Published online Apr 26, 2023. doi: 10.12998/wjcc.v11.i12.2788
Peer-review started: January 10, 2023
First decision: January 30, 2023
Revised: February 15, 2023
Accepted: March 29, 2023
Article in press: March 29, 2023
Published online: April 26, 2023
Processing time: 105 Days and 21.1 Hours
Hemophilia A is a rare inherited bleeding disorder caused by mutations in the factor VIII gene. This clotting factor plays an intrinsic role in the blood coagulation pathway. Patients with hemophilia may develop orthopedic manifestations such as hemarthrosis, but multiple malunion of fractures over the knee is rare and difficult to treat.
We report a patient with hemophilia A who developed severe knee osteoarthritis along with fracture malunion and nonunion. Total knee replacement was performed using a custom-made modular hinged knee prosthesis (cemented) equipped with extended distal and proximal stems. At 3 years’ follow-up, the patient exhibited excellent clinical function and remained satisfied with the surgical outcome. Surgical intervention was accompanied by rigorous coagulation factor replacement.
This case highlights various unique scenarios specific to individuals with hemophilia and fracture deformity.
Core Tip: This patient had hemophilia for many years, with hematopathic arthritis of both knees. An old fracture of the left lower extremity had healed, a distal femur fracture had recurred, and he had malunion of fractures of the proximal tibia and fibula. We resolved the left knee hematopathic arthritis, distal femur fracture nonunion, and proximal tibia fracture malunion with a single operation of total knee replacement with custom prosthesis.
- Citation: Yin DL, Lin JM, Li YH, Chen P, Zeng MD. Short-term outcome of total knee replacement in a patient with hemophilia: A case report and review of literature. World J Clin Cases 2023; 11(12): 2788-2795
- URL: https://www.wjgnet.com/2307-8960/full/v11/i12/2788.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i12.2788
Hemophilia A is a rare inherited bleeding disorder caused by mutations in the factor VIII gene. This clotting factor plays an intrinsic role in the blood coagulation pathway[1]. This disorder is known to be X-linked recessive and, is thus, more commonly encountered in males[2].
Hemophilia can be mild, moderate or severe, depending on the plasma factor levels of 6%–40%, 1%–5%, or < 1%, respectively[3]. Patients with hemophilia may develop orthopedic manifestations-hemarthrosis. Hemarthrosis is repeated bleeding into the joints, such as: Ankle, elbow and knee, leading to cartilage damage and degenerative articular changes, potentially resulting in severe osteoarthritis.
The third decade of life is the peak occurrence of the disease, and nearly 90% of patients with hemophilia have hemophiliac arthropathy[4]. The knee is the most involved joint in hemophilia, and some feasible treatment methods have been applied, and radiological and arthroscopic synovectomy is effective, in addition to arthrodesis, and most importantly, total knee replacement (TKR)[5-7]. The major surgical procedures can be safely performed in hemophilia patients with chronic arthropathy using available clotting factor concentrates, and TKR is considered the gold standard[8,9]. An increasing number of studies have reported TKR in patients with hemophilia[6,10-12], although this procedure is challenging due to the high risk of bleeding and periprosthetic joint infection[1,13,14].
However, cases involving patients with hemophiliac arthropathy and multiple malunion of fractures over the knee are rarely reported. Here, we report a patient with hemophilia and nonunion of a femoral fracture and malunion fractures of the tibia and fibula. The outcome of this patient has, to date, been satisfactory > 2 years after surgery. The patient exhibited excellent clinical function and has remained satisfied with the surgical outcome.
The patient was informed that anonymized data regarding the case would be submitted for publication, and he provided consent.
A 55-year-old man was diagnosed with moderate hemophilia A.
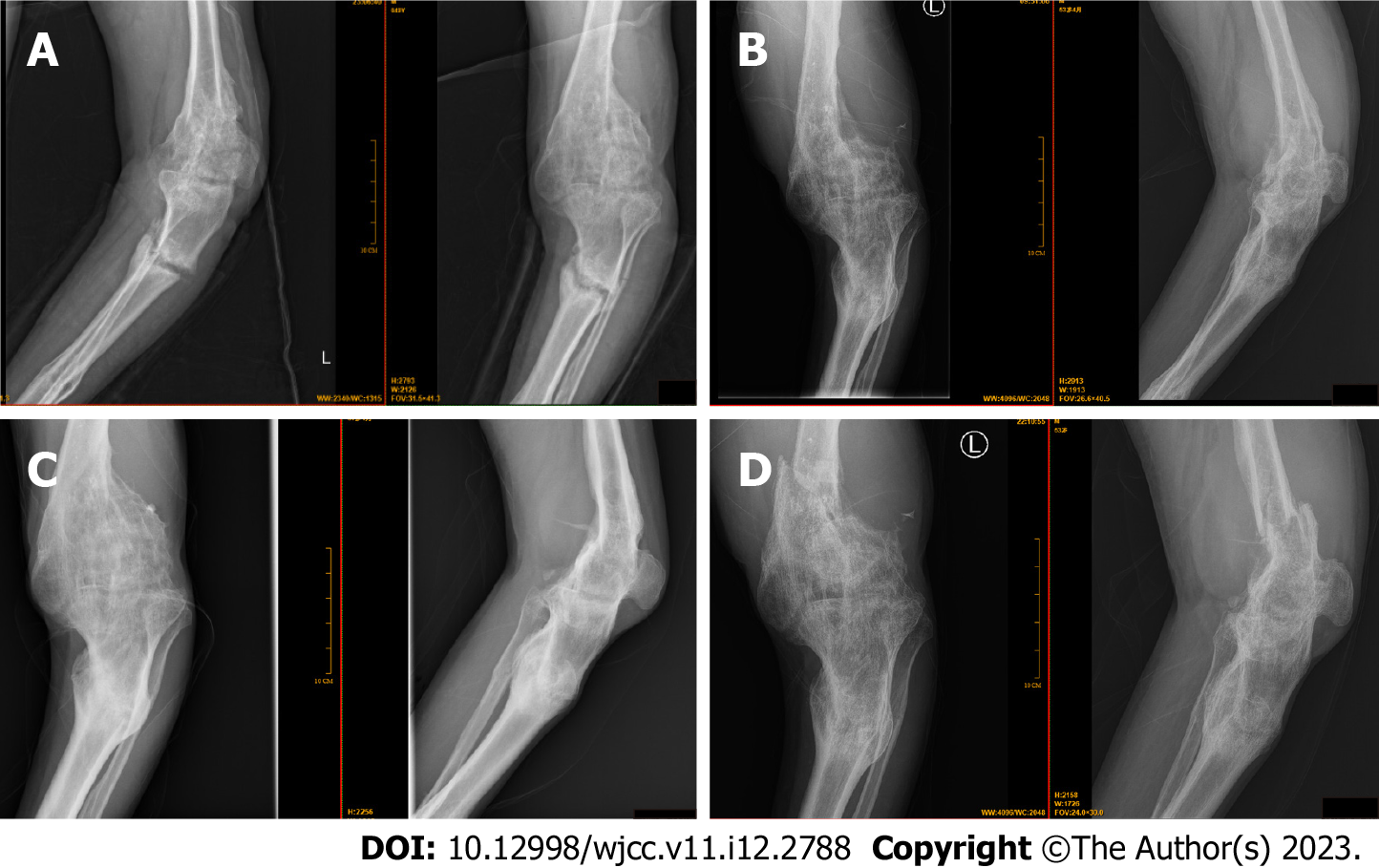
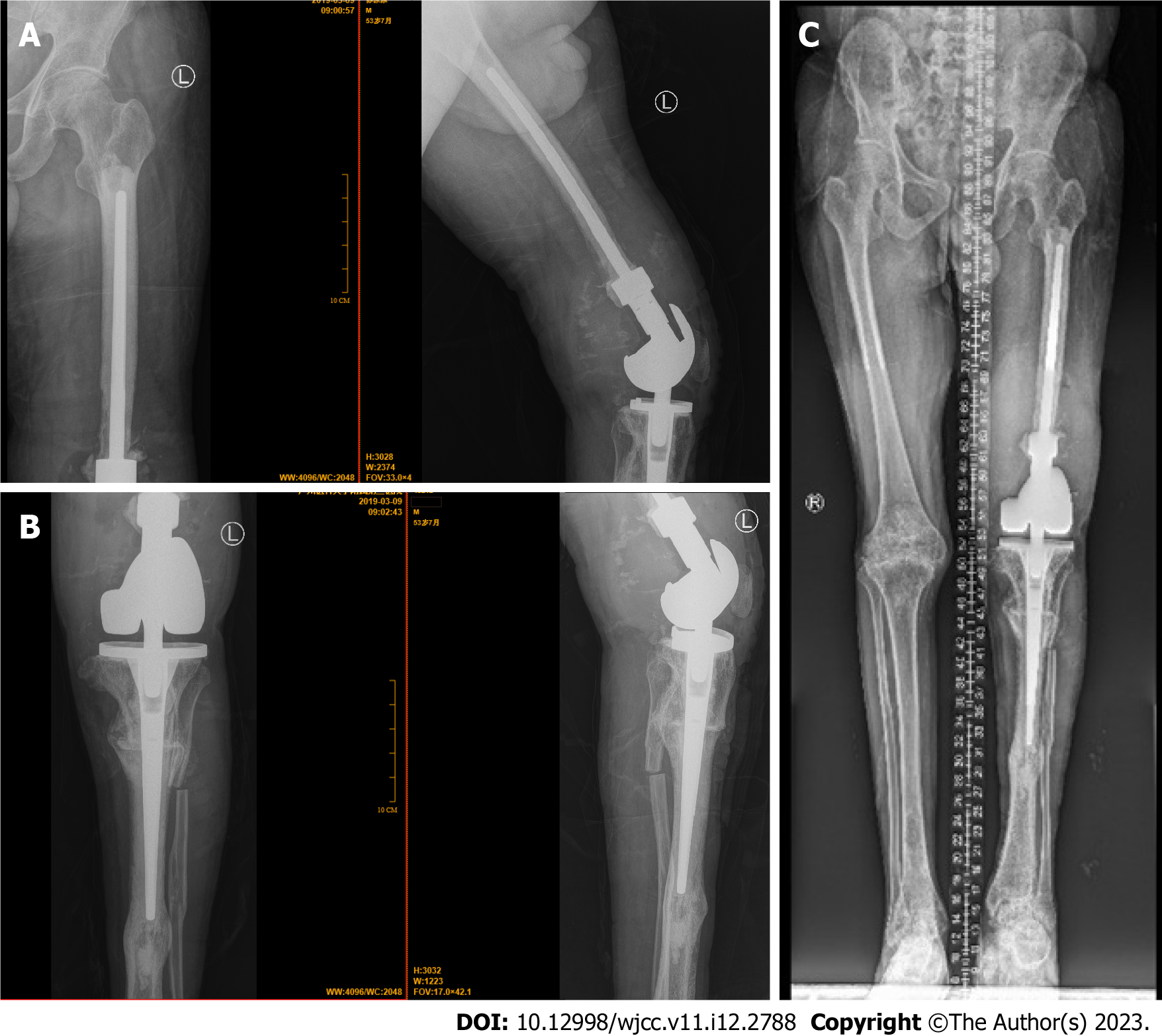
The patient sustained many fractures to his left thigh, in addition to tibia, fibula, and a femoral fracture in 2013. Due to economic reasons and the unique treatment difficulties in patients with hemophilia, all fractures had been treated nonsurgically with plaster fixation. Before and after the fractures in 2013, factor VIII was infused intermittently. However, medical hemostasis management was not standardized. Fortunately, all of the above fractures successfully healed in 2016, although deformity resulted (Figure 1A-C). He was unable to ambulate by himself. He sustained a fracture to his left thigh again in 2018, and the left knee had bony ankylosis (Figure 1D). Along with severe knee osteoarthritis, this prompted him to undergo surgery for his left thigh (Figure 2A and B). He consulted the authors due to severe pain and a severely dysfunctional left leg, although his right leg was also affected by hemophiliac arthritis (Figure 2C). At that time, the total range of motion (ROM) in his left knee joint was 0° and he had no mobility, with a Hospital for Special Surgery Knee Scale score (HSSKS)[15] of 30 (Tables 1 and 2). Panoramic X-ray of the lower limbs revealed that the left thigh was nearly 8 cm shorter than the right femur (Figures 2C-E).
| Variable | Preoperatively | Postoperatively | |
| 3 d | 16 mo | ||
| Flexion | 0 | 30 | 80 |
| Extension | 0 | 10 | 5 |
| Range of motion | 0 | 20 | 75 |
| Variable | Preoperatively | Postoperatively | |
| 3 d | 16 mo | ||
| Pain | 0 | 10 | 25 |
| Function | 2 | 6 | 15 |
| Range of motion | 0 | 3 | 11 |
| Muscle strength | 0 | 4 | 8 |
| Flexion deformity | 5 | 5 | 8 |
| Instability | 0 | 5 | 8 |
| Subtraction | -4 | -3 | -2 |
| Total score | 3 | 30 | 73 |
The patient had moderate hemophilia A.
The left thigh was nearly 8 cm shorter than the right thigh. The patient had left lower extremity dysfunction with tenderness at the distal femur and bone abrasion.
At the first examination, the patient’s serum factor VIII level was 5% and inhibitor of factor VIII was absent, and he was negative for hepatitis C and human immunodeficiency virus.
(1) Preoperative left knee anteroposterior and lateral radiographs in 2013, showed hemophiliac knee arthritis, old tibia and fibula fractures, and deformity of the distal femur fracture; (2) In 2016, radiographs showed aggravated hemophiliac knee arthritis with knee fusion, deformity of the distal femur fracture, and deformity of the tibia and fibula fractures; (3) On November 30, 2018, radiographs showed exacerbation of hemophiliac knee arthritis with knee fusion, deformity of the distal femur fracture, and deformity of the tibia and fibula fractures as before; and (4) On December 14, 2018, radiographs showed hemophiliac knee arthritis with knee fusion, deformity of the tibia and fibula fractures, and recurrent fresh fracture of the distal femur on the top of the original deformity.
Hemophiliac arthropathy of both knees; hemophiliac knee arthritis with left knee fusion; fracture of distal femur; deformity of the tibia and fibula; and hemophilia A.
To relieve joint dysfunction and pain in the left leg, TKR was scheduled. The other knee joint also appeared to require arthroplasty; however, this procedure was difficult for the patient to accept due to many factors, especially economic. The procedure was performed under the guidance of the expert consensus in China and a previous review[8,16]. Coagulation factors should be supplemented to 110% before the procedure, tranexamic acid should be used to prevent intraoperative bleeding[17], and should be supplemented according to operating duration, with a blood salvage system used during surgery. Blood loss during surgery in the present case was 900 mL, and the duration of the procedure was 4 h. The implants were cemented, and were a custom-made modular hinged knee prosthesis equipped with extended distal and proximal stems (Beijing Chunlizhengda Medical Instruments Co. Ltd., China) because it was necessary to treat both the femoral shaft fractures and the proximal tibial deformity fracture (Figure 3).
The plan for supplementation of clotting factors before, during and after surgery is summarized in Table 3. Rehabilitation exercise started on postoperative day 2 with partial weight bearing (Figure 4A and B). From previous investigators combined with patient characteristics, the patient received physical therapy from day 2 after the operative. Therapy sessions were carefully coordinated with factor replacement, also need to avoid exacerbation of pain or wound condition/hemostasis[18-20]. Furthermore, a continuous passive motion machine was used to restore total ROM of the knee joint, with flexion exercises starting at 45°. After 16 mo’ postoperative follow-up, the patient exhibited an ROM of 75° (5°–80°), with an HSSKS score of 73 (Table 2; Figure 4C-E and Video 1). At 3 years’ postoperative follow-up, the patient was satisfied with the left thigh outcome.
| Time of day | At surgery | 72 h | 1st week | 2nd week |
| Morning | 110 | 100 | 80 | > 50 |
| Evening | 110 | 100 | 80 | > 50 |
Hemophilia is among the most common bleeding disorders come across in orthopedic surgery. It is an X-linked recessive condition affecting 1 in 5000 males[3,7]. Factor deficiency leads to recurrent spontaneous hemarthroses, which then lead to contractures and early degenerative joint disease. The knee joint is the most common affected by hemophiliac arthropathy[7]. In a recent meta-analysis, the prevalence of hemophilia among males was estimated to be 5.5/100000 in Mainland China[21]. There were 16083 patients with hemophilia A and 2447 with hemophilia B registered in Mainland China in 2019[22]. The hemophilia care level in China lags behind that in developed countries[23]. Sun et al[24] found that hemophilia patients in China received less prophylaxis, these patients faced greater difficulty in obtaining replacement factor products, and were vulnerable to more annual bleeds. Currently, TKR is considered to be the gold standard for patients with hemophilia who develop severe arthropathy[6,25]. Several previous studies have reported satisfactory outcomes[25-28].
TKR in patients with hemophilia is a viable alternative to conventional methods of treatment for chronic arthropathy, and expectations for pain relief and functional gain can be high[10]. With continuous advances and developments in surgical treatment in recent years, and the emergence of recombinant clotting factors, the success ratio of surgical treatment for hemophilia has gradually increased[26]. In our case, we maintained a high level of clotting factor replacement throughout the first 2 wk postoperatively. Moreover, the level was higher than currently recommended by international guidelines. According to previous research, this can reduce the rate of infection[13]. Due to the complexity of orthopedic procedures, such as TKR and osteotomy, the duration of surgery is longer than normal, which increases the risk for intraoperative bleeding and infection. Postoperatively, the patient described in this report was treated with elastic bandages to prevent deep venous thrombosis. On postoperative days 2 and 7, intra-articular hemorrhage occurred twice, for which 150 and 300 mL of accumulated blood, respectively, was drawn from the knee joint under sterile conditions. Rehabilitation was effective. Safe rehabilitation exercises were prescribed after surgery and the patient used a walking cane the day after surgery[29] (Figure 4B). Physical therapy typically included isometric exercise for the quadriceps, hamstrings and gluteal muscles, knee ROM exercises include active and passive, and progressive resistive lower extremity exercises when the patient progressed[19]. We also prescribed rehabilitation to restore ROM of the knee joint by starting with continuous passive motion for functional exercises from postoperative day 2. All rehabilitation exercises followed daily supplementation of coagulation factors.
TKR is an effective procedure for improving ROM and decreasing functional deficits resulting from hemophiliac arthropathy. Knee score information show that TKR improves overall function[5]. TKR provides significant improvement in pain and better function in patients with end-stage hemophiliac arthropathy of the knee jiont. Peri- and postoperative care tends to be more complicated than in patients without hemophilia undergoing TKR and requires a multidisciplinary team approach[30]. With our patient, preoperative preparation included supplementation of clotting factors, an adjustment plan for supplementation, preparation of the prosthesis, and rehearsal of the surgical process. Postoperatively, we prevented possible complications such as hemorrhage, infection and venous thromboembolism. Our patient experienced intra-articular hemorrhage twice, with 150 and 300 mL of blood drained. However, under strict postoperative management and supplementation of coagulation factors, there was no postoperative infection and further bleeding. After careful postoperative rehabilitation, the patient achieved satisfactory recovery. Ideally, any patient with severe hemophilia should be followed-up by a specialist, with once or twice per year[20]. Our patient recover well during annual follow-up after discharge, with ambulatory function similar to healthy individuals.
Several important factors should be considered before considering surgery in patients with hemophilia. In particular, osteotomy orthopedic surgery should be performed at the same time. Osteotomy angle of the tibia, supplementation of clotting factors, customization of prostheses, and patient tolerance should all be considered. Postoperative rehabilitation exercise is also important to achieve good outcomes. Collectively, TKR using customized prostheses has been demonstrated to be a viable option for patients with hemophiliac arthropathy and fracture deformities.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Saito M, Japan; Velázquez-Saornil J, Spain S-Editor: Zhao S L-Editor: A P-Editor: Zhao S
| 1. | Franchini M, Mannucci PM. Past, present and future of hemophilia: a narrative review. Orphanet J Rare Dis. 2012;7:24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 158] [Cited by in RCA: 157] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 2. | Arnold WD, Hilgartner MW. Hemophilic arthropathy. Current concepts of pathogenesis and management. J Bone Joint Surg Am. 1977;59:287-305. [PubMed] |
| 3. | Mannucci PM, Tuddenham EG. The hemophilias--from royal genes to gene therapy. N Engl J Med. 2001;344:1773-1779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 720] [Cited by in RCA: 750] [Article Influence: 31.3] [Reference Citation Analysis (0)] |
| 4. | Rodriguez-Merchan EC, Valentino LA. Orthopedic disorders of the knee in hemophilia: A current concept review. World J Orthop. 2016;7:370-375. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 31] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Moore MF, Tobase P, Allen DD. Meta-analysis: outcomes of total knee arthroplasty in the haemophilia population. Haemophilia. 2016;22:e275-e285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 6. | Rodriguez-Merchan EC. Total knee replacement in haemophilic arthropathy. J Bone Joint Surg Br. 2007;89:186-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 79] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 7. | Liddle AD, Rodriguez-Merchan EC. Evidence-Based Management of the Knee in Hemophilia. JBJS Rev. 2017;5:e12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Solimeno LP, Pasta G. Knee and Ankle Arthroplasty in Hemophilia. J Clin Med. 2017;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 9. | Srivastava A, Santagostino E, Dougall A, Kitchen S, Sutherland M, Pipe SW, Carcao M, Mahlangu J, Ragni MV, Windyga J, Llinás A, Goddard NJ, Mohan R, Poonnoose PM, Feldman BM, Lewis SZ, van den Berg HM, Pierce GF; WFH Guidelines for the Management of Hemophilia panelists and co-authors. WFH Guidelines for the Management of Hemophilia, 3rd edition. Haemophilia. 2020;26 Suppl 6:1-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 431] [Cited by in RCA: 1155] [Article Influence: 231.0] [Reference Citation Analysis (0)] |
| 10. | Figgie MP, Goldberg VM, Figgie HE 3rd, Heiple KG, Sobel M. Total knee arthroplasty for the treatment of chronic hemophilic arthropathy. Clin Orthop Relat Res. 1989;98-107. [PubMed] |
| 11. | Norian JM, Ries MD, Karp S, Hambleton J. Total knee arthroplasty in hemophilic arthropathy. J Bone Joint Surg Am. 2002;84:1138-1141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 61] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 12. | Habermann B, Miesbach W, Sahner LM, Kurth A. [Total knee replacement in haemophilic arthropathy. A clinical and radiological evaluation of 30 patients]. Hamostaseologie. 2010;30 Suppl 1:S104-S106. [PubMed] |
| 13. | Wong JM, Mann HA, Goddard NJ. Perioperative clotting factor replacement and infection in total knee arthroplasty. Haemophilia. 2012;18:607-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Song SJ, Bae JK, Park CH, Yoo MC, Bae DK, Kim KI. Mid-term outcomes and complications of total knee arthroplasty in haemophilic arthropathy: A review of consecutive 131 knees between 2006 and 2015 in a single institute. Haemophilia. 2018;24:299-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 15. | Bach CM, Nogler M, Steingruber IE, Ogon M, Wimmer C, Göbel G, Krismer M. Scoring systems in total knee arthroplasty. Clin Orthop Relat Res. 2002;184-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 75] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 16. | Tong KM, Wang JD, Chang ST, Cheng YY, Wang SS. Outcome of perioperative hemostatic management in patients with hemophilia without inhibitors undergoing 161 invasive or surgical procedures. J Chin Med Assoc. 2018;81:926-929. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Huang ZY, Huang Q, Zeng HJ, Ma J, Shen B, Zhou ZK, Pei FX. Tranexamic acid may benefit patients undergoing total hip/knee arthroplasty because of haemophilia. BMC Musculoskelet Disord. 2019;20:402. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 18. | Atilla B, Güney-Deniz H. Musculoskeletal treatment in haemophilia. EFORT Open Rev. 2019;4:230-239. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 19. | Kamath AF, Horneff JG, Forsyth A, Nikci V, Nelson CL. Total knee arthroplasty in hemophiliacs: gains in range of motion realized beyond twelve months postoperatively. Clin Orthop Surg. 2012;4:121-128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Lobet S, Hermans C, Lambert C. Optimal management of hemophilic arthropathy and hematomas. J Blood Med. 2014;5:207-218. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 89] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 21. | Qu Y, Nie X, Yang Z, Yin H, Pang Y, Dong P, Zhan S. The prevalence of hemophilia in mainland China: a systematic review and meta-analysis. Southeast Asian J Trop Med Public Health. 2014;45:455-466. [PubMed] |
| 22. | Huang Z, Nicholas S, Yang Y, Chen X, Maitland E, Ma Y, Shi X. Medical costs and hospital utilization for hemophilia A and B urban inpatients in China: a national cross-sectional study. BMC Health Serv Res. 2022;22:230. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 23. | Dou X, Poon MC, Yang R. Haemophilia care in China: Achievements in the past decade. Haemophilia. 2020;26:759-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 24. | Sun J, Zhao Y, Yang R, Guan T, Iorio A; Chinese HERO study group. The demographics, treatment characteristics and quality of life of adult people with haemophilia in China - results from the HERO study. Haemophilia. 2017;23:89-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 25. | Solimeno LP, Mancuso ME, Pasta G, Santagostino E, Perfetto S, Mannucci PM. Factors influencing the long-term outcome of primary total knee replacement in haemophiliacs: a review of 116 procedures at a single institution. Br J Haematol. 2009;145:227-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 87] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 26. | Goddard NJ, Mann HA, Lee CA. Total knee replacement in patients with end-stage haemophilic arthropathy: 25-year results. J Bone Joint Surg Br. 2010;92:1085-1089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 78] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 27. | Zingg PO, Fucentese SF, Lutz W, Brand B, Mamisch N, Koch PP. Haemophilic knee arthropathy: long-term outcome after total knee replacement. Knee Surg Sports Traumatol Arthrosc. 2012;20:2465-2470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 37] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 28. | Bae JK, Kim KI, Lee SH, Yoo MC. Mid-to Long-Term Survival of Total Knee Arthroplasty in Hemophilic Arthropathy. J Clin Med. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 29. | Scaturro D, Benedetti MG, Lomonaco G, Tomasello S, Farella MGG, Passantino G, Frizziero A, Letizia Mauro G. Effectiveness of rehabilitation on pain and function in people affected by hemophilia. Medicine (Baltimore). 2021;100:e27863. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 30. | Wallny TA, Strauss AC, Goldmann G, Oldenburg J, Wirtz DC, Pennekamp PH. Elective total knee arthroplasty in haemophilic patients. Proposal for a clinical pathway. Hamostaseologie. 2014;34 Suppl 1:S23-S29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |