Published online Jan 6, 2023. doi: 10.12998/wjcc.v11.i1.57
Peer-review started: September 16, 2022
First decision: November 14, 2022
Revised: November 15, 2022
Accepted: December 15, 2022
Article in press: December 15, 2022
Published online: January 6, 2023
Processing time: 110 Days and 20.4 Hours
This article reviews the research progress of rehabilitation treatment and nursing care of patients with neurogenic bladder after spinal cord injury, in order to provide reference for the rehabilitation treatment and nursing care of patients. We reviewed recent medical literature on patients with neurogenic bladder, focusing on neurogenic bladder caused by spinal cord injury. We analyzed 30 recent of publications in patients with neurogenic bladder after spinal cord injury, in addition to reviewing and evaluating the commonly used rehabilitation nursing methods for neurogenic bladder. Psychological counseling is a vital aspect which cannot be neglected in the process of neurogenic bladder rehabilitation. Hitherto, the commonly used drug and surgical treatments may have negatively impacted the mental health of patients in varying degrees. However, in clinical practice, applying intermittent catheterization in patients who have neurogenic bladder with spinal cord injury may help improve patients’ life quality, mitigate psychological burden, and reduce negative emotions.
Core Tip: Existing treatments for neurogenic bladder mainly include surgery and drugs, but they all damage the patient's mental health to varying degrees. Intermittent catheterization not only helps to maintain bladder compliance, protect kidney function, and speed up recovery, but also helps to improve the patient's ability to live and reduce psychological burden and negative emotions.
- Citation: Xiang L, Li H, Xie QQ, Siau CS, Xie Z, Zhu MT, Zhou B, Li ZP, Wang SB. Rehabilitation care of patients with neurogenic bladder after spinal cord injury: A literature review. World J Clin Cases 2023; 11(1): 57-64
- URL: https://www.wjgnet.com/2307-8960/full/v11/i1/57.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i1.57
Spinal cord injury (SCI) is transverse damage to the spinal cord caused by various pathogenic factors, leading to paralysis of the limbs and trunk below the innervation level, combined with bladder and rectal dysfunction[1]. The global SCI incidence rate is 3.6/1 million to 195.4/1 million. The annual SCI incidence rate in the United States is about 40/1 million, and in Europe, it is 13.9-19.4/1 million[2,3]. A systematic review reported that the incidence of SCI in China ranged between 14.6% to 60.6%[4]and this indicated that the incidence of SCI in China is higher than that in developed countries and regions.
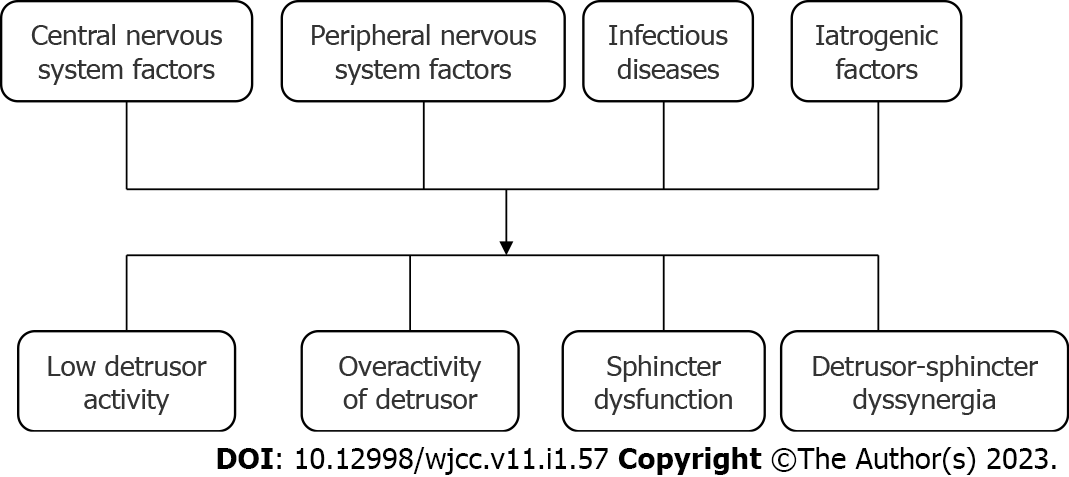
The results of the American standard SCI system study showed that 81% of SCI patients had diverse degrees of bladder dysfunction within one year after the onset of the disease[5]. There are also differences in incidence. Renal failure caused by urinary system dysfunction is one of the main causes of death in SCI patients[6]. Neurogenic bladder (NB) refers to the dysfunction of bladder storage and emptying of urine due to damage or disease of the central or peripheral nervous system that controls the voiding function (Figure 1), and patients may develop urinary tract infection or hydronephrosis which is one of the main complications of SCI patients. The high incidence of NB, the serious condition of the patients, and the ineffective rehabilitation treatment are important risk factors for the death of patients with spinal cord injury; NB patients often suffer from urinary dysfunction, which seriously affects their life quality. Reconstruction of bladder function is the key to restoring the urination function in SCI patients. It is of great significance to do rehabilitation training and nursing care of bladder function to help patients restore the bladder function as soon as possible, reduce the occurrence of complications, and cut down the mortality rate.
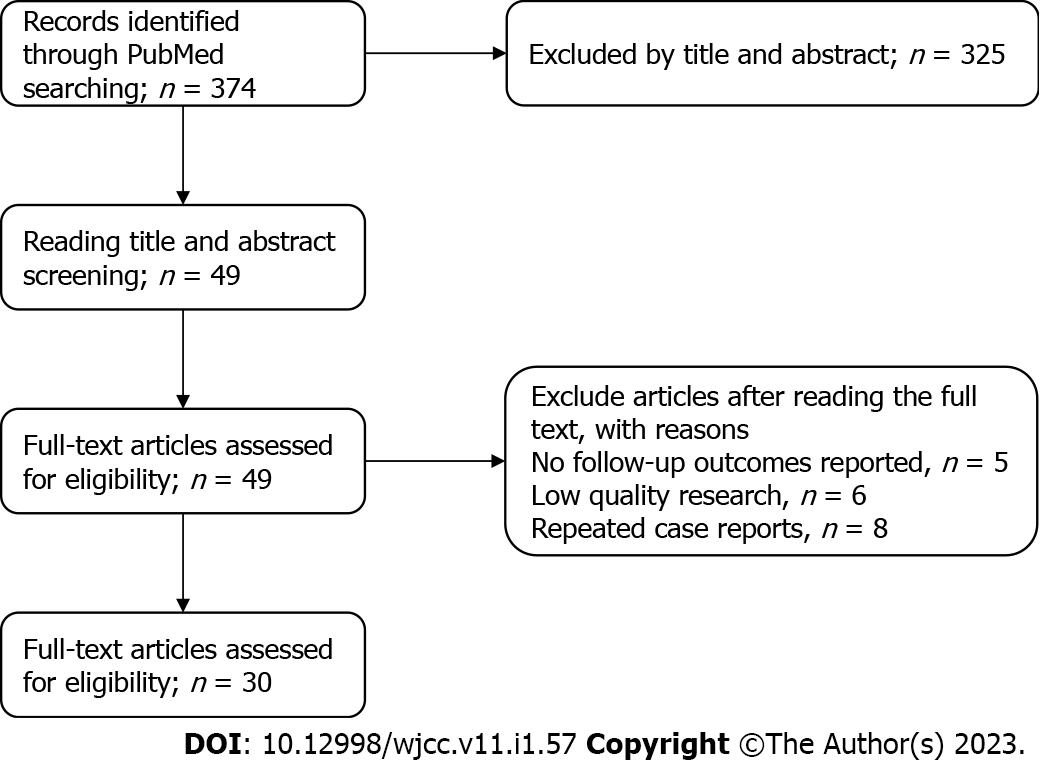
We reviewed the recent medical literature on patients with neurogenic bladder, focusing on neurogenic bladder caused by spinal cord injury. The articles published by PubMed from July 2007 to July 2022 were searched. The following medical subject titles or free-text terms are used in the search: Neurogenic bladder, anxiety, psychological burden, spinal cord injury, nursing. Search is limited to papers written in English, and there is no restriction on the types of articles. The literature retrieval strategy is shown in Figure 2.
The intravesical pressure of patients with neurogenic bladder should not exceed 40 cmH2O during storage and voiding. When the bladder pressure is equal to or higher than 40 cm H2O[7], clinical intervention is required to prevent potential complications such as renal injury or progression to renal failure. The main nursing principles of neurogenic bladder include: Reducing or avoiding complications such as urinary tract infection and stone formation; restoring normal bladder capacity, increasing bladder compliance, and enabling proper bladder emptying; restoring low-pressure urine storage function and protecting the upper urinary tract; mitigating urinary incontinence and enabling the bladder to have proper urinary continence; trying not to use indwelling catheters[8-10].
Manual-assisted urination mainly includes trigger point method, Valsalva breath-holding method, Greed maneuver, pelvic floor muscle training, and urethral sphincter coordination training. The above methods can be used in the pinch period and intermittent catheterization period of patients with indwelling catheterization, which can help the patient to establish autonomic reflexes in the bladder and induce spontaneous urination. The guidelines of Bragge et al[11] states that the use of reflex therapy and manual voiding in patients with neurogenic bladder has been criticized.
The main purposes of drug treatment are to reduce bladder storage pressure, prevent overactivity of the detrusor muscle, and prevent and treat urinary tract infections. Drug therapy can also be used to improve urine flow, reduce postoperative void residual volume[12] to counteract vesicoureteral reflux, or reduce spasticity. At present, the commonly used drugs for the treatment of neurogenic bladder include cholinergic receptor agonists, anticholinergic agents, α-adrenergic receptor blockers, and skeletal muscle relaxants. Before drug treatment, urodynamic examination should be performed on the patient to determine the type of bladder disorder, and then an appropriate drug would be selected according to the test results. The adverse reactions of drug therapy will increase with the increase of drug dose, and about 25% of urinary tract patients with benign prostatic obstruction stop taking drugs due to intolerance[13].
Currently, electrical nerve stimulation is a research hotspot in the treatment of neurogenic bladder patients[14]. Electric stimulation has the characteristics of low voltage, low frequency and no electrolysis, and can effectively stimulate the patient's sensory and motor nerves. Nerve electrical stimulation mainly simulates the nerve electrophysiological activities under different functional states by designing different parameters, so that the patient's muscles regularly contract to promote the recovery of the lesion. The methods of electrical nerve stimulation for the treatment of patients with neurogenic bladder mainly include transcutaneous electrical stimulation, electrical stimulation of the pelvic floor muscles, electrical stimulation of the pudendal nerve, etc. Magnetic therapy uses a certain intensity of time-varying electromagnetic field to stimulate the body tissue to generate induced current, thereby improving muscle rhythmic contraction by improving the nerve activity and muscle innervation.
Surgical treatment is an available option after evaluation for those patients who have neurogenic bladder after spinal cord injury and have undergone conservative treatment that was deemed ineffective[15]. The surgical method should be selected according to the site of neurogenic bladder injury, including bladder reconstruction and delayed bladder detrusor function reconstruction, technique, bladder denervation, and reinnervation.
The acute stage of spinal cord injury patients is the stage of spinal cord shock[16]. The bladder loses spinal cord innervation, resulting in complete paralysis of the detrusor muscle of the bladder, loss of contraction and relaxation functions, and reduced tension of the urethral sphincter. Only part of the contractile function is retained, which leads to urethral resistance greater than the pressure in the bladder, and urine is difficult to be discharged. Therefore, in the stage of spinal shock, the prevention and treatment of urinary retention in patients with neurogenic bladder and the promotion of bladder reflex contraction ability are the key points of nursing; at this time, due to the unstable bladder function of patients, the main nursing measures are indwelling urinary catheters, continuous drainage of urine, prevention of overfilled bladder, and reducing urinary tract infections. However, long-term indwelling catheters can easily lead to complications such as urinary tract infection and urethral injury, and it is rarely used in clinical practice.
Urodynamic testing is a common examination method in urology[17,18]. It mainly tests the pressure, flow rate, and bioelectrical activity of each part of the urinary tract to establish whether there are diseases associated with dysuria. Studies[19,20] have shown that patients with previous symptoms of lower urinary tract may not be accurately diagnosed with lower urinary tract dysfunction based only on clinical symptoms. Single or combined application of symptom score, urine flow measurement, residual urine measurement, bladder measurement, and bladder wall thickness has been widely used in clinic examination to preliminarily diagnose lower urinary tract dysfunction. However, although lower urinary tract dysfunction can be classified according to these research results and given initial treatment, there are still some lower urinary tract dysfunctions with extreme diagnostic criteria that may be missed or wrongly treated.
There may be some difficulties in the urodynamic examination of neurogenic bladder patients[21]. For example, many neurogenic bladder patients lack symptoms due to impaired bladder sensation, or it may be difficult for patients to determine the time of urinary incontinence. Patients with a neurogenic bladder may not be able to distinguish whether urine leakage is caused by urgency or pressure, such as urine leakage when entering or leaving a wheelchair. The severity of clinical symptoms in patients with complete neurological function is not completely consistent with urodynamic results, which is also true in patients with neurogenic bladder. Importantly, the severity of symptoms is not always related to the severity of urethral diseases. Some scholars[22-24] have reported that the correlation between neurological signs and symptoms and urodynamic evaluation results is poor in children with spinal cord dysplasia. In addition, although patients with spinal cord injury may have bladder dysfunction, the functional state of bladder and sphincter cannot be inferred based only on the results of neurological assessment. Urodynamics is very important to evaluate neurogenic bladder patients with high accuracy, because it is the only reliable index to judge upper urinary tract dysfunction and the best way to guide the treatment of the lower urinary tract.
Intermittent catheterization[25] refers to the method of inserting the catheter into the bladder when the patient's bladder is full, and removing the catheter immediately after emptying the urine, without leaving the catheter in the bladder. In fact, the residual urine volume decreases and the maximum voiding volume increases after intermittent catheterization indicating that the use of intermittent catheterization is helpful to promote the recovery of bladder voiding function and increase the urine output. At the same time, according to the specific condition of the patient during catheterization, formulating a strict drinking water plan and reasonably controlling the amount of drinking water and urine of patients will help to ensure the balance of bladder energy storage and better restore the bladder function.
Early intermittent catheterization is a prominent way of bladder training, allowing the bladder to empty intermittently, which is conducive to maintaining bladder capacity and restoring bladder contraction function. It is the "gold standard" for assisting bladder emptying training. Intermittent catheterization is recommended by the International Continence Society as the preferred method for the treatment of neurogenic bladder, including sterile intermittent catheterization and clean intermittent catheterization. Among them, clean intermittent catheterization is the most ideal approach to train the bladder function. Some scholars have suggested that repeated catheterization may increase the chance of urinary tract infection, but considerable studies have shown that intermittent catheterization does not increase the chance of urinary tract infection. Using intermittent catheterization to train the bladder function in patients with spinal cord injury can effectively reduce residual urine volume, cut down the rate of urinary system infection, and better control the disease. Orem self-care mode can not only improve the bladder function of patients, but is easily accepted by patients[26]. It does not increase the rate of urinary tract infection, and can play a positive role in the rehabilitation of intermittent catheterization patients.
Spinal cord injury can lead to abnormal motor and sensory function, urinary incontinence, and patients are prone to developing psychological disorders[27,28]. Through psychological counseling, it is particularly essential to deal with various psychological issues of patients in a targeted manner, in order to improve the compliance of patients with rehabilitation training. The rehabilitation process of neurogenic bladder after spinal cord injury is long, and many patients have difficulty receiving permanent rehabilitation training, contributing to low adherence and even treatment refusal; for such patients, the nursing staff should provide compassionate care and to cultivate the patients’ coping skills. In addition to accompanying the patient, the family members of the patient also need to continue living their daily life. They are under great psychological pressure. It is necessary to provide psychological care and health education to the family members of the patients, so that they can fully understand the relevant knowledge of the disease and establish a collaborative relationship through effective communication. Furthermore, guiding the family members of the patients to learn how to train patients' bladder function is also indispensable, so as to allow them to assume the responsibility of supervising and encouraging patients to adhere to rehabilitation training.
Neurogenic bladder is a common sequelae of spinal cord injury. Long-term urinary retention and incontinence in patients can result in complications such as urinary tract infection, kidney stones, ureteral stones, and hydronephrosis, which will develop into renal failure and endanger the patients’ life[29]. A large number of cohort studies have shown that 40% of patients with spinal cord injury neurogenic bladder require repeated outpatient urology visits, 33% require repeated admissions and discharges, and 15% require perennial home care. The above results can fully illustrate that neurogenic bladder after spinal cord injury will seriously affect the quality of patients’ life[30]. Therefore, the continuous optimization of rehabilitation nursing and other treatment measures for patients with spinal cord injury neurogenic bladder can improve the quality of life of patients and reduce the long-term mortality, which has important clinical and social significance.
The pathogenesis of neurogenic bladder after spinal cord injury is complex, and the clinical manifestations of patients are diverse. Although rehabilitation treatment is a complex and long process, reconstruction of bladder function and improvement of urinary incontinence are vital means to prolong the life expectancy and improve the quality of life of patients with spinal cord injury. Psychological counseling is also essential. The ability of the patient to instructions from medical staff, reciprocal communication, and counseling are strategies which could mitigate the psychological distress of patients and enable patients to better cooperate with rehabilitation treatment and nursing. This in turn will promote patient recovery and alleviate their pain. Bladder function training can improve the synergy of the detrusor and urethral sphincter, gradually form voiding reflex, and boost the bladder function. Intermittent catheterization can prevent bladder wall damage caused by overfilling of the bladder, bladder spasm from causing the volume reduction, help restore the bladder to store and discharge urine regularly, assist in maintaining bladder compliance, protect the kidney function, and accelerate recovery. The bladder plays a crucial role in spontaneous urination. In the process of rehabilitation nursing, it is necessary to observe the dynamic changes of a patient's urination in a timely manner, and take personalized nursing measures according to the changes of the patient in different stages of recovery. Initial comprehensive rehabilitation nursing can promote the early recovery of bladder function in patients with spinal cord injury neurogenic bladder, enhance and utilize bladder storage and urination functions, shorten the time of indwelling catheter, reduce the occurrence of residual urine volume, reduce urinary tract infection rate, thus ameliorate patient outcomes.
Although we have made efforts to search the existing literature on neurogenic bladder care, our research still has some limitations, including the retrospective nature of the studies reviewed and inherent limitations related to observational studies. Limited by our search strategies, our search results may not be comprehensive enough, so it may bring some bias to the conclusions. The incidence and nursing methods of neurogenic bladder may be geographically different and may vary according to the knowledge of local medical practitioners. These factors have not been analyzed in detail due to the lack of relevant supporting data. However, even though the number of studies reviewed was small, the clinical significance of the research results is still relevant.
This review reviews the research on neurogenic bladder care that can be retrieved in PubMed during the last fifteen years. Many complications caused by a neurogenic bladder, such as urinary tract infection, kidney calculi, ureteral stones, and hydronephrosis, not only bring trauma to the patient's body, but also seriously affect the diagnosis and treatment of these complications. Repeated hospital admissions and long-term home care could increase the psychological distress of the patients. Therefore, in the diagnosis, treatment, and care of neurogenic bladder, psychological care is also an essential component. It has been found in clinical practice that intermittent catheterization can assist in maintaining bladder compliance, protecting renal function, and accelerating recovery. At the same time, it helps to improve the patients' life quality and reduce psychological distress. Our review provides noteworthy information for the future care of patients with neurogenic bladder. Psychological care of patients with neurogenic bladder is also important during the process of the patients' rehabilitation. Intermittent urethral catheterization is superior to other forms of traditional urethral catheterization.
We thank the reviewers for their comments that helped to improve the manuscript.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Malaysia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Boopathy Vijayaraghavan KM, India; Cassell III AK, Liberia; Khosravi M, Iran S-Editor: Liu GL L-Editor: A P-Editor: Liu GL
| 1. | Jiang Y, Fu P, Liu Y, Wang C, Zhao P, Chu X, Jiang X, Yang W, Wu Y, Wang Y, Xu G, Hu J, Bu W. Near-infrared light-triggered NO release for spinal cord injury repair. Sci Adv. 2020;6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 73] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 2. | Huang H, Young W, Skaper S, Chen L, Moviglia G, Saberi H, Al-Zoubi Z, Sharma HS, Muresanu D, Sharma A, El Masry W, Feng S; International Association of Neurorestoratology and The Chinese Association of Neurorestoratology. Clinical Neurorestorative Therapeutic Guidelines for Spinal Cord Injury (IANR/CANR version 2019). J Orthop Translat. 2020;20:14-24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 95] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 3. | Jazayeri SB, Beygi S, Shokraneh F, Hagen EM, Rahimi-Movaghar V. Incidence of traumatic spinal cord injury worldwide: a systematic review. Eur Spine J. 2015;24:905-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 215] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 4. | Chen C, Qiao X, Liu W, Fekete C, Reinhardt JD. Epidemiology of spinal cord injury in China: A systematic review of the chinese and english literature. Spinal Cord. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 29] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 5. | Adriaansen JJ, van Asbeck FW, Tepper M, Faber WX, Visser-Meily JM, de Kort LM, Post MW. Bladder-emptying methods, neurogenic lower urinary tract dysfunction and impact on quality of life in people with long-term spinal cord injury. J Spinal Cord Med. 2017;40:43-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 52] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 6. | Chamberlain JD, Buzzell A, Gmünder HP, Hug K, Jordan X, Moser A, Schubert M, Zwahlen M, Brinkhof MWG; the SwiSCI Study Group and the Swiss National Cohort. Comparison of All-Cause and Cause-Specific Mortality of Persons with Traumatic Spinal Cord Injuries to the General Swiss Population: Results from a National Cohort Study. Neuroepidemiology. 2019;52:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 7. | Kroll P. Pharmacotherapy for Pediatric Neurogenic Bladder. Paediatr Drugs. 2017;19:463-478. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Le HK, Cardona-Grau D, Chiang G. Evaluation and Long-term Management of Neurogenic Bladder in Spinal Dysraphism. Neoreviews. 2019;20:e711-e724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Kuris EO, Alsoof D, Osorio C, Daniels AH. Bowel and Bladder Care in Patients With Spinal Cord Injury. J Am Acad Orthop Surg. 2022;30:263-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Paturel P, Bardet F, Cormier L, Mourey E. [Neurogenic bladder and continent cystostomy: Results of a monocentric cohort in a French university hospital]. Prog Urol. 2022;32:23-31. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 11. | Bragge P, Guy S, Boulet M, Ghafoori E, Goodwin D, Wright B. A systematic review of the content and quality of clinical practice guidelines for management of the neurogenic bladder following spinal cord injury. Spinal Cord. 2019;57:540-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 12. | Hashim H, Worthington J, Abrams P, Young G, Taylor H, Noble SM, Brookes ST, Cotterill N, Page T, Swami KS, Lane JA; UNBLOCS Trial Group. Thulium laser transurethral vaporesection of the prostate versus transurethral resection of the prostate for men with lower urinary tract symptoms or urinary retention (UNBLOCS): a randomised controlled trial. Lancet. 2020;396:50-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 13. | Sakalis V, Gkotsi A, Charpidou D, Tsafrakidis P, Apostolidis A. The effect of pharmacotherapy on prostate volume, prostate perfusion and prostate-specific antigen (prostate morphometric parameters) in patients with lower urinary tract symptoms and benign prostatic obstruction. A systematic review and meta-analysis. Cent European J Urol. 2021;74:388-421. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 14. | Zomkowski K, Kammers I, Back BBH, Moreira GM, Sonza A, Sacomori C, Sperandio FF. The effectiveness of different electrical nerve stimulation protocols for treating adults with non-neurogenic overactive bladder: a systematic review and meta-analysis. Int Urogynecol J. 2022;33:1045-1058. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 15. | DeWitt-Foy ME, Elliott SP. Neurogenic Bladder:: Assessment and Operative Management. Urol Clin North Am. 2022;49:519-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 16. | Joshi AD, Shukla A, Chawathe V, Gaur AK. Clean intermittent catheterization in long-term management of neurogenic bladder in spinal cord injury: Patient perspective and experiences. Int J Urol. 2022;29:317-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 22] [Article Influence: 7.3] [Reference Citation Analysis (1)] |
| 17. | Nager CW, Brubaker L, Litman HJ, Zyczynski HM, Varner RE, Amundsen C, Sirls LT, Norton PA, Arisco AM, Chai TC, Zimmern P, Barber MD, Dandreo KJ, Menefee SA, Kenton K, Lowder J, Richter HE, Khandwala S, Nygaard I, Kraus SR, Johnson HW, Lemack GE, Mihova M, Albo ME, Mueller E, Sutkin G, Wilson TS, Hsu Y, Rozanski TA, Rickey LM, Rahn D, Tennstedt S, Kusek JW, Gormley EA; Urinary Incontinence Treatment Network. A randomized trial of urodynamic testing before stress-incontinence surgery. N Engl J Med. 2012;366:1987-1997. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 328] [Cited by in RCA: 319] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 18. | Bodmer NS, Wirth C, Birkhäuser V, Sartori AM, Leitner L, Averbeck MA, de Wachter S, Finazzi Agro E, Gammie A, Goldman HB, Kirschner-Hermanns R, F W M Rosier P, Serati M, Solomon E, van Koeveringe G, Bachmann LM, Kessler TM. Randomised Controlled Trials Assessing the Clinical Value of Urodynamic Studies: A Systematic Review and Meta-analysis. Eur Urol Open Sci. 2022;44:131-141. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 19. | Kuo HC. Clinical symptoms are not reliable in the diagnosis of lower urinary tract dysfunction in women. J Formos Med Assoc. 2012;111:386-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 20. | Kuo HC. A Precision Urodynamic Diagnosis is Essential for Successful Treatment of Lower Urinary Tract Dysfunction. Eur Urol Open Sci. 2022;46:36-38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 21. | Arab Hassani F, Jin H, Yokota T, Someya T, Thakor NV. Soft sensors for a sensing-actuation system with high bladder voiding efficiency. Sci Adv. 2020;6:eaba0412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 22. | Stein R, Schröder A, Beetz R, Ermert A, Filipas D, Fisch M, Goepel M, Körner I, Schönberger B, Sparwasser C, Stöhrer M, Thüroff JW. [Urological problems in patients with meningomyelocele. Diagnostic studies and management]. Urologe A. 2007;46:1620-1642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Maison POM, Lazarus J. The management of paediatric neurogenic bladder: an approach in a resource-poor setting. Paediatr Int Child Health. 2017;37:280-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 24. | Metcalfe P. Nuances and Pitfalls in Pediatric Urodynamics: Perfecting Imperfection. J Urol. 2021;205:333-334. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 25. | Moghalu O, Stoffel JT, Elliott SP, Welk B, Zhang C, Presson A, Myers J. Time-Related Changes in Patient Reported Bladder Symptoms and Satisfaction after Spinal Cord Injury. J Urol. 2022;207:392-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 26. | Viaene AM, Roggeman S, Vanhaute OA, Raes A, Colman R, Everaert K. Nocturnal bladder emptying and Quality of Life in patients with spinal cord injury. Eur J Phys Rehabil Med. 2022;58:397-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 27. | Starowicz J, Cassidy C, Brunton L. Health Concerns of Adolescents and Adults With Spina Bifida. Front Neurol. 2021;12:745814. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 28. | Fumincelli L, Mazzo A, Martins JCA, Henriques FMD, Orlandin L. Quality of life of patients using intermittent urinary catheterization. Rev Lat Am Enfermagem. 2017;25:e2906. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 29. | Dekalo A, Myers JB, Kennelly M, Welk B. General and bladder-related quality of life: A focus on women living with spinal cord injury. Neurourol Urodyn. 2022;41:980-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 30. | Manack A, Motsko SP, Haag-Molkenteller C, Dmochowski RR, Goehring EL Jr, Nguyen-Khoa BA, Jones JK. Epidemiology and healthcare utilization of neurogenic bladder patients in a US claims database. Neurourol Urodyn. 2011;30:395-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 166] [Article Influence: 11.1] [Reference Citation Analysis (0)] |