Published online Mar 26, 2022. doi: 10.12998/wjcc.v10.i9.2883
Peer-review started: September 20, 2021
First decision: October 25, 2021
Revised: October 29, 2021
Accepted: February 12, 2022
Article in press: February 12, 2022
Published online: March 26, 2022
Processing time: 182 Days and 21.5 Hours
Disc herniation refers to the displacement of disc material beyond its anatomical space. Disc sequestration is defined as migration of the herniated disc fragment into the epidural space, completely separating it from the parent disc. The fragment can move in upward, inferior, and lateral directions, which often causes low back pain and discomfort, abnormal sensation, and movement of lower limbs. The free disc fragments detached from the parent disc often mimic spinal tumors. Tumor like lumbar disc herniation can cause clinical symptoms similar to spinal tumors, such as lumbar soreness, pain, numbness and weakness of lower limbs, radiation pain of lower limbs, etc. It is usually necessary to diagnose the disease according to the doctor's clinical experience, and make preliminary diagnosis and differential diagnosis with the help of magnetic resonance imaging (MRI) and contrast-enhanced MRI. However, pathological examination is the gold standard that distinguishes tumoral from non-tumoral status. We report four cases of disc herniation mimicking a tumor, and all the pathological results were intervertebral disc tissue.
The first case was a 71-year-old man with low back pain accompanied by left lower extremity radiating pain for 1 year, with exacerbation over the last 2 wk. After admission, MRI revealed a circular T2-hypointense lesion in the spinal canal of the L4 vertebral segment, with enhancement on contrast-enhanced MRI suggesting neurilemmoma. The second case was a 74-year-old man with pain in both knees associated with movement limitation for 3 years, with exacerbation over the last 3 mo. MRI revealed an oval T2-hyperintense lesion in the spinal canal at the L4–5 level, with obvious peripheral enhancement on contrast-enhanced MRI. Thus, neurilemmoma was suspected. The third case was a 53-year-old man who presented with numbness and weakness of the lumbar spine and right lower extremity for 2 wk. MRI revealed a round T2-hyperintense lesion in the spinal canal at the L4–5 level, with obvious rim enhancement on contrast-enhanced MRI. Thus, a spinal tumor was suspected. The fourth case was a 75-year-old man with right lower extremity pain for 2 wk, with exacerbation over the last week. MRI revealed a round T1-isointense lesion in the spinal canal of the L3 vertebral segment and a T2-hyperintense signal from the lesion. There was no obvious enhancement on contrast-enhanced MRI, so a spinal tumor was suspected. All four patients underwent surgery and recovered to ASIA grade E on postoperative days 5, 8, 8, and 6, respectively. All patients had an uneventful postoperative course and fully recovered within 3 mo.
Disc herniation mimicking a tumor is a relatively rare clinical entity and can be easily misdiagnosed as a spinal tumor. Examinations and tests should be improved preoperatively. Patients should undergo comprehensive preoperative evaluations, and the lesions should be removed surgically and confirmed by pathological diagnosis.
Core Tip: Lumbar disc herniation is a common condition in orthopedics. It is defined as displacement of disc material beyond its anatomical space and the formation of an isolated disc when the herniated disc is detached from the parent disc. Disc sequestration refers to migration of a herniated disc fragment into the epidural space with complete separation from the parent disc. Here, we report four cases of disc sequestration mimicking a spinal tumor. All of the patients underwent surgery, and the postoperative pathology showed intervertebral disc tissue. All four cases had an uneventful postoperative course and recovered completely within 3 mo.
- Citation: Li ST, Zhang T, Shi XW, Liu H, Yang CW, Zhen P, Li SK. Lumbar disc sequestration mimicking a tumor: Report of four cases and a literature review. World J Clin Cases 2022; 10(9): 2883-2894
- URL: https://www.wjgnet.com/2307-8960/full/v10/i9/2883.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i9.2883
Lumbar disc herniation is a common condition in orthopedics defined as the displacement of disc material beyond its anatomical space, and the formation of an isolated disc when the herniated disc is detached from the parent disc. Disc sequestration refers to the migration of herniated disc fragments into the epidural space; most disc fragments move in a lateral, cephalic, or caudal direction due to the anatomical structure of the anterior epidural space, and can be easily misdiagnosed as spinal tumors[1,2]. In rare cases, fragments may migrate dorsally into the posterior epidural space or be located intradurally. The lumbar spine is the most commonly affected region, but the cervical and thoracic spine can also be affected. Here, we report four cases of disc sequestration mimicking a spinal tumor and review the literature to provide insight into discriminating between a herniated disc and spinal tumor. All four cases underwent surgery, and the postoperative pathology showed intervertebral disc tissue. All four cases had an uneventful postoperative course and recovered completely within 3 mo[3].
Case 1: A 71-year-old man was admitted for low back pain with left lower extremity radiating pain for 1 year, with exacerbation over the past 2 wk.
Case 2: A 74-year-old man was admitted for pain in both knees and movement limitation for 3 years, with exacerbation over the past 3 mo.
Case 3: A 53-year-old man was admitted for numbness and weakness of the lumbar spine and right lower extremity for 2 wk.
Case 4: A 75-year-old man was admitted for pain in the right lower extremity for 2 wk, with exacerbation over the last week.
Case 1: The patient had low back pain with left lower extremity radiating pain for 1 year. After intermittent acupuncture treatment, the symptoms were slightly relieved, but the symptoms were exacerbated by physical work performed 2 wk ago. There was no numbness or weakness in either lower extremity, and defecation and urinary functions were normal.
Case 2: The patient had pain in both knees with limited movement for 3 years, which was not significantly improved after intake of oral painkillers and intra-articular injection of sodium hyaluronate. The symptoms had been more severe for nearly 3 mo. Defecation and urinary functions were normal.
Case 3: The patient had numbness and weakness of the lower back and right lower extremity for 2 wk. The sites of numbness of the right lower extremity were mainly the right hip, back of the thigh, and back of the lower leg, accompanied by an obvious limitation of movement. Walking 50 m required intermittent squatting, which relieved the symptoms. Physical therapy such as massage had a poor effect. Defecation and urinary functions were normal.
Case 4: There was no obvious trigger for right lower extremity pain in this patient. There was obvious pain in the anterolateral thigh and knee joint of the right lower extremity, but this was not accompanied by lumbar pain or limited movement of either lower extremity. The patient had not undergone any treatment. The symptoms became more severe 1 wk ago, so a painkiller was administered at a local hospital. The symptoms were not significantly relieved, so he was transferred to our hospital.
None of the four patients had a previous history of diseases.
None of the patients had any relevant personal or family history.
Case 1: Flexion and extension movements of the lumbar spine were slightly restricted, and there was mild tenderness over the L3–4, L4–5, and L5–S1 interspinous spaces. The muscle tone of both lower limbs was normal, the strength of the left gluteus maximus and iliopsoas muscles was grade IV, and the strength of the remaining muscles was normal. In the leg raising test, it was positive (50°) on the left lower limb. Knee and ankle reflexes were reduced bilaterally, but there were no pathological reflexes.
Case 2: Limping gait was present, and lumbar flexion and extension were slightly limited. Tenderness of the L4–5 spinous process and interspinous space was detected. Muscle strength and muscle tension were normal in both lower limbs. And the bilateral straight leg raising test was normal. The bilateral knee reflex was normal, but the bilateral ankle reflex was weak. There were no pathological reflexes.
Case 3: Limping gait was present, lumbar flexion and extension were significantly limited, and the L4–5 and L5–S1 spinous processes and interspinous space were tender. Muscle tension in the lower limbs was normal. Muscle strength of the right lower limb was grade IV. The skin sensation of the right hip, posterolateral thigh, and lateral leg was decreased, while muscle strength and skin sensation of the left lower limb were normal. The bilateral straight leg raising test was normal. The left knee and ankle reflexes were weak, but were normal on the right side. There were no pathological reflexes.
Case 4: Limping gait was present, and lumbar flexion and extension were limited, but muscle tension of both lower limbs was normal. Except for the iliopsoas muscle (grade III strength), the other muscles of the right lower limb were grade IV, and the muscle strength of the left lower limb was normal. The leg raising test was positive (60°). The right knee reflex was weak, and the bilateral Babinski sign was positive.
All parameters in all four cases, including but not limited to complete blood count, renal and liver function tests, prostate-specific antigen, and other specific tumor markers, were within the normal ranges.
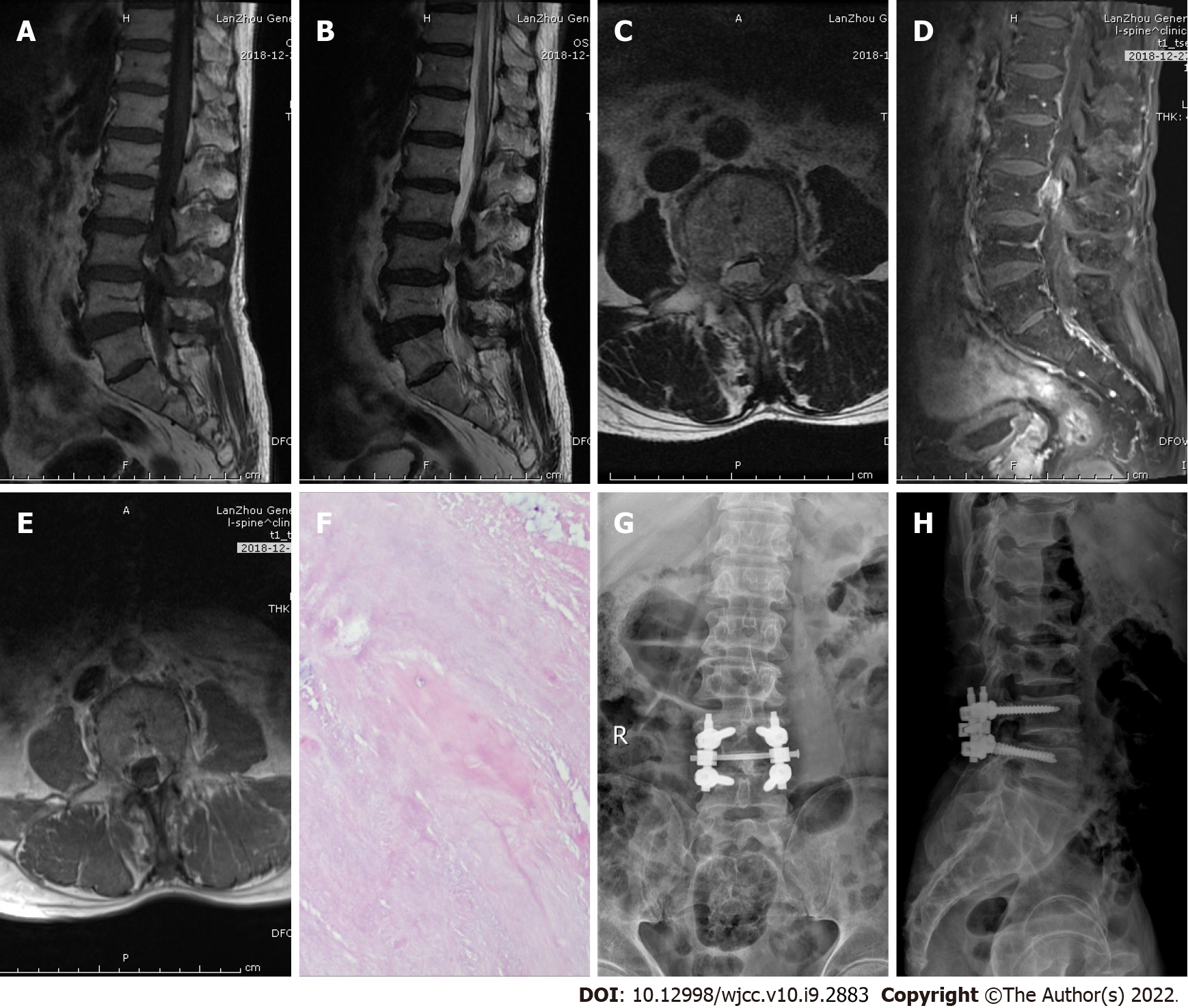
Case 1: After admission, magnetic resonance imaging (MRI) showed an abnormal shadow in the spinal canal of the L4 vertebral segment and compression of the dural sac. T1-weighted images showed high signal intensity, while T2-weighted images showed low signal intensity, with heterogeneous enhancement on contrast-enhanced MRI (Figure 1A-1E).
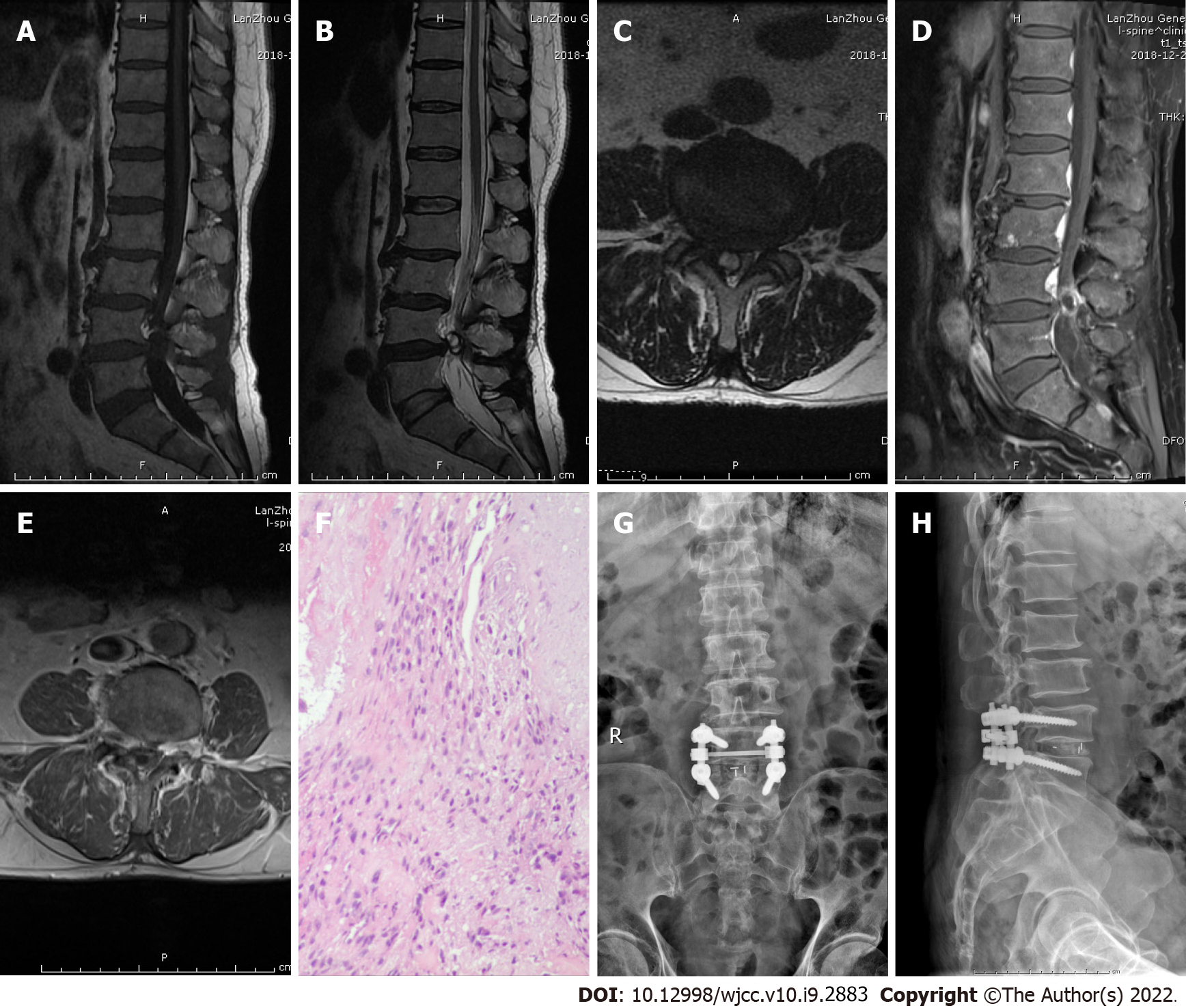
Case 2: After admission, an abnormal shadow on the right side of the L4–5 segment spinal canal was detected on MRI, compressing the cauda equina nerve and right nerve root. T1- and T2-weighted images showed low signal intensity. A “marginal capsule” and separation from the lesion were significantly enhanced on contrast-enhanced MRI (Figure 2A-2E).
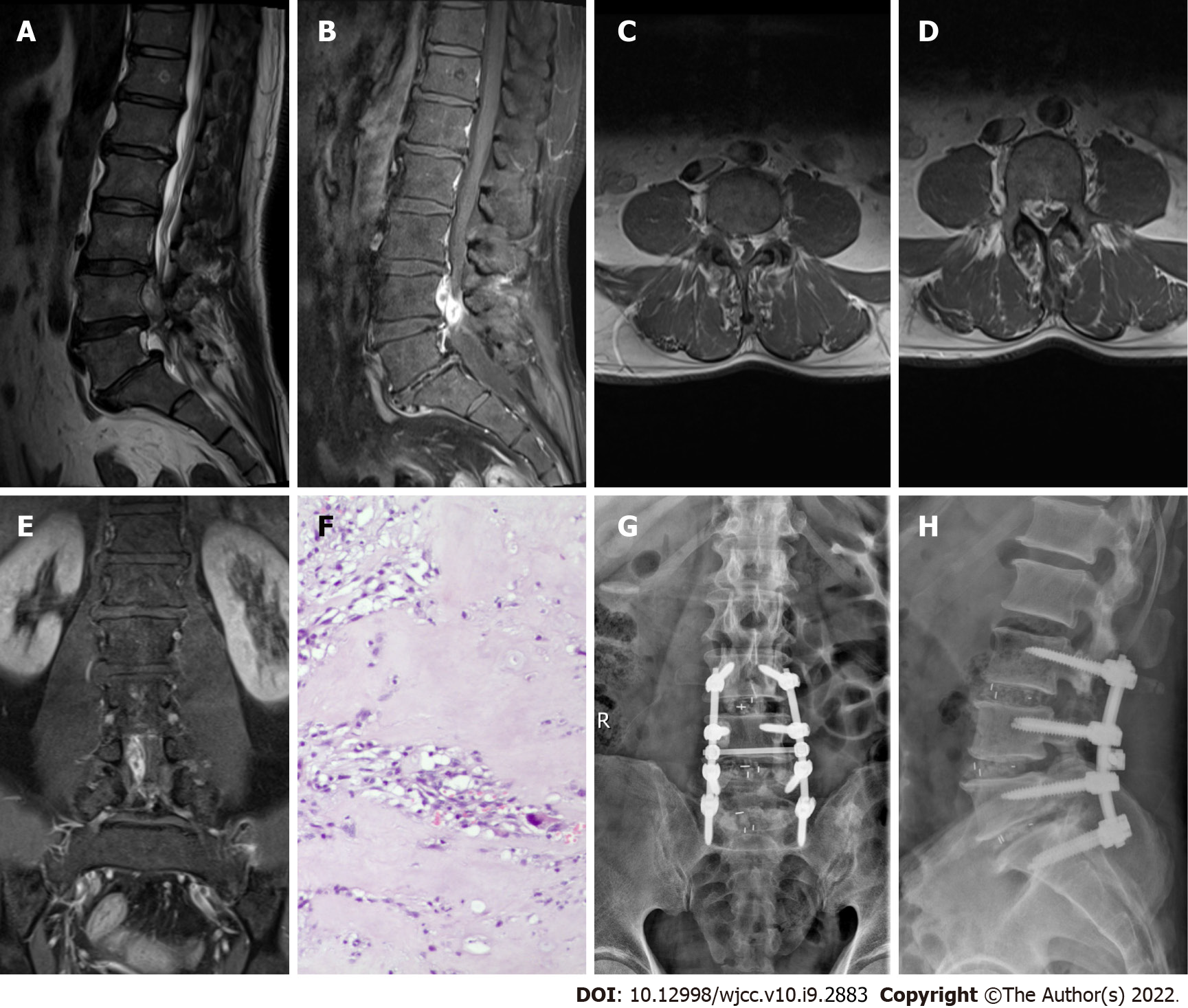
Case 3: After admission, an abnormal shadow was detected in the L4–5 segment spinal canal on MRI, and spinal canal stenosis was observed at the same level. High signal intensity was detected on the T2-weighted image, and peripheral enhancement was observed on contrast-enhanced MRI (Figure 3A-3E).
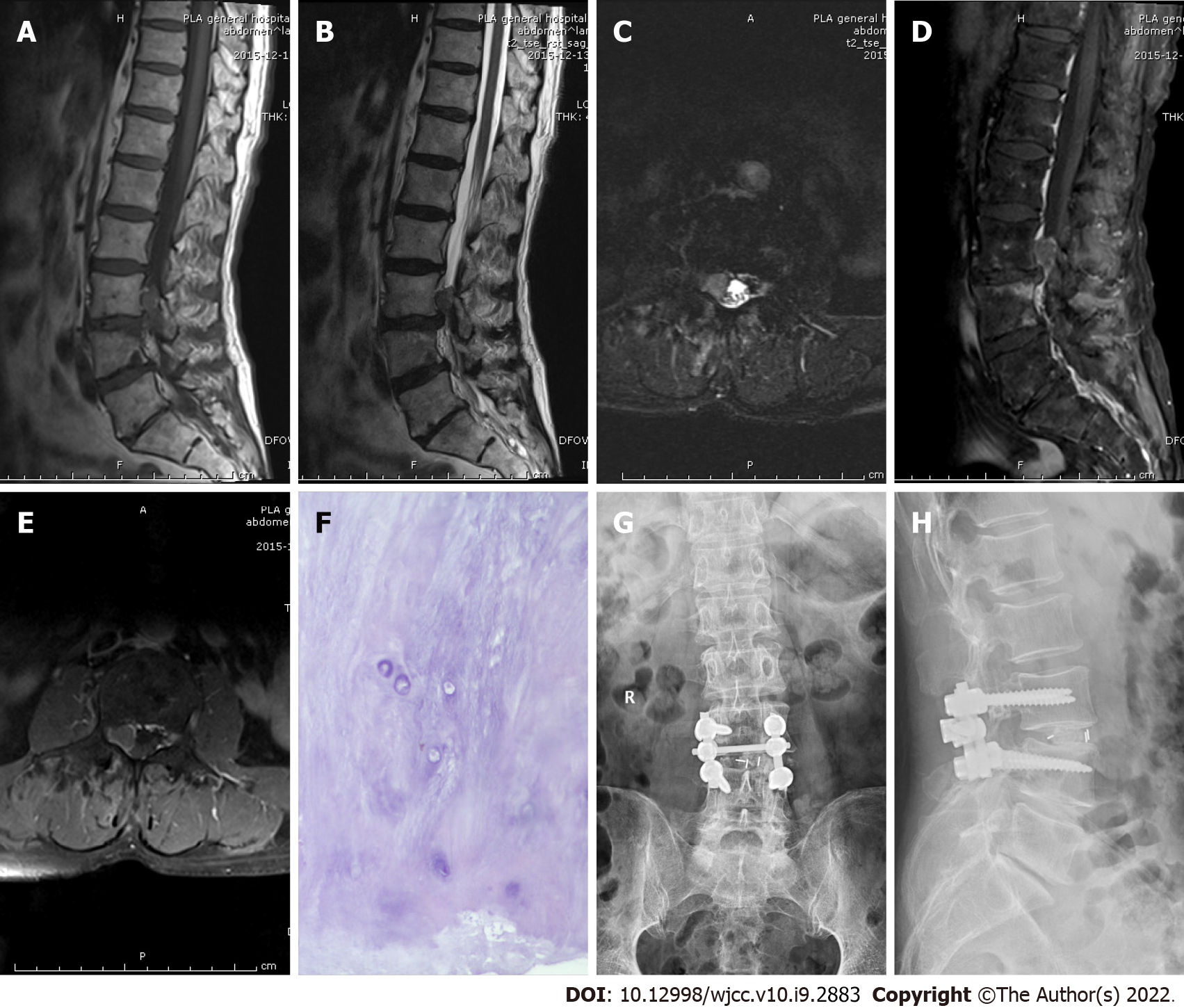
Case 4: After admission, an abnormal shadow was observed in the right intervertebral foramen of the L3 vertebral canal on MRI, and the adjacent dural sac was compressed. The T1-weighted image showed moderate signal intensity, while the T2-weighted image showed high signal intensity. There was no obvious enhancement on contrast-enhanced MRI (Figure 4A-4E).
According to the results of the preoperative physical, laboratory, and imaging examinations, cases 1 and 2 were diagnosed with neurilemmoma, and cases 3 and 4 with spinal tumors.
All four patients were diagnosed with lumbar disc herniation.
Case 1: A laminectomy, discectomy, and internal fixation were performed (Figure 1G-1H). The focus was located in the left posterior epidural space, which compressed the dural sac and left L4 nerve root. Postoperative pathology confirmed that the focus was intervertebral disc tissue (Figure 1F).
Case 2: A laminectomy, discectomy, and internal fixation were performed (Figure 2G–2H). The focus was located in the right posterior epidural space of L4–5, which significantly compressed the dural sac. Postoperative pathology confirmed that the focus was intervertebral disc tissue (Figure 2F).
Case 3: A laminectomy, discectomy, and internal fixation were performed (Figure 3G–3H). The focus was located in the right anterior L4–5 epidural space. Postoperative pathology confirmed that the focus was intervertebral disc tissue (Figure 3F).
Case 4: A hemilaminectomy, discectomy, and internal fixation were performed (Figure 4G–4H). The focus was located in the right anterior epidural space, compressing the dural sac and right L3 nerve root. Postoperative pathology confirmed that the focus was intervertebral disc tissue (Figure 4F).
Case 1: The patient was discharged on postoperative day 5 with fully recovered neurological function, and the preoperative pain had disappeared. He returned to normal life after the 3-mo follow-up.
Case 2: The patient was discharged on postoperative day 8 with fully recovered neurological function, and the preoperative pain symptoms had disappeared. He returned to normal life after the 3-mo follow-up.
Case 3: The patient was discharged on postoperative day 8 with fully recovered neurological function, and the preoperative numbness symptoms had disappeared. He returned to normal life after the 3-mo follow-up.
Case 4: The patient was discharged on postoperative day 6 with fully recovered neurological function, and the preoperative pain symptoms had disappeared. He returned to normal life after the 3-mo follow-up.
Intervertebral disc herniation refers to displacement of the intervertebral disc outside its anatomical space. Disc sequestration is defined as the migration of protruding disc fragments into the epidural space and complete separation from the parent disc[1,2]. Intervertebral disc herniation is closely related to degeneration of the intervertebral disc. When a herniated intervertebral disc prolapses into the epidural space, it expands rapidly because the intervertebral disc nucleus is rich in proteoglycans with strong hydrophilicity. The spinal cord and nerve root are easily compressed during the early stage of congestion, resulting in clinical symptoms[4].
The pathogenesis of lumbar disc herniation may be related to adhesions that form between the ventral dura mater and posterior longitudinal ligament. Repeated minor traumas or previous surgery can exacerbate the adhesions. The anterior epidural space is limited to the posterior longitudinal ligament and sagittal midline diaphragm. It spans the space between the vertebral body and posterior longitudinal ligament, preventing protruding disc fragments from crossing the midline. The lateral membrane is attached to the posterior longitudinal ligament and extends laterally to embed into the lateral wall of the spinal canal. The lateral membrane and posterior longitudinal ligament limit backward movement of free disc fragments[1,5]. Due to the anatomical structure of the anterior epidural space, most cases involve movement of intervertebral disc fragments in the lateral, cranial, or caudal direction[1,4,6-10]. In rare cases, fragments move back into the posterior epidural space or are located in the dura mater[2,3,11-17]. The lumbar spine is the most commonly affected area, but the intervertebral discs of cervical and thoracic vertebrae may be displaced[4,8,12].
Because of the uncertainty of the anatomical location and atypical imaging features, the free disc fragments in the spinal canal are easy to misdiagnose as spinal tumors. We used the term “disc herniation, mimicking tumor” to search PubMed from 1990 to 2020, and retrieved 65 articles. After reading the full texts, we identified 23 highly relevant reports (24 cases) that gave detailed information on all patients (Table 1). This encouraged us to report our four cases.
| Ref. | Age (yr), Sex | Symptoms | Duration of symptoms | Level | Location of disc fragments | Preoperative imaging | Gadolinium enhanced MRI | Preliminary diagnosis | Treatment | Outcome |
| Emamian et al[6], 1993 | 49, Female | Left-sided sciatica | Note report | L4-5 | Left intervertebral foramen | CT, My, MRI | Peripheral enhancement | Neurilemmoma | H + R | Partial recovery |
| Cusimano et al[22], 1995 | 42, Male | Left leg pain and paresthesia | Note report | L3-4 | Lateral to the left intervertebral foramen | CT, MRI | Enhancement | Neurilemmoma | Surgery (lateral intermuscular approach) | Partial recovery |
| Ashkenazi et al[7], 1997 | 59, Male | Pain in the lower back and right leg | 6 mo | L3-4 | Right intervertebral foramen | X-ray, CT, MRI | Remarkably enhanced | Neurilemmoma | H + R | Recovery |
| Saruhashi et al[11], 1999 | 44, Female | Pain in the lower back, right buttock, and leg | 1 mo | L5 vertebral body | Right posterior epidural space | X-ray, CT, My, MRI | Peripheral enhancement | Dumbbell tumor | L + R | Recovery |
| Bose[12], 2003 | 54, Male | Weakness and numbness in both lower limbs | 5 yr | T11-12 | Left posterior epidural space | MRI | Considerable peripheral enhancement | Neoplasm | L + R | Recovery |
| Aydin et al[13], 2004 | 58, Male | Pain in the low back and right leg | 2 yr, exacerbation of symptoms for 5 d | L5-S1 | Posterior intradural extra-medullary | MRI | Peripheral enhancement | Spinal tumor | L + R | Recovery |
| Lee and Suh[3],2006 | 61, Male | Pain in the low back and both lower legs | 4 mo, exacerbation of symptoms for 3 d | L5-S1 | Posterior intradural extra-medullary | MRI | Peripheral enhancement | Spinal tumor | L + R | Recovery |
| Bakar et al[18], 2009 | 46, Female | Pain in the low back and right leg | 1 mo | L4-5 | Lateral to the right intervertebral foramen | MRI | Enhanced homogenously | Nerve root neurilemmoma | H + R | Recovery |
| Stavrinou et al[4], 2009 | 46, Female | Neck pain and right brachialgia, weakness and numbness in the right hand | 3 wk | C5-6 | Right anterior epidural space | MRI | Enhanced homogenously | Neurilemmoma | Conservative | Recovery |
| Eksi et al[14], 2010 | 76, Female | Pain and weakness in the left foot | 1 mo | S1 vertebral body | Retroperitoneal left pre-sacral | MRI | Note report | Neurilemmoma | Surgery (anterior retroperitoneal approach) | Partial recovery |
| Levene et al[23], 2010 | 53, Female | Pain in the low back and numbness in the right leg | 3 wk | L2 vertebral body | Right anterior epidural space | X-ray, MRI | Peripheral enhancement | Cartilage neoplasm | Note report | Note report |
| Hoch and Hermann[1], 2010 | 50, Male | Pain in the low back and both lower legs | 4 mo, exacerbation of symptoms for 20 d | L3-4 | Right posterior epidural space | MRI | Peripheral ring enhancement | Spinal tumor | L + R | Recovery |
| Liu et al[15], 2011 | 50, Female | Pain in the low back, both hips, and left leg, numbness of both legs | 6 mo, exacerbation of symptoms for 2 wk | L5 vertebral body | Anterior intra-dural extra-medullary | MRI | Peripheral ring enhancement | Intraspinal tumor | L + R | Recovery |
| Demirci and Er[16], 2011 | 53, Female | Pain in the low back and both lower legs | 10 yr, exacerbation of symptoms for 15 d | L2-3 | Posterior intra-dural extramedullary | MRI | Enhanced homogenously | Spinal tumor | L + R | Recovery |
| Sharma et al[19], 2012 | 55, Male | Pain and weakness in the right leg | 2 mo | S1 vertebral body | Retroperitoneal right pre-sacral | CT, MRI | Peripheral enhancement | Neurilemmoma | Surgery (anterior retroperitoneal approach) | Recovery |
| Song et al[8], 2012 | 50, Female | Upper back pain and intermittent abdominal discomfort | 3 mo | T6-7 | Left intervertebral foramen | X-ray, CT, MRI | Peripheral enhancement | Bony tumor of the spinal canal | H + R | Recovery |
| Pillai[24], 2012 | 51, Male | Low backache with radiating pain to the right lower limb | 45 d | S1 | Intra-radicular in the right root | MRI | No enhancement | Nerve root tumor | H + R | Recovery |
| Dimogerontas et al[9], 2012 | 56, Male | Low back pain and right sciatica | 12 mo, exacerbation of symptoms for 4 d | L1-4 | Right anterior epidural space | MRI | Peripheral ring enhancement | Spinal tumor | L + R | Recovery |
| Peng and Pang[25], 2013 | 49, Male | Pain and numbness in the right leg | 1 yr, exacerbation of symptoms for 10 d | L5 vertebral body | Epidural space | MRI | Note report | Note report | H + R | Recovery |
| Li et al[2], 2016 | 48, Male | Intermittent pain in the low back and left lower limb and frequent urination | 4 yr, exacerbation of symptoms for 1 mo | L5-S1 | Left posterior epidural space | X-ray, CT, MRI | Peripheral ring enhancement | Extra-dural spinal tumor | L + R | Partial recovery |
| Ajayi et al[17], 2016 | 65, Female | Pain in the lower back and bilateral legs, weakness, and numbness in both legs | 1 mo, exacerbation of the symptoms for 2 wk | L3-4 | Left posterior epidural space | MRI | Peripheral ring enhancement | Spinal tumor | L + R | Recovery |
| Jia et al[10], 2018 | 57, Male | Low back pain, pain, and hypoesthesia in the right leg | 10 yr, exacerbation of symptoms for 1-mo | L4 vertebral body | Right anterior epidural space | MRI, 3D MRI | Note report | Neurilemmoma | Surgery | Recovery |
| 63, Male | Back pain and radiating pain in the right leg | 3 mo | L3-4 | Lateral recess | MRI, 3D MRI | Heterogeneous peripheral ring enhancement | Neurilemmoma | Minimally invasive endoscopic surgery | Recovery | |
| Ozpeynirci et al[26], 2019 | 42, Male | Right-sided radicular leg pain | 1 mo | L5-S1 | Retroperitoneal right pre-sacral | CT, MRI | Peripheral enhancement | Retroperitoneal peripheral neurilemmoma | Surgery (abdominal laparotomy) | Partial recovery |
| Present case one | 71, Male | Low back pain and radiating pain in the left leg | 1 yr, exacerbation of symptoms for 2 wk | L4 vertebral body | Left posterior epidural space | X-ray, MRI | Heterogeneous enhancement | Neurilemmoma | L + D + R | Recovery |
| Present case two | 74, Male | Pain in both knees with limited movement | 3 yr, exacerbation of symptoms for 3 wk | L4-5 | Right posterior epidural space | X-ray, CT, MRI | Heterogeneous peripheral ring enhancement | Neurilemmoma | L + D + R | Recovery |
| Present case three | 53, Male | Numbness and weakness in the low back and right lower limb | 2 wk | L4-5 | Right anterior epidural space | X-ray, CT, MRI | Considerable peripheral enhancement | Spinal tumor | L + D + R | Recovery |
| Present case four | 75, Male | Right-sided radicular leg pain | 15 d, exacerbation of symptoms for 1 wk | L3 vertebral body | Right anterior epidural space | X-ray, CT, MRI | No obvious enhancement | Spinal tumor | H + D + R | Recovery |
Although MRI helps clinicians to accurately diagnose intraspinal soft tissue lesions, it lacks specificity[12]. Therefore, it is necessary to distinguish prolapsed intervertebral disc tissue from epidural abscesses, dissolving epidural hematomas, synovial cysts, neurilemmomas, lipomas, and meningiomas. A free intervertebral disc in the spinal canal has low signal intensity on T1-weighted images and high signal intensity on T2-weighted images. Peripheral enhancement of non-enhanced intervertebral disc fragments is observed on contrast-enhanced MRI[8,17-19]. An epidural abscess is often located in the posterior epidural space. Compared with the spinal cord, it produces low or moderate signal intensity on T1-weighted images and high signal intensity on T2-weighted images. Contrast-enhanced MRI shows homogenous or peripheral enhancement. Subdural hematomas have similar manifestations, while dissolving epidural hematomas have a circular appearance and enhancement. MRI signal intensity is similar to that of the cerebrospinal fluid, and there are “focal marks” on the spinal cord. If there is no enhancement on contrast-enhanced MRI, a synovial cyst is likely. Neurilemmomas are often located within the epidural space; they are isointense on T1-weighted images, hyperintense on T2-weighted images, and enhanced on contrast-enhanced MRI. More than half of lipomas occur in the dura mater. Lipomas display high signal intensity on T1-weighted images, low signal intensity on T2-weighted images, and low signal intensity on fat-suppressed images. Meningiomas are most common in the thoracic spine and are often located in the dura mater. They are isointense on T1- and T2-weighted images and enhanced on contrast-enhanced MRI[1,8,12].
Case 1 showed high signal intensity on the T1-weighted image, low signal intensity on the T2-weighted image, and heterogeneous enhancement on contrast-enhanced MRI (Figure 1A–1E). Case 2 had low signal intensity on the T1-weighted image, low signal intensity on the T2-weighted image, and heterogeneous peripheral enhancement on contrast-enhanced MRI (Figure 2A–2E). These two cases were diagnosed as neurilemmomas before the operation. Case 3 displayed high signal intensity on the T2-weighted image and obvious peripheral enhancement on contrast-enhanced MRI (Figure 3A–3E). Case 4 exhibited moderate signal intensity on the T1-weighted image and high signal intensity on the T2-weighted image, without enhancement on contrast-enhanced MRI (Figure 4A–4E). These two cases were initially diagnosed as spinal tumors before the operation. Due to the nonspecific imaging findings, we were unable to diagnose these four patients by computed tomography, MRI, or enhanced MRI, so surgery was performed. The focus and adjacent intervertebral disc were resected, the intervertebral space was bone-grafted, and internal fixation was performed. The resected lesions were sent for pathological diagnosis. All four cases were pathologically diagnosed as herniated disc tissue (Figure 1F–4F).
Disc fragments usually show peripheral rim enhancement on contrast-enhanced MRI, which is related to the inflammatory reaction and new blood vessels around the intervertebral disc fragments. The degree of peripheral rim enhancement depends on the degree of angiogenesis[1,20,21]. However, atypical enhancement or non-enhancement on enhanced MRI made diagnosis difficult in this study.
Imaging is not ideal for diagnosing soft tissue masses. Even when the imaging diagnosis seems clear, pathological diagnosis is still the gold standard[7].
We describe and analyze the detailed characteristics of tumor-like disc herniations evident on contrast-enhanced MRI, and we sought to distinguish them from other spinal diseases with which herniations are easily confused. However, after reviewing the literature, we cannot draw a clear conclusion. We speculate that when peripheral enhancement is evident on contrast-enhanced MRI, a herniated disc should be strongly suspected. In the future, we will seek to enhance the accuracy of MRI and contrast-enhanced MRI used to diagnose intervertebral disc herniation.
We have described four cases of intervertebral disc herniation. The herniated intervertebral discs were all in the epidural space. In two cases, they migrated to the posterior space and did not have characteristic imaging findings on contrast-enhanced MRI. Our preliminary diagnosis of the four cases was spinal tumor. The free intervertebral disc should be considered when differentially diagnosing spinal lesions. For patients who cannot be diagnosed before surgery, surgical resection of the lesion and pathological examination can aid diagnosis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ghimire R, Meglio LD S-Editor: Xing YX L-Editor: Wang TQ P-Editor: Xing YX
| 1. | Hoch B, Hermann G. Migrated herniated disc mimicking a neoplasm. Skeletal Radiol. 2010;39:1245-1249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 2. | Li K, Li Z, Geng W, Wang C, Ma J. Postdural disc herniation at L5/S1 Level mimicking an extradural spinal tumor. Eur Spine J. 2016;25 Suppl 1:80-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Lee JS, Suh KT. Intradural disc herniation at L5-S1 mimicking an intradural extramedullary spinal tumor: a case report. J Korean Med Sci. 2006;21:778-780. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Stavrinou LC, Stranjalis G, Maratheftis N, Bouras T, Sakas DE. Cervical disc, mimicking nerve sheath tumor, with rapid spontaneous recovery: a case report. Eur Spine J. 2009;18 Suppl 2:176-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Akhaddar A, El-Asri A, Boucetta M. Posterior epidural migration of a lumbar disc fragment: a series of 6 cases. J Neurosurg Spine. 2011;15:117-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Emamian SA, Skriver EB, Henriksen L, Cortsen ME. Lumbar herniated disk mimicking neurinoma. Case report. Acta Radiol. 1993;34:127-129. [PubMed] |
| 7. | Ashkenazi E, Pomeranz S, Floman Y. Foraminal herniation of a lumbar disc mimicking neurinoma on CT and MR imaging. J Spinal Disord. 1997;10:448-450. [PubMed] |
| 8. | Song KJ, Kim KB, Lee KB. Sequestrated thoracic disc herniation mimicking a tumoral lesion in the spinal canal--a case report. Clin Imaging. 2012;36:416-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Dimogerontas G, Paidakakos NA, Konstantinidis E. Voluminous free disk fragment mimicking an extradural tumor. Neurol Med Chir (Tokyo). 2012;52:656-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Jia J, Wei Q, Wu T, He D, Cheng X. Two cases in which 3D MRI was used to differentiate between a disc mass that mimics a tumor and neurinoma. BMC Musculoskelet Disord. 2018;19:154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Saruhashi Y, Omura K, Miyamoto K, Katsuura A, Hukuda S. A migrated lumbar disc herniation simulating a dumbbell tumor. J Spinal Disord. 1999;12:307-309. [PubMed] |
| 12. | Bose B. Thoracic extruded disc mimicking spinal cord tumor. Spine J. 2003;3:82-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Aydin MV, Ozel S, Sen O, Erdogan B, Yildirim T. Intradural disc mimicking: a spinal tumor lesion. Spinal Cord. 2004;42:52-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Ekşi MS, Yener U, Akakin A, Akakin D, Konya D. Posterior epidural disc herniation at L3-L4 mimicking a spinal tumor: a case report. J Neurosurg Sci. 2010;54:71-76. [PubMed] |
| 15. | Liu CC, Huang CT, Lin CM, Liu KN. Intradural disc herniation at L5 Level mimicking an intradural spinal tumor. Eur Spine J. 2011;20 Suppl 2:S326-S329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Demirci A, Er U. A lumbar disc herniation mimicking spinal tumor with intra- and extradural components. Spine J. 2011;11:90-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Ajayi O, Shoakazemi A, Tubbs RS, Moisi M, Rostad S, Newell DW. Atypical Presentation of a Sequestered Posterolateral Disc Fragment. Cureus. 2016;8:e502. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Bakar B, Sumer MM, Cila A, Tekkok IH. An extreme lateral lumbar disc herniation mimicking L4 schwannoma. Acta Neurol Belg. 2009;109:155-158. [PubMed] |
| 19. | Sharma MS, Morris JM, Pichelmann MA, Spinner RJ. L5-S1 extraforaminal intraneural disc herniation mimicking a malignant peripheral nerve sheath tumor. Spine J. 2012;12:e7-e12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | D'Andrea G, Trillò G, Roperto R, Celli P, Orlando ER, Ferrante L. Intradural lumbar disc herniations: the role of MRI in preoperative diagnosis and review of the literature. Neurosurg Rev. 2004;27:75-80; discussion 81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 59] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 21. | Lakshmanan P, Ahuja S, Lyons K, Howes J, Davies PR. Sequestrated lumbar intervertebral disc in the posterior epidural space: a report on two cases and review of the literature. Spine J. 2006;6:583-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Cusimano MD, Bukala BP, Bilbao J. Extreme lateral disc herniation manifesting as nerve sheath tumor. Case report. J Neurosurg. 1995;82:654-656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 23. | Levene HB, Nimmagadda A, Levi AD. An unusual case of footdrop: anterior disc herniation mimicking a nerve sheath tumor. Neurosurgery. 2010;66:E419-20; discussion E420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Pillai SS. Intra-radicuar Disc Herniation mimicking a Nerve Root Tumor. J Orthop Case Rep. 2012;2:7-10. [PubMed] |
| 25. | Peng B, Pang X. Tumour-like lumbar disc herniation. BMJ Case Rep. 2013;2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 26. | Ozpeynirci Y, Braun M, Lubotzki I, Schmitz B, Antoniadis G. Extra-foraminal Intraneural L5-S1 Disc Herniation Mimicking a Retroperitoneal Peripheral Nerve Sheath Tumour: Case Report and Review of the Literature. Cureus. 2019;11:e4956. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |