Published online Jan 6, 2023. doi: 10.12998/wjcc.v11.i1.187
Peer-review started: September 23, 2022
First decision: October 30, 2022
Revised: November 11, 2022
Accepted: December 21, 2022
Article in press: December 21, 2022
Published online: January 6, 2023
Processing time: 103 Days and 18.6 Hours
Adequate bowel preparation is critical for colonoscopy screening. At present, the most widely used intestinal cleaner recommended at home and abroad is Polyethylene glycol (PEG). Intestinal cleansers can cause electrolyte disturbances and hyponatremia. However, hyponatremic encephalopathy due to hyponatremia induced by PEG solution, although rare, can lead to serious irreversible sequelae and even death.
In this report, we discuss a case of neurological dysfunction due to hyponatremia, also known as hyponatremic encephalopathy, observed in a 63-year-old woman who underwent PEG-based bowel preparation for colonoscopy. She was eventually transferred to our intensive care unit for treatment due to her Glasgow Coma Scale score of 9/15 (Eye opening 2; Verbal response 1; Motor response 6) and abnormal laboratory tests.
Physicians should be thoroughly familiarized with the patient's history before prescribing PEG for bowel preparation, and timely identification of patients with hyponatremic encephalopathy is essential as delayed treatment is associated with poor neurological outcomes. An intravenous infusion of 3% sodium chloride is recommended at the onset of early symptoms. The goal of treatment is to adequately treat cerebral edema while avoiding serum sodium correction beyond 15 to 20 mEq/L within 48 h of treatment to prevent osmotic demyelination syndrome.
Core Tip: Hyponatremic encephalopathy caused by the use of polyethylene glycol (PEG) solution for intestinal cleaning is rare, which can lead to irreversible sequelae and even death. This case is a female with neurological dysfunction due to hyponatremia induced by the use of pegylated for bowel preparation before colonoscopy. The patient was in a coma with the brain suggesting cerebral edema, and was transferred to the intensive care unit for treatment with 3% sodium chloride injection. The patient's medical history should be fully understood before using PEG for bowel preparation, as both untimely and overtreatment can lead to serious complications.
- Citation: Zhao Y, Dong HS. Hyponatremic encephalopathy due to polyethylene glycol-based bowel preparation for colonoscopy: A case report. World J Clin Cases 2023; 11(1): 187-192
- URL: https://www.wjgnet.com/2307-8960/full/v11/i1/187.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i1.187
Colonoscopy is a gold standard for diagnostic screening of colon disorders[1]. High-quality bowel cleansing is a prerequisite for colonoscopy. Polyethylene glycol (PEG)-based solution is the most widely used intestinal cleansing agent, although several cases have been reported to cause hyponatremia[2-4], it is a relatively safe option for patients at risk of electrolyte imbalance and dehydration[5]. As the most common electrolyte abnormality, hyponatremia is closely related to the brain. Indeed, several neurological disorders are frequently associated with hyponatremia, and hyponatremia itself can involve central nervous system dysfunction[6]. Thus, hyponatremic encephalopathy induced by PEG solutions is of concern to us, although rare and potentially serious. Hyponatremic encephalopathy was first proposed by Arieff et al[7] and is defined as neurological symptoms associated with hypotonic cerebral edema[8], is most commonly seen in the intensive care unit (ICU), with a prevalence of only 1% of postoperative patients[9,10]. Its clinical manifestations include headache, nausea and vomiting, seizures, and decreased consciousness, etc, but the severity depends on the degree and rate of serum sodium reduction. At present, relevant guidelines indicate that hypertonic saline is considered to be a safe and effective treatment for acute or symptomatic hyponatremic encephalopathy[11,12]. However, hyponatremic encephalopathy is the result of multiple factors, and the current studies on its clinical characteristics and treatment are limited[7,13]. Here, we describe a case of a 63-year-old female who presented with acute hyponatremic encephalopathy and seizures after bowel cleansing with PEG for colonoscopy.
A 63-year-old female patient was brought to the local hospital in September 2021 due to a loss of appetite for the past month.
Therefore, a tumor was first suspected and a colonoscopy was performed in combination with the patient's medical history. This patient took PEG with 4.5 L water to clean the bowel before the colonoscopy. This patient was found unconscious and developed seizures the following afternoon, and a series of differential diagnoses were made to consider whether the patient had suffered from intracranial vasculopathy, cardiogenic causes, shock, or hypoglycemia. She was eventually transferred to our ICU for management.
The patient presented with gastric cancer 13 years ago and underwent radical gastrectomy. The patient subsequently developed liver metastases and received multiple chemotherapy regimens. In addition, the patient had a 10-year history of ulcerative colitis.
The patient denied a family history of malignant tumors or other diseases.
This patient was admitted to the ICU with a Glasgow Coma Scale (GCS) score of 9/15 [Eye opening (E) 2; Verbal response (V) 1; Motor response (M) 6] and no signs of meningeal irritation. The pupil examination revealed equal-sized and reactive to light.
Laboratory results revealed serum sodium (114 mmol/L, reference: 136 - 144 mmol/L), potassium (3.4 mmol/L, reference: 3.6 - 5.2 mmol/L), chloride (82 mmol/L, reference: 101 - 111 mmol/L), bicarbonate (21 mmol/L, reference: 22 - 26 mmol/L), blood urea nitrogen (32.4 mg/dL, reference: 9 - 20 mg/dL), creatinine (0.44 mg/dL, reference: 0.6 - 1.2 mg/dL), glucose (187.2 mg/dL, reference: 70- 120 mg/dL). That means a total loss of 19.65 g Na deficit. The level of hematocrit decreased from 32.8% to 29.6%.
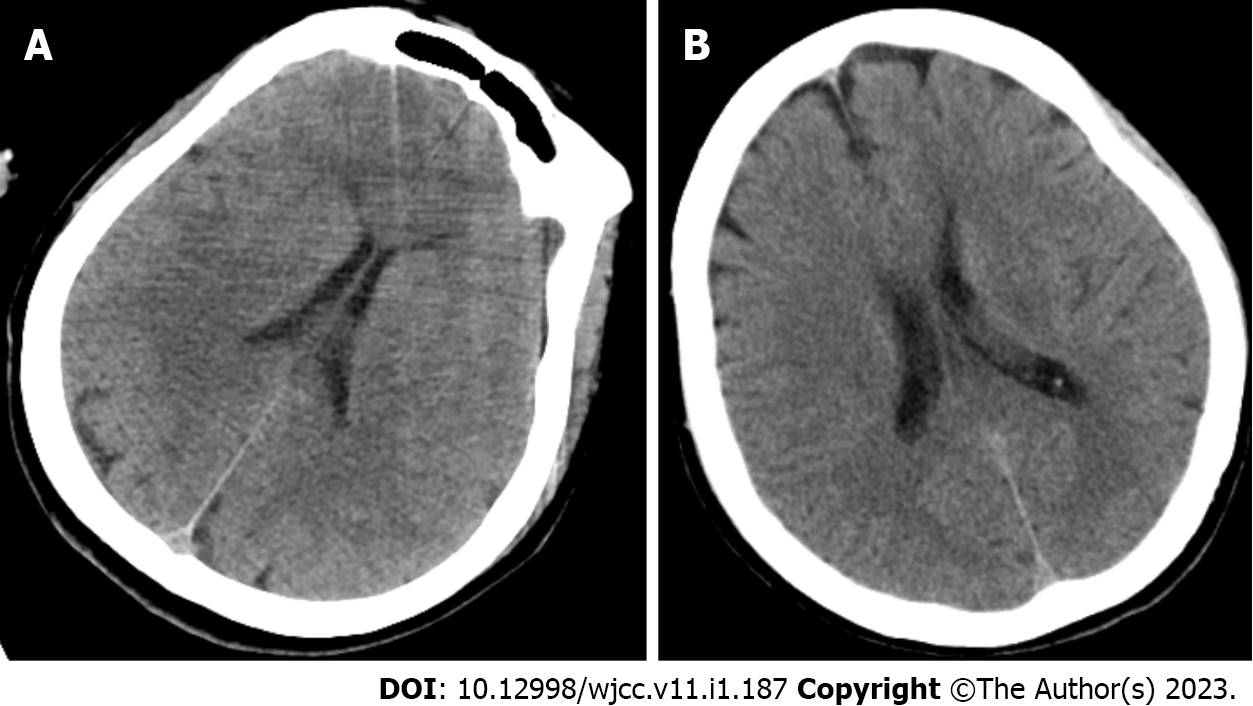
A computed tomography (CT) scan was performed and revealed cerebral edema (Figure 1).
After a series of differential diagnoses, combined with the patient's medical history, relevant examination, and treatment, the patient was finally diagnosed with hyponatremic encephalopathy.
This patient did not have any history of sedatives. She was initially treated with 3% sodium chloride (NaCl) injection. The serum sodium gradually increased to 124 mmol/L after 6 h. The infusions ceased once this patient was free from further seizures.
The following afternoon, the patient’s serum sodium returned to 135 mmol/L. Her neurological condition also improved dramatically during this period, with a GCS score of E4V5M6. A CT scan of the brain edema subsequently normalized (Figure 1). The patient was discharged home after 2 d of hospitalization. After a 1-mo of follow-up, the patient’s neurological function recovered completely.
Acute hyponatremia is often accompanied by major neurologic manifestations[13,14]. An increasing number of studies have reported acute hyponatremia caused by the use of PEG-based solutions during colonoscopy preparation[15,16]. The main symptoms of hyponatremia are nausea, vomiting, headache, seizures, and coma. However, cerebral edema is rare[3,15]. We demonstrate again that bowel preparation with PEG for colonoscopy with PEG may lead to brain cerebral edema associated with hyponatremia. The patient’s hyponatremia may be caused by several reasons. First of all, the patient had a history of gastric cancer and had undergone radical surgery at an early stage, which more or less affected gastrointestinal sodium absorption. Moreover, this patient had several high-risk factors, such as older age (> 60 years), female sex, and poor dietary intake. Hyponatremia is the most common electrolyte disorder in clinical practice, which is usually caused by excessive secretion of antidiuretic hormone (ADH) or infusion water retention. The syndrome of inappropriate ADH (SIADH) secretion can be caused by a variety of factors, such as ectopic secretion of ADH by tumor cells themselves, and the deterioration of the overall functional status of the patient can also induce ADH release independent of osmotic stimuli[17]. Therefore, hyponatremia is most likely the result of ectopic production of arginine vasopressin by the tumors in elderly patients in response to physiologic, non-osmotic ADH.
The European guideline recommends the use of hypertonic saline, usually 3% NaCl, for acute or symptomatic hyponatremia. Hypertonic saline is an effective and potentially life-saving treatment for brain edema induced by hyponatremia, because its high sodium concentration allows water to be diverted from the intracellular space[18].
Twelve cases of hyponatremia induced by PEG-based solutions have been reported (Table 1). Most patients were older than 60 years and most were female. Among them, one patient (case 3) had end-stage renal disease, and five patients (cases 2, 8, 9, 10, and 11) had their urination impaired due to thiazide diuretics. Cases 4 and case 6 had insufficient thyroid replacement and were older than 65 years, suggesting further exacerbation of their hyponatremia. In the presence of normal renal, thyroid, and adrenal function, patients 1 and 5 received an additional 4 L of rehydration and 3 L of PEG. Non-osmotic AHD stimulation combined with massive infusion is the main cause of hyponatremia in such patients. In addition, intestinal manipulation during bowel preparation for colonoscopy may lead to increased ADH. Patient (case 12) received a double dose of PEG, which caused a severe internal environmental disturbance. All the patients recovered fully except for the patient who had dialysis-dependent chronic kidney disease and who died from cardiac arrest. This case report has several limitations. First, the single case itself has limitations, and high-quality evidence is needed to confirm. Second, some techniques, like non-invasive brain stimulation techniques, should be more widely used in clinical practice in the future; Third, not all aspects of hyponatremia encephalopathy were discussed.
| Patient number | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
| Reference | [3] | [3] | [3] | [3] | [3] | [3] | [3] | [15] | [15] | [15] | [18] | [16] |
| Age | 59 | 62 | 51 | 73 | 70 | 65 | 69 | 53 | 79 | 68 | 64 | 71 |
| Sex | F | F | M | F | F | F | F | F | F | F | F | M |
| History | Hyster | Hyperte | Diabetes, End-stage renal disease | Depressi | Stenosis of internal carotid artery, Hyperte | Breast cancer, Total thyroid | Dyslip | Asthma, Osteopor | NA | Breast cancer, Nephrect | Hyperte | Diabetic, Colon cancer (suspicio |
| Prescript | Estradiol, Aspirin | Thiazide | Amlodip | Citalopr | Amlodip | Levothyr | Atorvast | Irbesart | Thiazides | Irbesarta | Thiazide | NA |
| Preparati | 3L PEG and 4L weak tea | 4L PEG | NA | 255g PEG and 64 ounces gatorade | 4L PEG and 3L clear water | 4L PEG | 4L PEG | NA | 10mg Bisacodyl and PEG mixed with 120mL gatorade | 2L Pico Prep and 1L PEG | 4L PEG | 7-8L PEG |
| Clinical presentat | Confusio | Seizure | Idioventr | Seizure | Seizure | Seizure | Seizure | Seizure | Nausea, Vomiting | Nausea, Vomiting, Malaise, Seizure | Seizure | Drowsy, Seizure |
| Blood pressure in mmHg | 110/70 | 130/90 | 167/78 | Normal | 190/100 | 156/85 | 143/74 | 150/86 | NA | 150/70 | NA | NA |
| Pulse in bpm | 60 | 90 | 103 | Normal | 84 | 86 | 76 | 79 | NA | 84 | NA | NA |
| Sodium in mmol/L | ||||||||||||
| Baseline | NA | 138 | 138 | NA | 140 | 144 | NA | NA | NA | NA | NA | NA |
| Lowest | 120 | 116 | 122 | 117 | 110 | 127 | 113 | 115 | 118 | 106 | 114 | 111 |
| Post-treatment | 138 | 130 | NA | 131 | 138 | 141 | 135 | NA | 133 | Normal | Normal | 132 |
| Potassi | 4.6 | 3.9 | 5.1 | 3.3 | 3.4 | 4.3 | 3.4 | 2.5 | NA | 3.1 | NA | NA |
| Chloride in mmol/L | NA | 79 | 94 | 79 | 72 | 104 | 72 | NA | NA | NA | NA | NA |
| Bicarbon | 17.2 | 26 | 20 | 21 | 17.3 | 17.3 | 17.3 | NA | NA | NA | NA | NA |
| Urea in mg/dL | NA | 2.5 | 24.3 | 6 | 11.8 | 14.6 | 11.8 | NA | NA | NA | NA | NA |
| Creatine in mg/dL | 0.9 | 0.6 | 7.7 | 0.6 | 0.67 | 0.71 | 0.67 | NA | NA | Normal | NA | NA |
| Glucose in mg/dL | 93 | NA | 95.5 | NA | 148 | 235 | 148 | NA | NA | NA | NA | Normal |
| Brain CT/MRI findings | Normal | Cerebral edema | Not done | Not done | Normal | Normal | Small vessel disease and tiny restrictio | Cerebral edema | Normal | Normal | Normal | Normal |
| Outcome | Complete recovery | Complete recovery | Death | Complete recovery | Complete recovery | Complete recovery | Complete recovery | Complete recovery | Complete recovery | Complete recovery | Complete recovery | Complete recovery |
Given this case report, physicians should be thoroughly familiarized with the patient's history before prescribing PEG for bowel preparation, and timely identification of patients with hyponatremic encephalopathy is essential, as delayed treatment is associated with poor neurological outcomes. An intravenous infusion of 3% sodium chloride is recommended at the onset of early symptoms while avoiding serum sodium correction beyond 15 to 20 mEq/L within 48 h of treatment to prevent osmotic demyelination syndrome.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Gkolfakis P, Belgium; Masaru T, Hungary; Sahin Y, Turkey S-Editor: Liu GL L-Editor: Filipodia P-Editor: Liu GL
| 1. | Windpessl M, Schwarz C, Wallner M. "Bowel prep hyponatremia" - a state of acute water intoxication facilitated by low dietary solute intake: case report and literature review. BMC Nephrol. 2017;18:54. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 2. | Seyrafian S, Sebghatollahi V, Bastani B. Hyponatremia-induced generalized seizure after taking polyethylene glycol for colon preparation-A case report and brief review of the literature. Clin Case Rep. 2022;10:e6247. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 3. | Ko SH, Lim CH, Kim JY, Kang SH, Baeg MK, Oh HJ. Case of inappropriate ADH syndrome: hyponatremia due to polyethylene glycol bowel preparation. World J Gastroenterol. 2014;20:12350-12354. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 14] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Matro R, Daskalakis C, Negoianu D, Katz L, Henry C, Share M, Kastenberg D. Randomised clinical trial: Polyethylene glycol 3350 with sports drink vs. polyethylene glycol with electrolyte solution as purgatives for colonoscopy--the incidence of hyponatraemia. Aliment Pharmacol Ther. 2014;40:610-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Yuanchao H, Xueping L, Tao L, Jianping N, Man M. The advantage of polyethylene glycol electrolyte solution combined with lactulose in patients with long interval preparation-to-colonoscopy. Turk J Gastroenterol. 2020;31:23-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Kirkman MA, Albert AF, Ibrahim A, Doberenz D. Hyponatremia and brain injury: historical and contemporary perspectives. Neurocrit Care. 2013;18:406-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Arieff AI. Hyponatremia, convulsions, respiratory arrest, and permanent brain damage after elective surgery in healthy women. N Engl J Med. 1986;314:1529-1535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 422] [Cited by in RCA: 353] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 8. | Ayus JC, Arieff AI. Chronic hyponatremic encephalopathy in postmenopausal women: association of therapies with morbidity and mortality. JAMA. 1999;281:2299-2304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 143] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 9. | Achinger SG, Ayus JC. Treatment of Hyponatremic Encephalopathy in the Critically Ill. Crit Care Med. 2017;45:1762-1771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 10. | Anderson RJ, Chung HM, Kluge R, Schrier RW. Hyponatremia: a prospective analysis of its epidemiology and the pathogenetic role of vasopressin. Ann Intern Med. 1985;102:164-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 460] [Cited by in RCA: 395] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 11. | Spasovski G, Vanholder R, Allolio B, Annane D, Ball S, Bichet D, Decaux G, Fenske W, Hoorn EJ, Ichai C, Joannidis M, Soupart A, Zietse R, Haller M, van der Veer S, Van Biesen W, Nagler E. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Intensive Care Med. 2014;40:320-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 118] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 12. | Hoorn EJ, Zietse R. Diagnosis and Treatment of Hyponatremia: Compilation of the Guidelines. J Am Soc Nephrol. 2017;28:1340-1349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 198] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 13. | Adrogué HJ, Madias NE. Hyponatremia. N Engl J Med. 2000;342:1581-1589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1255] [Cited by in RCA: 1106] [Article Influence: 44.2] [Reference Citation Analysis (0)] |
| 14. | Hsu YJ, Chiu JS, Lu KC, Chau T, Lin SH. Biochemical and etiological characteristics of acute hyponatremia in the emergency department. J Emerg Med. 2005;29:369-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Samad N, Fraser I. Severe symptomatic hyponatremia associated with the use of polyethylene glycol-based bowel preparation. Endocrinol Diabetes Metab Case Rep. 2017;2017. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 16. | Sunder Shrestha P, Acharya U, Karki B, Pathak R, Acharya SP. Symptomatic Hyponatremia following Bowel Preparation for Colonoscopy: A Case Report. JNMA J Nepal Med Assoc. 2020;58:938-940. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Ellison DH, Berl T. Clinical practice. The syndrome of inappropriate antidiuresis. N Engl J Med. 2007;356:2064-2072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 647] [Cited by in RCA: 567] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 18. | Spasovski G, Vanholder R, Allolio B, Annane D, Ball S, Bichet D, Decaux G, Fenske W, Hoorn EJ, Ichai C, Joannidis M, Soupart A, Zietse R, Haller M, van der Veer S, Van Biesen W, Nagler E; Hyponatraemia Guideline Development Group. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Nephrol Dial Transplant. 2014;29 Suppl 2:i1-i39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 353] [Article Influence: 32.1] [Reference Citation Analysis (0)] |