41], and 1 case originating from the psoas major muscle[42]. Detailed clinical data are shown in Table 1.
| No. | Gender | Age | Ultrasonic | CT | MRI | Positive sign | Preoperative diagnosis | Postoperative pathology | Ref. |
| 1 | Male | 20 | Small amount of low-velocity blood flow signal in the tumor with heterogeneous echogenicity | No | No | No | Retroperitoneal cavernous hemangioma | Cavernous hemangioma (lumbar major muscle origin) | [44] |
| 2 | Female | 51 | No | The edges of the mass are clear and smooth, with heterogeneous density, mild enhancement at the edge of enhancement, and nodular significant enhancement seen internally | The lesion shows delayed marked enhancement | Pain in the right lower abdomen, numbness and pain in the right lower extremity | Neurogenic tumor? | Cavernous hemangioma | [37] |
| 3 | Female | 16 | No | No | No | Fresh blood stools, black stools, severe anemia | Hemorrhoids? Colonic vasodilatation? | Cavernous hemangioma | [38] |
| 4 | Male | 35 | No | Uniform density mass. Homogeneous enhancement is seen | Smooth margins of the mass and uniform internal signal | Abdominal pain | Adrenal tumors; tumors of vascular origin; tumors of neurological origin; adrenal pheochromocytoma? | Cavernous hemangioma | [39] |
| 5 | Male | 57 | No | Isointense-slightly hypointense shadow of the right adrenal gland with clear margins, lobulated, heterogeneous density, nodular enhancement | No | Elevated blood pressure | Cortical cancer? | (Right adrenal gland) cavernous hemangioma | [19] |
| 6 | Male | 14 | Clearly defined mass with internal cystic mass and no significant blood flow signal | Hematoma in the right adrenal region | No | No | Tumor with hemorrhage | Hemangioma (left adrenal gland) with hemorrhagic necrosis | [20] |
| 7 | Male | 57 | No | Uneven density masses | No | Left upper abdominal pain | Left adrenocortical carcinoma, pheochromocytoma? Retroperitoneal mesenchymal-derived tumor? | Hemangioma (left adrenal gland) with hemorrhagic necrosis | [21] |
| 8 | Female | 70 | No | Clearly defined mass with heterogeneous density and scattered foci of speckled calcification at the margins; enhanced lesions with heterogeneous enhancement and multiple foci of nodular hyperenhancement at the periphery | No | Abdominal pain | Giant retroperitoneal occupancy with consideration of benign tumor of adrenal origin | (Left adrenal) cavernous hemangioma; immunohistochemistry: Vim (+) | [22] |
| 9 | Female | 47 | No | The density of the mass is uneven, and vascular shadow is seen in enhancement | T1W1 low signal, T2W1 heterogeneous high signal, lesion is heterogeneously reinforced, vascular shadow is seen | Abdominal distension, abdominal pain | Malignant tumors | Cavernous hemangioma with bleeding; Immunohistochemistry: CD31 (+); CD34 (+), CD2-40 (+), ERG (+), SMA (+) | [40] |
| 10 | Female | 71 | Irregular hypoechoic solid occupying lesion of the pancreas | Heterogeneous hypodense lesion in the pancreatic neck with clear borders and marked enhancement | No | Abdominal pain | No | Pancreatic cavernous hemangioma; immunohistochemistry: CD31 (+), CD34 (+), CD2-40 (-) | [25] |
| 11 | Female | 37 | Cystic solid mass | No | No | Abdominal pain | No | Pancreatic cavernous hemangioma | [26] |
| 12 | Female | 63 | Cystic solid mass | No | No | Abdominal pain | Pancreatic cancer | Pancreatic cavernous hemangioma with calcification and cyst formation | [26] |
| 13 | Male | 79 | Cystic solid mass in the head of the pancreas with clear borders, uneven internal echogenicity, scattered multiple echogenic areas, and poor blood flow signal | Occupation of the head of the pancreas with lamellar enhancement and increased delayed enhancement, with multiple microvascular shadows seen within | No | Abdominal pain, abdominal distension | No | Pancreatic cavernous hemangioma | [27] |
| 14 | Male | 55 | Cystic predominant mass in the tail of the pancreas with clear borders. Irregular shape, no obvious blood flow signal | Hypodense lesion in the body of the pancreas | Cystic occupying lesion in the body of the pancreas | Abdominal pain | Cystadenoma, cyst? | Pancreatic cavernous hemangioma | [28] |
| 15 | Male | 49 | No | A round-like hypodense lesion is seen in the neck of the pancreas, and enhancement is seen | Pancreatic neck occupancy with clear margins and homogeneous signal; enhancement is not obvious | Pain in the lower back and lower right abdomen | Pancreatic cancer? | Pancreatic cavernous Hemangioma | [29] |
| 16 | Female | 58 | No | Plain scan shows a round-like hypodense mass in the tail of the pancreas with well-defined borders, and moderate enhancement in the arterial phase and "thin thread-like" moderate enhancement in the venous and delayed phases | A round-like lesion was seen in the tail of the pancreas, with uniform low signal on T1WI and high signal on T2WI, and a little bit of slightly low signal was seen inside (DW1 showed slightly high signal, and mild to moderate patchy enhancement was seen inside the lesion) | Abdominal distension, abdominal pain, jaundice | Cystadenoma of the pancreas | Pancreatic cavernous hemangioma | [30] |
| 17 | Male | 66 | The envelope was intact and continuous, and multiple irregular echogenic areas were visible inside, separated by hyperechoic structures | A large round-like hypodense mass in the right upper abdomen with clear borders and nodular irregular enhancement around the mass in the arterial phase | A round abdominal abnormal signal shadow with well-defined borders, T1-weighted moderately low signal and nodular low signal in the periphery; T2-weighted mass is predominantly high signal, with striated low signal inside. After enhancement, T1-weighted nodular enhancement was seen in the periphery, and the enhancement became more obvious on delayed scan and expanded inward. There was no central enhancement on both scans | Symptomless | Cavernous hemangioma | Adrenal cavernous hemangioma | [31] |
| 18 | Female | 54 | Strongly echogenic mass in the right posterior lobe of the liver with clear boundaries and uneven internal echogenicity | A rounded hypointense shadow is seen in the right adrenal area, and a more hypointense area with clear borders is visible within it; the periphery of the lesion is mildly enhanced | The oval-shaped mass between the liver and the right kidney is hyposignal on T1WI, with an eccentric more hyposignal area within it; it is high-signal on T2WI, with a well-defined border and a non-enhancing hyposignal area within it | Abdominal pain | Retroperitoneal space-occupying lesions (malignant) | Primary retroperitoneal cavernous hemangioma | [34] |
| 19 | Female | 60 | Cystic | Slightly hypointense shadow with inconspicuous enhancement | No | Abdominal pain, fever | Cystic lesion of the tail of the pancreas. Cystic adenoma? Cystic adenocarcinoma? | Pancreatic cavernous hemangioma | [32] |
| 20 | Female | 41 | Cystic solid | No | No | Medical examination | Cystic dominant cystadenoma or islet cell carcinoma in the body of the pancreas | Pancreatic cavernous hemangioma | [32] |
| 21 | Female | 30 | Cystic solid | No | No | Abdominal pain, choking on food | Cystic solid occupancy of the head of the pancreas is likely to be benign | Pancreatic cavernous hemangioma | [32] |
| 22 | Female | 57 | Uneven hypoechoic | Uneven reinforcement | No | No | Gastrointestinal mesenchymal tumors (GISTs), carcinoid tumors, neurogenic tumors, metastatic lymphadenopathy, or other rare tumors | Retroperitoneal cavernous hemangioma | [41] |
| 23 | Male* | 63 | Mixed echogenicity within the indistinct contour of the head of the pancreas, CDFI shows hyperechoic and visible blood flow within the separation | A well-defined cystic mass in the head of the pancreas with foci of internal calcification | No | Abdominal pain, constipation | Pancreatic cavernous hemangioma | [33] | |
| 24 | Male | 36 | Uneven echoes | Tumor between the dorsal head of the pancreas and right kidney without significant enhancement | Lower signal in the tumor, some relatively high intensity areas | Abdominal pain | Retroperitoneal sarcoma | Cavernous hemangioma; Immunohistochemistry: CD31 (+), CD34 (+), CD2-40 (partially +) | [42] |
| 25 | Male | 35 | No | Well-defined, cyst-like masses, no enhancement of the mass wall in the arterial and portal phases, persistent hypodensity of the mass | No | Abdominal pain | Benign tumors such as lymphangioma cysts, GISTs, or primitive retroperitoneal benign tumors | Primary retroperitoneal cavernous hemangioma; Immunohistochemistry: CD31 (+), CD34 (+), DOG1 (-), CD117 (-) | [35] |
| 26 | Female | 71 | No | Low density, no enhancement | No | Lower limb edema, dyspnea, abdominal distention, anemia | Retroperitoneal cavernous hemangioma; Immunohistochemistry: CD34 (+) | [43] | |
| 27 | Male | 70 | No | Uniform density, surrounding calcification | (a) Molecular water diffusion limitation within the lesion on T2 fat-saturated weighted image; (b) high signal intensity intra-lesion region on T1 fat-saturated weighted image; (c) high signal region on enhanced T1 fat-saturated weighted image; (d) inhomogeneous enhancement | Physical examination | Adrenal cavernous hemangioma | [23] | |
| 28 | Male | 67 | No | Clearly defined mass with significant peripheral enhancement in the early arterial phase | No | Back pain | Adrenal tumor, pheochromocytoma | Adrenal cavernous hemangioma | [24] |
| 29 | Male | 38 | No | Cyst-like, well-enveloped tumor with mildly enhancing walls in the portal phase | No | Abdominal pain | Primary retroperitoneal cavernous hemangioma; Immunohistochemistry: CD31 (+), Vim (+) | [36] |
The imaging manifestations of cavernous hemangioma are also varied. On ultrasound, cavernous hemangioma is often manifested as internal hypo-echo or irregular mixed echo, usually with no or low blood flow signal, so it is difficult to determine the nature of the lesion. CT and MRI are extensively used for preoperative diagnosis of cavernous hemangioma. Usually, hemangiomas can be significantly enhanced in the arterial phase on CT. However, pancreatic cavernous hemangioma is a cystic tumor that usually contains neurovascular components, with an arteriovenous shunt, and lacks larger supply vessels, which may result in the absence of enhancement in the arterial phase[32]. Also, the different proportions of cystic and solid components in the tumor may lead to different degrees of enhancement in the arterial phase[43]. Only a small number of patients show characteristic changes, and it is usually difficult to make a diagnosis by imaging means. CT scan can locate the tumor and distinguish the density changes of the tumor, but origin determination and qualitative diagnosis can hardly be realized. It is also because cavernous hemangioma lacks enough characteristic imaging manifestations that it is easy to be misdiagnosed.
Retroperitoneal lymphatic cyst usually presents as a large, thin-walled, multi-septal cystic mass, with fluid content varying from fluid to fat attenuation. The elongated shape and crossover from the retroperitoneal compartment to the adjacent area are the characteristics of the mass. Few cystic lymphangiomas have wall calcification[44], and there is no gold standard for diagnosis.
Currently, the gold standard for the diagnosis of retroperitoneal cavernous hemangioma is still pathological examination. Microscopically, cavernous hemangioma is mainly composed of dilated abnormal sinuses lined with monolayer vascular endothelial cells and incompletely spaced fibrous tissues within the sinuses, forming a sponge-like structure[45,46]. Depending on the size of the vascular spaces, they can be capillary or spongy. In immunohistochemistry, CD31- and CD34-positivity suggests benign vascular tumors such as hemangiomas and lymphangioleiomas, and D2-40-negativity excludes lymphangioleiomas.
There is no need for further treatment or surgical intervention when retroperitoneal hemangioma is asymptomatic, but further surgical treatment is needed when the tumor grows rapidly, oppresses adjacent organs, or develops non-specific symptoms[47]. Unlike the polycythemia exhibited by hemangiomas originating from other regions, retroperitoneal cavernous hemangioma is mostly ischemic. It is generally considered to be associated with asymptomatic episodes[48]. Due to the difficulty in diagnosing retroperitoneal cavernous hemangioma, it is necessary to fully understand the imaging features of retroperitoneal hemangioma and combine them with relevant clinical and laboratory tests to exclude the possibility of malignant tumor, thereby reducing the surgical or postoperative complications. The surgical modality should be selected according to the location of the tumor and its proximity to the adjacent tissues. If the tumor is large or invades the adjacent organs, interventional treatment can be chosen accordingly; relatively, in the presence of symptoms of gastrointestinal or biliary tract obstruction, pancreaticoduodenectomy, gastrojejunostomy, or choledochojejunostomy can be performed to relieve the obstruction if necessary.
Overall, although retroperitoneal cavernous hemangioma is a benign lesion, it is difficult to make a diagnosis preoperatively. Surgical resection may be the only treatment, which not only allows histopathological confirmation as a diagnostic purpose and excludes any risk of malignancy, but also avoids invasion of adjacent tissues, oppression, and other complications as a therapeutic goal.
Overall, although retroperitoneal cavernous hemangioma is a benign lesion, it is difficult to make a diagnosis preoperatively. Surgical resection may be the only treatment, which not only allows histopathological confirmation as a diagnostic purpose and excludes any risk of malignancy, but also avoids invasion of adjacent tissues, oppression, and other complications as a therapeutic goal.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Moshref L, Saudi Arabia; Surani S, United States S-Editor: Liu JH L-Editor: Wang TQ P-Editor: Zhao S
| 1. | Zheng JW, Zhou Q, Yang XJ, Wang YA, Fan XD, Zhou GY, Zhang ZY, Suen JY. Treatment guideline for hemangiomas and vascular malformations of the head and neck. Head Neck. 2010;32:1088-1098. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 80] [Article Influence: 5.3] [Reference Citation Analysis (1)] |
| 2. | Fujimoto K, Oshima J, Katayma K, Tei N, Harada Y, Nishimura K, Kiyokawa H, Kodama Y, Mano M. [A Case of Retroperitoneal Cavernous Hemangioma Difficult to Differentiate from Retroperitoneal Liposarcoma]. Hinyokika Kiyo. 2017;63:521-524. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Korumilli R, Reddy G. A rare case of retroperitoneal cavernous hemangioma. Int Surg J. 2014;1:37-38. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Matsuda D, Iwamura M, Baba S. Cavernous hemangioma of the adrenal gland. Int J Urol. 2009;16:424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Weidenfeld J, Zakai BB, Faermann R, Barshack I, Aviel-Ronen S. Hemangioma of pancreas: a rare tumor of adulthood. Isr Med Assoc J. 2011;13:512-514. [PubMed] |
| 6. | Geenen RW, Den Bakker MA, Bangma CH, Hussain SM, Krestin GP. Sonography, CT, and MRI of giant cavernous hemangioma of the kidney: correlation with pathologic findings. AJR Am J Roentgenol. 2004;182:411-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Gordon FH, Watkinson A, Hodgson H. Vascular malformations of the gastrointestinal tract. Best Pract Res Clin Gastroenterol. 2001;15:41-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 88] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 8. | Haik BG, Karcioglu ZA, Gordon RA, Pechous BP. Capillary hemangioma (infantile periocular hemangioma). Surv Ophthalmol. 1994;38:399-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 113] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Rosca TI, Pop MI, Curca M, Vladescu TG, Tihoan CS, Serban AT, Bontas EA, Gherghescu G. Vascular tumors in the orbit--capillary and cavernous hemangiomas. Ann Diagn Pathol. 2006;10:13-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Pack GT, Tabah EJ. Primary retroperitoneal tumors: a study of 120 cases. Int Abstr Surg. 1954;99:313-341. [PubMed] |
| 11. | Tai PT, Jewell LD. Case report: mesenteric mixed haemangioma and lymphangioma; report of a case with 10 year follow-up after radiation treatment. Br J Radiol. 1995;68:657-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Ruiz AR Jr, Ginsberg AL. Giant mesenteric hemangioma with small intestinal involvement: an unusual cause of recurrent gastrointestinal bleed and review of gastrointestinal hemangiomas. Dig Dis Sci. 1999;44:2545-2551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | McCallum OJ, Burke JJ 2nd, Childs AJ, Ferro A, Gallup DG. Retroperitoneal liposarcoma weighing over one hundred pounds with review of the literature. Gynecol Oncol. 2006;103:1152-1154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Laih CY, Hsieh PF, Chen GH, Chang H, Lin WC, Lai CM, Chang CH. A retroperitoneal cavernous hemangioma arising from the gonadal vein: A case report. Medicine (Baltimore). 2020;99:e22325. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Le Borgne J, de Calan L, Partensky C. Cystadenomas and cystadenocarcinomas of the pancreas: a multiinstitutional retrospective study of 398 cases. French Surgical Association. Ann Surg. 1999;230:152-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 318] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 16. | Zhao X, Zhang J, Zhong Z, Koh CJ, Xie HW, Hardy BE. Large renal cavernous hemangioma with renal vein thrombosis: case report and review of literature. Urology. 2009;73:443.e1-443.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Chang WT, Lee KT, Yang SF. Cavernous hemangioma of the pancreas: report of a case. Pancreas. 2003;26:310-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Kang WY, Wang L, Qiu M, Zhang F, Guo W, Qiang YY, Tuo PF, Zong YL, Liu LL, Wang SS. [Adrenal cavernous hemangioma: A case report and literature review]. Beijing Da Xue Xue Bao Yi Xue Ban. 2021;53:808-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 19. | Liu YX, Liu YQ. [Ultrasound findings of adrenal cavernous hemangioma complicated with hematoma occurred in one case]. Zhonghua Chaosheng Yixue Zazhi. 2008;209. [DOI] [Full Text] |
| 20. | Li FY, Tang BH. [A case of adrenal cavernous hemangioma complicated with hemorrhagic necrosis]. Radiology Practice. 2014;29:729. [DOI] [Full Text] |
| 21. | Ang L, Wang JZ, Wu YJ, Shi P. [One case of giant cavernous adrenal hemangioma]. Chinese Interventional Imaging and Therapeutics. 2021;18:62. [DOI] [Full Text] |
| 22. | Feo CV, De Troia A, Pedriali M, Sala S, Zatelli MC, Carcoforo P, Feo CF. Adrenal cavernous hemangioma: a case report. BMC Surg. 2018;18:103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 23. | Huang T, Yang Q, Hu Y, Wu HX. Adrenal cavernous hemangioma misdiagnosed as pheochromocytoma: a case report. BMC Surg. 2021;21:210. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 24. | Zhang JP, Liu XM, Liu XH. [A case of a cavernous hemangioma of the pancreas]. Zhongguo Putong Waike Zazhi. 2017;32:996. [DOI] [Full Text] |
| 25. | Fan D, Deng XG, Guo HF, Zhang LT. [Two cases of pancreatic giant cavernous hemangioma were reported]. Zhonghua Putong Waike Zhazhi. 1996;121. |
| 26. | Wu XY, Dai B, Shi XL. [One case of a giant cavernous hemangioma of the pancreas]. Zhonghua Putong Waike Zhazhi. 2020;35:589-589. [DOI] [Full Text] |
| 27. | Dai JQ, Wang J, Chen T. One cavernous hemangioma of pancreatic pancreas [J]. Gandanyi Waike Zazhi. 2009;21:409-410. [DOI] [Full Text] |
| 28. | Fang WK, Luo YH, Li JX, Cao MY, Li ZD. [One cavernous hemangioma of pancreatic pancreas]. Zhonghua Putong Waike Zazhi. 2012;21:1607-1608. |
| 29. | Xiao XY, Zhang K, Li HJ, Li D, Liu HP, Zeng XJ. [One case of pancreatic body tail cavernous hemangioma]. Zhongyi Yingxiang Jishu. 2018;34:1277. [DOI] [Full Text] |
| 30. | Liu GJ, Xu HX, Lu MD, Xie XY, Liu L. [Right adrenal giant unfunctional cavernous hemangioma in 1 case]. Zhonghua Chaosheng Yingxiangxue Zazhi. 2002;60-61. [DOI] [Full Text] |
| 31. | Xu Q, Wang CF, Zhao P, Shan Y, Zhao DB, Liu Q. [Clinical analysis of three cases of pancreatic cavernous hemangioma]. Chin Med J. 2008;28-30. [DOI] [Full Text] |
| 32. | Lianyuan T, Yafeng W, Haibo Y, Yadong D, Jiahao M, Yuanxiang L, Deyu L. Adult pancreatic cavernous hemangioma: case presentation of a benign tumor with a complex composition. BMC Gastroenterol. 2019;19:197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 33. | Meng LP. [One case of primary retroperitoneal cavernous hemangioma]. Zhonghua Fang She Xue Za Zhi. 1998;67. |
| 34. | Debaibi M, Sghair A, Sahnoun M, Zouari R, Essid R, Kchaou M, Dhaoui A, Chouchen A. Primary retroperitoneal cavernous hemangioma: An exceptional disease in adulthood. Clin Case Rep. 2022;10:e05850. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 35. | He H, Du Z, Hao S, Yao L, Yang F, Di Y, Li J, Jiang Y, Jin C, Fu D. Adult primary retroperitoneal cavernous hemangioma: a case report. World J Surg Oncol. 2012;10:261. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 36. | Meng LZ, Wang Q, Xie MQ, Liu J, Xiang LB. [A retroperitoneal invasive giant cavernous hemangioma with lumbosacral nerve invasion occurred in 1 case]. Linchuang Junshi Yixue Zazhi. 2020;48:1119-1120. [DOI] [Full Text] |
| 37. | Wang H, Wan HM, Zhang G, Zhu JJ, He QS, Yang DS. [A retroperitoneal giant cavernous hemangioma involving ileocecum and sigmoid colon]. Zhonghua Waike Zazhi. 2006;1654-1655. [DOI] [Full Text] |
| 38. | Jing JZ, Li HX, Zhang JN. [One case of retroperitoneal hemangioma was reported]. Shiyong Fangshexue Zazhi. 2005;116-119. [DOI] [Full Text] |
| 39. | Huang ZQ, Zhang J, Meng XC, Wu ZM. [One case of pancreatic cavernous hemangioma was misdiagnosed as a pancreatic malignancy]. Gandanyi Waike Zazhi. 2021;33:694-695. [DOI] [Full Text] |
| 40. | Hanaoka M, Hashimoto M, Sasaki K, Matsuda M, Fujii T, Ohashi K, Watanabe G. Retroperitoneal cavernous hemangioma resected by a pylorus preserving pancreaticoduodenectomy. World J Gastroenterol. 2013;19:4624-4629. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 41. | Zielinski J, Haponiuk I, Jaworski R, Peksa R, Irga-Jaworska N, Jaskiewicz J. Retroperitoneal tumor: giant cavernous hemangioma - case presentation and literature review. Kardiochir Torakochirurgia Pol. 2016;13:375-379. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 42. | Zhao YH. [Ultrasound imaging diagnosed one case of retroperitoneal cavernous hemangioma]. Zhonghua Chaosheng Yixue Zazhi. 1999;9. [DOI] [Full Text] |
| 43. | Mundinger GS, Gust S, Micchelli ST, Fishman EK, Hruban RH, Wolfgang CL. Adult pancreatic hemangioma: case report and literature review. Gastroenterol Res Pract. 2009;2009:839730. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 44. | Davidson AJ, Hartman DS. Lymphangioma of the retroperitoneum: CT and sonographic characteristic. Radiology. 1990;175:507-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 123] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 45. | Lu T, Yang C. Rare case of adult pancreatic hemangioma and review of the literature. World J Gastroenterol. 2015;21:9228-9232. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 46. | Mondal U, Henkes N, Henkes D, Rosenkranz L. Cavernous hemangioma of adult pancreas: A case report and literature review. World J Gastroenterol. 2015;21:9793-9802. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 47. | Mathai V, Vyas FL, Jesudason SR. Cavernous haemangioma of the rectum: an uncommon cause of rectal bleeding. Trop Gastroenterol. 2003;24:42-43. [PubMed] |
| 48. | Murakami J, Aoyama K, Nishiki Y, Uotani H, Yamashita J. A case of cavernous hemangioma in the retroperitoneum. Diagnostic Imaging of the Abdomen. 1995;15:811-818. [PubMed] |