Published online Apr 26, 2023. doi: 10.12998/wjcc.v11.i12.2729
Peer-review started: December 24, 2022
First decision: February 28, 2023
Revised: March 8, 2023
Accepted: March 27, 2023
Article in press: March 27, 2023
Published online: April 26, 2023
Processing time: 122 Days and 7.1 Hours
Postpartum depression refers to a depressive episode or depressive symptoms up to 12 mo after delivery. Trait mindfulness has presented a protective factor for postpartum depressive symptoms and proved efficient in improving relationship satisfaction among couples.
To investigate the correlations among mindfulness, marital quality, anxiety, and depression in a large city in western China during the post-corona virus infectious disease-2019 era and determine whether trait mindfulness mediates the relationship between marital quality and postpartum anxiety and depression among primiparas.
A cross-sectional study was conducted. The self-administered questionnaire was submitted online through smartphones. The levels of mindfulness, anxiety, depression, and marital quality were respectively investigated by the mindful attention awareness scale (MAAS), the self-rating anxiety scale (SAS), the self-rating depression scale (SDS), and the marriage perception scale (MPS) in these enrolled Han and Tujia primiparas.
No statistical significance was observed in the prevalence of postpartum anxiety and depression, nor scores of MAAS and MPS-Total in different regions or ethnicities (P > 0.05). However, MPS-Marital interaction (P < 0.05), MPS-Family relationship (MPS-FR) (P < 0.01), and MPS-Marital conflict (MPS-MC) (P < 0.01) scores of urban primiparas were higher than those of rural primiparas. The MPS-MC score of Han primiparas was higher than that of Tujia primiparas (P < 0.05). Negative correlations were observed between MAAS and SAS (r = -0.457, P < 0.01), and MAAS and SDS (r = -0.439, P < 0.01). SAS has revealed a highly positive correlation with SDS (r = 0.720, P < 0.01) and a weak negative correlation with MPS (r = -0.200, P < 0.05). Besides, a weak negative correlation was observed between MAAS and MPS-MC (r = -0.184, P < 0.05), and a weak positive correlation was noticed between SAS and MPS-MC (r = -0.225, P < 0.01). Mediation analysis demonstrated a full mediation effect of mindfulness level on the relationship between MPS-FR and postpartum anxiety (P < 0.05, 95%CI: -0.384 to 0.033), MPS-MC and postpartum anxiety (P < 0.01, 95%CI: 0.027-0.193), MPS-FR and postpartum depression (P < 0.05, 95%CI: -0.365 to 0.031), and MPS-MC and postpartum depression (P < 0.01, 95%CI: 0.022-0.206).
Mindfulness demonstrates negative correlations with marital conflict, postpartum anxiety and depression, and it may have cross-ethnic and trans-regional characteristics. Although the mindfulness levels have revealed no significant mediating effect between the total score of marital quality and postpartum depression in this study, it demonstrates a full mediation effect on the relationships between family relationships, marital conflict, and postpartum anxiety and depression.
Core Tip: Postpartum depression is a common mental complication during the postpartum period. This cross-sectional observational study aimed to investigate the correlations among mindfulness, marital quality, anxiety, and depression in different regions and ethnicities in a large city in western China during the post-corona virus infectious disease-2019 era and determine whether trait mindfulness mediates the relationship between marital quality and postpartum anxiety and depression among primiparas. Mindfulness is closely related to the mental health conditions of primiparas, and it may have cross-ethnic and trans-regional characteristics. Although the mindfulness levels revealed no significant mediating effect between the total score of marital quality and postpartum depression in this study, it demonstrated a full mediation effect on the relationship between family relationships, marital conflict, and postpartum anxiety and depression. Our findings can provide a reference for further application of mindfulness in Chinese postpartum mental disorders.
- Citation: Yang J, Lin XZ, Guo QW, Wang CL, Yang RY, Zhang JW, Zeng Y. Mediating effect of mindfulness level on the relationship between marital quality and postpartum depression among primiparas. World J Clin Cases 2023; 11(12): 2729-2739
- URL: https://www.wjgnet.com/2307-8960/full/v11/i12/2729.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i12.2729
The number and proportion of disability-adjusted life-years (DALYs) due to mental disorders have increased since 1990[1], and depressive and anxiety disorders have been listed among the top three causes of DALYs in females[2]. Postpartum depression, a common mental complication during the postpartum period, refers to a depressive episode or depressive symptoms up to 12 mo after delivery[3,4]. Postpartum depression may lead to long-term cognitive impairment, emotional difficulties, and behavioral problems in both mother and child[5], and its prevalence in China has presented a significantly increasing trend in recent years[6]. Therefore postpartum depression has been a hot spot for research and intervention[6,7].
Each individual's mental health, including that of a primipara, has always been influenced by unique social and environmental factors[8], and accumulating evidence suggests that marital quality plays an essential role in postpartum depression[9,10]. Meanwhile, trait mindfulness has proved efficient in improving relationship satisfaction among couples[11].
Mindfulness refers to moment-to-moment awareness, and it is based on our inner capacities for relaxation, paying attention, awareness, and insight[12]. Mindfulness helps promote relief from depressing thoughts and feelings, and mindfulness-based therapy has been developed as an effective psychological intervention for depressive individuals[13]. Moreover, trait mindfulness has presented a protective factor for postpartum depressive symptoms[14]. However, there is scant evidence on the mediating effect of mindfulness levels on the relationship between marital quality and postpartum depression among primiparas.
The prevalence of postpartum depression across Mainland China varied in different provinces[3,6], and southwest China has been among the regions suggested to pay more attention[3]. Thus, this observational study aims to investigate the mediating effect of mindfulness levels on relationships between marital quality and postpartum depression among primiparas in southwestern China and provide a reference for future application of mindfulness in Chinese postpartum mental disorders.
Ethics approval for the study was granted by the Ethics Committee of the Second Affiliated Hospital of Chongqing Medical University (2021-288). All participants provided informed consent.
Participants in this cross-sectional study were a subset of the Chongqing Science and Health Joint Medical Research Project (No. 2021MSXM034), with an estimated sample size of 120 subjects[15]. Two tertiary hospitals from a large city in western China were enrolled in this study, including one from a developed main urban area and the other from an underdeveloped Tujia ethnic area. Primiparas who gave birth in or visited these hospitals within 4 wk postpartum were randomly sampled and consecutively recruited between November 2021 and June 2022, with no compensation or honoraria. Primiparas with different lifestyles and cultural customs have no difference in access to medical services. The inclusion criteria were: (1) Primiparas aged from 18 to 40 years old; (2) proficiency in spoken Chinese; (3) good compliance with completing online questionnaires; and (4) providing informed consent.
The exclusion criterion was as follows: (1) Severe physical disease; (2) gestational hypertension or gestational diabetes mellitus; (3) premature delivery or multiple pregnancies; (4) mental disorder or personality disorder; (5) previous history of labor or labor induction; (6) previous mindfulness training; and (7) non-local resident. A total of 132 primiparas were initially included. All enrolled participants underwent an initial interview to confirm their eligibility for this study, during which seven primiparas were excluded. Three primiparas withdrew from the study, and one primipara returned incomplete questionnaires. Thus, 121 individuals were eventually enrolled (71 from developed and 50 from underdeveloped areas). All participants received a full explanation of this study from the researchers and volunteered to participate. After signing the informed consent, the questionnaire was completed and submitted online through smartphones. Socio-demographic characteristics were obtained through interviews and personal reports. The levels of mindfulness, anxiety, depression and marriage perception were respectively investigated in these enrolled primiparas. All data is encrypted to ensure privacy.
The mindful attention awareness scale (MAAS): MAAS is an effective and reliable instrument for measuring mindfulness levels[16,17]. The MAAS score has proven a significant and inverse association with various mental health indicators, including depression, anxiety, stress, hostility, and negative affect, and also a positive relationship with psychological and physical health, including optimism, self-esteem, self-control, and life satisfaction, in contrast[16,18]. The Chinese version of MAAS presents a Cronbach's α coefficient of 0.89 and a two-week test-retest reliability of 0.82, indicating good reliability, similar results to the original English version, and acceptable psychometric quality in the Chinese population[19].
The self-rating anxiety scale (SAS) and self-rating depression scale (SDS): Depression and anxiety were assessed via the SDS and SAS[20,21]. The reliability and validity of SDS and SAS have been examined in the Chinese population[22,23]. Higher scores of SDS or SAS indicate a higher level of depression or anxiety, respectively. According to the Chinese norm, a score of 50 or above indicates anxiety or depression[24].
The marriage perception scale (MPS): MPS is an effective tool to assess the perception of marriage in urban and rural China, and MPS takes participants' subjective evaluations and feelings about their own marital life as the leading indicator of marital quality evaluation. MPS presents a Cronbach's α coefficient of 0.889 and a four-week test-retest reliability of 0.758, indicating good reliability and stability[25].
Statistical analysis was performed using SPSS 26.0 software (IBM SPSS 26.0, SPSS Inc.) and SPSSAU (version 22.0, online application software, https://www.spssau.com). Continuous variables were compared via the t-test or Wilcoxon test, and categorical variables were compared using Chi-square tests or Fisher exact tests. Correlation analysis was performed using Pearson correlation analysis, and the mediating effects were tested by the bootstrap method. Statistical significance was considered if P < 0.05.
The study sample consisted of 121 participants, among which 71 (58.68%) were from rural areas, and 61 (50.41%) were Tujia primiparas. Age ranged from 18 to 40, with a mean of 27.26 years (SD = 3.60). Sixty-eight primiparas (56.20%) have an educational experience of junior college or below, while 53 primiparas (43.80%) have experienced undergraduate or above. These results are summarized in Table 1.
| Variables | n | % |
| Age (yr) | ||
| 18-25 | 37 | 30.58 |
| 26-30 | 66 | 54.54 |
| 31-35 | 14 | 11.57 |
| 36-40 | 4 | 3.31 |
| Regions | ||
| Urban | 50 | 41.32 |
| Rural | 71 | 58.68 |
| Ethnicity | ||
| Han | 60 | 49.59 |
| Tujia | 61 | 50.41 |
| Educational Status | ||
| Junior high school or below | 13 | 10.74 |
| Senior high school | 23 | 19.01 |
| Junior college | 32 | 26.45 |
| Undergraduate | 49 | 40.5 |
| Postgraduate | 4 | 3.3 |
Anxiety and depression presented in 19 (15.70%) and 62 (51.24%) primiparas, respectively, among which 10 (20.00%) of anxiety and 33 (66.00%) of depression were in urban primiparas, 9 (12.68%) of anxiety and 29 (40.85%) of depression in rural primiparas, while 9 (15.00%) of anxiety and 33 (55.00%) of depression in Han ethnicity, 10 (16.39%) of anxiety and 29 (47.54%) of depression in Tujia ethnicity. No statistical significance was observed in the prevalence of postpartum anxiety and depression in different regions or ethnicities (Table 2).
| SAS (n) | χ2 | P value | SDS (n) | χ2 | P value | |||
| Normal | Abnormal | Normal | Abnormal | |||||
| Urban | 40 | 10 | 0.084 | 0.772 | 17 | 33 | 0.674 | 0.412 |
| Rural | 62 | 9 | 42 | 29 | ||||
| Han | 41 | 9 | 0.044 | 0.833 | 17 | 33 | 0.674 | 0.412 |
| Tujia | 61 | 10 | 42 | 29 | ||||
No significant differences were observed in MAAS or MPS-Total between different regions (P > 0.05); however, MPS-Marital interaction (MPS-MI) (P < 0.05), MPS-Family relationship (MPS-FR) (P < 0.01), and MPS-Marital conflict (MPS-MC) (P < 0.01) scores of urban primiparas were significantly higher than those of rural primiparas (Table 3). In contrast, no significant differences between Han and Tujia primiparas were noticed in MAAS, MPS-Total, MPS-MI, or MPS-FR (P > 0.05); however, the MPS-MC score of Han primiparas was higher than that of Tujia primiparas (P < 0.05) (Table 4).
| Region | mean ± SD | t value | P value | |
| MAAS | Urban | 63.86 ± 11.86 | -0.416 | 0.678 |
| Rural | 64.76 ± 11.63 | |||
| MPS-Total | Urban | 62.78 ± 12.85 | 1.611 | 0.11 |
| Rural | 58.35 ± 17.38 | |||
| MPS-MI | Urban | 59.22 ± 9.81 | 2.626 | 0.01 |
| Rural | 54.24 ± 1059 | |||
| MPS-FR | Urban | 30.66 ± 4.22 | 3.965 | < 0.001 |
| Rural | 26.8 ± 6.47 | |||
| MPS-MC | Urban | 27.1 ± 4.29 | 3.785 | < 0.001 |
| Rural | 22.69 ± 8.38 |
| Ethnicity | mean ± SD | t value | P value | |
| MAAS | Han | 64.6 ± 10.96 | 0.349 | 0.727 |
| Tujia | 63.85 ± 12.5 | |||
| MPS-Total | Han | 59.58 ± 14.71 | -0.227 | 0.821 |
| Tujia | 60.24 ± 16.67 | |||
| MPS-MI | Han | 56.65 ± 10.62 | -0.447 | 0.656 |
| Tujia | 55.78 ± 10.62 | |||
| MPS-FR | Han | 28.88 ± 5.5 | 0.975 | 0.332 |
| Tujia | 27.81 ± 6.45 | |||
| MPS-MC | Han | 25.95 ± 5.99 | 1.997 | 0.048 |
| Tujia | 23.36 ± 8.01 |
Significant but moderate negative correlations were observed between MAAS and SAS (r = -0.457, P < 0.01), and MAAS and SDS (r = -0.439, P < 0.01). SAS has revealed a highly positive correlation with SDS (r = 0.720, P < 0.01), and a weak negative correlation with MPS (r = -0.200, P < 0.05). Besides, a weak negative correlation was observed between MAAS and MPS-MC (r = -0.184, P < 0.05), and a weak positive correlation was noticed between SAS and MPS-MC (r = -0.225, P < 0.01) (Table 5).
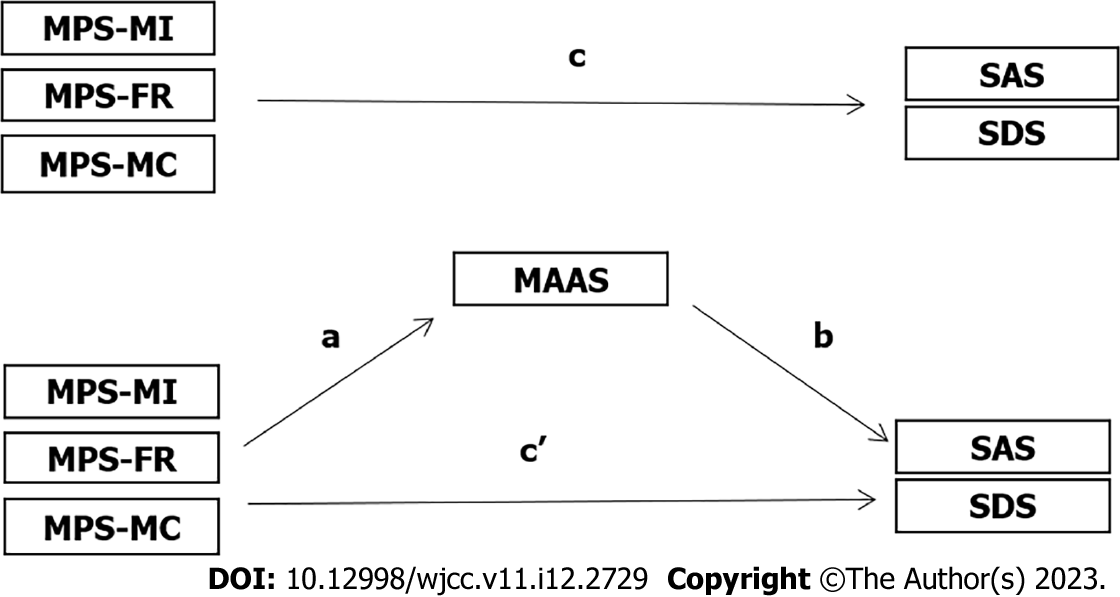
MPS-MI, MPS-FR, and MPS-MC were analyzed as independent variables X1, X2, X3, postpartum anxiety and depression as dependent variables Y1, Y2, and mindfulness level as mediating variable M. Three types of mediation analysis model are established: Firstly, the regression model of independent variable X (X1, X2, X3) and dependent variable Y (Y1, Y2); secondly, the regression model of independent variable X (X1, X2, X3) and mediating variable M; thirdly, the regression model of the independent variable X (X1, X2, X3) and the mediating variable M together with the dependent variable Y (Y1, Y2) (Figure 1). Mediation analysis demonstrated a full mediation effect of mindfulness level on the relationships between MPS-FR and postpartum anxiety (P < 0.05, 95%CI: -0.384 to 0.033), MPS-MC and postpartum anxiety (P < 0.01, 95%CI: 0.027-0.193) (Table 6), MPS-FR and postpartum depression (P < 0.05, 95%CI: -0.365 to 0.031), and MPS-MC and postpartum depression (P < 0.01, 95%CI: 0.022-0.206) (Table 7).
| Mediating relationship | c (Total effect) | a | b | a × b (ME value) | a × b (Boot SE) | a × b (z value) | a × b (P value) | a × b (95% Boot CI) | c' (Direct effect) |
| MPS→MAAS→SAS | -0.100d | 0.091 | -0.297e | -0.027 | 0.046 | -0.592 | 0.554 | -0.146-0.029 | -0.073 |
| MPS-MI→MAAS→SAS | -0.083 | -0.304 | -0.296e | 0.09 | 0.08 | 1.128 | 0.259 | -0.038-0.273 | -0.173 |
| MPS-FR→MAAS→SAS | -0.073 | 0.772d | -0.296e | -0.228 | 0.105 | -2.182 | 0.029 | -0.384-0.033 | 0.155 |
| MPS-MC→MAAS→SAS | 0.285e | -0.408e | -0.296e | 0.121 | 0.042 | 2.84 | 0.005 | 0.027-0.193 | 0.164 |
| Mediating relationship | c (Total effect) | a | b | a × b (ME value) | a × b (Boot SE) | a × b (z value) | a × b (P value) | a × b (95% Boot CI) | c' (Direct effect) |
| MPS→MAAS→SDS | -0.113 | 0.091 | -0.414e | -0.038 | 0.044 | -0.855 | 0.392 | -0.143-0.026 | -0.076 |
| MPS-MI→MAAS→SDS | -0.034 | -0.304 | -0.413e | 0.125 | 0.078 | 1.615 | 0.106 | -0.039-0.267 | -0.159 |
| MPS-FR→MAAS→SDS | -0.204 | 0.772d | -0.413e | -0.319 | 0.101 | -3.166 | 0.002 | -0.365-0.031 | 0.115 |
| MPS-MC→MAAS→SDS | 0.317d | -0.408e | -0.413e | 0.169 | 0.047 | 3.597 | < 0.001 | 0.022-0.206 | 0.149 |
The prevalence of postpartum depression has been affected by numerous factors, including marital quality, life stress, social support, income, and region[9]. This study of Han and Tujia primipara in a large southwestern city of China has demonstrated the prevalence of postpartum anxiety and depression as 15.70% and 51.24%, respectively. The prevalence of postpartum anxiety among primiparas in Chongqing is similar to the previous data from other Chinese cities[26]. However, the elevation in the prevalence of postpartum depression may be related to economic and regional differences, varied instruments and cut-off scores, selection bias due to voluntary enrollment, and the research period during corona virus infectious disease-2019 (COVID-19) rather than the non-pandemic period[3,27]. This study has provided a reference for currently limited data on postpartum anxiety and depression among Tujia primiparas and comparisons with Han primiparas. This study revealed no statistical significance in the prevalence of postpartum anxiety and depression between Tujia and Han ethnicities, while another survey before COVID-19 presented varied incidences between Kazak and Han women[28]. These differences may be related to different regions, comparisons between ethnicities, instruments used, and research periods. The prevalence of postpartum anxiety and depression in this study also suggests that mental disorders are postpartum complications worthy of attention and timely interventions.
Previous studies have paid little attention to the influence of cultural differences in different regions and ethnicities in China on mindfulness levels. According to the results of this study, there is no statistically significant difference in trait mindfulness among different regions and ethnicities, which indicates that trait mindfulness may have cross-ethnic and trans-regional characteristics. Thus, further research in this field is necessary. This study has demonstrated significant negative correlations between mindfulness levels and postpartum anxiety and depression, which suggests trait mindfulness is closely related to mental health conditions of primiparas. Previous studies have also reached the same conclusion[29]. This study also shows that the trait mindfulness of primipara has no significant correlation with the overall score of marital quality. However, mindfulness negatively correlates with the marital conflict factor in marital quality, while marital conflict is positively correlated with postpartum anxiety. That is, the higher the level of mindfulness, the less marital conflict, and the lower the level of anxiety, the less marital conflict. We consider that the role of mindfulness in reducing marital conflict is related to its benefits in increasing happiness and relationship satisfaction[30].
Although the mindfulness levels revealed no significant mediating effect between the total score of marital quality and postpartum depression in this study, it demonstrated a full mediation effect on the relationships between family relationships, marital conflict, and postpartum anxiety and depression. Studies have shown that primiparity and good family relations, social support, and economic conditions are positive factors for the good quality of life of pregnant and postpartum women[31]. However, in the years since the COVID-19 outbreak, the worldwide prevalence of postpartum depression has presented a significantly increasing trend due to numerous potential causes, including disease-related stress and anxiety and lack of social support[6,27]. The relative decline in social support due to decreased social interaction and the recent downturn in economic conditions during the post-COVID-19 era have made good marital quality and relationships increasingly important for primiparas' emotional stability and quality of life. Distress from intimate relationships has already been proven as a causal risk factor for depression[32], while close marital or cohabiting relationships have assisted in lower depression rates during the COVID-19 pandemic[33]. Mindfulness is a protective factor against depression, anxiety, and other psychological distress in the post-COVID-19 era[34]. Mindfulness may affect marital satisfaction by regulating psychological distress, emotional regulation, empathy, marital intimacy, and positive emotions[35], and higher mindfulness has presented an association with higher levels of happiness and reduced anxiety and depression symptoms through a connection with both a sense of purpose in life and positive outcomes[36]. Moreover, mindfulness has demonstrated benefits in promoting general health among couples in China[37], and smartphone-based mindfulness training has been proven effective in improving perinatal depression for those with a potential risk of depression[38]. Although higher trait mindfulness may not lead to better emotional recognition, it was positively associated with cognitive empathy and improved emotional skills[39]. In addition, the previous study has indicated that trait mindfulness can increase relationship satisfaction in couples by impacting their forgiving ability[11]. The above effects of mindfulness may be the potential reasons for mindfulness's positive full mediation effect on the relationship between family relationships, marital conflict, and postpartum anxiety and depression.
This study had some limitations. First, voluntary participation may have led to a selection bias, and self-administered questionnaires may also lead to a reporting bias. Second, this was a cross-sectional observational study, and further prospective studies are required to confirm the current findings. Third, although the results revealed a cross-ethnic characteristic of mindfulness, more participants from different ethnicities and regions need to be recruited in future studies to testify to current findings.
Mindfulness is closely related to the mental health conditions of primiparas due to negative correlations with both postpartum anxiety and depression, and it may have cross-ethnic and trans-regional characteristics. Mindfulness is also negatively correlated with marital conflict, while marital conflict is positively correlated with postpartum anxiety. Although the mindfulness levels have revealed no significant mediating effect between the total score of marital quality and postpartum depression in this study, it demonstrates a full mediation effect on the relationships between family relationships, marital conflict, and postpartum anxiety and depression.
Postpartum depression is a common mental complication during the postpartum period, and it may lead to long-term cognitive impairment, emotional difficulties, and behavioral problems in both mother and child. Trait mindfulness has proved efficient in improving relationship satisfaction among couples, while marital quality is essential in postpartum depression.
This manuscript investigates the correlations among mindfulness, marital quality, anxiety, and depression in different regions and ethnicities in a large city in western China during the post-corona virus infectious disease-2019 era and whether trait mindfulness mediates the relationship between marital quality and postpartum anxiety and depression among primiparas. Our findings can provide a reference for further application of mindfulness in Chinese postpartum mental disorders.
This observational study aims to investigate the mediating effect of mindfulness levels on relationships between marital quality and postpartum depression among primiparas in southwestern China and provide a reference for the future application of mindfulness in Chinese postpartum mental disorders.
This cross-sectional study was conducted in Chongqing, China, from November 2021 and June 2022. The self-administered questionnaire was completed and submitted online through smartphones. The levels of mindfulness, anxiety, depression, and marital quality were respectively investigated by the mindful attention awareness scale, the self-rating anxiety scale, the self-rating depression scale, and the marriage perception scale in these enrolled Han and Tujia primiparas. In contrast, previous studies have paid little attention to the influence of cultural differences in different regions and ethnicities in China on mindfulness levels.
This observational study found no statistically significant difference in trait mindfulness among different regions and ethnicities. Significant negative correlations have been observed between mindfulness levels and postpartum anxiety and depression. The marriage perception scale (MPS)-marital Interaction, MPS-family relationship (FR), and MPS-marital conflict (MC) scores of urban primiparas were higher than those of rural primiparas. Mediation analysis demonstrated a full mediation effect of mindfulness level on the relationship between MPS-FR and postpartum anxiety, MPS-MC and postpartum anxiety, MPS-FR and postpartum depression, and MPS-MC and postpartum depression.
Mindfulness is closely related to the mental health conditions of primiparas due to negative correlations with both postpartum anxiety and depression, and it may have cross-ethnic and trans-regional characteristics. Mindfulness is also negatively correlated with marital conflict, while marital conflict is positively correlated with postpartum anxiety. This study demonstrates a full mediation effect on the relationships between family relationships, marital conflict, and postpartum anxiety and depression. Therefore, attempts can be made to improve postpartum anxiety and depression by increasing levels of mindfulness.
Further prospective studies with more participants from different ethnicities and regions are required in future studies to testify to current findings.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Committee member, Psychiatric Medicine Committee of Chongqing Medical Association; Committee member, Psychosomatic and Behavioral Medicine Committee of Chongqing Medical Association; and Committee member, Chongqing Maternal and Child Health Association.
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Byeon H, South Korea; Nooripour R, Iran S-Editor: Li L L-Editor: A P-Editor: Yu HG
| 1. | GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9:137-150. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 436] [Cited by in RCA: 2605] [Article Influence: 868.3] [Reference Citation Analysis (0)] |
| 2. | GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204-1222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11327] [Cited by in RCA: 9637] [Article Influence: 1927.4] [Reference Citation Analysis (35)] |
| 3. | Mu TY, Li YH, Pan HF, Zhang L, Zha DH, Zhang CL, Xu RX. Postpartum depressive mood (PDM) among Chinese women: a meta-analysis. Arch Womens Ment Health. 2019;22:279-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 4. | Yan J, Liu Y, Cao L, Zheng Y, Li W, Huang G. Association between Duration of Folic Acid Supplementation during Pregnancy and Risk of Postpartum Depression. Nutrients. 2017;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 5. | Sockol LE, Epperson CN, Barber JP. Preventing postpartum depression: a meta-analytic review. Clin Psychol Rev. 2013;33:1205-1217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 95] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 6. | Nisar A, Yin J, Waqas A, Bai X, Wang D, Rahman A, Li X. Prevalence of perinatal depression and its determinants in Mainland China: A systematic review and meta-analysis. J Affect Disord. 2020;277:1022-1037. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 176] [Article Influence: 35.2] [Reference Citation Analysis (0)] |
| 7. | Zhuang CY, Lin SY, Cheng CJ, Chen XJ, Shi HL, Sun H, Zhang HY, Fu MA. Home-based nursing for improvement of quality of life and depression in patients with postpartum depression. World J Clin Cases. 2020;8:4785-4792. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, Chisholm D, Collins PY, Cooper JL, Eaton J, Herrman H, Herzallah MM, Huang Y, Jordans MJD, Kleinman A, Medina-Mora ME, Morgan E, Niaz U, Omigbodun O, Prince M, Rahman A, Saraceno B, Sarkar BK, De Silva M, Singh I, Stein DJ, Sunkel C, UnÜtzer J. The Lancet Commission on global mental health and sustainable development. Lancet. 2018;392:1553-1598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1438] [Cited by in RCA: 1387] [Article Influence: 198.1] [Reference Citation Analysis (0)] |
| 9. | Wang Z, Liu J, Shuai H, Cai Z, Fu X, Liu Y, Xiao X, Zhang W, Krabbendam E, Liu S, Liu Z, Li Z, Yang BX. Mapping global prevalence of depression among postpartum women. Transl Psychiatry. 2021;11:543. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 283] [Article Influence: 70.8] [Reference Citation Analysis (0)] |
| 10. | Jeong YJ, Nho JH, Kim HY, Kim JY. Factors Influencing Quality of Life in Early Postpartum Women. Int J Environ Res Public Health. 2021;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 11. | Roberts K, Jaurequi ME, Kimmes JG, Selice L. Trait Mindfulness and Relationship Satisfaction: The Role of Forgiveness Among Couples. J Marital Fam Ther. 2021;47:196-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind in everyday life. London: Piatkus, 1996; . [DOI] [Full Text] |
| 13. | MacKenzie MB, Kocovski NL. Mindfulness-based cognitive therapy for depression: trends and developments. Psychol Res Behav Manag. 2016;9:125-132. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Hulsbosch LP, van de Poel E, Nyklíček I, Boekhorst MG. Trait mindfulness facets as a protective factor for the development of postpartum depressive symptoms. J Psychiatr Res. 2023;157:264-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 15. | Chow S, Shao J, Wang H. Sample Size Calculations in Clinical Research. 2nd Ed. New York: Chapman & Hall/CRC Biostatistics Series. 2008. |
| 16. | Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84:822-848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6591] [Cited by in RCA: 4976] [Article Influence: 226.2] [Reference Citation Analysis (0)] |
| 17. | Nooripour R, Ghanbari N, Hoseinian S, Vakili Y, Dobkins K. Psychometric Validation of the Farsi Version of the Mindful Attention Awareness Scale (MAAS) in a Sample of Iranian Students in the USA. Int J Ment Health Addiction. 2021;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 18. | Black DS, Sussman S, Johnson CA, Milam J. Psychometric assessment of the Mindful Attention Awareness Scale (MAAS) among Chinese adolescents. Assessment. 2012;19:42-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 108] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 19. | Chen SY, Cui H, Zhou RL, Jia YY. [Revision of Mindful Attention Awareness Scale (MAAS)]. Zhongguo Linchuang Xinlixue Zazhi. 2012;20:148-151. |
| 20. | Zung WW, Richards CB, Short MJ. Self-rating depression scale in an outpatient clinic. Further validation of the SDS. Arch Gen Psychiatry. 1965;13:508-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 748] [Cited by in RCA: 758] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 21. | Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12:371-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2251] [Cited by in RCA: 2723] [Article Influence: 50.4] [Reference Citation Analysis (0)] |
| 22. | Peng H, Zhang YY, Ji Y, Tang WQ, Li Q, Yan XL, Zhuang Q. [Analysis of reliability and validity of Chinese version SDS Scale in women of rural area]. Shanghai Yiyao. 2013;20-23. [DOI] [Full Text] |
| 23. | Feng Q, Zhang QL, Du Y, Ye YL, He QQ. Associations of physical activity, screen time with depression, anxiety and sleep quality among Chinese college freshmen. PLoS One. 2014;9:e100914. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 113] [Cited by in RCA: 168] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 24. | Xu J, Wei Y. Social support as a moderator of the relationship between anxiety and depression: an empirical study with adult survivors of Wenchuan earthquake. PLoS One. 2013;8:e79045. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 61] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 25. | Wang YZ, Wang ZJ, Jia LZ, Zhao JT, Li RF. [The Development of the Marriage Perception Scale (MPS)]. Zhongguo Jiankang Xinlixue Zazhi. 2009;17: 112-114. |
| 26. | Liu Y, Guo N, Li T, Zhuang W, Jiang H. Prevalence and Associated Factors of Postpartum Anxiety and Depression Symptoms Among Women in Shanghai, China. J Affect Disord. 2020;274:848-856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 27. | Chen Q, Li W, Xiong J, Zheng X. Prevalence and Risk Factors Associated with Postpartum Depression during the COVID-19 Pandemic: A Literature Review and Meta-Analysis. Int J Environ Res Public Health. 2022;19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 84] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 28. | Chen L, Ding L, Qi M, Jiang C, Mao XM, Cai WZ. Incidence of and social-demographic and obstetric factors associated with postpartum depression: differences among ethnic Han and Kazak women of Northwestern China. PeerJ. 2018;6:e4335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 29. | Dillard AJ, Meier BP. Trait mindfulness is negatively associated with distress related to COVID-19. Pers Individ Dif. 2021;179:110955. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 30. | Kappen G, Karremans JC, Burk WJ, Buyukcan-Tetik A. On the Association Between Mindfulness and Romantic Relationship Satisfaction: the Role of Partner Acceptance. Mindfulness (N Y). 2018;9:1543-1556. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 31. | Lagadec N, Steinecker M, Kapassi A, Magnier AM, Chastang J, Robert S, Gaouaou N, Ibanez G. Factors influencing the quality of life of pregnant women: a systematic review. BMC Pregnancy Childbirth. 2018;18:455. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 83] [Cited by in RCA: 179] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 32. | Whisman MA, Sbarra DA, Beach SRH. Intimate Relationships and Depression: Searching for Causation in the Sea of Association. Annu Rev Clin Psychol. 2021;17:233-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 45] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 33. | Tsang S, Avery AR, Duncan GE. Do married and/or cohabiting individuals fare better during the COVID-19 pandemic? Psychol Health Med. 2023;28:131-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 34. | Mamede A, Merkelbach I, Noordzij G, Denktas S. Mindfulness as a Protective Factor Against Depression, Anxiety and Psychological Distress During the COVID-19 Pandemic: Emotion Regulation and Insomnia Symptoms as Mediators. Front Psychol. 2022;13:820959. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 35. | Yekta FF, Yaghoubi H, Ghomian S, Gholami Fesharaki M. Mediators for Effect of Mindfulness in Promoting Marital Satisfaction: Modeling Structural Equations in an Experimental Study. Iran J Psychiatry. 2022;17:72-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 36. | Crego A, Yela JR, Gómez-Martínez MÁ, Riesco-Matías P, Petisco-Rodríguez C. Relationships between Mindfulness, Purpose in Life, Happiness, Anxiety, and Depression: Testing a Mediation Model in a Sample of Women. Int J Environ Res Public Health. 2021;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 37. | Xie J, Zhou D, Tan Y. Relationship between mindfulness and general health among couples in Mainland China: A crossover perspective. Soc Sci Med. 2021;281:114095. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 38. | Sun Y, Li Y, Wang J, Chen Q, Bazzano AN, Cao F. Effectiveness of Smartphone-Based Mindfulness Training on Maternal Perinatal Depression: Randomized Controlled Trial. J Med Internet Res. 2021;23:e23410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 80] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 39. | Vilaverde RF, Correia AI, Lima CF. Higher trait mindfulness is associated with empathy but not with emotion recognition abilities. R Soc Open Sci. 2020;7:192077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |