Published online Jan 6, 2023. doi: 10.12998/wjcc.v11.i1.164
Peer-review started: September 4, 2022
First decision: December 13, 2022
Revised: December 15, 2022
Accepted: December 21, 2022
Article in press: December 21, 2022
Published online: January 6, 2023
Processing time: 120 Days and 13.7 Hours
Thymic lipofibroadenomas are extremely rare. In this study, we investigated the clinicopathological characteristics of thymic lipofibroadenomas.
This study included three patients with thymic lipofibroadenomas. We retrospectively analyzed the patient data to determine the clinicopathological characteristics of thymic lipofibroadenomas. The study included one man and two women [mean age, 43 (33–59) years]. All patients were non-smokers and presented with well-defined anterior mediastinal tumors. The cut surfaces of the tumors were solid, with a mixture of yellow and white areas. Microscopic evaluation of resected specimens showed scattered cord-like structures of epithelial cells embedded within abundant fibrotic and hyaline stroma admixed with variable quantities of adipose tissue. One patient showed hyperplastic thymic tissue in a part of the tumor.
Thymic lipofibroadenomas are an extremely rare type of benign thymic tumor. Surgical removal of lipofibroadenomas is usually curative.
Core Tip: Thymic lipofibroadenomas are an extremely rare variety of benign thymic tumors. Morphological and immunohistochemical features can be useful in diagnosing thymic lipofibroadenomas. Surgical removal of lipofibroadenomas is usually curative.
- Citation: Yang MQ, Wang ZQ, Chen LQ, Gao SM, Fu XN, Zhang HN, Zhang KX, Xu HT. Thymic lipofibroadenomas: Three case reports. World J Clin Cases 2023; 11(1): 164-171
- URL: https://www.wjgnet.com/2307-8960/full/v11/i1/164.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i1.164
A thymic lipofibroadenoma is a rare benign anterior mediastinal tumor. This lesion has been classified as “rare thymomas” by the World Health Organization (WHO) classification[1]. The tumor is usually well circumscribed and morphologically resembles a breast fibroadenoma[1,2]. Previous studies have reported no more than 10 cases of lipofibroadenomas[2-4]. Whether this lesion is a neoplasm or a hamartoma remains controversial[1,2]. Furthermore, the etiopathogenesis of thymic fibroadenoma is unclear because of its rarity. Here, we report three cases of thymic lipofibroadenomas and summarize the clinicopathological features of this tumor.
Case 1: A 59-year-old non-smoker woman underwent chest computed tomography (CT) for the evaluation of occasional chest tightness at another hospital 2 wk prior to presentation. She was admitted to our hospital for further treatment.
Case 2: A 33-year-old non-smoker woman was incidentally diagnosed with a mediastinal mass on physical examination 8 mo prior to presentation.
Case 3: A 37-year-old non-smoker man developed mild dyspnea 5 mo prior to presentation and underwent chest CT at another hospital. CT revealed an anterior mediastinal mass, and the patient was admitted to our hospital for surgical treatment.
Case 1: The patient felt chest tightness occasionally for 2 wk.
Case 2: The patient was asymptomatic and was diagnosed incidentally during routine medical examination.
Case 3: The patient had mild dyspnea for 5 mo.
None of the three patients had any significant past medical history.
Personal and family history, medication history, social history, and allergic history of all three patients were non-contributory.
Physical examination of all three patients showed no abnormality.
Laboratory analyses of samples from all three patients did not reveal any abnormal test results.
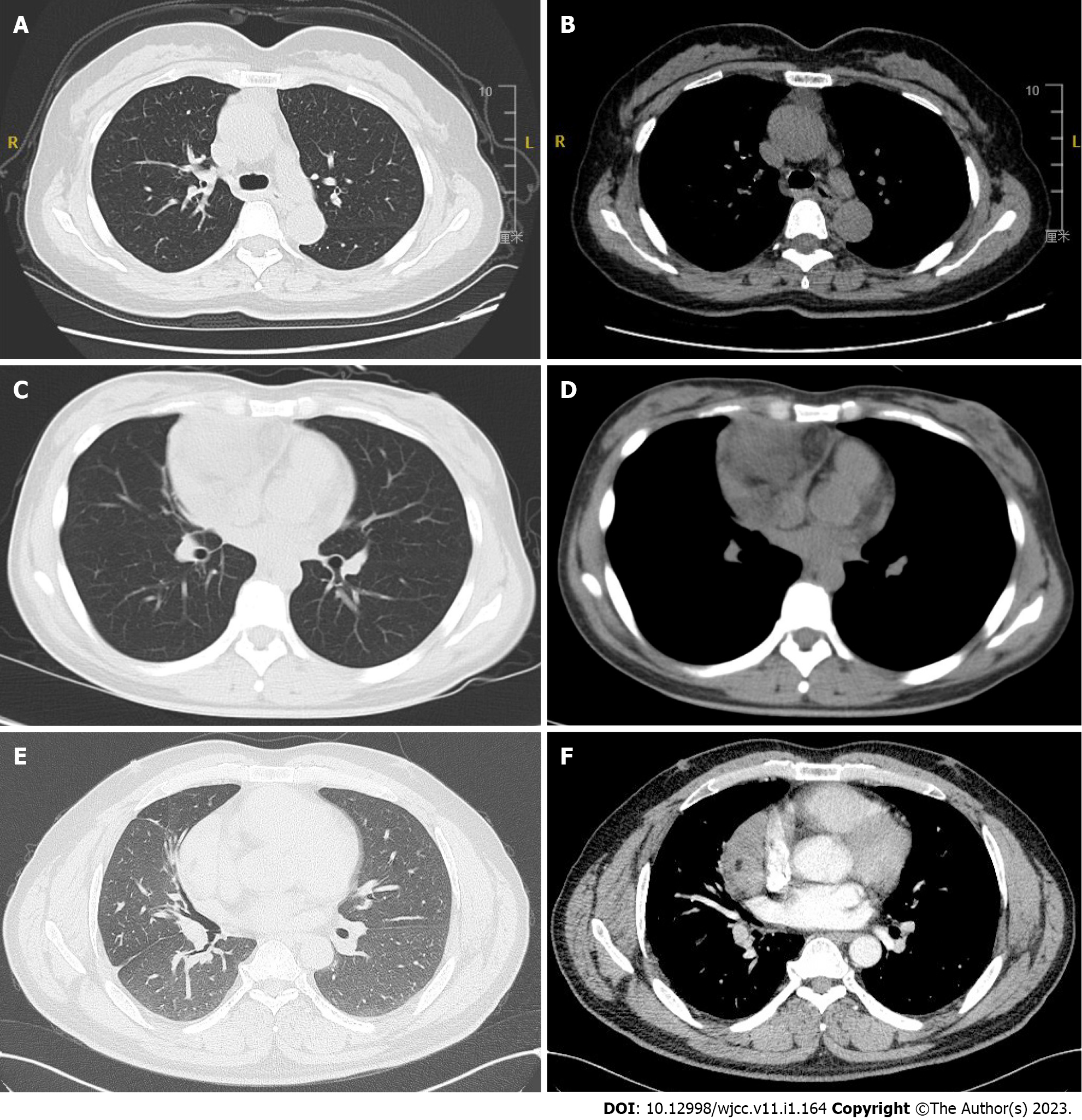
Case 1: CT evaluation revealed an anterior mediastinal mass. Repeat CT revealed an anterior mediastinal shadow (approximately 3.9 cm × 1.8 cm in size) with clear boundaries, no bilateral hilar enlargement, no mediastinal shift, and no lymphadenopathy. The patient’s heart size was acceptable and the soft tissues of the chest wall showed no abnormalities (Figure 1A and B).
Case 2: CT revealed an irregular anterior upper mediastinal shadow (approximately 7.1 cm × 7.5 cm in size), with clear boundaries, protruding into the right lung. The mass showed uneven internal density, and a fat density shadow was observed within it. The lesion was not well-demarcated from the adjacent large blood vessels and cardiac structures (Figure 1C and D).
Case 3: Chest CT revealed a mass (approximately 9.9 cm × 9.8 cm × 4.9 cm in size) beside the anterior mid mediastinum, with a capsule and spot-like calcifications in addition to small, patchy low-density shadows (Figure 1E and F).
Thymic lipofibroadenoma.
Thymic lipofibroadenoma accompanied by thymic hyperplasia.
Thymic lipofibroadenoma.
We performed thoracoscopic resection of the anterior mediastinal mass and surrounding thymus tissue. Intraoperatively, we detected an oval, noninvasive anterior mediastinal mass (3-4 cm in diameter) in the right lobe of the thymus.
Mediastinal biopsy evaluation suggested “probable thymoma.” Therefore, the patient underwent surgery following a preoperative diagnosis of thymoma. Intraoperatively, we observed a large mass (12 cm × 10 cm × 6 cm) from the hilum to the right of the pericardium. The pink, soft, and smooth mass was well-demarcated from the surrounding tissues. The tumor and the circumambient thymus were completely resected.
We resected the anterior mediastinal mass. Intraoperatively, we detected an anterior mediastinal mass measuring approximately 10 cm in diameter over the upper right side of the heart anteriorly, and extending to the lower right, covering the surface of the heart, with an intact capsule. The mass was completely resected.
All patients had well-circumscribed encapsulated tumors with transparent capsules that were well demarcated from the surrounding tissue. The tumor diameter ranged from 3-12 cm. Yellow greasy areas and solid, grey firm areas were visible on the cut surface. The resected specimens were fixed using 10% neutral-buffered formalin, routinely dehydrated, embedded in paraffin blocks, cut into 4-μm thick sections, and stained with hematoxylin and eosin. Immunohistochemical evaluation was performed using the EnVision two-step immunohistochemical staining method, with negative and positive controls. Ready-to-use selected antibodies, such as broad-spectrum cytokeratin (CK), CK19, P63, epithelial membrane antibody (EMA), terminal deoxynucleotidyl transferase (TdT), CD3, CD5, CD20, and Ki-67, purchased from Fuzhou Maixin Biotechnology Co., Ltd. China, were used in this study. The results were interpreted as positive or negative based on the nuclear, cytoplasmic, or membrane reactivity of the different antibodies used.
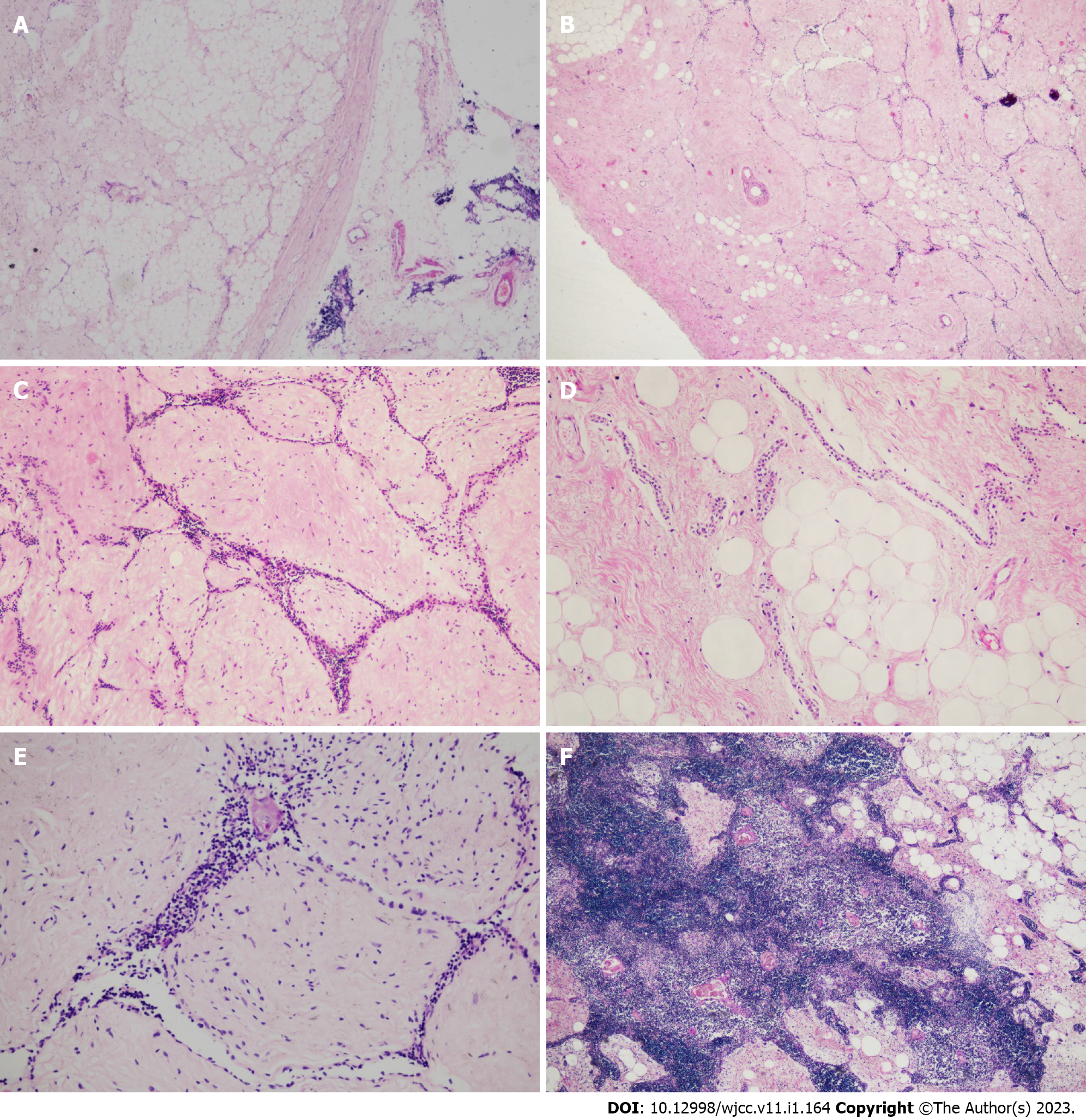
Light microscopy revealed a clear connective tissue capsule between the tumor and the surrounding thymic tissue. The tumor contained fibrotic and hyaline stroma, narrow strands of epithelial cells, and variable quantities of adipose tissue, resembling a breast fibroadenoma. The bland-looking epithelial cells formed narrow cords that were interspersed in the fibrotic and hyaline stroma. Some adipocytes were mixed with fibrotic stroma, and abundant adipose tissue was detected in some areas. A few lymphocytes mixed with epithelial cells, residual Hassall corpuscles, and small calcifications were observed in some regions. Hyperplastic thymic tissue was observed in one part of the tumor (Case 2). Atypia and mitotic figures were not identified in any of the tumor cells (Figure 2).
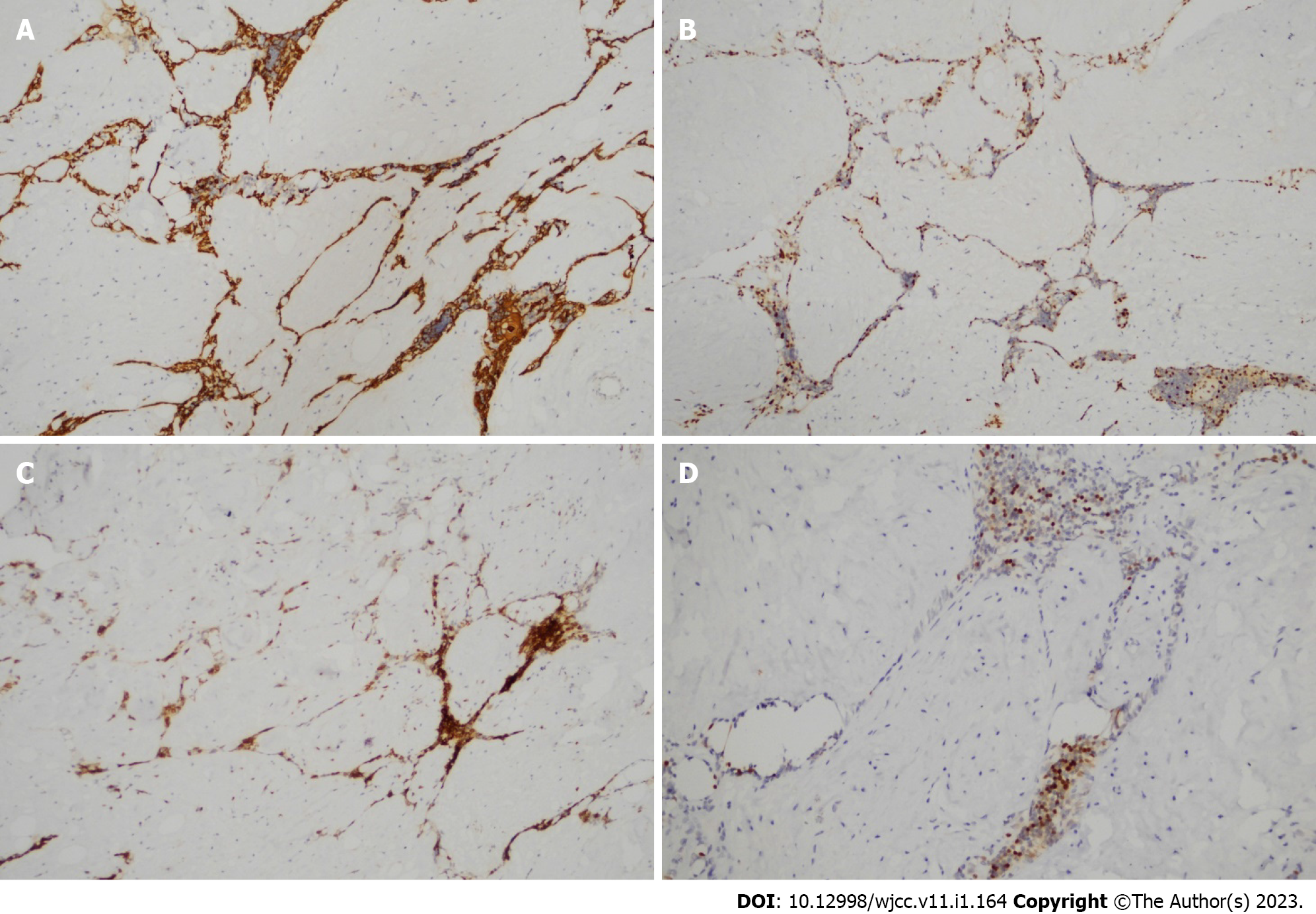
Epithelial cells were immunopositive for broad-spectrum CK, CK19, P63, and EMA. Lymphocytes in the tumor were immunopositive for CD3 and CD5. A few lymphocytes were also immunopositive for TdT (Figure 3), indicating residual thymic tissue.
There was no recurrence 19 mo after operation.
There was no recurrence 7 mo after operation.
There was no recurrence 30 mo after operation.
Thymic lipofibroadenomas are rare benign thymic tumors. Although we have encountered three cases in our work in recent years, thymic lipofibroadenoma is extremely rare. To our knowledge, only 13 cases (including ours) of thymic lipofibroadenomas have been reported in the literature[2-11]. Table 1 summarizes the clinicopathological features of these patients. All patients presented with a well-defined anterior mediastinal tumor. The lesion was detected in seven men and six women aged 9-64 years (mean age, 37 years). The tumor diameter ranged from 3 cm to 23 cm (mean, 10 cm; the diameter was unknown in three cases). All 13 patients underwent surgery alone, and postoperative recurrence occurred in only four cases. The longest postoperative follow-up period was > 6 years and 8 mo[2-11].
| Case | Symptoms | Year | Sex | Age | Size (cm) | Site | Therapy | Outcome |
| 1[5] | Unknown | 1994 | M | 32 | Unknown | Anterior mediastinal | Unknown | |
| 2[5] | Unknown | 1994 | F | 9 | Unknown | Anterior mediastinal | Unknown | |
| 3[6] | Dyspnea,dizziness | 2001 | M | 62 | Unknown | Anterior mediastinal | S | No recurrence more than 6 yr 8 mo after operation |
| 4[7] | Unknown | 2009 | M | 32 | 3 | anterior mediastinal | S | Unknown |
| 5[8] | Chest pain and dyspnea | 2012 | F | 23 | 21 × 7.5 × 7 | Anterior mediastinum | S | No recurrence 1 yr after operation |
| 6[9] | No | 2013 | M | 21 | 10 × 6 × 4 | Left heart edge | S | No recurrence 46 mo after operation |
| 7[10] | Cough, fever, andnight sweats | 2015 | M | 20 | 23 × 14 × 5 | Anterior mediastinum extending throughout theright thorax | S | asymptomatic 6 mo after operation. |
| 8[3] | No | 2020 | M | 28 | 8.8 × 6.7 × 4.2 | Right edge of the heart | S | No recurrence 6 mo after operation |
| 9[2] | Progressive dyspnea | 2021 | F | 64 | 16 × 8 × 6 | Anterior mediastinum and left pleural cavity | S | No recurrence 4 yr after operation |
| 10[4] | No | 2021 | F | 55 | 4.5 × 1.8 × 1.3 | Mediastinal | S | Unknown |
| 11 (Present case) | Occasional chest congestion | 2022 | F | 59 | 3-4 | Anterior mediastinum | S | No recurrence 19 mo after operation |
| 12 (Present case) | No | 2022 | F | 33 | 12 × 10 × 6 | Anterior upper mediastinum | S | No recurrence 7 mo after operation |
| 13 (Present case) | Mild dyspnea | 2022 | M | 37 | 10 | Beside the anterior middle mediastinum | S | No recurrence 30 mo after operation |
Histopathological examination remains the gold standard for diagnosing thymic lipofibroadenomas. Lipofibroadenoma is characterized by a mixture of adipocytic, fibrotic, and thymic epithelial elements with lymphocytic infiltration of epithelial and adipose tissues. Epithelial cells tend to be immunopositive for broad-spectrum CK and CK19. Scattered CD3+ T cells, CD20+ B cells, and a few TdT+ immature lymphocytes have been identified in previous studies. Thymic lipofibroadenomas often mimic other tumors, such as thymolipoma, thymofibrolipoma, sclerosing thymoma, lipoma, and liposarcoma, which show similar histopathological features[1,10]. Thymolipoma is characterized by a predominant adipose tissue component, with or without thymic parenchyma, and the absence of a fibrous component. Thymofibrolipoma is a subtype of thymolipoma with a significant fibrous component. Sclerosing thymomas are distinguished by islands of epithelial tumor cells interspersed within a dense collagenous stroma without intermixed adipose tissue. According to the latest WHO classification, a sclerosing thymoma is considered to represent the sclerosing portion of other common thymomas, and is therefore removed from the classification[1]. Lipomas predominantly contain mature adipose tissues. Liposarcomas are a heterogeneous group of mesenchymal neoplasms with adipocytic differentiation[1]. Therefore, histopathological and immunohistochemical analyses are useful diagnostic tools.
Whether this lesion represents a neoplasm or a hamartoma remains debatable, and the etiopathogenesis of this tumor is unclear owing to its rarity. Complete surgical resection is recommended as a curative therapy.
We report three cases of thymic lipofibroadenoma, a rare type of thymic neoplasm. In addition to creating greater awareness regarding this condition, our report will benefit pathologists and surgeons in the treatment of patients with this clinical presentation. Comprehensive histopathological and immunohistochemical analyses are important for accurate diagnosis and prompt management.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Pathology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hegazy AA, Egypt S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Board WCoTE. Thoracic Tumours WHO Classification of Tumours, 5th Edition, Volume 5. 2021. Available from: https://publications.iarc.fr/595. |
| 2. | Bolca C, Has A, Bobocea A, Afetelor A, Stoica R, Strambu I, Stoicescu I, Magheran E, Balescu I, Bacalbasa N, Gherghiceanu F, Furtunescu F, Radavoi D, Diaconu C, Paleru C, Cordos I. A Rare Thymic Tumor - Lipofibroadenoma - Always a Postoperative Surprise. In Vivo. 2021;35:3623-3626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Kurebayashi Y, Hayashi Y, Emoto K, Kaseda K, Asamura H, Mukai K, Sakamoto M. Lipofibroadenoma arising in hyperplastic thymic tissue: Possible perivascular origin of lipofibroadenoma. Pathol Int. 2021;71:275-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 4. | Hakiri S, Kawaguchi K, Tateyama H, Fukui T, Nakamura S, Ozeki N, Mori S, Chen-Yoshikawa TF. Thymic lipofibroadenoma accompanied with largish calcifications. Gen Thorac Cardiovasc Surg. 2021;69:394-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 5. | Moran CA, Zeren H, Koss MN. Thymofibrolipoma. A histologic variant of thymolipoma. Arch Pathol Lab Med. 1994;118:281-282. [PubMed] |
| 6. | Kuo T, Shih LY. Histologic types of thymoma associated with pure red cell aplasia: a study of five cases including a composite tumor of organoid thymoma associated with an unusual lipofibroadenoma. Int J Surg Pathol. 2001;9:29-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Onuki T, Iguchi K, Inagaki M, Suzuki K. [Lipofibroadenoma of the thymus]. Kyobu Geka. 2009;62:395-398. [PubMed] |
| 8. | Aydin Y, Sipal S, Celik M, Araz O, Ulas AB, Alper F, Eroglu A. A rare thymoma type presenting as a giant intrathoracic tumor: lipofibroadenoma. Eurasian J Med. 2012;44:176-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Qu G, Yu G, Zhang Q, Ma J, Wang X. Lipofibroadenoma of the thymus: a case report. Diagn Pathol. 2013;8:117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Makdisi G, Roden AC, Shen KR. Successful Resection of Giant Mediastinal Lipofibroadenoma of the Thymus by Video-Assisted Thoracoscopic Surgery. Ann Thorac Surg. 2015;100:698-700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Hui M, Paul TR, Uppin SG, Jyothi N. Lipofibroadenoma with B1 thymoma: A case report of a rare thymic tumor. Indian J Pathol Microbiol. 2018;61:630-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |