Published online Jan 6, 2023. doi: 10.12998/wjcc.v11.i1.172
Peer-review started: August 30, 2022
First decision: November 22, 2022
Revised: December 3, 2022
Accepted: December 19, 2022
Article in press: December 19, 2022
Published online: January 6, 2023
Processing time: 127 Days and 10.8 Hours
The levonorgestrel-releasing intrauterine system (LNG-IUS) is widely used in contraception, menorrhagia, dysmenorrhea and to prevent endometrial hyperplasia during estrogen supplementation. Perforation is more often seen after early postpartum placement. Perforation of the LNG-IUS occurring one month after placement is rare.
A 42-year-old female complained of progressive dysmenorrhea and increased menstrual volume. She was diagnosed with adenomyosis and the LNG-IUS was inserted in her uterine cavity. Routine ultrasound examination one month later revealed that the intra-uterine device (IUD) was not found in the uterine cavity, and further X-ray and pelvic magnetic resonance imaging showed an abnormal signal area in the left posterior region of the uterus. Laparoscopic exploratory surgery was performed and the LNG-IUS was found in the left uterosacral ligament.
Perforation of a LNG-IUS occurring one month after placement is rare, and is more common in inexperienced operators and after early postpartum placement. When the operation is difficult, ultrasound monitoring is recommended to reduce the risk of IUD perforation. For patients with inadequate surgery, postoperative imaging is recommended to detect potential risks as soon as possible.
Core Tip: Perforation of a levonorgestrel-releasing intrauterine system occurring one month after placement is rare. We report a patient who underwent levonorgestrel-releasing intrauterine system placement due to adenomyosis, and perforation was found one month later. Perforation is more common in inexperienced operators and after early postpartum placement. When the operation is difficult, ultrasound monitoring is recommended to reduce the risk of intra-uterine device perforation. Postoperative imaging is recommended to detect potential risks as soon as possible.
- Citation: Zhang GR, Yu X. Perforation of levonorgestrel-releasing intrauterine system found at one month after insertion: A case report. World J Clin Cases 2023; 11(1): 172-176
- URL: https://www.wjgnet.com/2307-8960/full/v11/i1/172.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i1.172
The levonorgestrel-releasing intrauterine system (LNG-IUS) is a widely used effective intrauterine progesterone release system. The most common adverse effects of the LNG-IUS include pelvic pain, dysmenorrhea, heavy menstrual bleeding, infection and malposition[1,2]. Perforation of the LNG-IUS is rare. We report a case of LNG-IUS perforation found one month after insertion.
A 42-year-old female patient complained of intermittent lower abdominal pain, with a visual analogue score of 2 points, and anal distension.
The patient had progressive dysmenorrhea and increased menstrual volume over the past years. She was diagnosed with adenomyosis and the LNG-IUS was placed in her uterine cavity by a certified doctor in November, 2021. Routine ultrasound examination in December, 2021 showed a strong echo area 0.6 cm × 0.2 cm in size in the uterine cavity, and no echo due to the intra-uterine device (IUD) was detected in the uterine cavity. The patient denied a history of vaginal exclusion of contraceptives. Hysteroscopy was performed in December 2021, and no IUD was found in the uterine cavity.
The patient had no previous disease history.
Gravidity 7 and parity 2 were noted. Menstrual history was 4-5 d/28 d. Her previous contraceptive method was the use of condoms. The patient had no history of family or genetic diseases.
Gynecological examination showed that the uterus was posterior, tough and flexible. Bimanual examination showed that a tough cord was felt in the left side of the uterus, with positive tenderness.
Laboratory examinations showed that the total number of white blood cells was 4.65 × 109/L, and the proportion of neutrophils was 51.6%.
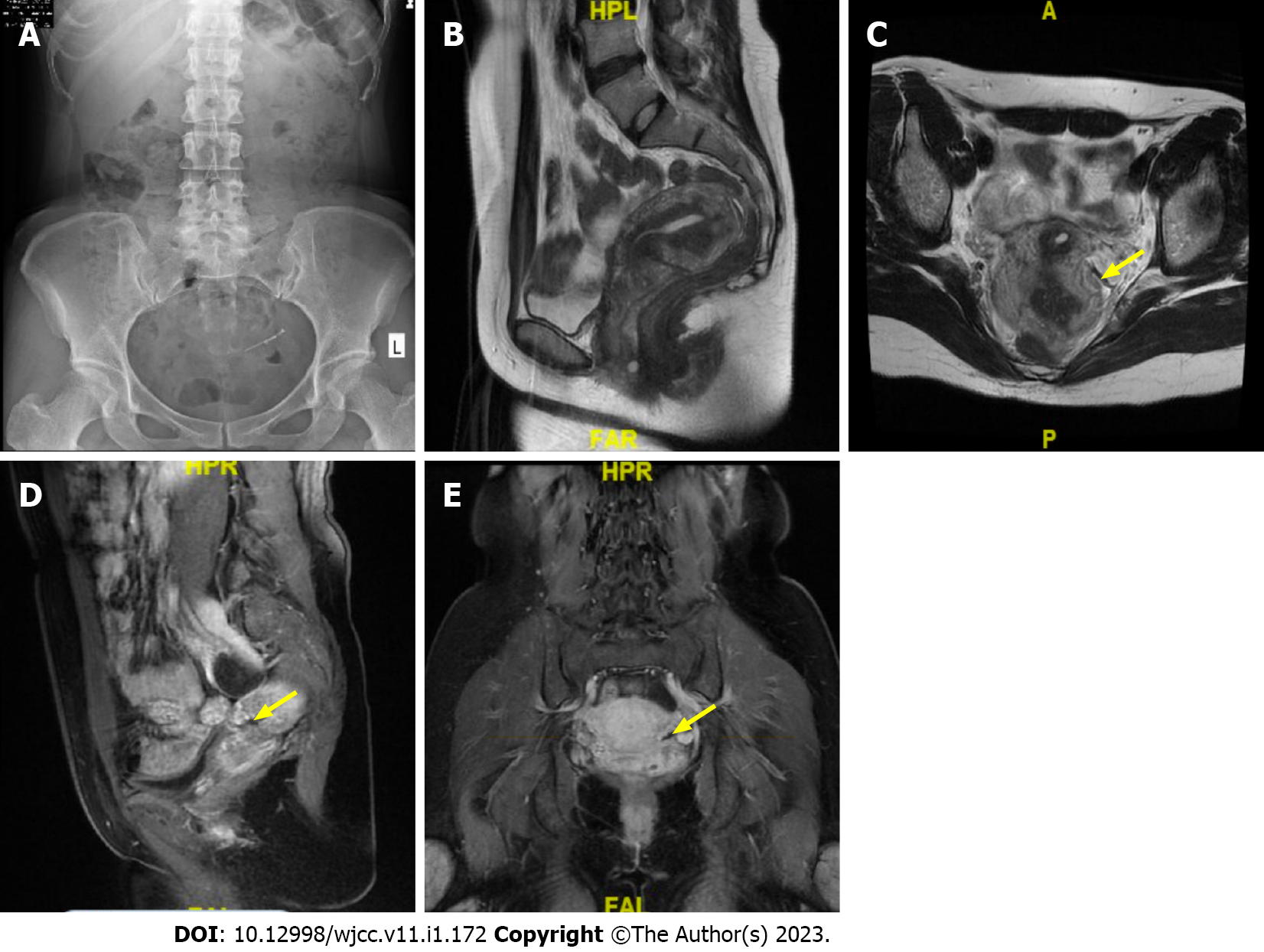
X-ray showed that a radiopaque T-shaped device was visible in the pelvis. Transvaginal ultrasonography revealed that the uterus was 5.9 cm × 7.5 cm × 5.2 cm in size; the endometrium was 0.4 cm thick; the muscular layer showed uneven echo patterns, with a thickness of 2.2 cm in the anterior muscular layer and 2.7 cm in the posterior; no echo area was detected in the left ovary, which was 3.5 cm × 2.3 cm in size, with a clear boundary and no blood flow signal. Pelvic magnetic resonance imaging presented abnormal signal in the left posterior area of the uterus (Figure 1).
Extrauterine device malposition.
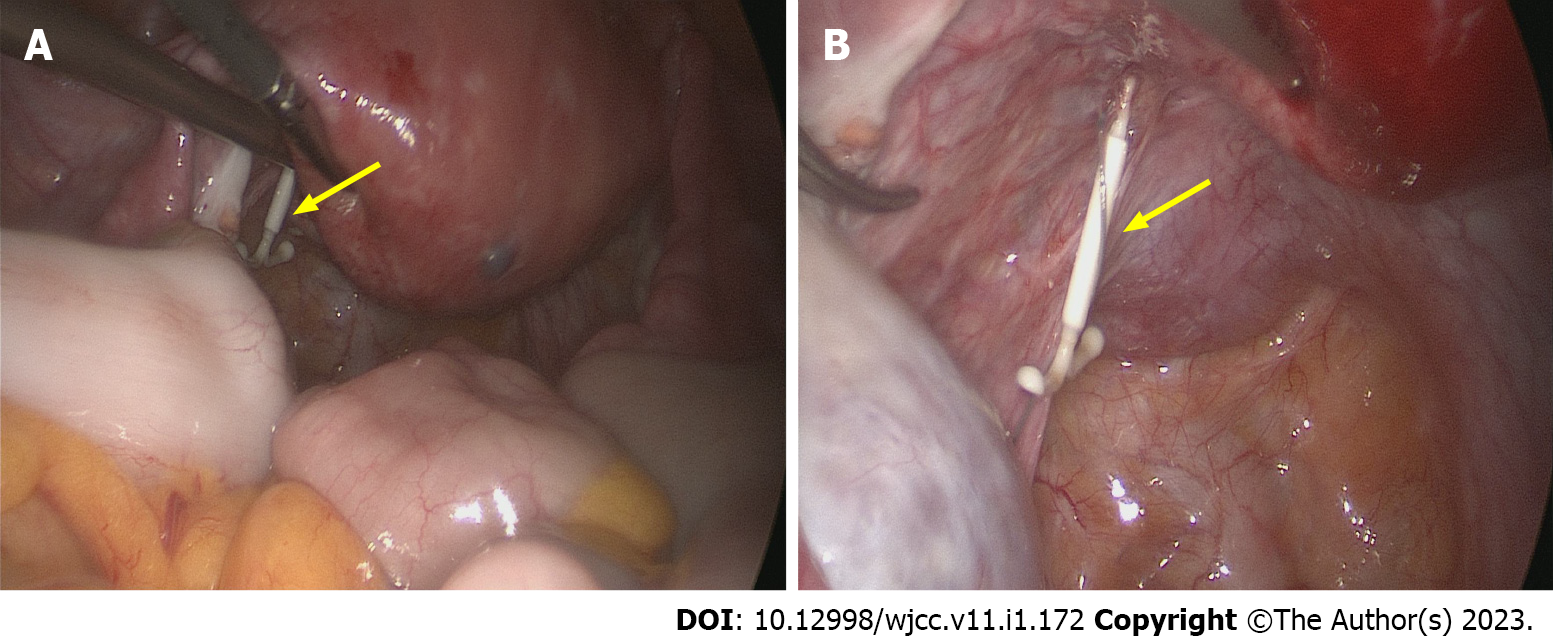
Given the possibility of IUD malposition, the patient underwent emergency laparoscopic exploratory surgery. During the operation, an intact LNG-IUS with a tail wire was found near the left uterosacral ligament (Figure 2), without adhesion to the surrounding tissues. After thorough examination, no rupture was found in the uterus. A 3 cm diameter cyst with clear fluid inside was found in the left ovary and was removed. A new LNG-IUS was inserted in the uterine cavity.
The patient was discharged after recovery. Postoperative pathology showed that the left ovarian cyst was a follicular cyst.
The LNG-IUS is an effective intrauterine progesterone release system, which is widely used in contraception, menorrhagia, dysmenorrhea and to prevent endometrial hyperplasia during estrogen supplementation[2]. The LNG-IUS is also a radiopaque T-shaped device, approved for up to 5 years of use.
The adverse effects of IUDs include pelvic pain, heavy menstrual bleeding, dysmenorrhea, infection and malposition. IUD malposition, with a rate ranging from 10.4% to 25%, is described as expulsion, embedding, displacement and perforation[2]. Malposition often occurs with abnormal bleeding and pain, but may also be asymptomatic. Perforation is an IUD that penetrates through both the myometrium and the serosa.
The overall perforation rate is 2.1 per 1000 insertions for LNG-IUS users and 1.6 per 1000 insertions for copper-IUD users[3]. Perforation is more often seen in inexperienced operators and after early postpartum placement[4]. Malposition is more common in the condition of retroflexed uterine positions (7.6% vs 1.8%). Multivariable logistic regression has revealed that the anterior midline position and absence of uterine anomalies are factors associated with a lower incidence of IUD malposition[5]. The repositioned uterus may be a potential cause of uterine perforation upon insertion of the device. Therefore, doctors should take care in these cases.
Ultrasonography serves as the first-line imaging method to evaluate position of IUD in patients presenting with abnormal bleeding, pelvic pain, or absent retrieval strings[6]. If an IUD is not detected on initial ultrasonography, further abdominal radiographs are recommended to locate the IUD[7]. Cross-sectional imaging can provide clues and strategies for surgical planning, as well as to evaluate potential complications such as abscess formation or bowel injury.
Surgical removal of IUDs is the main treatment strategy. In a previous report, laparoscopic surgeries to remove perforated IUDs were successfully achieved in 64.2% of cases (115/179)[8]. However 22.5% (27/120) of laparoscopic surgeries were converted to trans-abdominal operations in another report, and an overall rate of open surgery was 27.9%[9]. The most common location of malpositioned IUDs include the omentum and around the uterus[8]. Intra-abdominal adhesions are more common in the copper-IUD group than LNG-IUS group (58% vs 20%)[8].
This case report shows that during placement of an IUD, uterine position should be confirmed by gynecological examination before surgery, and the operation should be performed with care. When the operation is difficult, ultrasound monitoring is recommended to reduce the risk of IUD perforation. Postoperative imaging is recommended to detect potential risks as soon as possible.
We thank the patient for the consent to publish this case report.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Obstetrics and gynecology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hegazy AA, Egypt; Shelat VG, Singapore S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Hegazy RA, Hegazy AA, Etman WM. Bilateral Tubo-ovarian actinomycosis in perimenopausal woman with neglected intrauterine device: A case report and review of literature. J Medical Case Repo. 2021;3:1-5. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Evans AT, Szlachetka K, Thornburg LL. Ultrasound Assessment of the Intrauterine Device. Obstet Gynecol Clin North Am. 2019;46:661-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Barnett C, Moehner S, Do Minh T, Heinemann K. Perforation risk and intra-uterine devices: results of the EURAS-IUD 5-year extension study. Eur J Contracept Reprod Health Care. 2017;22:424-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 4. | Cole M, Thomas S, Mercer BM, Arora KS. Impact of training level on postplacental levonorgestrel 52 mg intrauterine device expulsion. Contraception. 2019;99:94-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Gerkowicz SA, Fiorentino DG, Kovacs AP, Arheart KL, Verma U. Uterine structural abnormality and intrauterine device malposition: analysis of ultrasonographic and demographic variables of 517 patients. Am J Obstet Gynecol. 2019;220:183.e1-183.e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Connolly CT, Fox NS. Incidence and Risk Factors for a Malpositioned Intrauterine Device Detected on Three-Dimensional Ultrasound Within Eight Weeks of Placement. J Ultrasound Med. 2022;41:1525-1536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Kaislasuo J, Suhonen S, Gissler M, Lähteenmäki P, Heikinheimo O. Uterine perforation caused by intrauterine devices: clinical course and treatment. Hum Reprod. 2013;28:1546-1551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 8. | Gill RS, Mok D, Hudson M, Shi X, Birch DW, Karmali S. Laparoscopic removal of an intra-abdominal intrauterine device: case and systematic review. Contraception. 2012;85:15-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 9. | Mosley FR, Shahi N, Kurer MA. Elective surgical removal of migrated intrauterine contraceptive devices from within the peritoneal cavity: a comparison between open and laparoscopic removal. JSLS. 2012;16:236-241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |