Published online May 26, 2023. doi: 10.12998/wjcc.v11.i15.3522
Peer-review started: December 24, 2022
First decision: February 17, 2023
Revised: February 28, 2023
Accepted: April 13, 2023
Article in press: April 13, 2023
Published online: May 26, 2023
Processing time: 152 Days and 13.8 Hours
Digital intraoral scanning, although developing rapidly, is rarely used in occlusal reconstruction. To compensate for the technical drawbacks of current occlusal reconstruction techniques, such as time consumption and high technical requirements, digital intraoral scanning can be used in clinics. This report aims to provide a way of selecting the most suitable maxillo-mandibular relationship (MMR) during recovery.
A 68-year-old man with severely worn posterior teeth underwent occlusal reconstruction with fixed prosthesis using digital intraoral scanning. A series of digital models in different stages of treatment were obtained, subsequently compared, and selected using digital intraoral scanning together with traditional measurements, such as cone beam computed tomography, joint imaging, and clinical examination. Using digital intraoral scanning, the MMR in different stages of treatment was accurately recorded, which provided feasibility for deciding the best occlusal reconstruction treatment, made the treatment process easier, and improved patient satisfaction.
This case report highlights the clarity, recordability, repeatability, and selectivity of digital intraoral scanning to replicate and transfer the MMR during occlusal reconstruction, expanding new perspectives for its design, fabrication, and postoperative evaluation.
Core Tip: Selection of the most appropriate maxillo-mandibular relationship and transfer of occlusal information are crucial steps in occlusal reconstruction. The traditional method is complicated, has high technical sensitivity, and may cause the accumulation of errors. In this case, a digital occlusal relation transfer method was established using digital intraoral scanning to improve the accuracy and efficiency of occlusal reconstruction. This method not only prevents the loss of the optimal maxillo-mandibular relationship but also directly transfers the facial morphology of the temporary prosthesis to the final prosthesis, thus achieving a good transfer of aesthetic and functional information. Digital intraoral scanning makes recording the jaw position relationship between the maxilla and mandible, which is the most important but challenging aspect in the treatment process, clear, recordable, reproducible, and selectable.
- Citation: Hou C, Zhu HZ, Xue B, Song HJ, Yang YB, Wang XX, Sun HQ. New clinical application of digital intraoral scanning technology in occlusal reconstruction: A case report. World J Clin Cases 2023; 11(15): 3522-3532
- URL: https://www.wjgnet.com/2307-8960/full/v11/i15/3522.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i15.3522
Occlusal reconstruction refers to all treatment methods that can change the existing abnormal occlusal contact relationship to restore the patient's normal occlusal function[1]. The key to occlusal recon
A 68-year-old man visited our hospital for crown restoration because of root canal treatment of the upper right posterior teeth 2 wk previously.
The patient’s teeth were worn to varying degrees. One month prior, the patient's upper right posterior teeth developed symptoms of pulpitis due to severe enamel wear and dentin exposure for a long time. He was treated with root canal therapy. He returned to see a dentist for crown restoration.
The patient denied a history of systemic diseases, such as hypertension, coronary heart disease, and diabetes. He reported no history of food or drug allergy, trauma, surgery, or blood transfusion, and his vaccination history was unknown.
No individual or family history of mental illness was reported.
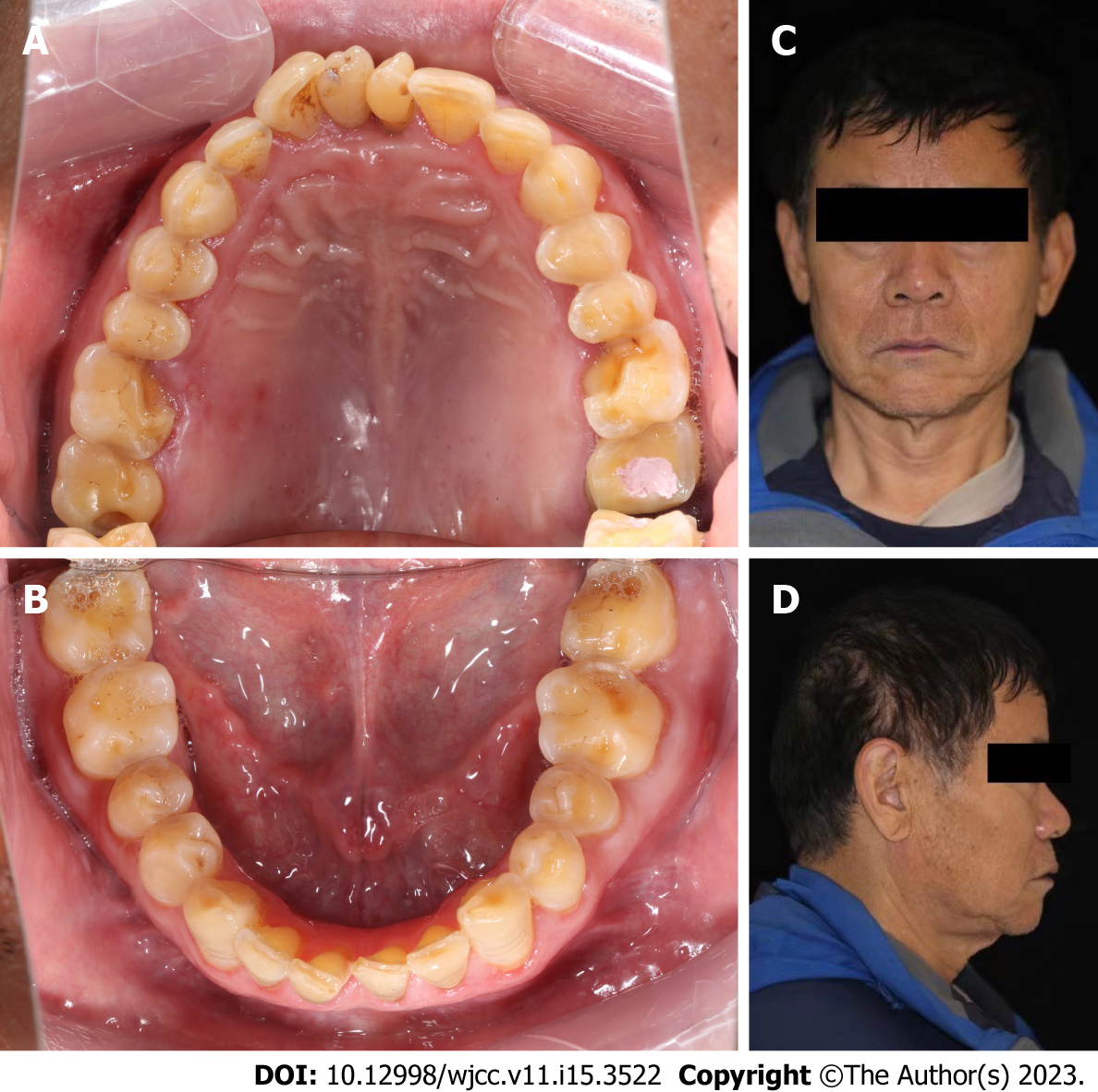
The patient's facial morphology was left-right symmetrical, the lower 1/3 height of the face was shorter, the jaw space at rest was normal, the degree of opening was normal, the opening type was biased at the initial stage of closure, and there was no clicking or tenderness in either joint. The impact force of the bilateral condyles was large, according to the external auditory canal digital examination. All the teeth were worn to varying degrees, overbite and overjet were normal, and the incisal edge was slightly worn. The enamel of 15-17, 26, 27, 36, 37, and 44-47 was worn in large areas, the mesial lingual tips of 16 and 26 were worn to 1 mm below the gum, and most teeth were probe examined (+/-), cold stimulated (-), and percussed (-). Dental plaque 1°, dental calculus (+), pigment segment (+), and localized gingival congestion and swelling were observed. There were no loose teeth, and the periodontal probing depth was 2-4 mm (Figure 1).
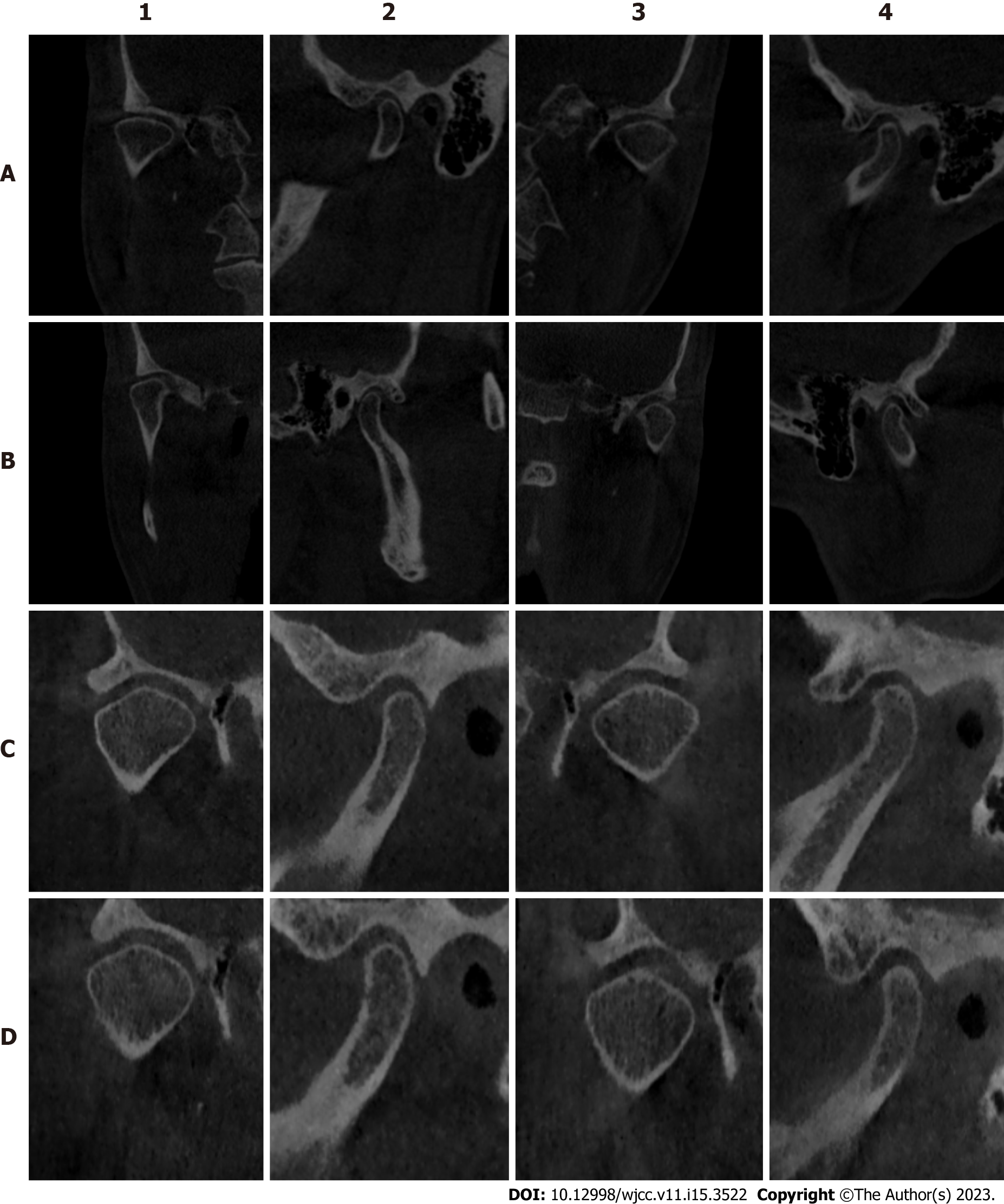
Initial temporomandibular joint CBCT: The posterior space of both temporomandibular joints was narrow, the anterior space increased, the upper space increased slightly, and the condyle moved backward and upward (Figure 2A).
CBCT of the temporomandibular joint when wearing the occlusal pad: The anterior space of the joint decreased, the posterior space increased, the upper space slightly increased, and the condyle moved forward and downward. The left joint space was normal, and the right posterior joint space improved compared with when not wearing the occlusal pad (Figure 2B).
CBCT of the temporomandibular joint 1 mo after wearing the temporary crowns: The left joint space was normal, and the right posterior joint space was slightly wider than when wearing the jaw pad (Figure 2C).
CBCT of the temporomandibular joint after bonding the final denture: The left joint space was normal, the right posterior joint space was wider than before, and the bilateral temporomandibular joint space was improved (Figure 2D).
Heavy abrasion.
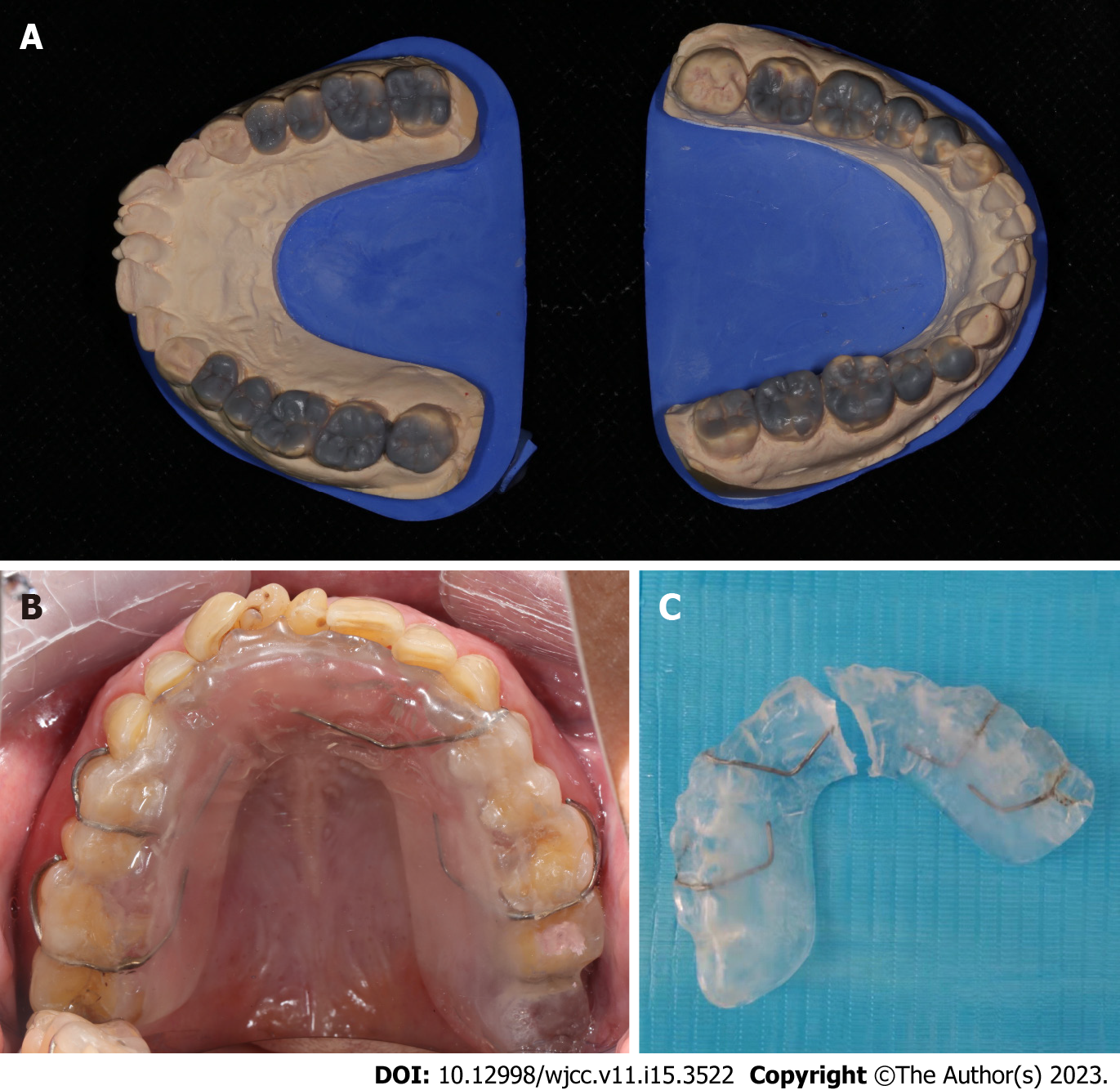
CBCT was performed before restoration (Figure 2A). Upper and lower alginate impressions were taken, the occlusal relationship was recorded, facial arch was transferred to the articulator, the lifting distance was analyzed and determined, and a dental diagnostic wax-up of 14-17, 24-27, 34-37, and 44-47 was made (Figure 3A), including the occlusal relationship, cusp and fossa relationship, and aesthetic adjustment. Simultaneously, the jaw pad was made according to the same jaw position relationship.
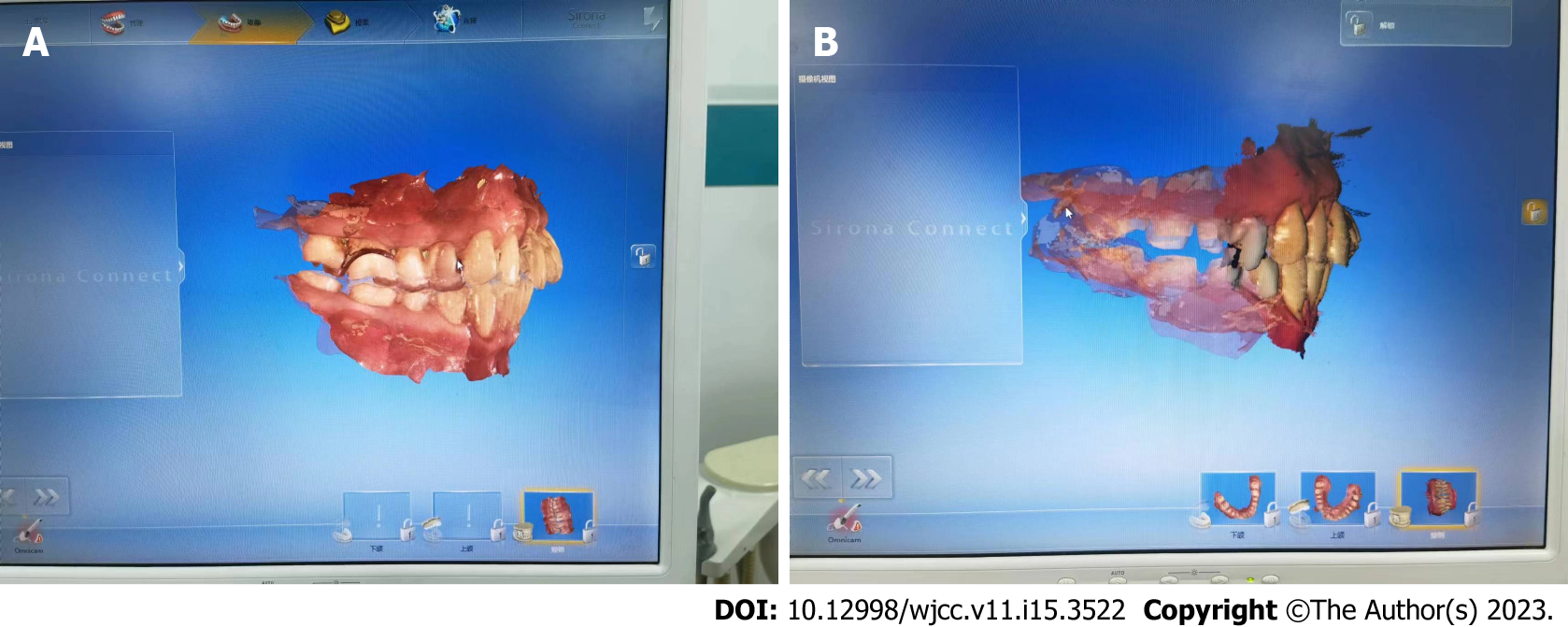
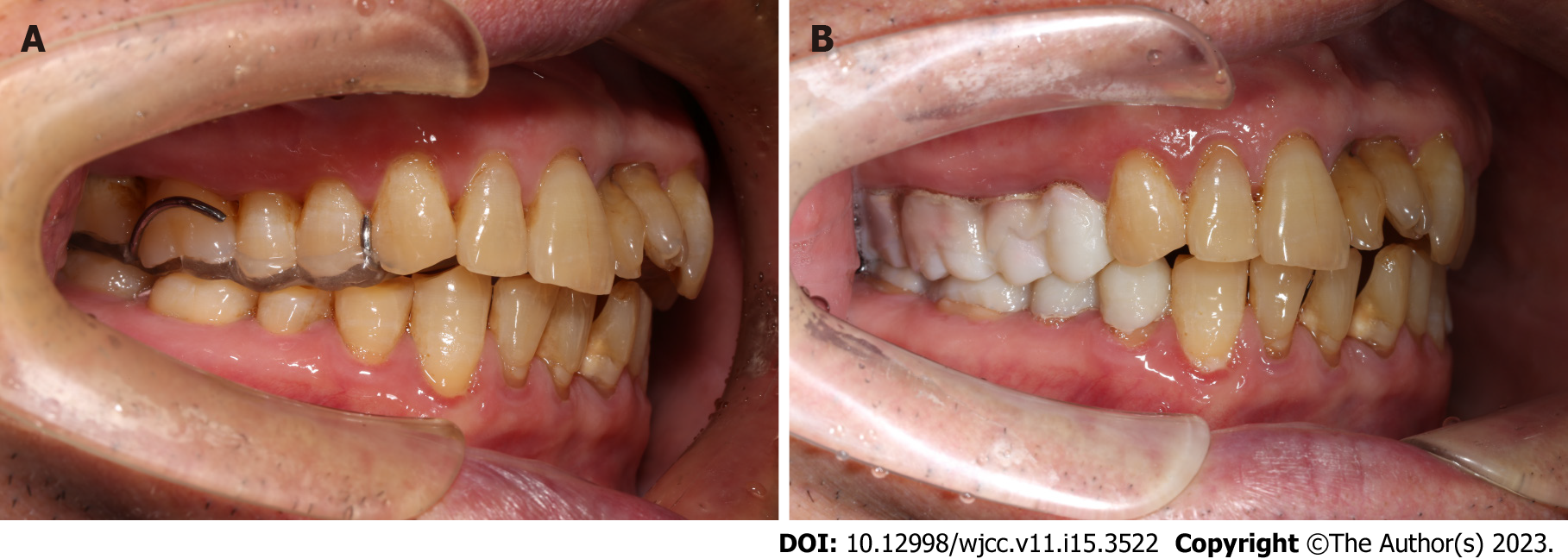
The patient wore a maxillary occlusal pad and was instructed to visit once a week (Figure 3B). After wearing an occlusal pad for 3 mo, the patient reported no discomfort, and CBCT of the temporomandibular joint was performed (Figure 2B). At that time, the patient wore an occlusal pad for a digital intraoral scan (Figure 4A).
The occlusal pad was divided into two at the central line for standby (Figure 3C). According to the principle of segmented preparation, tooth preparation was first performed. Referring to the Zhao et al[6] method of facial arch transfer to a cross-mounting articulator, the adapted jaw position and vertical distance records determined by the transitional treatment were transferred to the articulator, and temporary restorations for 14-17, 24-27, 34-37, and 44-47 for routine adjustments were made (Figure 5).
After using the temporary crowns for 1 mo, CBCT of the temporomandibular joint was performed (Figure 2C). Joints, masticatory muscles, occlusal contact, and periodontal health of the teeth were re-evaluated, and formal restoration after full communication with the patient was commenced. Digital intraoral scanning models were then taken with the temporary crowns (Figure 4B).
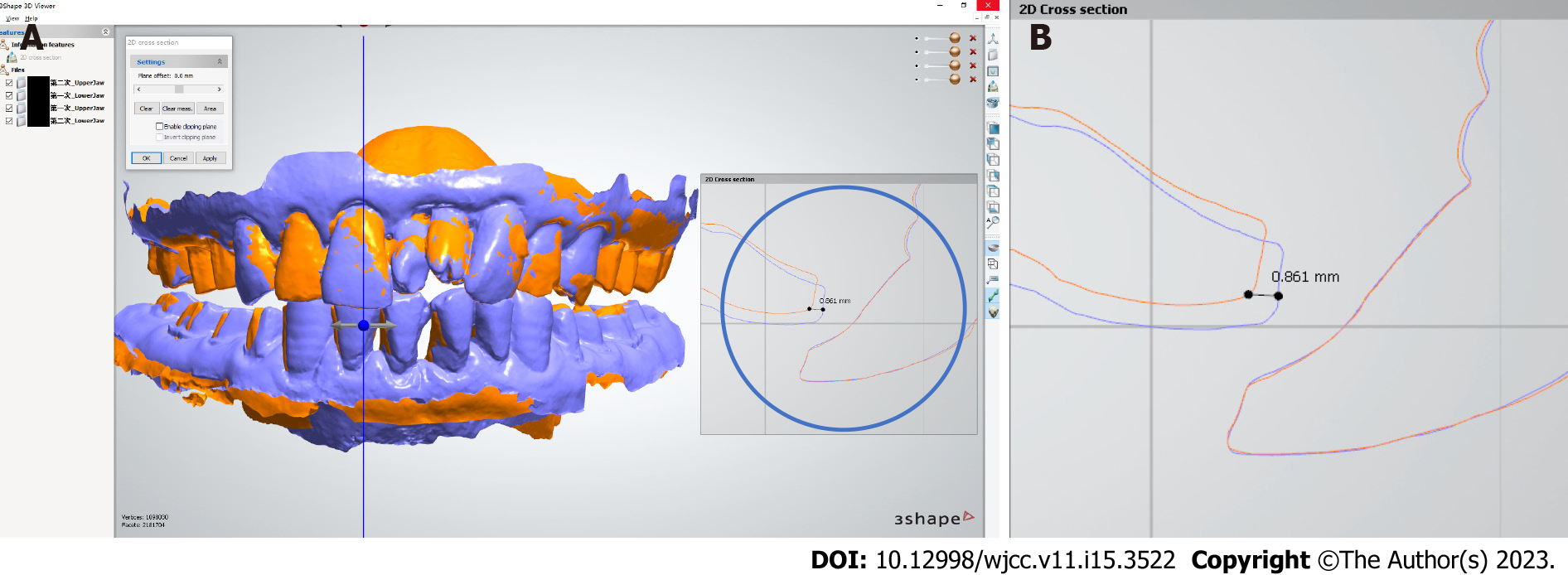
Before the final restoration was made, the most suitable MMR to meet the requirements of the patient was determined. After completion of the above steps, two occlusal reconstruction models were obtained and retained through digital intraoral scanning (Figure 4). To select the most suitable model for occlusal reconstruction of the patient, comparisons were made using Shape 3D viewer software. With the image of the upper jaw used as the reference coordinate for the comparisons, the models overlapped each other in the same spatial position (Figure 6A). The yellow model was the jaw position relationship obtained with the occlusal pad, while the blue model was obtained after wearing the temporary crowns. A locally amplified image (Figure 6B) illustrated the difference in the MMR; the anterior edge of the lateral labial margin of the mandibular central incisor was shifted upward and medially by approximately 0.861 mm in the MMR with the temporary crowns compared with that with the occlusal pad. In addition, at the end of the mock-up phase, the occlusal reconstruction vertical distance decreased, overjet decreased slightly, and the patient had a more comfortable bite (Figure 7). Finally, we determined that the occlusal relationship of the second oral scan was most suitable for the final restoration and reconstruction for the patient.
After removing the temporary crowns, 16 altron all-ceramic crowns were used. In addition, other aspects such as decreased overjet and better condylar position resulted in a more comfortable bite and a pleasing appearance.
Eventually, after wearing the all-ceramic crowns for 2 wk, the patient felt beautiful and comfortable, without obvious discomfort or temporomandibular joint-related symptoms, and underwent CBCT (Figure 2D). At 1 mo follow-up visit, the patient's face shape was normal, the muscle strength of both sides of the maxillofacial region was symmetrical, and the occlusal relationship was excellent during oral examination. The jaw position did not slide during clenching compared with the jaw position during light bite. The patient reported an improved quality of life after treatment. A re-evaluation visit was in 3 mo; if there were no obvious symptoms, the patient could visit yearly.
Digital technology of stomatology refers to the technology that helps dentists realize an accurate, efficient, automatic, and intelligent diagnosis and treatment of oral diseases with the help of digital hardware or software. Digital hardware or software includes but is not limited to intraoral scanning, CBCT, digital diagnosis and design, digital occlusion analysis based on virtual articulators, artificial intelligence, navigation, robotics, and related materials. Dental CAD and CAM are typical applications of digital stomatology. The process includes digital impression, denture CAD, and CAM[7]. In traditional occlusal reconstruction, the acquisition of jaw position relationship largely depends on the doctors' experience and patients' subjective feedback, and therefore lacks an objective evaluation. Digital tools enable an objective evaluation of the treatment to help verify whether the reconstructed occlusion is coordinated with the functional state of the oral and maxillofacial system. The application of digital technology can help simulate and predict the effect of reconstructed occlusion and the accuracy of replication and transfer of occlusal relationships before invasive procedures. Treatment that was originally highly dependent on clinical experience has become procedural and reproducible with digitalization, and the technical threshold for doctors is relatively low. Digitalization can help achieve personalized medical treatment that conforms to patients' anatomical and physiological states and improve the pathological state, patient satisfaction with treatment, and quality and efficiency of communication between doctors and patients and between doctors and technicians. Digitalization in prosthodontics has been widely accepted by peers and is regarded as an irreversible trend. There is also consensus to build a complete process of digital prosthodontics—digital diagnosis, digital designing, digital manufacturing, and digital treatment"[8,9].
When the patient adapts to the new occlusal relationship formed using the occlusal pad and has no obvious subjective discomfort, objective assessment is performed by palpation with both hands to check the strength of contraction of the temporal muscle and CBCT to check whether the condylar position is normal. Then, the occlusal pad is debugged, and the first digital intraoral scanning is performed to collect the digital information of the MMR, to obtain the first type of occlusal relationship. After a certain period of temporary crown treatment with varying degrees of adjustment, running-in diagnosis, and verification, depending on the adaptability of patients, digital intraoral scanning is used once again to acquire another type of occlusal relationship.
In the widely used traditional method, the key to achieving occlusal reconstruction lies in the clinical experience of doctors to guarantee the accuracy of MMR in the entire process of copying, transferring from the occlusal pad to the temporary crowns, and making the final restorations. Moreover, with the restriction of its mock-up stage, the MMR available is, simply, the one acquired in the final coronal phase and is, therefore, comparatively limited. In this case report, digital intraoral scanning accurately recorded a series of digital information of the MMR during occlusal pad commissioning and temporary crown wearing. These data can help us find the best position for occlusal reconstruction, thus minimizing the errors generated in the tedious process of recording the best MMR relationship.
In traditional occlusal reconstruction, adaptive grinding of diagnostic temporary restorations, such as occlusal pads and temporary crowns, has advantages and disadvantages. Adjusting the occlusal relationship in the horizontal direction can better reduce the overbite of the anterior teeth, which is conducive to the condyle sliding upward and forward to achieve a satisfying central position relationship. The vertical distance will decrease due to wear, thus reducing the increased vertical distance in the process of occlusal reconstruction. Digital intraoral scanning technology can not only prevent the loss of optimal jaw relationship caused by various errors in the occlusal pad commissioning stage and temporary crown fabrication and grinding process but also provide a chance to choose the appropriate MMR in the clinic. The application of digital intraoral scanning in the occlusal reconstruction of fixed prosthesis makes recording the jaw position relationship between the maxilla and mandible, which is the most essential but fuzzy aspect in the treatment process, clear, recordable, reproducible, and selectable.
We can select either the occlusal relationship of the first oral scan (Figure 4A) or the second (Figure 4B) for the final reconstruction. In the digital software system, at the end of the mock-up phase, compared to when wearing the occlusal pad, the most anterior end of the lateral labial margin of the mandibular central incisor was shifted upward and medially by approximately 0.861 mm. Compared with digitally recorded information on the occlusal relationship between the end of the temporary crown and the end of the occlusal pad wearing, the occlusal reconstruction vertical distance decreased, and the overjet decreased slightly. There were supernumerary teeth between the maxillary central incisors of this patient; however, he refused extraction of the supernumerary teeth and restoration of the occlusal relationship in the anterior tooth area. The occlusal relationship of the temporary crown stage, with a slightly smaller overjet, was used for posterior teeth occlusal reconstruction, which helped retain the guiding function of the anterior teeth to a greater extent and was more conducive to the comfort of the patient's temporomandibular joint. By comparing the occlusal relationship of the patient's two oral scans, we determined that the occlusal relationship of the second oral scan was most suitable for the final restoration and reconstruction. Digital intraoral scanning has two advantages in occlusal reconstruction: (1) The occlusal relationship can be accurately reproduced and transferred stepwise from the occlusal pad to the temporary crown to the final restoration; and (2) It can establish a perfect occlusion that includes correct lateral occlusal guidance, uniform contact during centric occlusion, and a reasonable opening angle during non-centric motion.
In addition, the final occlusal relationship replication and transfer of diagnostic temporary restorations in traditional full-mouth occlusal reconstruction often use cross-mounting articulators. The traditional steps in this method include taking multiple impressions, pouring models, and recording multiple occlusions. Each step has potential for errors, and they cannot be quantified. These complex steps and potential errors can affect the occlusal accuracy of the final prosthesis and often requires considerable time to adjust in the clinic[10-12]. Digital intraoral scanning can minimize these errors and simplify the process. Digital intraoral scanning allows the direct transformation of the scanned information of the intraoral dentition to a digital dental model, three-dimensional prediction of the repair effect, and transfer the treatment design to the final prosthesis through digital design and production technology to enable the "what you see is what you get" treatment effect[13,14]. Using digital dental scanning equipment, the morphology of temporary restorations after functional adaptive wear, occlusal contact relationship, and refined abutment preparation can be recorded and the digital model established and matched. Digital intraoral scanning has become an important dental operation technology. Based on the data obtained, crown restoration and the production of implant super
Owing to the close relationship between digitalization and artificial intelligence (AI), it is believed that with the rapid development of AI technology in the future, the application of digitalization technology in clinical practice will become increasingly more common and operation will become increasingly simple and standardized; this in turn will provide a strong support for the development of AI medicine.
CBCT has been widely used in various fields of stomatology, including orthodontic three-dimensional cephalometry, orthodontic treatment plan design, implant surgery planning and guide plate design, maxillofacial surgery diagnosis and surgery design, maxillofacial surgery navigation implementation and guide plate design, temporomandibular joint diagnosis, periodontal diagnosis, root canal apical morphology and root fracture diagnosis, sleep apnea syndrome, and soft palate and pharyngeal morphology diagnosis. It is the most widely used and promising digital technology in stomatology. In addition to routine clinical examination, the examination methods in the occlusal reconstruction process of the fixed prosthesis also include the use of imaging to evaluate the structural changes of the oral and maxillofacial system, evaluate the motor functions of the oral and maxillofacial system, detect bruits of the temporomandibular joint, and examine the electrophysiological function of the masticatory muscles[22,23]. In this case, CBCT was used for occlusal reconstruction in a patient with severe abrasion. By a combination of the clinical symptoms of the patient before repair and 1 mo after permanent repair and the morphological changes of the temporomandibular joint space and condylar position shown by CBCT, the clinical treatment effect of fixed denture occlusal reconstruction was objectively evaluated Researchers believe that long-term dentition loss or serious wear leads to reduction in the vertical distance, and the condyle then shifts backward[24]. Consistent with the results of previous studies, in this patient, CBCT showed that the anterior space of the TMJ was significantly larger than the posterior space before occlusal reconstruction and that the condyle was displaced posteriorly. After digital intraoral scan-assisted occlusal reconstruction, CBCT showed that the left joint space was normal, the right posterior joint space was wider than before, and the space of the bilateral temporomandibular space was better. The patient's temporomandibular joint had not undergone pathological changes; therefore, only the jaw position and movement adapted to the physiological state of the joint muscles needed to be determined by digital equipment. Using this case as a reference, restoration with an accurate occlusal relationship can be achieved.
This clinical report showed that the application of digital intraoral scanning for occlusal reconstruction of a fixed prosthesis can accurately record the occlusal relationship of jaw position in different stages to avoid the loss of an optimal jaw relationship. Digital intraoral scanning makes recording the jaw position relationship between the maxilla and mandible, which is the most important but challenging aspect in the treatment process, clear, recordable, reproducible, and selectable. We hope that this clinical report will provide a new clinical reference for the design, fabrication, and postoperative evaluation of occlusal reconstruction of fixed prostheses. These conclusions should be verified with the treatment of more patients in the future.
The authors are grateful to Mr. Teng K for technical support.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Galiatsatos A, Greece; Nagamine T, Japan S-Editor: Yan JP L-Editor: A P-Editor: Yuan YY
| 1. | Edelhoff D, Probst F, Ehrenfeld M, Prandtner O, Schweiger J, Liebermann A. Interdisciplinary full-mouth rehabilitation for redefining esthetics, function, and orofacial harmony. J Esthet Restor Dent. 2019;31:179-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 2. | Li DL, Tan JG. Creating esthetic provisional restorations: step by step. Zhonghua Kou Qiang Yi Xue Za Zhi. 2021;56:226-230. [PubMed] |
| 3. | Fabbri G, Cannistraro G, Pulcini C, Sorrentino R. The full-mouth mock-up: a dynamic diagnostic approach (DDA) to test function and esthetics in complex rehabilitations with increased vertical dimension of occlusion. Int J Esthet Dent. 2018;13:460-474. [PubMed] |
| 4. | Gao H, Liu X, Liu M, Yang X, Tan J. Accuracy of three digital scanning methods for complete-arch tooth preparation: An in vitro comparison. J Prosthet Dent. 2022;128:1001-1008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 5. | Christensen GJ. Will digital impressions eliminate the current problems with conventional impressions? J Am Dent Assoc. 2008;139:761-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 79] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 6. | Zhao YW, Gao R, Sun HQ. The Protocol of Fixed Reconstruction for Severely Worn Teeth Combined with Anterior Deep Bite. Case Rep Dent. 2017;2017:9378091. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 7. | Duret F, Blouin JL, Duret B. CAD-CAM in dentistry. J Am Dent Assoc. 1988;117:715-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 132] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 8. | van Noort R. The future of dental devices is digital. Dent Mater. 2012;28:3-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 694] [Cited by in RCA: 715] [Article Influence: 51.1] [Reference Citation Analysis (0)] |
| 9. | Rekow ED. Digital dentistry: The new state of the art - Is it disruptive or destructive? Dent Mater. 2020;36:9-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 130] [Article Influence: 21.7] [Reference Citation Analysis (0)] |
| 10. | Liu Y. Several important issues concerning occlusal reconstruction. Hua Xi Kou Qiang Yi Xue Za Zhi. 2020;38:357-363. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 11. | Kordass B, Gärtner C, Söhnel A, Bisler A, Voss G, Bockholt U, Seipel S. The virtual articulator in dentistry: concept and development. Dent Clin North Am. 2002;46:493-506, vi. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 46] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Lee W, Kwon HB. Vertical repositioning accuracy of magnetic mounting systems on 4 articulator models. J Prosthet Dent. 2018;119:446-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Liu YS, Ye HQ, Gu M, Lv LW, Sun YC, Zhao YJ, Zhou YS. [Application of patient-participated digital design in esthetic rehabilitation of anterior teeth]. Beijing Da Xue Xue Bao Yi Xue Ban. 2014;46:90-94. [PubMed] |
| 14. | Coachman C, Georg R, Bohner L, Rigo LC, Sesma N. Chairside 3D digital design and trial restoration workflow. J Prosthet Dent. 2020;124:514-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 15. | Miyazaki T, Hotta Y, Kunii J, Kuriyama S, Tamaki Y. A review of dental CAD/CAM: current status and future perspectives from 20 years of experience. Dent Mater J. 2009;28:44-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 546] [Cited by in RCA: 472] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 16. | Goo CL, Tan KB. Fabricating CAD/CAM Implant-Retained Mandibular Bar Overdentures: A Clinical and Technical Overview. Case Rep Dent. 2017;2017:9373818. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Alghazzawi TF. Advancements in CAD/CAM technology: Options for practical implementation. J Prosthodont Res. 2016;60:72-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 313] [Article Influence: 34.8] [Reference Citation Analysis (0)] |
| 18. | Kattadiyil MT, Mursic Z, AlRumaih H, Goodacre CJ. Intraoral scanning of hard and soft tissues for partial removable dental prosthesis fabrication. J Prosthet Dent. 2014;112:444-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 87] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 19. | Williams RJ, Bibb R, Eggbeer D, Collis J. Use of CAD/CAM technology to fabricate a removable partial denture framework. J Prosthet Dent. 2006;96:96-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 111] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 20. | Li Z, Xia Y, Chen K, Zhao H, Liu Y. Maintenance of the Maxillomandibular Position with Digital Workflow in Oral Rehabilitation: A Technical Note. Int J Prosthodont. 2018;31:280-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Ho CT, Lin HH, Lo LJ. Intraoral Scanning and Setting Up the Digital Final Occlusion in Three-Dimensional Planning of Orthognathic Surgery: Its Comparison with the Dental Model Approach. Plast Reconstr Surg. 2019;143:1027e-1036e. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 22. | Hanchi Z, Tingting L, Bilu X, Zhongjie L, Yang L. Features of condylography curves. Hua Xi Kou Qiang Yi Xue Za Zhi. 2017;35:555-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 23. | Sharma S, Crow HC, Kartha K, McCall WD Jr, Gonzalez YM. Reliability and diagnostic validity of a joint vibration analysis device. BMC Oral Health. 2017;17:56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Krishnamoorthy B, Mamatha N, Kumar VA. TMJ imaging by CBCT: Current scenario. Ann Maxillofac Surg. 2013;3:80-83. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |