Published online Mar 26, 2022. doi: 10.12998/wjcc.v10.i9.2948
Peer-review started: October 11, 2021
First decision: December 10, 2021
Revised: January 4, 2022
Accepted: February 20, 2022
Article in press: February 20, 2022
Published online: March 26, 2022
Processing time: 162 Days and 3.6 Hours
Hemifacial microsomia (HFM) is a rare congenital malformation characterized by a combination of various anomalies, including the face, ears, eyes, and vertebrae. Prenatal diagnosis for HFM is possible, and quite accurate ultrasound can detect obvious defects. The etiology is still unknown, although some hypotheses have been proposed, including gene mutation, chromosome anomaly, and environmental risk factors. However, there are few reports of pulmonary hypoplasia and dextrocardia in HFM.
A 2-year-old boy presented to the ear reconstruction department of our hospital complaining of deviation of the face to the right side and auricular anomaly. Physical examination revealed facial asymmetry, preauricular skin tags, and concha-type microtia with stricture of the external auditory canal on the right side. Head magnetic resonance imaging showed bilateral semicircular canal dysplasia and bilateral internal auditory canals stenosis. Audiometric examination showed bilateral severe sensorineural hearing loss. Chest radiography and computed tomography showed dextrocardia and right pulmonary hypoplasia.
This case presented a rare finding and an unusual association of 3 malformations, ipsilateral HFM, pulmonary agenesis, and dextrocardia.
Core Tip: Hemifacial microsomia (HFM) is a rare congenital malformation characterized by a combination of various anomalies including face, ears, eyes, and vertebrae. We present a rare case of ipsilateral HFM with dextrocardia and pulmonary hypoplasia. Those malformations may compose a laterality syndrome or just an extension of an expanded spectrum of HFM.
- Citation: Guo R, Chang SH, Wang BQ, Zhang QG. Ipsilateral hemifacial microsomia with dextrocardia and pulmonary hypoplasia: A case report . World J Clin Cases 2022; 10(9): 2948-2953
- URL: https://www.wjgnet.com/2307-8960/full/v10/i9/2948.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i9.2948
Hemifacial microsomia (HFM) is a rare multi-system congenital malformation caused by hypoplasia of the first and second branchial arches[1]. The incidence reported ranges from 1/3500 to 1/5600 live births[2]. It is characterized by dysplasia of the mandible and auricle, resulting in facial asymmetry[3]. Other terms used for the description are craniofacial microsomia, oculoauriculovertebral spectrum, and goldenhar syndrome[1]. The anomalies associated with HFM include craniofacial and extracranial manifestations, such as microtia, facial asymmetry, cardiac malformations. No specific genes are associated with this syndrome, although chromosomal anomalies have been observed, such as del (22q), dup (22q) and trisomy 22[1]. Previous studies have also found that environmental factors are relevant, such as the use of retinoic acid during pregnancy, gestational diabetes mellitus, and multiple gestations[2]. In developmental biology, the branchial arches related to auricular development are evident in the 5th week of pregnancy, the respiratory system develops from the foregut at 4-7 wk of pregnancy, and the heart is the earliest organ formed during embryonic development[4,5]. Previous studies have proved that partial heart and auricle derived from neural crest cells (NCCs) and disturbance with their growth and migration can lead to microtia and cardiac anomalies[6]. Co-occurrence of malformations of the lungs, heart and auricle indicates a disturbance at the same stage of embryonic development.
Here, we describe a case of ipsilateral HFM with dextrocardia and pulmonary hypoplasia, and also conducted a literature review to have a comprehensive understanding of this syndrome. Pulmonary hypoplasia with dextrocardia in HFM has not been reported before in China. The present case adds to the variable clinical presentation of HFM and suggests a new association.
A 2-year-old Chinese boy, born to nonconsanguineous parents, presented to plastic surgery hospital with complaints of face deviation to the right side and abnormal appearance of the right ear.
After birth, an abnormal appearance of the right ear and facial asymmetry was found in this child. The facial deviation gradually aggravated over time.
Because the patients lived in a rural area and lacked medical knowledge, they did not have a regular prenatal examination, such as ultrasound. The patient’s birth history was uneventful, and there was no family history of congenital malformations or mental retardation. Developmental milestones were normal. The child also had a bilateral hearing impairment and speech retardation.
Physical examination revealed facial asymmetry (face and mouth deviated to the right side), preauricular skin tags, and concha-type microtia with stricture of the external auditory canal on the right side (Figure 1). During chest auscultation, no breath sounds could be heard on the right hemithorax, but normal heart sounds could be heard. The other examinations were unremarkable.
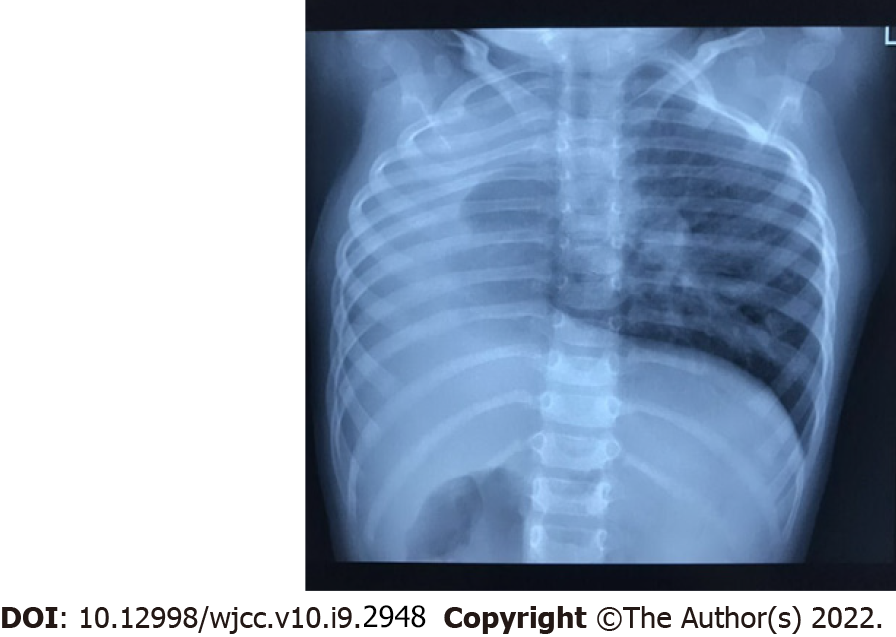
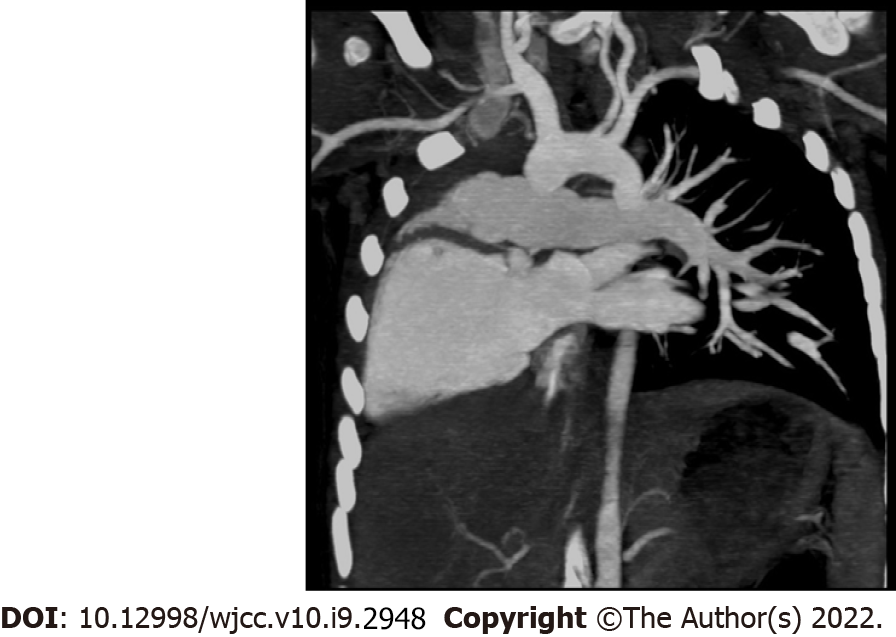
Head magnetic resonance imaging showed bilateral semicircular canal dysplasia and bilateral internal auditory canals stenosis. Chest radiography showed dextrocardia and single left lung (Figure 2), and chest computed tomography confirmed that the thoracic aorta was located on the right front side of the thoracic vertebrae, right pulmonary hypoplasia, and the left pulmonary artery arose directly from the right ventricle (Figure 3). Echocardiography also showed situs solitus, dextrocardia, ectopic origin of the left pulmonary artery, and moderate regurgitation of mitral, tricuspid, and aortic valves. Audiometric examination showed bilateral severe sensorineural hearing loss.
Ipsilateral HFM with dextrocardia and pulmonary hypoplasia.
The patient was too young to receive surgical treatment for auricular malformation, so we only provided diagnosis and consultation in the outpatient department. We suggested the parents feed the child scientifically, provide diversified and nutritious foods (cereals, fish, meat, vegetables and fruits,
Periodic follow-ups were conducted every 6 mo to monitor progress of the deformity. The patient’s condition was stable during the 10 months’ follow-up.
HFM is a heterogeneous, multifactorial congenital disease. Its diagnosis is mainly clinical, while radiographic examinations help to support the clinical diagnosis. Prenatal diagnosis is possible, and accurate ultrasound can detect obvious defects. From a developmental perspective, the involved mandible and ear that embryologically originated from the first and second branchial arches suggest that this condition may be due to the maldevelopment of these branchial arches during the 1th week of gestation. The vascular disruption theory and the NCCs disturbance theory are pathogenetic hypotheses that might explain the malformations correlated with HFM[7]. Primitive lungs generally form in the 4th week of pregnancy. At this time, pulmonary hypoplasia may occur, accompanied by other ipsilateral congenital anomalies, such as cardiovascular system, gastrointestinal system, central nervous system, and musculoskeletal system[8]. As a rare congenital anomaly, right pulmonary hypoplasia can lead to secondary dextrocardia in situs solitus in scimitar syndrome[9]. The heart is the earliest organ formed during embryonic development. Cardiac malformations with pulmonary hypoplasia include Ebstein’s anomaly, tetralogy of Fallot, pulmonary stenosis, and right heart dysplasia[10,11]. Previous studies have found that pulmonary hypoplasia and cardiovascular anomalies are most commonly associated with minor auricle deformity, while this patient suffered from concha-type microtia[12,13].
A comprehensive search of PubMed and Embase was performed to identify studies using MeSH terms and keywords “HFM” or “oculo-auriculo-vertebral syndrome” or “Goldenhar Syndrome” or “microtia”. Only thred cases[14-16] of HFM combined with pulmonary hypoplasia and dextrocardia were retrieved and reviewed (Table 1). Two patients were male with an ipsilateral malformation (right-side involvement), and one case was female with left HFM. Our patient was also male and had a right-side involvement. Male and right-side predominance has been observed in HFM. One hypothesis is the establishment of left-right asymmetry before organogenesis, resulting in subtle differences in the morphology of the left and right sides of the embryo. In rat embryos, the right-side predominance may be related to the observation of delayed maturation of the right mitochondria, resulting in decreased energy reserves and increased tissue damage during hypoxia[14]. In addition, male sex hormones might reduce the mitochondrial respiration rate and increase the sensitivity to chemical hypoxia[17]. Previous studies have confirmed that some genes are expressed differently on both sides of developing vertebrate embryos, leading to differential susceptibility of specific bilateral structures to teratogens during organogenesis. Furthermore, some human genes related to laterality are located on sex chromosomes, indicating a high correlation between male sex and laterality patterns[17].
| Clinical features | This study | Maymon et al[14] (2001) | Fan et al[15] (2015) | Chaudhary et al[16] (2017) |
| Sex | M | M | M | F |
| Age of examination | 2 yr | 20 wk gestation | 3 yr | 7 yr |
| Microtia | ||||
| Side | R | R | R | L |
| Type | Concha-type | Lobule-type | Concha-type | Concha-type |
| EAM stenotic/atresia | + | NA | + | - |
| Facial asymmetry | + | NA | + | + |
| Preauricular tags | + | + | - | + |
| Macromastia | - | NA | - | + |
| Hearing impairment | + | NA | + | - |
| Epibulbar dermoid | - | NA | - | + |
| Pulmonary hypoplasia | ||||
| Side | R | R | R | R |
| Cardiovascular anomalies | ||||
| Atrial septal defect | - | - | + | - |
| Dextrocardia | + | + | + | + |
| Heart valve disease | + | - | - | + |
| Others | Ectopic origin of left pulmonary artery | Main pulmonary artery dilated | Hepatic vein drainage directly into right atrium | Pulmonary stenosis |
| Inguinal hernia | - | NA | + | - |
| Treatment | NA | Termination of the pregnancy | Indirect inguinal hernia repair + Repair of atrial septal defect | NA |
The contribution of the present case report lies in discovering a rare finding and an unusual association of 3 malformations: (1) Ipsilateral HFM; (2) pulmonary agenesis; and (3) dextrocardia. Those malformations may compose a laterality syndrome or an extension of an expanded spectrum of HFM. The etiology and epidemiology of pulmonary and cardiovascular anomalies in HFM are still unclear and demand a further investigation to explore relevant pathogenic mechanisms.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Otorhinolaryngology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Abubakar MS, Cristaldi PMF, Di Meglio L S-Editor: Guo XR L-Editor: Kerr C P-Editor: Guo XR
| 1. | Cohen N, Cohen E, Gaiero A, Zecca S, Fichera G, Baldi F, Giordanetto JF, Mercier JM, Cohen A. Maxillofacial features and systemic malformations in expanded spectrum Hemifacial Microsomia. Am J Med Genet A. 2017;173:1208-1218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 2. | Zhao S, Sun P, Li X, Xu X, Peng Q, Shu K, Ma L, Liang Y, Liu B, Zhang Z. Identification of Hub Genes in Hemifacial Microsomia: Evidence From Bioinformatic Analysis. J Craniofac Surg. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Berker N, Acaroğlu G, Soykan E. Goldenhar's Syndrome (oculo-auriculo-vertebral dysplasia) with congenital facial nerve palsy. Yonsei Med J. 2004;45:157-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Cox TC, Camci ED, Vora S, Luquetti DV, Turner EE. The genetics of auricular development and malformation: new findings in model systems driving future directions for microtia research. Eur J Med Genet. 2014;57:394-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 74] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 5. | Schittny JC. Development of the lung. Cell Tissue Res. 2017;367:427-444. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 279] [Cited by in RCA: 428] [Article Influence: 53.5] [Reference Citation Analysis (0)] |
| 6. | Minoux M, Rijli FM. Molecular mechanisms of cranial neural crest cell migration and patterning in craniofacial development. Development. 2010;137:2605-2621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 323] [Cited by in RCA: 329] [Article Influence: 21.9] [Reference Citation Analysis (0)] |
| 7. | Luquetti DV, Heike CL, Hing AV, Cunningham ML, Cox TC. Microtia: epidemiology and genetics. Am J Med Genet A. 2012;158A:124-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 287] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 8. | Festa P, Lamia AA, Murzi B, Bini MR. Tetralogy of fallot with left heart hypoplasia, total anomalous pulmonary venous return, and right lung hypoplasia: role of magnetic resonance imaging. Pediatr Cardiol. 2005;26:467-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Jue KL, Amplatz K, Adams P Jr, Anderson RC. Anomalies of great vessels associated with lung hypoplasia. The scimitar syndrome. Am J Dis Child. 1966;111:35-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 43] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Cunningham ML, Mann N. Pulmonary agenesis: a predictor of ipsilateral malformations. Am J Med Genet. 1997;70:391-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Ahamed MF, Al Hameed F. Hypogenetic lung syndrome in an adolescent: imaging findings with short review. Ann Thorac Med. 2008;3:60-63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Zhang Y, Jiang H, Yang Q, He L, Yu X, Huang X, Wu R, Yang M, Li C, Pan B. Microtia in a Chinese Specialty Clinic Population: Clinical Heterogeneity and Associated Congenital Anomalies. Plast Reconstr Surg. 2018;142:892e-903e. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 13. | Huang X, Chen W, Wang C, Lin L, Yang Q, Pan B, Jiang H. Evaluation of respiratory system anomalies associated with microtia in a Chinese specialty clinic population. Int J Pediatr Otorhinolaryngol. 2021;146:110762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (1)] |
| 14. | Maymon R, Schneider D, Hegesh J, Herman A, Weinraub Z, Achiron R. Antenatal sonographic findings of right pulmonary agenesis with ipsilateral microtia: a possible new laterality association. Prenat Diagn. 2001;21:125-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 15. | Fan C, Huang C, Liu J, Yang J. A Child with Lung Hypoplasia, Congenital Heart Disease, Hemifacial Microsomia, and Inguinal Hernia: Ipsilateral Congenital Malformations. Case Rep Pediatr. 2015;2015:741540. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Chaudhary N, Shrestha S, Halwai HK. Goldenhar Syndrome with Dextrocardia and Right Pulmonary Hypoplasia: An Unusual Association. Case Rep Genet. 2017;2017:2625030. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Paulozzi LJ, Lary JM. Laterality patterns in infants with external birth defects. Teratology. 1999;60:265-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |