Published online Apr 26, 2023. doi: 10.12998/wjcc.v11.i12.2803
Peer-review started: December 3, 2022
First decision: February 17, 2023
Revised: March 1, 2023
Accepted: March 20, 2023
Article in press: March 20, 2023
Published online: April 26, 2023
Processing time: 143 Days and 13.7 Hours
Postoperative complications of triceps surae intramuscular hemangioma surgery with talipes equinovarus have rarely been described, and the evidence for treatment is limited. The purpose of this case study was to report the new application of the Ilizarov technique, which successfully treated talipes equino
A 29-year-old woman treated with the Ilizarov technique for talipes equinovarus in the right leg after triceps surae intramuscular hemangioma surgery. The equinus deformity was roughly corrected after 2 years of follow-up, without significant secondary sequelae.
Talipes equinovarus caused by postoperative sequelae of intramuscular heman
Core Tip: The purpose of this case study was to report the new application of the Ilizarov technique, which successfully treated talipes equinovarus in adults after triceps surae intramuscular hemangioma. The Ilizarov technique may be a surgical method for treating postoperative deformity of limbs, even in adult patients. Physicians should be aware of new uses for this type of treatment.
- Citation: Chen ZX, Wang MY, Zhang C, Ding ZQ, Chen W. Treatment of talipes equinovarus after triceps surae intramuscular hemangioma surgery by Ilizarov technology in adults: A case report. World J Clin Cases 2023; 11(12): 2803-2810
- URL: https://www.wjgnet.com/2307-8960/full/v11/i12/2803.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i12.2803
Conditions such as cerebral palsy[1], trauma[2], diabetes mellitus[3], muscular dystrophy[4], maldevelopment, or idiopathic[5] all have the potential to cause spasticity or contractures of the Achilles tendons, leading to clubfoot deformity[6]. Several genetic factors also have the potential to cause clubfoot deformity[3]. Clinical cases of Triceps surae intramuscular hemangioma resulting in ankle Achilles tendon contracture with equinus deformity and toe walking are rare[7-12]. Several surgical approaches have been described for treating the deformity, including serial casting of the ankle and knee[13], primary soft tissue release[14], the Ponseti method[15], Z-plasty, total talus resection, and tibioclavicular fusion with Achilles tendon lengthening[16]. Among them, the serial casting of the ankle and knee for surgical extension, which, like primary soft tissue release, requires surgical release and predisposes to bleeding from damaged vessels and makes full correction difficult in patients with more severe contractures[13,14]. The Ponseti method has good results mainly for congenital idiopathic clubfoot, but there is still a recurrence rate of one in three for clubfoot deformities after angioma surgery[17].
No clinical evidence can be reported at this time. Z-plasty, total talus resection, and tibioclavicular fusion with Achilles tendon lengthening all appear to provoke limb incongruence, bone loss, and other conditions with some probability of recurrence due to some disruption of the original ankle structure[18]. For patients after sural angioma surgery, there are no cases of Achilles tendon contracture treated with the sequelae of sural angioma surgery using the Ilizarov technique. This case report describes the Ilizarov technique to treat postoperative Achilles tendon contractures resulting from triceps surae hemangioma.
A 29-year-old Chinese woman presented to the orthopedics clinic with the inability to walk for 11 years due to talipes equinovarus.
Symptoms started 11 years before presentation with talipes equinovarus walk after intramuscular hemangioma surgery.
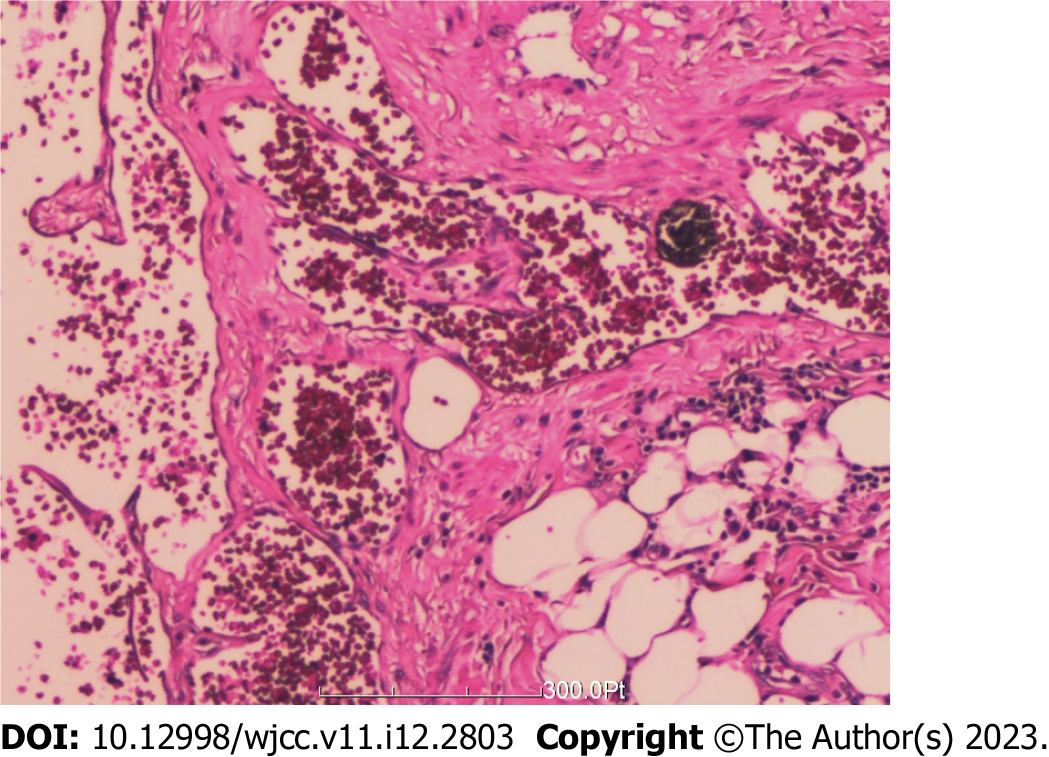
The patient was admitted with a high arch deformity of her right foot. At the age of 11 years, a right lower leg tumor was detected, which was not given special attention. The patient was found to have an increased mass in the right leg at the age of 27 years and attended hospital for magnetic resonance imaging, which indicated abnormal signals in the right thigh. Hemangioma was considered and confirmed as intramuscular hemangioma (Figure 1). After surgery, the patient gradually developed a high arch deformity of the right foot, and could not walk normally. She sought treatment in many hospitals, and most of them suggested amputation of stump and installation of a prosthetic limb, which was rejected by the patient.
The patient denied any family history of malignant tumors.
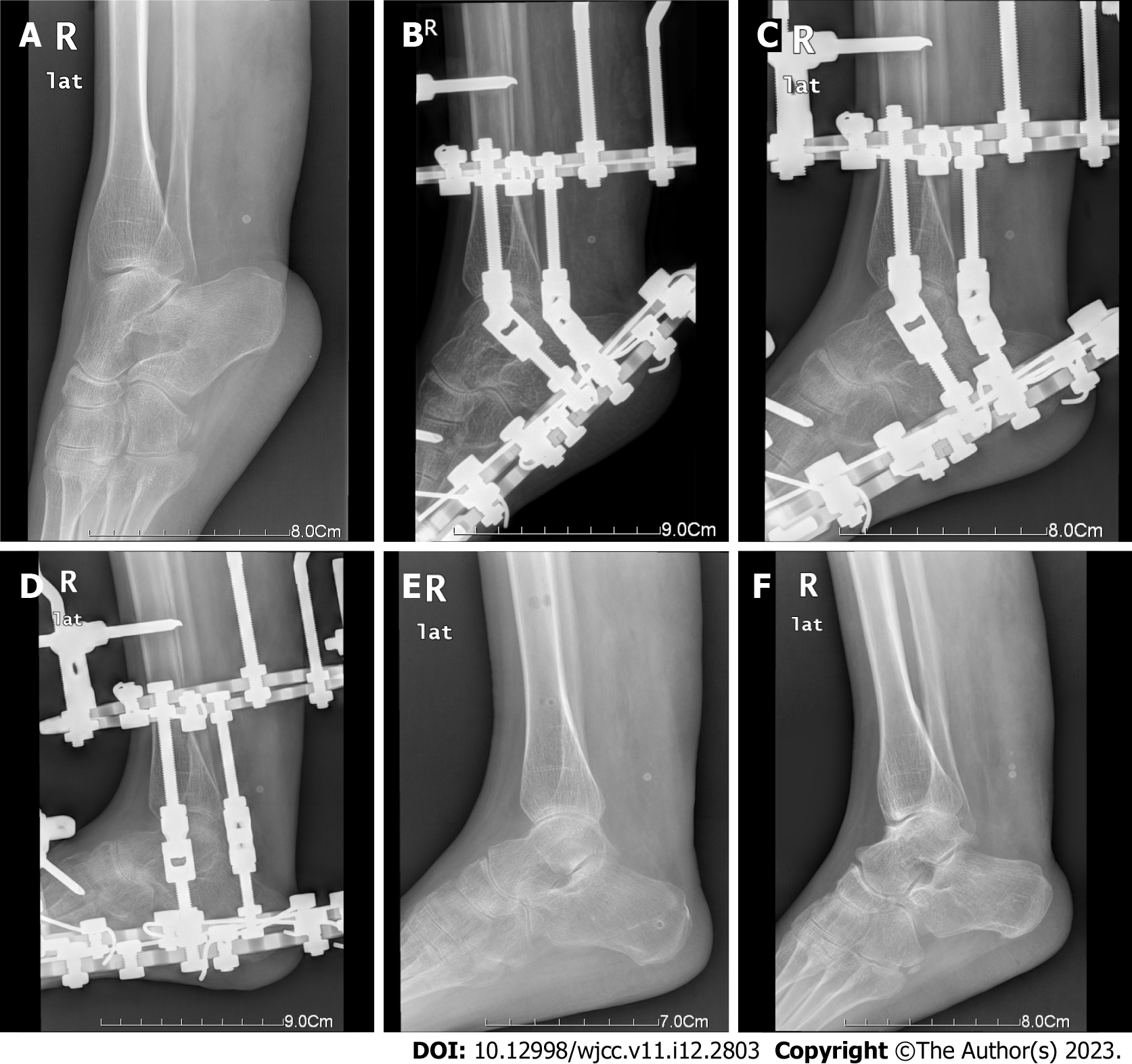
A marked 15-cm surgical scar was noted on the right lower leg, which was markedly thin and reduced by 6 cm compared with the contralateral circumference, a high arched right equinus foot, broken skin on the right foot, flexor plantar deformity of the right ankle, limited dorsiflexor activity, regular movement of the right knee, and normal sensation (Figure 2).
Hemangioma was considered and confirmed as intramuscular hemangioma.
Preoperative X-ray showed corrected foot drop deformity, and no signs of fracture, and other bone abnormalities in the ankle joints. Preoperative tibial tuberosity advancement (TTA) was 164° (Figure 3A). The TTA reflects the degree of talus inclination in the sagittal plane and is an indicator of the correction of pronation deformity, which is important for the stability of the entire hindfoot. TTA was measured between the tibial anatomical axis and the axis of the talus[19]. Postoperative X-ray re-examination showed that the right ankle was in a functional position, and an external fixator was in position (Figure 3B). A 1-mo review by postoperative X-ray showed that the right ankle was in a functional position, the ankle joint space was narrowed, and an external fixator was in position (Figure 3C). A 4-mo postoperative review (removal of the external fixator) showed that the right ankle joint had a normal relationship; there were no signs of fracture or other bony abnormalities in the constituted bones (Figure 3D-F). The patient's postoperative changes were consistent with the preoperative assessment and the expected surgical outcome. The surrounding soft tissues were slightly swollen (TTA 113°).
Combined with the patient’s medical history, the final diagnosis was talipes equinovarus after triceps surae intramuscular hemangioma surgery.
A routine preoperative examination was performed. According to the length, circumferential diameter, and degree of deformity of the affected limb, the Ilizarov annular external fixator with a three-dimensional orthopedic function was assembled. The orthopedic device was equipped with two full rings in the lower leg, one U-shaped ring, and one-half ring in the foot, which could correct the foot dropping horseshoe high arch deformity.
Under anesthesia, the patient was lied in supine position, and a tourniquet was placed on the middle and upper third of the right thigh (pressure 55 KPa). After routine disinfection, a sterile cavity towel was placed. After making a 6-cm long incision along the medial side of the calf, the subcutaneous fascia was separated to expose the tendon. The tendon was extended by about 4 cm in a "Z" incision. When overlapping sutures of the Achilles tendon, the ankle ring holder was put on, the external ring fixator was adjusted with the axis in line with the middle course of the affected limb, and two and two half whole stitches were passed through the calf segment, respectively. One full needle was inserted in the forefoot, one-half needle in the heel, and two full needles across the heel. The medial and lateral hinges were located at the medial and lateral malleolus (i.e., the rotation centerline of the ankle joint). The front and rear tie rods and adjusting areas were installed to stabilize the annular fixator in the appropriate position of the right foot to avoid the high skin tension caused by surgical incision (Figure 4).
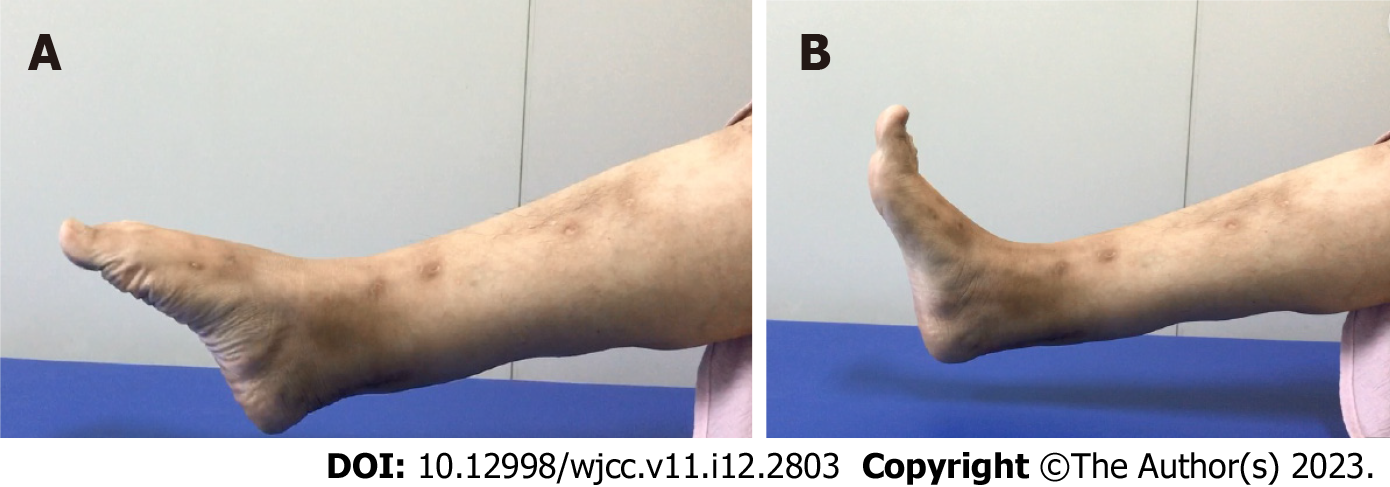
After surgery, the wound was kept dry until routine healing, and on the 7th postoperative day, the anterior and posterior bars were adjusted to correct the deformed stump. The stump could be turned and walk with the protection of the external fixation frame and the help of the orthopedic insole. Four weeks after the operation, the foot drop was corrected roughly, the ankle movement was expected, after which the external fixator was continued to perform the flexion-extension exercise. There was no pain and discomfort in the ankle joint, and at 4 mo after surgery, after removal of the external frame, the abduction was discarded and the patient walked on her own, with normal ankle movement and no dysmorphic activity (Figure 5).
TTA 164° was measured by preoperative radiography. Two physicians performed grading according to the American Orthopedic Foot and Ankle Society Ankle Hindfoot Scale (AOFAS-AHFS)[19], which yielded a mean score of 22.5, illustrating that the patient had poor ankle movement preoperatively, and 4 mo after corrective surgery, TTA was 113°. After return to normal angulation, the average AOFAS-AHFS score was 90.0, the ankle function returned to normal, the dorsiflexion activity was significantly improved, and there was adequate ankle activity at 2 year’s follow-up, with no other complications.
Most intramuscular tumors with fatty rings are benign, and peripheral nerve sheath tumor is the most common tumor type[20,21]. Two major categories of lesions emerged from the study of Mulliken and Glowacki[22] in 1982: Hemangioma and vascular malformation. For hemangioma treatment, percutaneous sclerotherapy is often used, which may cause equinus[23]. When sclerotherapy fails, the embedded hemangioma is usually treated by resection. Most muscle tissue needs to be removed simultaneously with tumor resection. This may lead to patients without average muscle mass, muscle strength reduction, and stress contracture of the Achilles tendon, leading to the limitation of the ankle joint activity and appearance of equinus[24].
Equinus correction using the Ilizarov technique provides the benefits of early weight bearing. The unique advantage is to promote regeneration of soft tissue around the bone, including skin, muscle, and neurovascular structures. Its versatility allows correction of the foot position by adjusting the frame postoperatively[25]. The Ilizarov technique can enhance the direct total load capacity and promote osteogenesis because of its unique biomechanical principles[26]. Applying the Ilizarov technique in postoperative adjustment and tissue regeneration under slow drafting after surgery does not cause paralysis of nerves and blood vessels and skin necrosis, thus avoiding scar formation. The Ilizarov technique can be used for all causes of Achilles tendon contracture. Our patient had a rare case of muscle fibrosis and scarring due to surgical excision following invasion of the muscle by a hemangioma. The Ilizarov technique may provide a new solution for foot drop due to muscle scarring from various causes or muscle necrosis due to osteofascial syndrome.
In this study, the Achilles tendon can be extended acutely during the operation due to the Z-shaped incision. However, the length of skin, blood vessels, and neuroanatomy[19] are limited, and their elasticity is finite, so they cannot be extended acutely during the operation. Skin, blood vessels, and neuroanatomy can only develop slowly after the procedure, ensuring that the hinges are correctly positioned during surgery. When adjusting the external fixator postoperatively, it is important to adjust the distance between the anterior and posterior bars after opening the joint gap. At the same time, postoperative lengthening can adjust it in accordance with the patient’s tolerance. In this process, in protecting the outer frame hinge, we advocate postoperative ankle flexion and extension exercise to prevent joint stiffness, ensure the stability of the ankle joint, and restore the function of the ankle. Follow-up with regular postoperative radiography can prevent traumatic arthritis due to anterior ankle impingement.
We report a case of postoperative sequelae of triceps surae hemangioma that caused Achilles tendon contracture, which was successfully corrected by the Ilizarov technique. The tolerance of skin, nerve, and blood vessels should be considered when acute lengthening of the Achilles tendon is performed interactively. The patient’s postoperative orthopedic exercises were performed interactively. Meanwhile, foot and ankle flexion and extension exercises were performed under the protection of the hinge, guaranteeing foot and ankle functional recovery. In this case, good outcomes were achieved, with the range of motion of the ankle roughly restored and ability to walk normally with no toe-walking. This case may advise physicians to correct talipes equinovarus by the Ilizarov technique.
We want to express our gratitude to all physicians and nurses involved in the management of the patient.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zang J, China S-Editor: Gao CC L-Editor: A P-Editor: Zhao S
| 1. | Gasq D, Molinier F, Reina N, Dupui P, Chiron P, Marque P. Posterior tibial tendon transfer in the spastic brain-damaged adult does not lead to valgus flatfoot. Foot Ankle Surg. 2013;19:182-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Wang XJ, Chang F, Su Y, Chen B, Song JF, Wei XC, Wei L. Ilizarov technique and limited surgical methods for correction of post-traumatic talipes equinovarus in children. ANZ J Surg. 2017;87:815-819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Chen C, Kaushal N, Scher DM, Doyle SM, Blanco JS, Dodwell ER. Clubfoot Etiology: A Meta-Analysis and Systematic Review of Observational and Randomized Trials. J Pediatr Orthop. 2018;38:e462-e469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 4. | Sun JX, Yang ZY, Xie LM, Wang B, Bai N, Cai AL. TAZ and myostatin involved in muscle atrophy of congenital neurogenic clubfoot. World J Clin Cases. 2019;7:2238-2246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Joe KJ, Huitron SS, Crawford JJ, Frink SJ. Idiopathic equinocavovarus foot deformity in an 8-year-old girl. Clin Orthop Relat Res. 2009;467:2482-2486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Bohner-Beke A, Kőnigné Péter A, Vass L, Halasi S, Kránicz J, Pusztafalvi H. [Hungarian validation of the Clubfoot Disease-Specific Instrument]. Orv Hetil. 2018;159:1269-1277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Babiker MO, Yeo TH, Goodwin S. A venous malformation presenting as toe walking. Pediatr Neurol. 2015;52:133-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Klemme WR, James P, Skinner SR. Latent onset unilateral toe-walking secondary to hemangioma of the gastrocnemius. J Pediatr Orthop. 1994;14:773-775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Nakamura T, Matsumine A, Nishiyama M, Uchida A, Sudo A. Recurrent ankle equinus deformity due to intramuscular hemangioma of the gastrocnemius: case report. Foot Ankle Int. 2011;32:905-907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Scheuer F. [Talipes equinus and Hemangioma]. Z Orthop Ihre Grenzgeb. 1952;81:640. [PubMed] |
| 12. | Umehara F, Matsuura E, Kitajima S, Osame M. Unilateral toe-walking secondary to intramuscular hemangioma in the gastrocnemius. Neurology. 2005;65:E15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Peyton C. Serial Casting of the Ankle and Knee in a Child With Vascular Anomaly of the Calf Musculature: A Case Report. Phys Ther. 2020;100:317-323. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Abraham J, Wall JC Jr, Diab M, Beaver C. Ponseti Casting vs. Soft Tissue Release for the Initial Treatment of Non-idiopathic Clubfoot. Front Surg. 2021;8:668334. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 15. | Radler C, Mindler GT. [Pediatric clubfoot : Treatment of recurrence]. Orthopade. 2016;45:909-924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Oesman I, Sari CM. Neglected neurogenic clubfoot treated with Achilles tendon lengthening using Z-plasty, total talectomy, and tibiocalcaneal arthrodesis. Int J Surg Case Rep. 2021;84:106051. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Agarwal A, Rastogi A, Rastogi P. Relapses in clubfoot treated with Ponseti technique and standard bracing protocol- a systematic analysis. J Clin Orthop Trauma. 2021;18:199-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 18. | Fuentes P, Cuchacovich N, Gutierrez P, Hube M, Bastías GF. Treatment of Severe Rigid Posttraumatic Equinus Deformity With Gradual Deformity Correction and Arthroscopic Ankle Arthrodesis. Foot Ankle Int. 2021;42:1525-1535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Bernasconi A, Najefi AA, Goldberg AJ. Comparison of Mechanical Axis of the Limb Versus Anatomical Axis of the Tibia for Assessment of Tibiotalar Alignment in End-Stage Ankle Arthritis. Foot Ankle Int. 2021;42:616-623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Alomari AI, Spencer SA, Arnold RW, Chaudry G, Kasser JR, Burrows PE, Govender P, Padua HM, Dillon B, Upton J, Taghinia AH, Fishman SJ, Mulliken JB, Fevurly RD, Greene AK, Landrigan-Ossar M, Paltiel HJ, Trenor CC 3rd, Kozakewich HP. Fibro-adipose vascular anomaly: clinical-radiologic-pathologic features of a newly delineated disorder of the extremity. J Pediatr Orthop. 2014;34:109-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 84] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 21. | Sung J, Kim JY. Fatty rind of intramuscular soft-tissue tumors of the extremity: is it different from the split fat sign? Skeletal Radiol. 2017;46:665-673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg. 1982;69:412-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2357] [Cited by in RCA: 2035] [Article Influence: 47.3] [Reference Citation Analysis (0)] |
| 23. | Domb BG, Khanna AJ, Mitchell SE, Frassica FJ. Toe-walking attributable to venous malformation of the calf muscle. Clin Orthop Relat Res. 2004;225-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 24. | Kryzak TJ Jr, DeGroot H 3rd. Adult onset flatfoot associated with an intramuscular hemangioma of the posterior tibialis muscle. Orthopedics. 2008;31:280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Hasan O, Fahad S, Sattar S, Umer M, Rashid H. Ankle Arthrodesis using Ilizarov Ring Fixator: A Primary or Salvage Procedure? Malays Orthop J. 2018;12:24-30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 26. | Reinke C, Bäcker H, Lotzien S, Schildhauer TA, Seybold D, Gessmann J. Arthrodesis of the Infected Knee Joint with the Ilizarov External Fixator: an Analysis of 13 Cases. Z Orthop Unfall. 2020;158:58-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |