Published online Jan 6, 2023. doi: 10.12998/wjcc.v11.i1.225
Peer-review started: October 17, 2022
First decision: October 28, 2022
Revised: November 7, 2022
Accepted: December 9, 2022
Article in press: December 9, 2022
Published online: January 6, 2023
Processing time: 79 Days and 11 Hours
High flow priapism (HFP) is a rare type of priapism. Perineal trauma is the most common cause of HFP. Trauma-induced penile artery injury may lead to an arterial-cavernosal fistula, whereas persistent irregular arterial blood flow entering the corpora cavernosum can cause a persistent penile erection. The routine treatment of HFP focuses on addressing the abnormal penile erectile status and avoiding post-treatment erectile dysfunction. Interventional embolization is an important therapeutic modality for HFP, and bilateral embolization therapy is currently the most commonly used technique for patients with bilateral cavernous artery fistulas; however, unilateral embolization therapy has yet to be reported.
Herein, we report of the case of a 26-year-old Chinese male who presented with a persistent abnormal erection for 12 h after perineal impact injury. Medical history, cavernous arterial blood gas analysis and radiological examinations led to a diagnosis of HFP caused by bilateral cavernous artery fistulas. We performed routine conservative treatment (compression therapy and ice application) for the patient after admission; however, 10 d later, his symptoms had not been relieved. After completion of the preoperative workup, right (severe side) selective perineal artery embolization was performed; the left cavernous artery fistula was left untreated. After postoperative continuation of conservative treatment for 72 h, the patient experienced complete penile thinning. The patient had no symptoms of erectile dysfunction over a follow-up period of 12 mo.
Compared with bilateral cavernous artery fistula embolization, we believe that unilateral cavernous artery fistula embolization can achieve positive clinical efficacy and reduce the risk of postoperative erectile dysfunction secondary to penile ischemia.
Core Tip: High flow priapism (HFP) is a rare type of priapism. Interventional embolization is the treatment of choice for HFP that is refractory to conservative management (compression therapy and ice application). In patients with HFP due to bilateral cavernous artery fistulas, the interventional treatment has primarily involved bilateral embolization. However, the treatment modality of bilateral embolization may increase the risk of erectile dysfunction because of postoperative ischemia. Compared with bilateral embolization, unilateral embolization may reduce the risk of erectile dysfunction while achieving clinical outcomes. This is the first report of successful HFP using unilateral embolization for bilateral cavernous artery fistulas.
- Citation: Li G, Liu Y, Wang HY, Du FZ, Zuo ZW. High-flow priapism due to bilateral cavernous artery fistulas treated by unilateral embolization: A case report. World J Clin Cases 2023; 11(1): 225-232
- URL: https://www.wjgnet.com/2307-8960/full/v11/i1/225.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i1.225
Priapism is defined as a prolonged penile erection that persists beyond 4 h and is not associated with sexual stimulation. The annual incidence of priapism is approximately 0.5-0.9 in every 100000 males, and it mainly occurs in men who are 40-years-old or older (mean age: 50 years)[1]. Priapism can be classified as ischemic (veno-occlusive, low flow) priapism, nonischemic (arterial, high flow) priapism, and stuttering (intermittent) priapism[2]. High flow priapism (HFP) is mainly attributed to trauma and accounts for less than 5% of all cases involving priapism[3]. Cavernous artery fistulas due to penile injury can cause arterial flow to persistently enter the cavernous body, thus resulting in a persistent abnormal erection[4]; this condition can cause secondary arterial hematoma and pseudoaneurysm.
HFP is not an emergency because the involvement of cavernous body ischemia or acidosis is rare. Therefore, interventional embolization is the first choice for patients with HFP when conservative treatment fails[5]. Most previous reports[6,7] have advocated for the use of simultaneous bilateral embolization for HFP patients with bilateral cavernous artery fistulas. However, bilateral arterial embolization can cause a significant reduction in penile blood supply; this condition is linked to a greater risk of postoperative erectile dysfunction (ED). To the best of our knowledge, no case of successful unilateral arterial embolization for patients with HFP has been previously reported.
