Published online Apr 26, 2023. doi: 10.12998/wjcc.v11.i12.2848
Peer-review started: January 24, 2023
First decision: February 17, 2023
Revised: February 20, 2023
Accepted: March 24, 2023
Article in press: March 24, 2023
Published online: April 26, 2023
Processing time: 91 Days and 5.3 Hours
Acute diverticulitis is one of the most prevalent complications of diverticular disease and may result in abscess formation, perforation, fistula formation, obstruction, or bleeding. Diverticular abscesses may be initially treated with antibiotics and/or percutaneous drainage and/or surgery. Endoscopic ultrasound (EUS)-guided drainage techniques are increasingly used as a minimally invasive alternative to percutaneous or surgical approaches, as they are associated with better treatment outcomes, shorter recovery time and duration of hospitalization.
A 57-year-old female presented to the emergency department on account of abdominal pain and fever. Clinical examination revealed tenderness in the left lower abdominal quadrant, with elevated inflammatory markers in laboratory tests. Abdominal computed tomography (CT) revealed an 8 cm × 8 cm × 5 cm well-encapsulated abscess of the sigmoid colon, surrounded by numerous diverticula. A diagnosis of Hinchey II diverticular abscess was made, and the patient was admitted and commenced on appropriate antibiotic treatment. A transrectal EUS showed a fluid collection in direct contact with the sigmoid colon. Transluminal drainage was performed, and a lumen-apposing metal stent was inserted into the abscess collection. A follow-up CT scan showed a regression of the collection. The patient's general condition improved, and the stent was removed during a follow-up transrectal EUS that revealed no visible collection.
We report the first successful management of a pelvic abscess in patient with Hinchey II acute diverticulitis using EUS-guided transluminal drainage in Slovenia. The technique appears effective for well-encapsulated intra-abdominal abscesses larger than 4 cm in direct contact with the intestinal wall of left colon.
Core Tip: The incidence of colonic diverticulosis and its complications is rising in developed countries. An abscess due to acute diverticulitis may be initially treated with antibiotics and/or percutaneous drainage and/or surgery. Since percutaneous drainage of an abscess is not always feasible, endoscopic ultrasound-guided transluminal drainage seems to be an effective minimally invasive alternative for well-encapsulated intra-abdominal abscesses lying in direct contact with the intestinal wall, which reduces the need for surgery and stoma formation in selected patients. However, given the limitations of the supporting evidence, the optimal treatment strategy should be determined on a case-by-case basis by a multidisciplinary team.
- Citation: Drnovšek J, Čebron Ž, Grosek J, Janež J. Endoscopic ultrasound-guided transrectal drainage of a pelvic abscess after Hinchey II sigmoid colon diverticulitis: A case report. World J Clin Cases 2023; 11(12): 2848-2854
- URL: https://www.wjgnet.com/2307-8960/full/v11/i12/2848.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i12.2848
Diverticulosis of the colon is defined as the existence of false diverticula or outpouchings of the mucosa and serosa through openings in the muscular layer of the bowel known as locus minoris resitentiae. The condition is remarkably prevalent in Western countries, affecting a substantial proportion of the middle-aged and elderly populations. Inflammation of a colonic diverticulum, or acute diverticulitis, is one of the most prevalent complications of diverticular disease and represents an abdominal emergency[1]. The incidence of acute diverticulitis is rising, especially among individuals under the age of 50. This is likely attributable to factors such as a low-fibre diet, obesity, smoking, physical inactivity, and a diet high in red meat[2-4]. Approximately 5% of patients with known diverticula are estimated to develop an episode of acute diverticulitis[5].
Numerous classifications and modifications describe the various stages of diverticular disease. The first widely used classification by Hinchey was intended as an intra-operative stratification of perforated diverticulitis with abscess or peritonitis, enabling surgeons to adjust the surgical approach. The treatment of acute diverticulitis depends on whether the presentation is uncomplicated or complicated. Complicated presentation occurs in approximately 12% of patients. An intraabdominal abscess (Hinchey Ib or II) can be managed non-operatively, but an abscess larger than 4 cm in diameter must be drained[3,6,7].
In recent years, minimally invasive methods have replaced classical surgical techniques where possible. Drainage is usually performed percutaneously by an interventional radiologist. However, percutaneous drainage is not always feasible, and endoscopic ultrasound (EUS)-guided drainage represents a compelling alternative that eliminates the need for an invasive surgical approach.
In the present report, we describe the clinical presentation, management, and outcome of EUS-guided drainage of a pelvic abscess due to complicated Hinchey II acute sigmoid diverticulitis. The management approach is discussed in the context of available literature.
A 57-year-old otherwise healthy female was admitted to the abdominal emergency department on account of abdominal pain and a fever of up to 38 ˚C since the preceding five days.
A patient's history of past illness is unremarkable.
A patient's personal and family history is unremarkable.
Clinical examination revealed localized tenderness in the left lower abdominal quadrant without clinical signs of diffuse peritonitis.
Laboratory tests at admission showed elevated inflammatory markers with a C-reactive protein (CRP) value of 353 mg/L and a leucocyte count of 12.4 × 109/L.
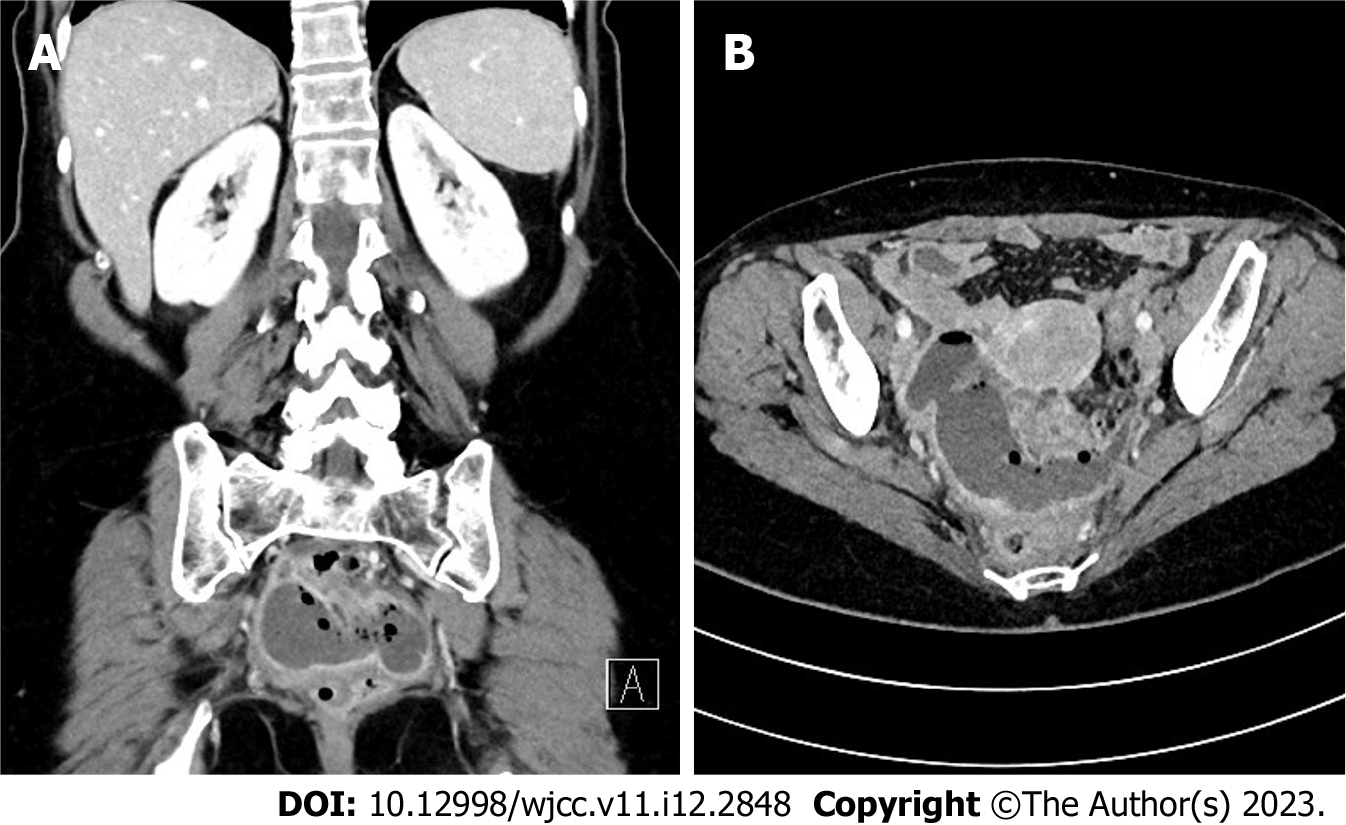
An urgent abdominal computed tomography (CT) scan revealed a well-encapsulated pelvic abscess measuring 8 cm × 8 cm × 5 cm, located in the proximity of a very long sigmoid colon surrounded by numerous diverticula (Figure 1). There was only a small amount of free fluid in the lesser pelvis with no other pathological findings.
Pelvic abscess due to acute sigmoid diverticulitis (Hinchey II) without evidence of diffuse peritonitis.
The patient was hospitalized at the department of abdominal surgery, and empirical antibiotic treatment with amoxicillin and clavulanic acid was commenced, in line with national guidelines for acute complicated diverticulitis. Additionally, in the first 48 h she was put on nil by mouth and received intravenous fluids and analgesics. Due to the size of the abscess and the elevated inflammatory markers despite antibiotic treatment, an interventional radiologist was consulted to perform percutaneous drainage. However, the collection was not safely approachable via the percutaneous route. After consulting a gastroenterologist, a decision was jointly made to attempt draining the collection transrectally under EUS guidance.
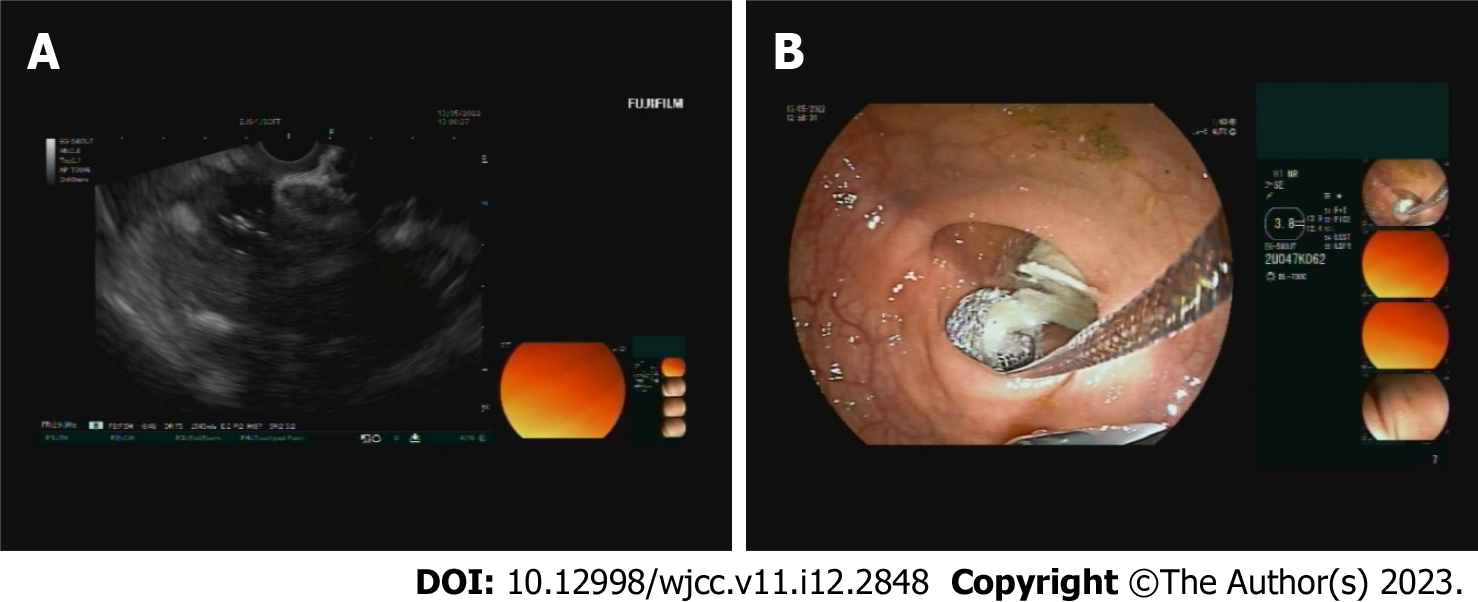
On the third day of admission, a transrectal EUS scan was performed, which showed an encapsulated fluid collection lying in direct contact with the wall of the sigmoid colon. Transluminal drainage of the collection was performed by placing a lumen-apposing metal stent (LAMS) into the collection (Figure 2). The procedure was completed without complications, and purulent content was observed leaking through the open stent. The patient’s condition gradually improved over the first few days after the procedure; she started with enteral nutrition, abdominal pain diminished, and defecation was normal. The previously elevated inflammatory parameters also began to decline.
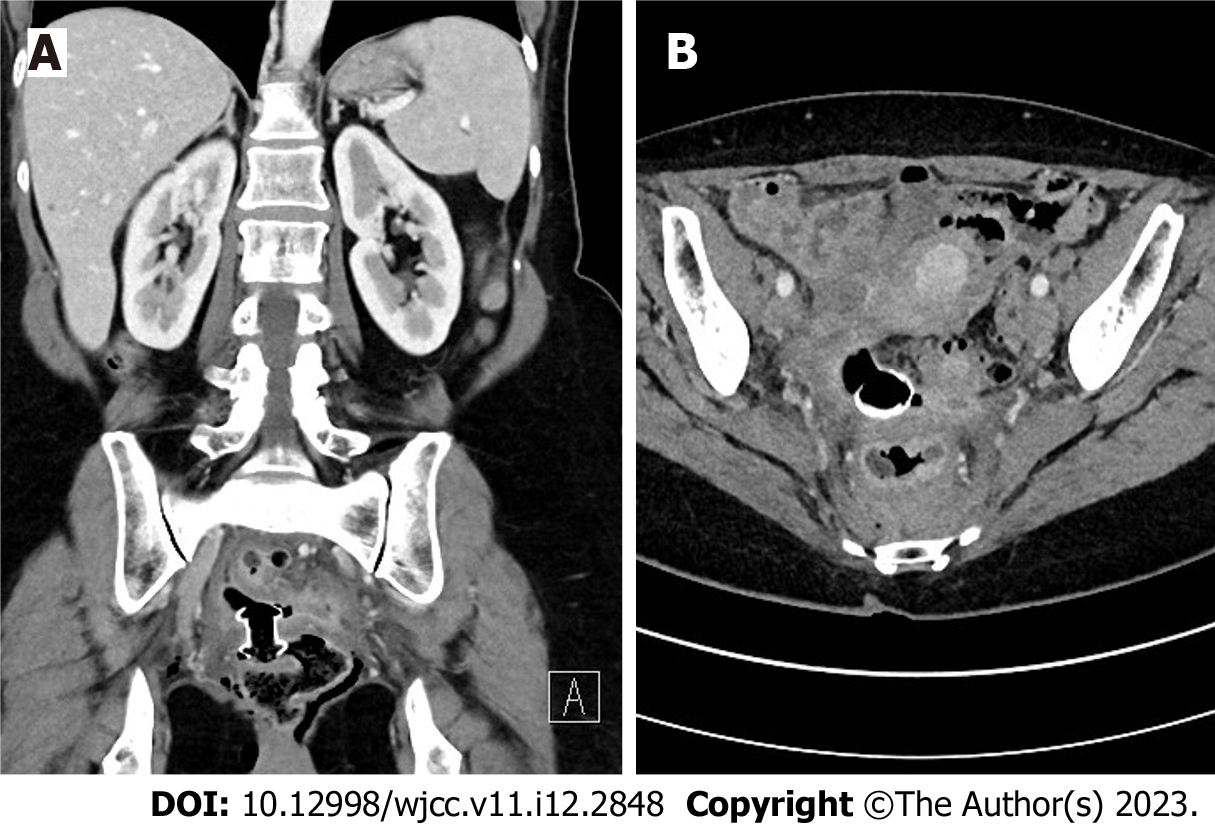
A follow-up abdominal CT scan showed an appropriate stent position and regression of the collection with only some residual gas at the site (Figure 3). As the patient was asymptomatic, the antibiotic treatment was switched from intravenous to enteral route by the 9th day after admission. She was temporarily discharged home with the prescribed antibiotic and care instructions.
The patient returned as scheduled on the 16th day after the primary admission and repeat laboratory studies showed complete normalization of inflammatory parameters (CRP 6 mg/L, leukocytes 6.6 × 109/L). She reported no complaints and was discharged from the hospital on the same day. The antibiotic treatment was also discontinued after 16 d of administration (9 d intravenously and 8 d enterally).
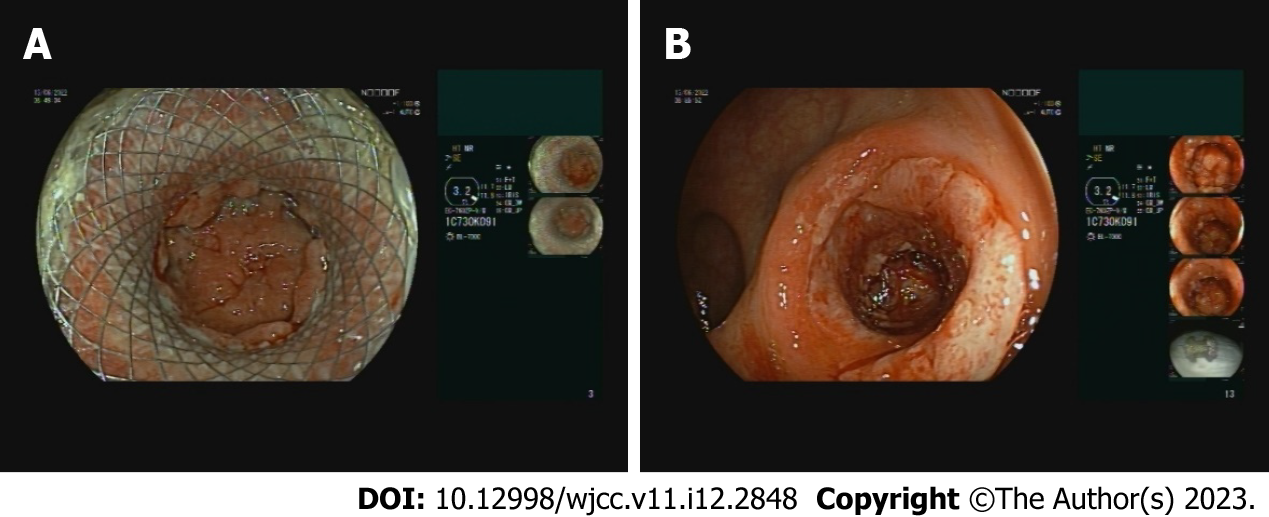
Thirty days after the stent insertion, an elective follow-up transrectal EUS was performed at the outpatient clinic. The endoscopic view demonstrated almost complete closure of the abscess cavity, surrounded by granulation tissue; accordingly, the LAMS was endoscopically removed during the same procedure (Figure 4). The procedure was uneventful, and at a subsequent follow-up clinical review, the patient remained well without any complaints. Three months after the LAMS removal, we additionally performed a colonoscopy and noted the disappearance of the fistular canal at the previous puncture site and no other remarkable findings.
We present a case of successful EUS-guided drainage of a pelvic abscess due to complicated Hinchey II acute sigmoid diverticulitis. Because the percutaneous route of abscess drainage was not safely accessible, the decision was made to use this alternative option after interdisciplinary consultations and discussions. The EUS-guided transrectal drainage with LAMS insertion was performed and, in combination with antibiotic treatment, proved effective for managing the diverticular abscess. LAMS removal was performed 30 d after the insertion uneventfully.
There are several classification systems for describing acute diverticulitis, but the modified Hinchey classification, introduced in 1978 and revised by Wasvary et al[8] in 1999, remains the most commonly used in the international literature[8-12]. In general, the management of acute diverticulitis is well-established in the guidelines[6,7,12,13]. For the Hinchey stages 0 and Ia, antibiotic treatment is usually sufficient; stages Ib and II require additional drainage if an abscess is larger than 4 cm[6,7,13]. The drainage may be performed surgically, percutaneously or endoscopically[11,13].
However, the most appropriate drainage method for the patient may not always be accurately determined, and treatment choice must be individualized. The surgical treatment being the most invasive and associated with the highest morbidity and mortality, should be performed as a last resort and only when other methods fail. The most widely accepted clinical practice is to perform percutaneous drainage via transabdominal anterior or transgluteal posterior approach; however, percutaneous drainage is not always feasible[11-14]. Additionally, even though it is considered safe, the complication rate of percutaneous drainage is 2.5% (ranging from 0 to 12.5%), and possible complications include enterocutaneous fistulas, small bowel lesions, and sciatic nerve injuries[15].
Deep pelvic abscesses often present a clinical challenge, since they are surrounded by intra-abdominal organs and other structures, which may interfere with safe percutaneous drainage route. Over the past few decades, endoscopic drainage has emerged as a compelling and feasible option when percutaneous drainage cannot be performed safely, reducing the need for surgery and stoma formation in selected patients[11]. However, endoscopic drainage of diverticular abscess is not yet reflected in the major guidelines, and its supporting evidence is currently limited to only several retrospective case studies or case reports[6,12-17]. In contrast, the experience with endoscopic drainage of intraabdominal abscesses is rich. Besides acute diverticulitis, an intraabdominal abscess may also be associated with other inflammatory gastrointestinal or urogenital conditions or may occur as a complication after surgical procedures. Appropriate drainage is of vital importance for a successful treatment of an intra-abdominal abscess[18,19]. Extensive and positive experiences with LAMS in treating peripancreatic collections also open new possibilities for treating other types of fluid collections. Their characteristic shape prevents stent dislocation, and the diameter of the lumen allows efficient drainage and further endoscopic necrosectomy via an open stent. EUS-guided transluminal drainage might be a safer procedure in comparison to surgical or percutaneous drainage techniques as the risk of vessel injury and a puncture site leakage are neglectable. Interestingly, fecal contamination in the abscess cavity is unlikely as the intrinsic negative luminal pressure ensures adequate drainage. Thus, EUS-guided transluminal drainage is a suitable drainage method of all pelvic abscesses, regardless of their etiology.
The crucial abscess characteristics for a safe EUS drainage are size larger than 4 cm, a well-formed capsule and the position in close contact with the intestinal wall of the left colon[14,19]. As already noted, although percutaneous drainage is considered the method of choice in the existing guidelines, it is not always feasible. In the event of a failed or impractical percutaneous approach, an attempt at endoscopic drainage should be considered in any patient without evidence of sepsis before initiating surgical therapy. Meanwhile, more case reports or larger prospective studies are needed to evaluate and compare both drainage methods. Because EUS-guided drainage is not included in the guidelines, the exact role of endoscopic drainage in the treatment of diverticular abscesses remains unclear.
Since percutaneous drainage of diverticular abscess is not always feasible, EUS-guided transluminal drainage appears to be a promising and practical alternative for managing well-encapsulated intra-abdominal abscesses that lie in direct contact with the intestinal wall of left colon, reducing the need for surgery and stoma formation. However, given the limited evidence, a careful interdisciplinary review of each clinical case by the abdominal surgeon, gastroenterologist, and interventional radiologist is required to determine the optimal treatment strategy.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Slovenia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bains L, India; Bal’afif F, Indonesia; Liang P, China S-Editor: Zhao S L-Editor: A P-Editor: Zhao S
| 1. | Wilkins T, Embry K, George R. Diagnosis and management of acute diverticulitis. Am Fam Physician. 2013;87:612-620. [PubMed] |
| 2. | Swanson SM, Strate LL. Acute Colonic Diverticulitis. Ann Intern Med. 2018;168:ITC65-ITC80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 54] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 3. | Strate LL, Morris AM. Epidemiology, Pathophysiology, and Treatment of Diverticulitis. Gastroenterology. 2019;156:1282-1298.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 267] [Article Influence: 44.5] [Reference Citation Analysis (0)] |
| 4. | Hawkins AT, Wise PE, Chan T, Lee JT, Glyn T, Wood V, Eglinton T, Frizelle F, Khan A, Hall J, Ilyas MIM, Michailidou M, Nfonsam VN, Cowan ML, Williams J, Steele SR, Alavi K, Ellis CT, Collins D, Winter DC, Zaghiyan K, Gallo G, Carvello M, Spinelli A, Lightner AL. Diverticulitis: An Update From the Age Old Paradigm. Curr Probl Surg. 2020;57:100862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 72] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 5. | Piscopo N, Ellul P. Diverticular Disease: A Review on Pathophysiology and Recent Evidence. Ulster Med J. 2020;89:83-88. [PubMed] |
| 6. | Francis NK, Sylla P, Abou-Khalil M, Arolfo S, Berler D, Curtis NJ, Dolejs SC, Garfinkle R, Gorter-Stam M, Hashimoto DA, Hassinger TE, Molenaar CJL, Pucher PH, Schuermans V, Arezzo A, Agresta F, Antoniou SA, Arulampalam T, Boutros M, Bouvy N, Campbell K, Francone T, Haggerty SP, Hedrick TL, Stefanidis D, Truitt MS, Kelly J, Ket H, Dunkin BJ, Pietrabissa A. EAES and SAGES 2018 consensus conference on acute diverticulitis management: evidence-based recommendations for clinical practice. Surg Endosc. 2019;33:2726-2741. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 139] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Schultz JK, Azhar N, Binda GA, Barbara G, Biondo S, Boermeester MA, Chabok A, Consten ECJ, van Dijk ST, Johanssen A, Kruis W, Lambrichts D, Post S, Ris F, Rockall TA, Samuelsson A, Di Saverio S, Tartaglia D, Thorisson A, Winter DC, Bemelman W, Angenete E. European Society of Coloproctology: guidelines for the management of diverticular disease of the colon. Colorectal Dis. 2020;22 Suppl 2:5-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 151] [Article Influence: 30.2] [Reference Citation Analysis (0)] |
| 8. | Wasvary H, Turfah F, Kadro O, Beauregard W. Same hospitalization resection for acute diverticulitis. Am Surg. 1999;65:632-5; discussion 636. [PubMed] |
| 9. | Hinchey EJ, Schaal PG, Richards GK. Treatment of perforated diverticular disease of the colon. Adv Surg. 1978;12:85-109. [PubMed] |
| 10. | Klarenbeek BR, de Korte N, van der Peet DL, Cuesta MA. Review of current classifications for diverticular disease and a translation into clinical practice. Int J Colorectal Dis. 2012;27:207-214. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 108] [Cited by in RCA: 125] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 11. | Zaborowski AM, Winter DC. Evidence-based treatment strategies for acute diverticulitis. Int J Colorectal Dis. 2021;36:467-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Qaseem A, Etxeandia-Ikobaltzeta I, Lin JS, Fitterman N, Shamliyan T, Wilt TJ; Clinical Guidelines Committee of the American College of Physicians*, Crandall CJ, Cooney TG, Cross JT Jr, Hicks LA, Maroto M, Mustafa RA, Obley AJ, Owens DK, Tice J, Williams JW Jr; Clinical Guidelines Committee of the American College of Physicians. Diagnosis and Management of Acute Left-Sided Colonic Diverticulitis: A Clinical Guideline From the American College of Physicians. Ann Intern Med. 2022;175:399-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 37] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 13. | Sartelli M, Weber DG, Kluger Y, Ansaloni L, Coccolini F, Abu-Zidan F, Augustin G, Ben-Ishay O, Biffl WL, Bouliaris K, Catena R, Ceresoli M, Chiara O, Chiarugi M, Coimbra R, Cortese F, Cui Y, Damaskos D, De' Angelis GL, Delibegovic S, Demetrashvili Z, De Simone B, Di Marzo F, Di Saverio S, Duane TM, Faro MP, Fraga GP, Gkiokas G, Gomes CA, Hardcastle TC, Hecker A, Karamarkovic A, Kashuk J, Khokha V, Kirkpatrick AW, Kok KYY, Inaba K, Isik A, Labricciosa FM, Latifi R, Leppäniemi A, Litvin A, Mazuski JE, Maier RV, Marwah S, McFarlane M, Moore EE, Moore FA, Negoi I, Pagani L, Rasa K, Rubio-Perez I, Sakakushev B, Sato N, Sganga G, Siquini W, Tarasconi A, Tolonen M, Ulrych J, Zachariah SK, Catena F. 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J Emerg Surg. 2020;15:32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 224] [Cited by in RCA: 201] [Article Influence: 40.2] [Reference Citation Analysis (0)] |
| 14. | Lisotti A, Cominardi A, Bacchilega I, Linguerri R, Fusaroli P. EUS-guided transrectal drainage of pelvic fluid collections using electrocautery-enhanced lumen-apposing metal stents: a case series. VideoGIE. 2020;5:380-385. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Gregersen R, Mortensen LQ, Burcharth J, Pommergaard HC, Rosenberg J. Treatment of patients with acute colonic diverticulitis complicated by abscess formation: A systematic review. Int J Surg. 2016;35:201-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 86] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 16. | Donatelli G, Cereatti F, Fazi M, Ceci V, Dhumane P. Endoscopic ultrasound-guided drainage of intra-abdominal diverticular abscess. A case series. J Minim Access Surg. 2021;17:513-518. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Hadithi M, Bruno MJ. Endoscopic ultrasound-guided drainage of pelvic abscess: A case series of 8 patients. World J Gastrointest Endosc. 2014;6:373-378. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 26] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (1)] |
| 18. | Dawod E, Nieto JM. Endoscopic Ultrasound-Guided Drainage of Pelvic, Intra-abdominal, and Mediastinal Abscesses. In: Interventional Endoscopic Ultrasound. Springer. 2019;. [DOI] [Full Text] |
| 19. | Dhindsa BS, Naga Y, Saghir SM, Dhaliwal A, Ramai D, Cross C, Singh S, Bhat I, Adler DG. EUS-guided pelvic drainage: A systematic review and meta-analysis. Endosc Ultrasound. 2021;10:185-190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |