Published online Jan 6, 2023. doi: 10.12998/wjcc.v11.i1.84
Peer-review started: November 14, 2022
First decision: December 1, 2022
Revised: December 12, 2022
Accepted: December 23, 2022
Article in press: December 23, 2022
Published online: January 6, 2023
Processing time: 51 Days and 19 Hours
Diabetic wound takes longer time to heal due to micro and macro-vascular ailment. This longer healing time can lead to infections and other health complications. Foot ulcers are one of the most common diabetic wounds. These are one of the leading cause of amputations. Medical science is continuously striving for improving quality of human life. A recent trend of amalgamation of knowledge, efforts and technological advancement of medical science experts and artificial intelligence researchers, has made tremendous success in diagnosis, prognosis and treatment of a variety of diseases. Diabetic wounds are no exception, as artificial intelligence experts are putting their research efforts to apply latest technological advancements in the field to help medical care personnel to deal with diabetic wounds in more effective manner. The presented study reviews the diagnostic and treatment research under the umbrella of Artificial Intelligence and computational science, for diabetic wound healing. Framework for diabetic wound assessment using artificial intelligence is presented. Moreover, this review is focused on existing and potential contribution of artificial intelligence to improve medical services for diabetic wound patients. The article also discusses the future directions for the betterment of the field that can lead to facilitate both, clinician and patients.
Core Tip: This mini-review covers the contributions of Artificial Intelligence (AI) in the field of diabetic wound assessment, treatment and healing. It discusses the AI based framework for the diagnosis of Diabetic wounds. It also highlights the limitations and future endeavors of the said field in collaboration with technological advancements. This review can give the clinicians the idea of scientific innovations in their field and can facilitate the adoption of the technology as well. This also pathways for the collaborative research opportunities for clinicians and AI experts.
- Citation: Tehsin S, Kausar S, Jameel A. Diabetic wounds and artificial intelligence: A mini-review. World J Clin Cases 2023; 11(1): 84-91
- URL: https://www.wjgnet.com/2307-8960/full/v11/i1/84.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i1.84
Lessened wound healing is a crucial diabetic impediment coupled with enhanced illness. It is the result of micro and macrovascular ailment. Diabetic neuropathy results in loss of protective sensation (LOPS). LOPS triggers overdue recovery in diabetic foot sores[1,2]. Patients suffering with diabetes mellitus have a lifetime threat of 15% to 25% of diabetic foot ulcers (DFUs) occurrence. Diabetic wound healing is a time-consuming crucial health issue that is imposing a serious burden on health care system. Moreover, Diabetic wounds have a considerable affect on disability, diseased state, and mortality[3,4]. Diabetes is the foremost source of atraumatic lower limb amputations in the USA, and nearly 14%-24% of diabetic patients with limb ulcer results in amputation. Whereas 90% of the total amputations are caused by diabetic wounds[5].
Technology has evolved swiftly in last few decades casing astronomy to entertainment fields[6-8]. But, health sector gained special attention in this technological transformation. Technology in general, and Artificial Intelligence (AI) in particular have improved the health sector. Artificial intelligence has extensively improved the diagnostics and prognostic assessments[9-12]. Few highlights are skin lesions[13-15], pathological analysis[16,17], radiograph analysis[18,19], cancer stage assessments etc.[20-22].
This article analyzes potential role of AI in diabetic wound care, treatment, diagnosis and prognosis.
The medical field is very swiftly relying on the computer technologies. There are few major milestones of technology that helped medical science a lot. Hospital computing feasibility study was carried out by the Baylor University Medical Center between 1958-1959 and the term hospital information system is first used in this study. This feasibility study lead towards many healthcare information systems in 60’s and 70’s era. Lockheed Eclipsys, Health Evaluation through Logical Processing, and Regenstrief Medical Record System are few examples.
AI started its contribution in 1970’s by providing systems for biomedical problems[23-27]. Machine learning and knowledge based expert system were extensively used in the diagnosis, assessment, monitoring and treatment of different diseases[28-30]. Between 1970 and 2012, a lot of research is done on these two fields for medical science, particularly in diagnosis of diseases.
2012 is the start of era of deep learning that is acting as a revolution to AI and its applications. Machine Learning is a subset of AI and deep learning is a subset of machine learning. Machine learning learns patterns and general trends from the example data. It tries to mimic the results of example data to the query data. Machine learning is very much reliant on the domain knowledge, features sets and defined properties of the problem. Deep learning on the other hand is less dependent on the specification of domain knowledge and more dependent upon the amount of data provided. Deep learning is actually millions of artificial neurons connected together, hence capable of work like human brains. Although, in most of the problem domains it is not replacing the human experts, but surely is assisting.
Computer technology has been used vastly in the prevention, diagnosis and cure of diabetic wounds. AI techniques, computer vision and digital image analysis methodologies, machine learning and deep learning are key players in the recent technological advancement in healthcare. But the progression is strongly linked to the deep neural networks. These networks play a revolutionary part in medical field. Neural networks are based on the idea of mimicking the human neurons in the brain. Thousands of artificial neurons, connected in different patterns, are capable of achieving human-level task accomplishment. Although such networks require high computation machines and plenty of data to achieve good results.
The amount of digital medical data in 1950 doubled in fifty years. By 2010 the time to double the data reduced to three and half years. But in 2020, it requires only 73 d to double the medical data[31]. This rapid increase in medical data availability is facilitating AI experts to employ more sophisticated data hungry AI techniques for improving healthcare facilities[32].
Rest of the article discusses the role of AI in the diagnosis, prognosis and treatment of diabetic wounds.
Characteristically, there are three stages to a diabetic ulcer. The very first stage is callus-forming. Neuropathy is the cause of callus. The sensory neuropathy results in sensory loss, leads to continuing trauma, as a consequence motor neuropathy substantially deforms the foot. Another contributory characteristic is autonomic neuropathy, which causes dehydration of the skin. Ultimately, continual pressure to the callus produces subcutaneous bleeding, and gradually, it grows to an ulcer.
The medical assessment must consists of investigating the peripheral pulses of the feet, analyzing structural variances, the existence of callus, indications of vascular inadequacy, This may be indicative of hair loss, muscle atrophy, and position of the ulcer. Also evaluate the existence of purulence, shells, and indication of neuropathy by assessing with a monofilament[33].
Diabetic wound detection is laborious job and requires special skills and knowledge. However these expertise are not available in all regions of globe. Computer aided systems and tele-medicine can improve the health facilities in such remote areas.
For the diagnosis and assessment of diabetic wounds, AI based solutions are giving very encouraging results[34-38]. Early detection of such diabetic problems can lessen the treatment time. Moreover, it can also reduce the chances of imputation and morbidity. Lack of medical expertise and other resource constraints may lead to delayed diagnosis of diabetic ulcers. Computer Aided Diagnosis (CAD) are mostly using infrared thermography for the detection of ulcers in diabetic patients. It shows the temperature distribution of plantar foot. The connotation of thermographs and patient wound condition is quite complex. These patterns can be studied and analyzed using data mining, machine learning and deep learning mechanisms. It can reduce the clinician’s burden and assist in analysis of the thermograph. Moreover, the human analysis can be subjective based on the experience, knowledge, fatigue etc. We can achieve the objective diagnostics through mathematical modeling of the underlying patterns. CAD systems are very efficient and proven effective in detecting ulcer-prone regions.
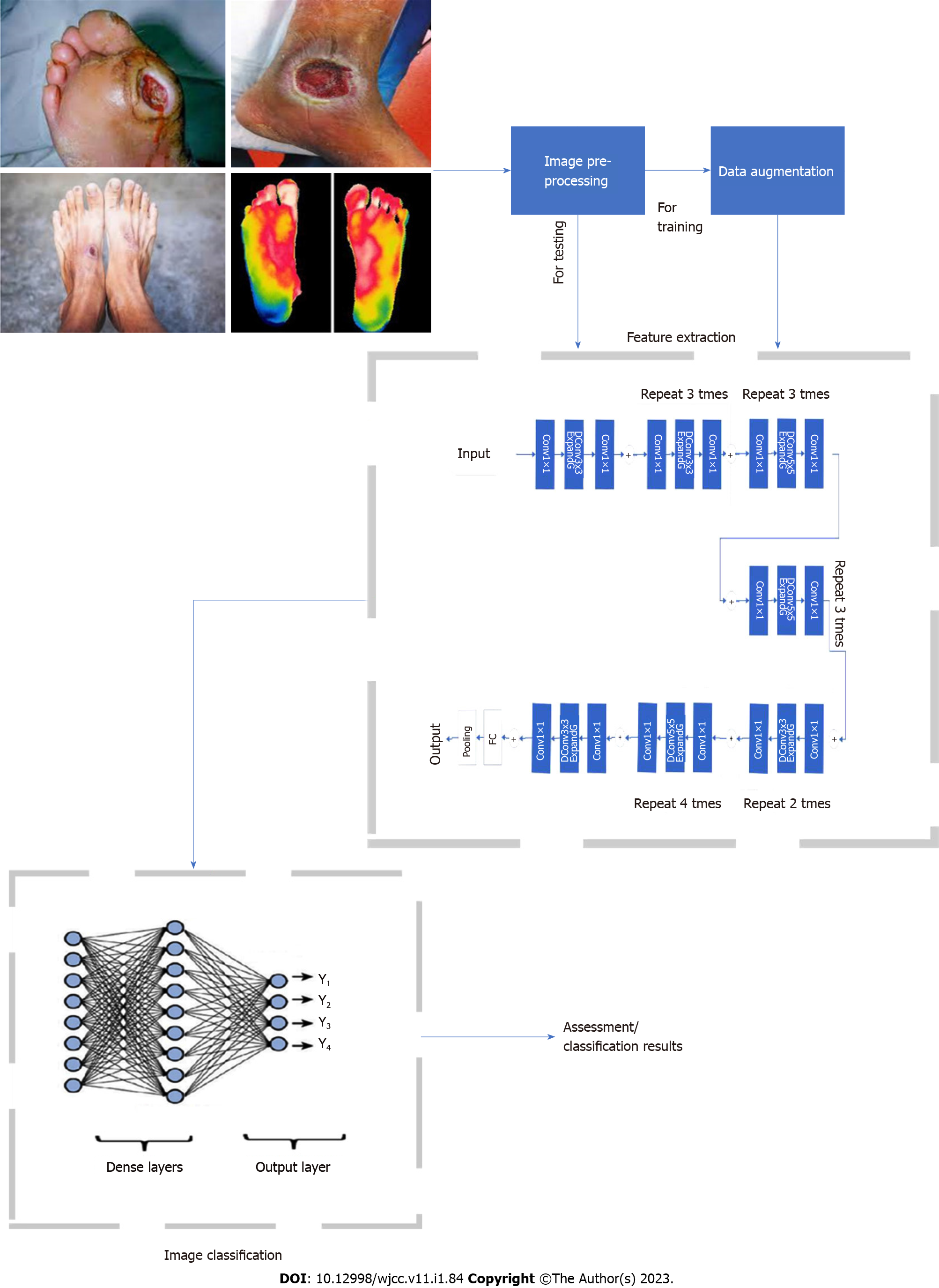
A general artificial intelligence based framework for diagnosis is shown in Figure 1.
One of the significant potential contributions of artificial intelligence for serving the diabetic wound patients can be predictive assessment of risks related to foot ulcer and other diabetic wounds. This can be accomplished by AI supported automated/semi-automated wound screening methods. AI can also be beneficial in preventive and protective monitoring of wounds to facilitate timely intervention. Risk assessment and risk analysis can also be supported by artificially intelligent methods. Deep learning can be utilized to analyze the correlation and probability of different known and unknown risk factors. This particular area needs more focused attention of AI researchers who needs to jointly work with medical experts. One very good initiative in this direction has been taken by NHS Scotland, who is currently working on risk stratification by employing machine learning techniques.
In one of the earlier studies, Singh et al[39] used an artificial neural network to analyze patients with type 2 diabetes mellitus (T2DM) in order to determine the risk for developing a DFU, in relation to five single nucleotide polymorphisms (SNPs) in the TLR4 gene (namely, Asp299Gly, Thr399Ile, rs11536858, rs1927911, and rs1927914). A total of 255 T2DM patients were enrolled in the study, including 130 patients without DFU and 125 patients who already had DFU. Five input nodes, ten hidden layer nodes, and one output node that represented the risk of DFU made up the final ANN architecture. With the five SNPs as inputs, the ANN model was able to accurately predict the presence or absence of DFU in 83% of the validation set (25%) of the dataset. According to the study's findings, some of the investigated SNPs' haplotypes may contribute to the development and progression of DFU, whereas other haplotypes appear to be protective against the disease.
Ferreira et al[40] uses an unsupervised learning methodology to classify the prognosis stage before visual signs. It works on the data collected by questionnaire asking questions about health conditions, foot care routine, numbness, loss of sensation, and tingling etc. The study involves 73 subjects and achieves sensitivity of 71%, specificity of 100%, and accuracy of 90%.
The research conducted in 2021 by Khandakar et al[41] was relatively similar to that conducted a year earlier by Cruz-Vega et al[42] because both investigations used thermograms to identify diabetic foot anomalies early on (and perhaps determine the risk of DFU). In Khandakar's study, machine learning algorithms were trained using data from 122 diabetic patients and 45 healthy controls, including each subject's gender, age, weight, height, and thermograms of a foot pair. The only goal of this study was to identify diabetes and control participants (i.e., two-class classifier). While deep CNN methods were used to process the entire images.
Arteaga-Marrero et al[43] employed U-net based deep learning approach for the segmentation of foot sole. It can be helpful for the thermographic technique for foot care protocols. Studies of Muralidhara et al[44] and Khandakar et al[41] performs two levels of multi-class classification. The categorizations includes five classes of diabetic thermograms and six classes of non-diabetic thermograms.
Artificial intelligence has diverse technologies that poses potential to be utilized for diabetic wound treatment as well. This area is still required to be explored by AI community. AI based technologies can be utilized to prescribe individualized treatment plan. As diabetic wounds comes in variety of condition, severity, covariates and correlated factors. This makes it challenging to plan accurate and individualized treatment. This particular dimension requires an active collaboration of AI and medical experts.
Another important factor that is addressed by computer scientist is, appropriate shoe making for diabetic patients. Diabetic foot ulcers are very sensitive to touch and sensations. Normal foot wears can not be used for such patients. It can worsen the condition and pain. Computer assisted shoe molds have been developed for such patients[45-47]. While doing daily routine activities, the diabetic foot undergoes from plantar weight spread. This can be injurious and can lead to serious consequences. The human foot design, shape and structure vary a lot. Customized shoe insoles are very much required in this scenario. Such insoles can be customized by AI based computer systems.
AI based computer systems are very helpful in the diagnosis and detection of diabetic wounds. But most of the work is tested on the limited data. There is a need of close collaboration between computer researchers and medical experts for deployment of such systems. Majority of the recent algorithms require a lot of data. Medical data is difficult to acquire due to legal and privacy issues. Moreover, annotation of the data is a big hassle. Annotating millions of instances of data is very laborious job. It requires time, resources and coordination of both the communities. Modern AI is moving towards the data-centric approaches. Clean and reliable data is the biggest requirement of the modern AI based systems.
Though AI experts have recently contributed to the domain of diabetic wounds. But as literature is evident that majority of the AI research is focused on detection and classification of diabetic foot wounds by employing computer vision technologies. Diagnosis is not the only dimension, in which AI community can contribute.
The standard and quality of life and of patients suffering with DFU might be greatly improved by prevention of amputation. DFU treatment is a large-scale problem of health care which results in a high mortality rate. Techniques for early prevention could help save a diabetic patient’s life and prevent disease. DFU analysis and recognition using image-based algorithms of machine learning is an emerging area of research. Amputation risk prediction and individualized study of the risk factors for amputation in patients with DFU could lead to early treatment methods, improve healing rates, lower the number of amputations, and lower treatment costs.
None of the DFU categorization systems has been acknowledged as the gold standard, despite the fact that they can all predict amputation. The majority of these systems rely more on clinical experience than on objective statistical techniques. These systems are insensitive and non-specific since they do not fully evaluate the impact of demographic data, clinical or laboratory data, medical history, foot problems, or other risk factors on the amputation rate.
There are other potential areas, which have potential to get exploited by AI techniques and currently few to none has been contributed in this direction. These potential areas are prognosis, risk factor analysis, risk stratification, prediction, intelligent intervention and medicine, intelligent treatment and monitoring devices.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Engineering, biomedical
Country/Territory of origin: Pakistan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Moldogazieva NT, Russia; Özlem Ş, Turkey S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Peppa M, Stavroulakis P, Raptis SA. Advanced glycoxidation products and impaired diabetic wound healing. Wound Repair Regen. 2009;17:461-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 145] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 2. | Sweitzer SM, Fann SA, Borg TK, Baynes JW, Yost MJ. What is the future of diabetic wound care? Diabetes Educ. 2006;32:197-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Armstrong DG, Swerdlow MA, Armstrong AA, Conte MS, Padula WV, Bus SA. Five year mortality and direct costs of care for people with diabetic foot complications are comparable to cancer. J Foot Ankle Res. 2020;13:16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 350] [Cited by in RCA: 500] [Article Influence: 100.0] [Reference Citation Analysis (2)] |
| 4. | Zhao X, Pei D, Yang Y, Xu K, Yu J, Zhang Y, Zhang Q, He G, Li A, Chen X. Green tea derivative driven smart hydrogels with desired functions for chronic diabetic wound treatment. Advanced Functional Materials. 2021;31:2009442. [DOI] [Full Text] |
| 5. | Alvarsson A, Sandgren B, Wendel C, Alvarsson M, Brismar K. A retrospective analysis of amputation rates in diabetic patients: can lower extremity amputations be further prevented? Cardiovasc Diabetol. 2012;11:18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 54] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 6. | Yan Q, Dong H, Su J, Han J, Song B, Wei Q, Shi Y. A review of 3D printing technology for medical applications. Engineering. 2018;4:729-742. [DOI] [Full Text] |
| 7. | Hu HZ, Feng XB, Shao ZW, Xie M, Xu S, Wu XH, Ye ZW. Application and Prospect of Mixed Reality Technology in Medical Field. Curr Med Sci. 2019;39:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 70] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 8. | Park SH, Han K. Methodologic Guide for Evaluating Clinical Performance and Effect of Artificial Intelligence Technology for Medical Diagnosis and Prediction. Radiology. 2018;286:800-809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 467] [Cited by in RCA: 498] [Article Influence: 71.1] [Reference Citation Analysis (0)] |
| 9. | Chen JH, Asch SM. Machine Learning and Prediction in Medicine - Beyond the Peak of Inflated Expectations. N Engl J Med. 2017;376:2507-2509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 547] [Cited by in RCA: 602] [Article Influence: 75.3] [Reference Citation Analysis (4)] |
| 10. | Cabitza F, Rasoini R, Gensini GF. Unintended Consequences of Machine Learning in Medicine. JAMA. 2017;318:517-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 455] [Cited by in RCA: 499] [Article Influence: 62.4] [Reference Citation Analysis (0)] |
| 11. | Lee JG, Jun S, Cho YW, Lee H, Kim GB, Seo JB, Kim N. Deep Learning in Medical Imaging: General Overview. Korean J Radiol. 2017;18:570-584. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 555] [Cited by in RCA: 597] [Article Influence: 74.6] [Reference Citation Analysis (2)] |
| 12. | Kohli M, Prevedello LM, Filice RW, Geis JR. Implementing Machine Learning in Radiology Practice and Research. AJR Am J Roentgenol. 2017;208:754-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 191] [Article Influence: 23.9] [Reference Citation Analysis (0)] |
| 13. | Esteva A, Kuprel B, Novoa RA, Ko J, Swetter SM, Blau HM, Thrun S. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017;542:115-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5683] [Cited by in RCA: 5361] [Article Influence: 670.1] [Reference Citation Analysis (0)] |
| 14. | Bibi M, Hamid A, Tehseen S. Automated Skin Lesion Detection towards Melanoma. EAI Endorsed Transactions on Scalable Information Systems. 2019;6. [DOI] [Full Text] |
| 15. | Sengupta S, Mittal N, Modi M. Improved skin lesions detection using color space and artificial intelligence techniques. J Dermatolog Treat. 2020;31:511-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Tehsin S, Zameer S, Saif S. Myeloma cell detection in bone marrow aspiration using microscopic images. In 2019 11th International Conference on Knowledge and Smart Technology (KST). IEEE. 2019;57-61. [DOI] [Full Text] |
| 17. | Försch S, Klauschen F, Hufnagl P, Roth W. Artificial Intelligence in Pathology. Dtsch Arztebl Int. 2021;118:194-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 18. | Zhang R, Tie X, Qi Z, Bevins NB, Zhang C, Griner D, Song TK, Nadig JD, Schiebler ML, Garrett JW, Li K, Reeder SB, Chen GH. Diagnosis of Coronavirus Disease 2019 Pneumonia by Using Chest Radiography: Value of Artificial Intelligence. Radiology. 2021;298:E88-E97. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 92] [Cited by in RCA: 73] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 19. | Hardy M, Harvey H. Artificial intelligence in diagnostic imaging: impact on the radiography profession. Br J Radiol. 2020;93:20190840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 107] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 20. | Reichling C, Taieb J, Derangere V, Klopfenstein Q, Le Malicot K, Gornet JM, Becheur H, Fein F, Cojocarasu O, Kaminsky MC, Lagasse JP, Luet D, Nguyen S, Etienne PL, Gasmi M, Vanoli A, Perrier H, Puig PL, Emile JF, Lepage C, Ghiringhelli F. Artificial intelligence-guided tissue analysis combined with immune infiltrate assessment predicts stage III colon cancer outcomes in PETACC08 study. Gut. 2020;69:681-690. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 84] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 21. | Liu X, Zhou H, Hu Z, Jin Q, Wang J, Ye B. [Clinical Application of Artificial Intelligence Recognition Technology in the Diagnosis of Stage T1 Lung Cancer]. Zhongguo Fei Ai Za Zhi. 2019;22:319-323. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 22. | Hasserjian RP. Acute myeloid leukemia: advances in diagnosis and classification. Int J Lab Hematol. 2013;35:358-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 23. | Ohura N, Mitsuno R, Sakisaka M, Terabe Y, Morishige Y, Uchiyama A, Okoshi T, Shinji I, Takushima A. Convolutional neural networks for wound detection: the role of artificial intelligence in wound care. J Wound Care. 2019;28:S13-S24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 24. | Szolovits P, Pauker SG. Categorical and probabilistic reasoning in medical diagnosis. Artificial Intelligence. 1978;11:115-144. [RCA] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 131] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Blum RL, Wiederhold G. Inferring knowledge from clinical data banks utilizing techniques from artificial intelligence. In The Second Annual Symposium on Computer Application in Medical Care, 1978. Proceedings. IEEE. 1978;303-307. [DOI] [Full Text] |
| 26. | Shortliffe EH, Axline SG, Buchanan BG, Merigan TC, Cohen SN. An artificial intelligence program to advise physicians regarding antimicrobial therapy. Comput Biomed Res. 1973;6:544-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 80] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 27. | Chandrasekaran B, Gomez F, Mittal S, Smith J. An approach to medical diagnosis based on conceptual structures. In Proceedings of the 6th international joint conference on Artificial intelligence-Volume 1 1979; 134-142. [DOI] [Full Text] |
| 28. | Ramesh AN, Kambhampati C, Monson JR, Drew PJ. Artificial intelligence in medicine. Ann R Coll Surg Engl. 2004;86:334-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 310] [Cited by in RCA: 390] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 29. | Hudson DL, Cohen ME, Deedwania PC. A hybrid system for diagnosis and treatment of heart disease. In Proceedings of 16th Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE. 1994;2:1368-1369). [DOI] [Full Text] |
| 30. | Mitelpunkt A, Galili T, Kozlovski T, Bregman N, Shachar N, Markus-Kalish M, Benjamini Y. Novel Alzheimer's disease subtypes identified using a data and knowledge driven strategy. Sci Rep. 2020;10:1327. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 31. | Pawlak Z. Rough set approach to knowledge-based decision support. EJOR. 1997;99: 48-57. [DOI] [Full Text] |
| 32. | Densen P. Challenges and opportunities facing medical education. Trans Am Clin Climatol Assoc. 2011;122:48-58. [PubMed] |
| 33. | Cervantes-García E, Salazar-Schettino PM. Clinical and surgical characteristics of infected diabetic foot ulcers in a tertiary hospital of Mexico. Diabet Foot Ankle. 2017;8:1367210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 34. | Chan KS, Lo ZJ. Wound assessment, imaging and monitoring systems in diabetic foot ulcers: A systematic review. Int Wound J. 2020;17:1909-1923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 35. | Adam M, Ng EYK, Tan JH, Heng ML, Tong JWK, Acharya UR. Computer aided diagnosis of diabetic foot using infrared thermography: A review. Comput Biol Med. 2017;91:326-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 36. | Saminathan J, Sasikala M, Narayanamurthy VB, Rajesh K, Arvind RJIP. Computer aided detection of diabetic foot ulcer using asymmetry analysis of texture and temperature features. Infrared Physics & Technology. 2020;105:103219. [DOI] [Full Text] |
| 37. | Faust O, Rajendra Acharya U, Ng EYK, Hong TJ, Yu W. Application of infrared thermography in computer aided diagnosis. Infrared Phys Technol. 2014;66:160-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 46] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 38. | Goyal M, Reeves ND, Rajbhandari S, Ahmad N, Wang C, Yap MH. Recognition of ischaemia and infection in diabetic foot ulcers: Dataset and techniques. Comput Biol Med. 2020;117:103616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 104] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 39. | Singh K, Singh VK, Agrawal NK, Gupta SK, Singh K. Association of Toll-like receptor 4 polymorphisms with diabetic foot ulcers and application of artificial neural network in DFU risk assessment in type 2 diabetes patients. Biomed Res Int. 2013;2013:318686. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 52] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 40. | Ferreira ACBH, Ferreira DD, Oliveira HC, Resende IC, Anjos A, Lopes MHBM. Competitive neural layer-based method to identify people with high risk for diabetic foot. Comput Biol Med. 2020;120:103744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 41. | Khandakar A, Chowdhury MEH, Reaz MBI, Ali SHM, Kiranyaz S, Rahman T, Chowdhury MH, Ayari MA, Alfkey R, Bakar AAA, Malik RA, Hasan A. A Novel Machine Learning Approach for Severity Classification of Diabetic Foot Complications Using Thermogram Images. Sensors (Basel). 2022;22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 42. | Cruz-Vega I, Hernandez-Contreras D, Peregrina-Barreto H, Rangel-Magdaleno JJ, Ramirez-Cortes JM. Deep Learning Classification for Diabetic Foot Thermograms. Sensors (Basel). 2020;20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 54] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 43. | Arteaga-Marrero N, Hernández A, Villa E, González-Pérez S, Luque C, Ruiz-Alzola J. Segmentation Approaches for Diabetic Foot Disorders. Sensors (Basel). 2021;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 44. | Muralidhara S, Lucieri A, Dengel A, Ahmed S. Holistic multi-class classification & grading of diabetic foot ulcerations from plantar thermal images using deep learning. Health Inf Sci Syst. 2022;10:21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 45. | Davia M, Germani M, Mandolini M, Mengoni M, Montiel E, Raffaeli R. Shoes Customization Design Tools for the "Diabetic Foot". CAD&A. 2011;8:693-711. [DOI] [Full Text] |
| 46. | Zequera M, Stephan S, Paul J. Effectiveness of moulded insoles in reducing plantar pressure in diabetic patients. Annu Int Conf IEEE Eng Med Biol Soc. 2007;2007:4671-4674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 47. | Bernabéu JA, Germani M, Mandolini M, Mengoni M, Nester C, Preece S, Raffaeli R. CAD tools for designing shoe lasts for people with diabetes. Computer-Aided Design. 2013;45:977-990. [DOI] [Full Text] |