The therapeutic concept of unilateral arterial embolization is to convert bilateral cavernous artery fistulas into unilateral fistulas. We hypothesized that unilateral arterial embolization could also reduce the overall penile blood flow rate because it is more conducive to platelet formation and aggregation, thus allowing for the spontaneous occlusion of the fistula. This treatment may also increase the efficacy of subsequent conservative treatment[8,9]. Furthermore, the preservation of the contralateral blood supply may reduce the postoperative risk of ED, which is secondary to penile ischemia. Herein, we present a case report involving the unilateral arterial embolization of a young patient with HFP due to bilateral cavernous artery fistulas. This case is described in accordance with the CARE reporting checklist[10].
A 26-year-old man presented to the urology clinic with a chief complaint of persistent penile erection for over 12 h after trauma.
The patient reported that his perineum was hit by a dumbbell during exercise approximately 24 h before presenting to the clinic; he did not feel any obvious pain.
The patient had no other physical problems, and there was nothing of relevance in his medical history.
The patient denied any family history of reproductive disease.
The angle of the abnormal erection of his penis was greater than 45°. Preinjury sexual function assessment on the 5-item version of the International Index of Erectile Function (IIEF-5)[11] was 24; additionally, his erection hardness score level (EHS)[12] was 4.
Corporal arterial blood gas analysis showed a PaO2 of 101 mmHg, a PaCO2 of 32 mmHg, and a pH of 7.45 (suggestive of arterial blood).
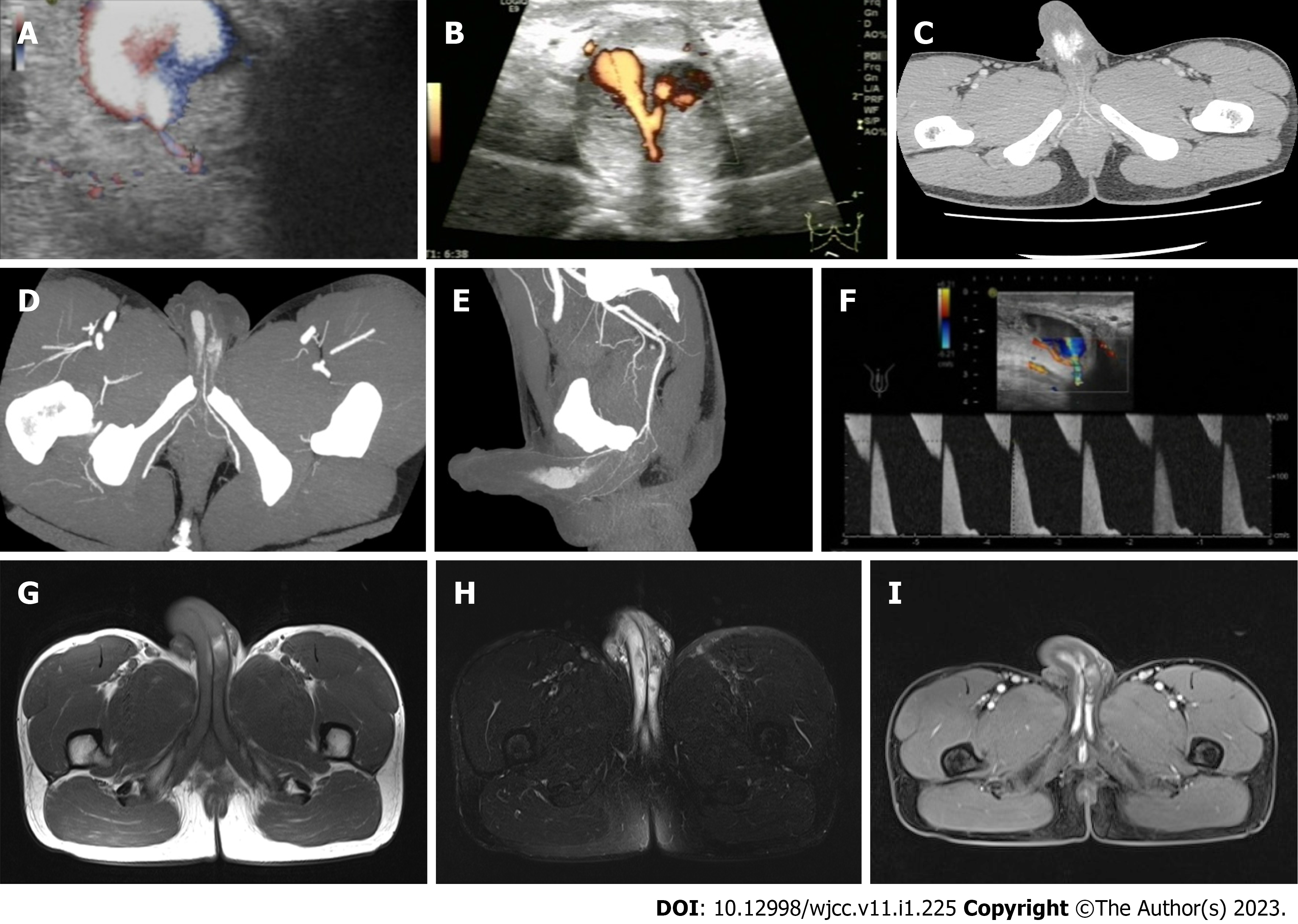
Imaging examinations revealed bilateral cavernous artery fistulas and bilateral pseudoaneurysms complicated by an interaneurysmal fistula (Figure 1A-E). Color Doppler ultrasonography (CDUS) also revealed an arterial flow that was characterized by a high flow with high resistance and irregular biphasic bidirectional flow (Figure 1F). Magnetic resonance imaging (MRI) of the pelvis was also suggestive of bilateral cavernous pseudoaneurysms and cavernous smooth muscle injury (Figure 1G-I).
Combined with the patient’s medical history and the abovementioned examinations, the final diagnosis was HFP.
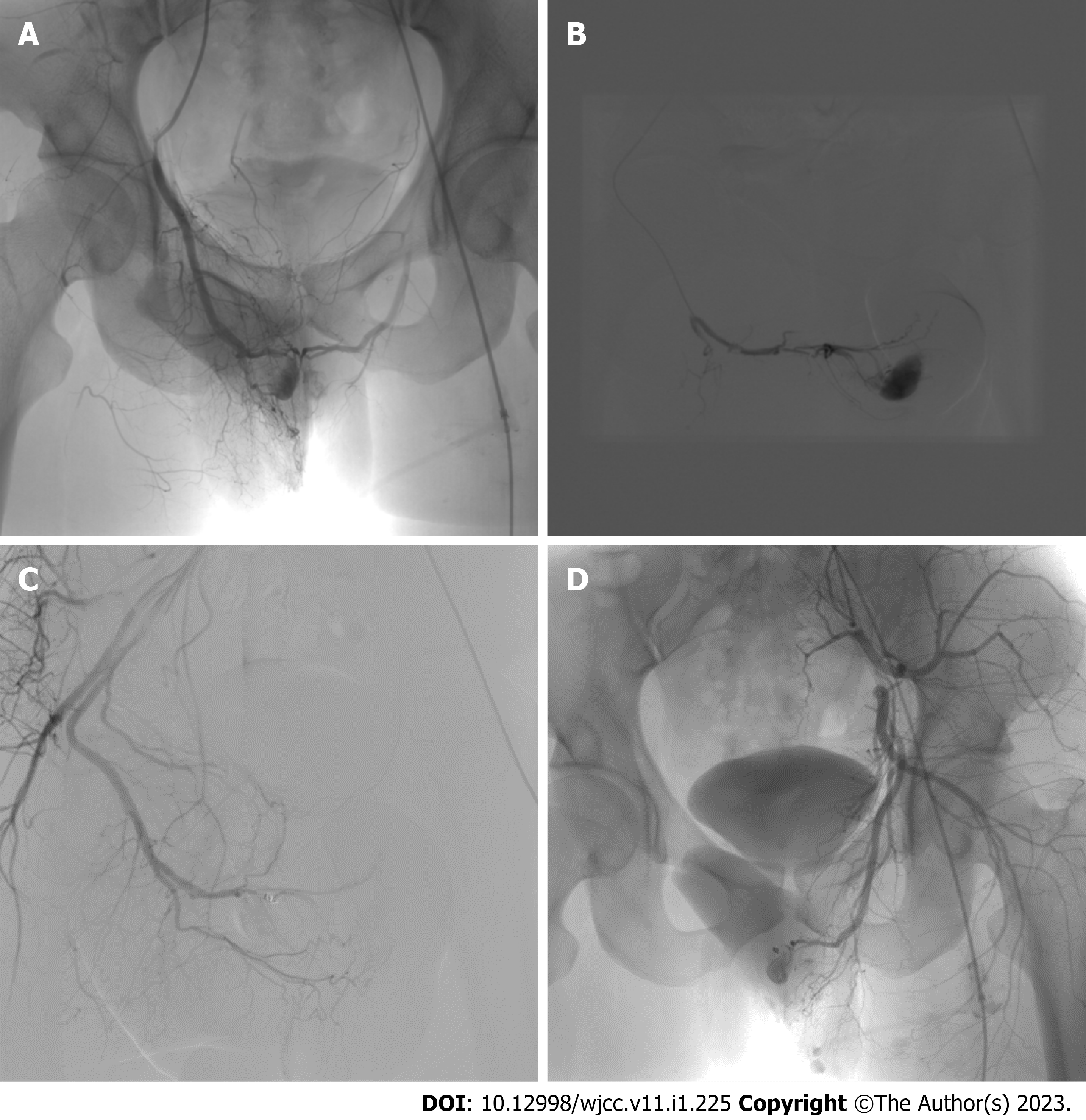
The patient’s symptoms were not significantly relieved after conservative treatment (regional compression and ice application) for 10 d. Given that the patient was young and had strongly requested postoperative sexual function recovery, we planned to apply unilateral arterial embolization as an experimental surgical method that may reduce the incidence of postoperative ED. Informed consent was obtained from the patient, and interventional embolization was performed after the relevant preoperative examinations were completed. During the intervention operation, the left femoral artery was cannulated via the Seldinger’s method; moreover, bilateral internal iliac artery angiography with a 5 F-Cobra catheter revealed a bilateral cavernous artery fistula, pseudoaneurysm, and an intertumoral fistula (Figure 2A). The 2.7 F microcatheter was superselectively inserted into the right internal pudendal artery for angiographic confirmation (Figure 2B). Embolization was performed with microcoils (1 mm) combined with gel-foam particles (750-1200 µm) at the proximal position of the right penile dorsal artery (Figure 2C). The left cavernous artery fistula was not treated with embolization (Figure 2D). With conservative treatment, the patient completely stopped experiencing penile erection 72 h after interventional surgery.
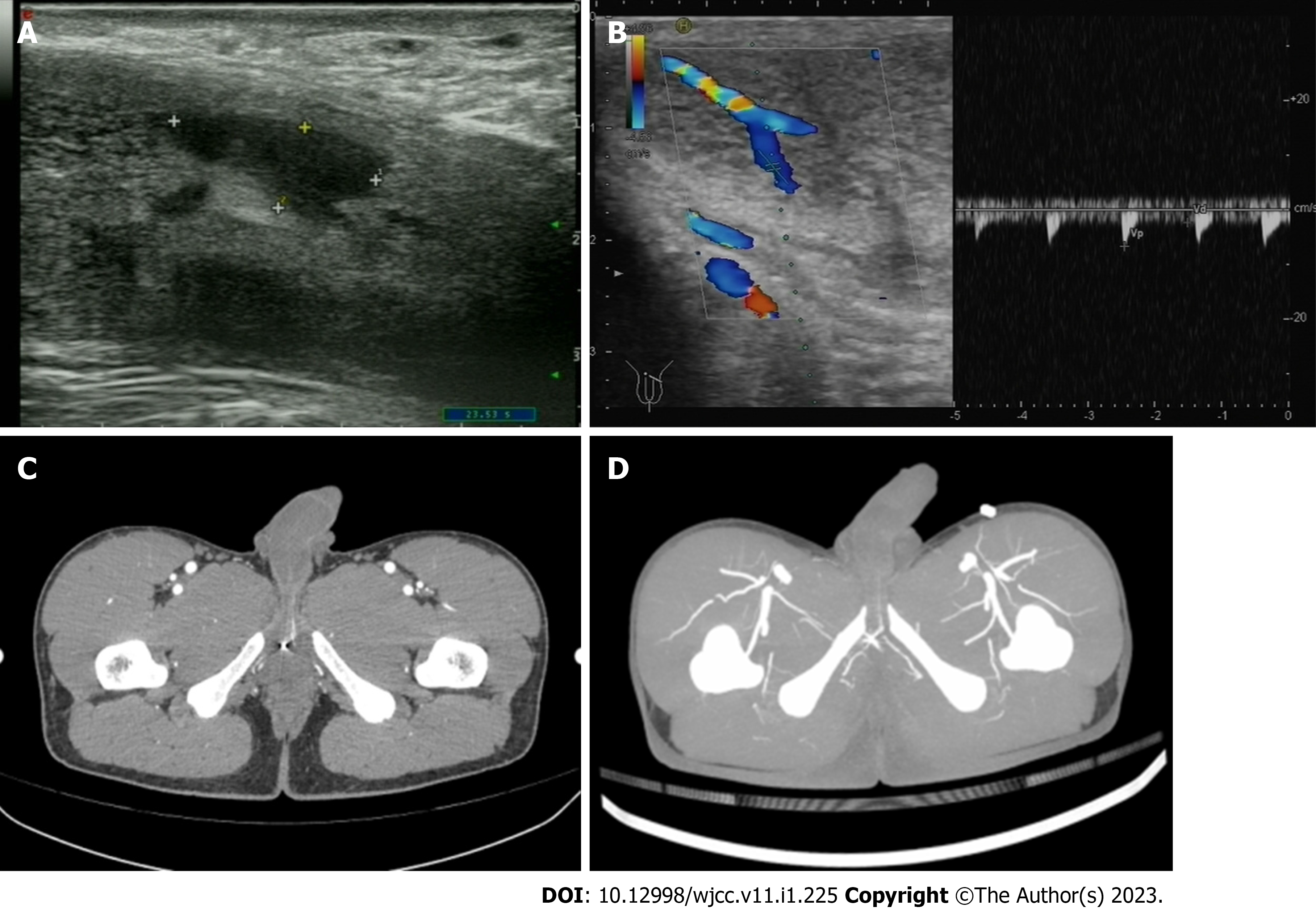
The patient underwent re-examinations 6 mo after embolization. CDUS revealed anechoic areas of the bilateral cavernous body (Figure 3A) and an increased resistance index in the right penile dorsal artery (embolization side) (Figure 3B). Computed tomography angiography (CTA) revealed that the microcoil was fixed in the right penile dorsal artery (Figure 3C), and the distal part of the right penile dorsal artery had faded (Figure 3D). During the 12-mo follow-up, the patient did not experience recurrent abnormal persistent erection or ED. The assessment of sexual function was as follows: preoperative data (IIEF-5: 24, EHS: 4); 6-mo postoperative data (IIEF-5: 24, EHS: 4); and 12-mo postoperative data (IIEF-5: 25, EHS: 4). The patient was very satisfied with the treatment outcome and reported marriage plans in the near future. All of the procedures that were performed in this study were in accordance with the ethical standards of the Medical Ethics Committee of the General Hospital of Western Theater Command and complied with the Helsinki Declaration (as revised in 2013). The patient provided signed informed consent for the publication of this case report and the accompanying images.
HFP refers to a persistent erection caused by an unregulated cavernous artery fistula; the etiology of this condition is predominantly attributed to perineal trauma[13]. Based on medical history, clinical manifestation, and auxiliary examination, the diagnosis of HFP is not difficult[14,15]. Corporal arterial blood gas analysis can distinguish whether priapism is HFP. Additionally, it is an inexpensive and simple diagnostic method[16]. Generally, in cases of high-flow priapism, the blood is red in color and well oxygenated (PaO2 > 90 mmHg, PaCO2 < 40 mmHg and pH 7.40)[17].
CDUS is a rapid and noninvasive tool for fistula localization, type discrimination, and the monitoring of treatment outcomes. Moreover, it is considered the most efficient and safe technique for the diagnosis of HFP[18,19]. In addition, the sensitivity of CDUS in localizing an arteriocavernosal fistula is almost 100%[20]. CTA has a similar value to CDUS in the diagnosis and follow-up of HFP[21]. Relative to CDUS, CTA has advantages in the detection of pelvic injuries, pelvic vascular anatomy, and anatomic variants. It can provide significant guidance in preoperative preparation for interventional embolization[22].
The diagnostic value of MRI and positron emission tomography-computed tomography for priapism has not been established in detail. In a previous study, Nasiri et al[23] reported that benign HFP was characterized by diffuse and intense 18F-fluorodeoxyglucose uptake. MRI is advantageous for the understanding of cavernous smooth muscle injury and the detection of unusual conditions, such as malignant infiltration[24]. Our case involved a typical trauma-induced HFP with high-flow arterial cavernous artery blood gas. Furthermore, CDUS, CTA, and MRI clearly revealed bilateral cavernous artery fistulas, bilateral pseudoaneurysms with an interaneurysmal fistula, penile artery flow, and pelvic vascular anatomy, thus providing a good preoperative reference for interventional embolization evaluation. Digital subtraction angiography further confirmed the diagnosis.
The main treatment modalities for HFP are conservative management, interventional embolization, medical therapy, and surgical management. Penile exploration and direct surgical ligation of sinusoidal fistulas are efficacious in up to 63% of cases (with a 50% rate of ED)[5]. The surgical management of nonischemic priapism is the last resort option. At present, only a small number of studies have reported the use of androgen blockade to suppress nocturnal erections as an alternative treatment for HFP. Mwamukonda et al[25] stated that leuprorelin, bicalutamide, and other drugs can induce the cavernous arteriovenous fistula to close. However, all of the patients (a total of 7) reported some degree of ED during therapy in this study. The effectiveness and side effects of this treatment remain to be further verified in a large multicenter study.
The American Urological Association Guidelines on the Management of Priapism[5] and the European Association of Urology Guidelines on Priapism[14] both indicate that interventional embolization is the first choice treatment modality for patients with HFP in which conservative treatment has failed; this technique has an effective rate of approximately 70%-89% as well as a < 20% incidence rate of ED. Occlusive agents include temporary occlusive agents (such as autologous blood clots and gel foam) and permanent occlusive agents (such as microcoils, n-butyl cyanoacrylate, and polyvinyl alcohol). Currently, the choice of material for embolization remains controversial. Materials used for permanent embolization are associated with better embolization effects, whereas temporary embolization materials can reduce the postoperative incidence rate of ED[5,26,27].
The American Urological Association Guidelines on the Management of Priapism stated that when using permanent occlusive agents, 78% of patients with HFP were effectively treated (with an incidence rate of ED of 39%). In contrast, with temporary embolization materials, 74% of patients with HFP were effectively treated, and the incidence rate of ED was 5% (based on data retrieved from the MEDLINE database from 1966 to 2001)[5]. Thus, temporary embolization materials were recommended. However, Kojima et al[26] reviewed reports published from 2001 to 2009 in the MEDLINE database and extracted a total of 96 patients with HFP who experienced arterial embolization. These authors found that the rates of symptom improvement were more favorable with permanent embolizing materials than with temporary embolizing materials; thus, permanent occlusive agents were recommended.
In another study, Arrichiello et al[27] reviewed a total of 113 patients with HFP undergoing interventional embolization between 1990 and 2020 and found that gel foam was associated with the highest clinical effective rate (89%) and the lowest recurrence rate (13%), thus suggesting that the choice of embolizing material should be based on the experience of the operator, the characteristics of the fistula, and the specific clinical features of the patient. Nevertheless, as key representatives of the two types of embolizing materials, gel foam and microcoils are superior to other materials in terms of therapeutic efficacy, recurrence rate, and prognosis. Moreover, they are the mainstream materials used for interventional embolization[9,26,27].
Due to the fact that the width of the fistula in our patient was approximately 0.6 mm, as determined by preoperative ultrasound (Figure 1A), a 2.7 F microcatheter (approximately 0.9 mm) was not able to superselectively penetrate into the fistula. Thus, we chose to embolize the right penile dorsal artery at a point proximal to the fistula with a microcoil (1 mm) combined with gel-foam particles (750 µm-1200 µm) (Figure 2B and C). The left arterial fistula was not embolized (Figure 2D); instead, we planned to observe the effect of postoperative conservative treatment to decide whether to perform contralateral embolization. The penile erection experienced by this patient was completely eliminated within 72 h of the operation. Postoperative imaging did not reveal any bilateral cavernous fistulas (Figure 3). Furthermore, the patient did not experience recurrent abnormal persistent erection or ED at the 12-mo follow-up.
Unilateral embolization therapy converts bilateral cavernous artery fistulas into unilateral fistulas with an overall reduction in penile blood flow. This treatment modality preserves the contralateral cavernosa blood supply and may reduce the risk of ED secondary to penile ischemia. However, relative to bilateral embolization, unilateral embolization demonstrates a risk of secondary contralateral embolization for patients with poor postoperative outcomes; this increases the number of procedures and the financial burden on patients. To the best of our knowledge, no previous reports have described a successful case involving successful unilateral arterial embolization in HFP patients with bilateral cavernous artery fistulas.
Langenhuijsen et al[28] and Čechová et al[29] both attempted to perform unilateral arterial embolization; however, their patients did not achieve clinical expectations and had to receive a second round of complementary embolization. Langenhuijsen et al[28] believed that bilateral embolization is indicated when unilateral treatment does not result in detumescence of the penis. Moreover, Čechová et al[29] held the viewpoint that when no further embolization was possible, a conservative approach after embolization should be performed, even though the fistula was still present.
Our patient was fortunate enough that the objective of treatment was attained through a single unilateral embolization with postoperative conservative treatment. This case successfully verified that unilateral arterial embolization may be a practically feasible treatment method for patients with HFP due to bilateral cavernous artery fistulas and has the potential to reduce the incidence rate of postoperative ED. Therefore, we believe that although unilateral arterial embolization may increase the number of operations, it is worth attempting in patients with a strong need for postoperative sexual function recovery. We should perform contralateral embolization in cases where conservative treatment has continued for some time after unilateral embolization and then failed in achieving clinical outcomes. Furthermore, the direct selection of bilateral embolization is the more appropriate surgical approach for patients who do not have a strong need for postoperative sexual recovery.
To the best of our knowledge, this is the first report to describe the successful application of unilateral arterial embolization in a young patient with HFP due to bilateral cavernous artery fistulas. We believe that unilateral embolization can achieve clinical efficacy and can safely and flexibly reduce the risk of ED secondary to postoperative penile ischemia. Unilateral arterial embolization is the interventional treatment modality of choice for patients who strongly demand postoperative sexual recovery. Future studies need to involve an increased sample size to accurately determine the specific efficacy and prognosis of unilateral arterial embolization. The medical images, laboratory indices, and clinical assessments of this patient were relatively complete, and we believe that this successful experience of unilateral embolization for the treatment of HFP caused by bilateral cavernous artery fistula will provide more ideas for the future diagnosis and treatment of HFP.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Gao C, China; Li W, China S-Editor: Xing YX L-Editor: Filipodia P-Editor: Xing YX
| 1. | Eland IA, van der Lei J, Stricker BH, Sturkenboom MJ. Incidence of priapism in the general population. Urology. 2001;57:970-972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 146] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 2. | Maan Z, Arya M, Patel HR. Priapism--a review of the medical management. Expert Opin Pharmacother. 2003;4:2271-2277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Broderick GA, Kadioglu A, Bivalacqua TJ, Ghanem H, Nehra A, Shamloul R. Priapism: pathogenesis, epidemiology, and management. J Sex Med. 2010;7:476-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 208] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 4. | Witt MA, Goldstein I, Saenz de Tejada I, Greenfield A, Krane RJ. Traumatic laceration of intracavernosal arteries: the pathophysiology of nonischemic, high flow, arterial priapism. J Urol. 1990;143:129-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 109] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 5. | Montague DK, Jarow J, Broderick GA, Dmochowski RR, Heaton JP, Lue TF, Nehra A, Sharlip ID; Members of the Erectile Dysfunction Guideline Update Panel; Americal Urological Association. American Urological Association guideline on the management of priapism. J Urol. 2003;170:1318-1324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 337] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 6. | Lazinger M, Beckmann CF, Cossi A, Roth RA. Selective embolization of bilateral arterial cavernous fistulas for posttraumatic penile arterial priapism. Cardiovasc Intervent Radiol. 1996;19:281-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Williams AB, Lax LG. A rare case of post-traumatic high-flow priapism requiring endovascular salvage with bilateral superselective microcoil embolization. J Surg Case Rep. 2021;2021:rjab077. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 8. | Ilkay AK, Levine LA. Conservative management of high-flow priapism. Urology. 1995;46:419-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 32] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Ingram AR, Stillings SA, Jenkins LC. An Update on Non-Ischemic Priapism. Sex Med Rev. 2020;8:140-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Riley DS, Barber MS, Kienle GS, Aronson JK, von Schoen-Angerer T, Tugwell P, Kiene H, Helfand M, Altman DG, Sox H, Werthmann PG, Moher D, Rison RA, Shamseer L, Koch CA, Sun GH, Hanaway P, Sudak NL, Kaszkin-Bettag M, Carpenter JE, Gagnier JJ. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol. 2017;89:218-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 741] [Cited by in RCA: 1022] [Article Influence: 127.8] [Reference Citation Analysis (0)] |
| 11. | Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Peña BM. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1933] [Cited by in RCA: 2175] [Article Influence: 83.7] [Reference Citation Analysis (0)] |
| 12. | Sönmez MG, Öztürk A. Is there a relation between priapism occurring after penile doppler ultrasonography and international erectile function index score and erection hardness score levels? Turk J Urol. 2017;43:439-743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Acampora C, Borzelli A, Di Serafino M, Iacobellis F, Barbuto L, D'errico C, Ponticiello G, Romano L. High-flow post-traumatic priapism: diagnostic and therapeutic workup. J Ultrasound. 2021;24:539-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Salonia A, Eardley I, Giuliano F, Hatzichristou D, Moncada I, Vardi Y, Wespes E, Hatzimouratidis K; European Association of Urology. European Association of Urology guidelines on priapism. Eur Urol. 2014;65:480-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 203] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 15. | Ericson C, Baird B, Broderick GA. Management of Priapism: 2021 Update. Urol Clin North Am. 2021;48:565-576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 16. | Llorente C, Baena V, Carnero J, Rodríguez J, Fernández Ovies JM. [Value of cavernous gasometry in the physiopathologic diagnosis and treatment of priapism]. Actas Urol Esp. 1990;14:444-445. [PubMed] |
| 17. | Magoha GA. Priapism: a historical and update review. East Afr Med J. 1995;72:399-401. [PubMed] |
| 18. | Sancak T, Conkbayir I. Post-traumatic high-flow priapism: management by superselective transcatheter autologous clot embolization and duplex sonography-guided compression. J Clin Ultrasound. 2001;29:349-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Wakrim S, Ziouziou I, Ralph D, Khabbal Y. Penile Doppler ultrasound study in priapism: A systematic review. Prog Urol. 2022;32:61-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 20. | Bertolotto M, Zappetti R, Pizzolato R, Liguori G. Color Doppler appearance of penile cavernosal-spongiosal communications in patients with high-flow priapism. Acta Radiol. 2008;49:710-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 21. | Suzuki K, Nishizawa S, Muraishi O, Fujita A, Hyodoh H, Tokue A. Post-traumatic high flow priapism: demonstrable findings of penile enhanced computed tomography. Int J Urol. 2001;8:648-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | He G, Li T, Tang J, Zhang G. Utility of cone-beam CT imaging for the determination of feeding vessels during arterial embolization for massive hemoptysis. Diagn Interv Radiol. 2018;24:372-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Nasiri Z, Zarehparvar Moghadam S, Kiamanesh Z, Emami F, Sadeghi R. Benign High-Flow Priapism With a Diffuse and Intense 18F-FDG Uptake on 18F-FDG PET/CT Scanning. Clin Nucl Med. 2019;44:e442-e444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 24. | Levey HR, Segal RL, Bivalacqua TJ. Management of priapism: an update for clinicians. Ther Adv Urol. 2014;6:230-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 68] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 25. | Mwamukonda KB, Chi T, Shindel AW, Lue TF. Androgen blockade for the treatment of high-flow priapism. J Sex Med. 2010;7:2532-2537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 26. | Kojima H, Tanigawa N, Kariya S, Komemushi A, Shomura Y, Yanishi M, Murota T, Sawada S. High-flow priapism undergoing arterial embolization: review of literature following American Urological Association guideline on the management of priapism. Minim Invasive Ther Allied Technol. 2009;18:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 27. | Arrichiello A, Angileri SA, Buccimazza G, Di Bartolomeo F, Di Meglio L, Liguori A, Gurgitano M, Ierardi AM, Papa M, Paolucci A, Carrafiello G. Interventional radiology management of high flow priapism: review of the literature. Acta Biomed. 2020;91:e2020010. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 28. | Langenhuijsen JF, Reisman Y, Reekers JA, de Reijke Th M. Highly selective embolization of bilateral cavernous arteries for post-traumatic penile arterial priapism. Int J Impot Res. 2001;13:354-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 29. | Čechová M, Pádr R, Hanek P, Chocholatý M. Spontaneous detumescence and full restoration of erection in a patient with high-flow priapism with persistent arterial-lacunar fistula after repeated selective embolisation-A case report. Andrologia. 2018;50:e13019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |