Published online Mar 26, 2022. doi: 10.12998/wjcc.v10.i9.2878
Peer-review started: October 10, 2021
First decision: November 17, 2021
Revised: November 22, 2021
Accepted: February 12, 2022
Article in press: February 12, 2022
Published online: March 26, 2022
Processing time: 163 Days and 12.3 Hours
Diphallia is a highly uncommon congenital urogenital abnormality and a few connected reports have been published. However, no case of intraabdominal heterotopic diphallus has been documented to date. In the present study, we present a rare case of intraperitoneal ectopic bipenis.
A 49-year-old man was hospitalized with the chief complaint of hydronephrosis of both kidneys, which was discovered three days earlier through regular physical examination performed using urological ultrasound without significant lumbar or abdominal pain or bladder irritation. Physical examination showed normal external penile development, bilateral testes located on the left side of the scrotum, and a fused epididymis. Urological plain and enhanced computed tomography suggested bilateral hydronephrosis, bilateral ureters opened to the left side of the bladder wall; an intrapelvic soft tissue shadow on the left side of the bladder was considered a germline malformation called bipenis (hidden penis in the abdominal cavity). Based on the urological plain and enhanced computed tomography results, a 49-year-old man was diagnosed with bipenis (one hidden in the abdominal cavity). Ectopic penile compression produced bilateral ureteral dilatation and hydronephrosis. The ectopic penis was amputated and partially removed during surgery, and bilateral ureteral replantation was successfully performed. At a 2-mo follow-up, the patient was very satisfied with the operation, there was no significant hydronephrosis in both kidneys, and urination and erectile function were normal.
To our knowledge, this is the first report of diphallia with an intraperitoneal ectopic penis. Computed tomography or magnetic resonance imaging can be used to assess the associated internal anomalies before surgery. Postoperative pathological findings are the gold standard for the diagnosis.
Core Tip: We report a case diagnosed with bipenis (one hidden in the abdominal cavity). The main characteristics of the clinical manifestations and Sensitivity diagnosis, and treatments were assessed and a review of the related literature was performed, which may help to improve the understanding of the disease.
- Citation: Jia YT, Shi BL, Zhang J, Li YY, Zhu J. Bilateral ureteral reimplantation in a patient with an intraperitoneal ectopic bipenis: A case report. World J Clin Cases 2022; 10(9): 2878-2882
- URL: https://www.wjgnet.com/2307-8960/full/v10/i9/2878.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i9.2878
Diphallia (penile duplication) is an extremely rare congenital urogenital anomaly, with an incidence of approximately one in 5-6 million births[1,2] Since Wecker reported the first case in 1609, reports on more than 100 cases have been published[3]. Most of the available reports are about penile duplication in the perineum, which is visible to the naked eye. This is the first report of a patient with intraperitoneal ectopic bipenis to our knowledge, Mainly based on the literature review on PubMed database.
A man in his 40s was admitted to the hospital with the chief complaint of hydronephrosis in both kidneys for 3 d.
Without significant lumbar or abdominal pain or bladder irritation.
He had previously undergone ureteral stent placement on the right side due to bilateral hydronephrosis in January 2020; however, ureteroscopic placement on the left side failed. Left ureterotomy and ureteral stent implantation were performed accordingly. The bilateral ureteral stents were removed 3 mo postoperatively. Other past history were all negative.
The patient had no relevant personal and family history.
Physical examination showed normal external penile development, bilateral testes located on the left side of the scrotum, and a fused epididymis. The left-sided scrotal swelling that transilluminated upon application of light suggested a hydrocele.
Biochemical blood tests revealed no apparent abnormalities.
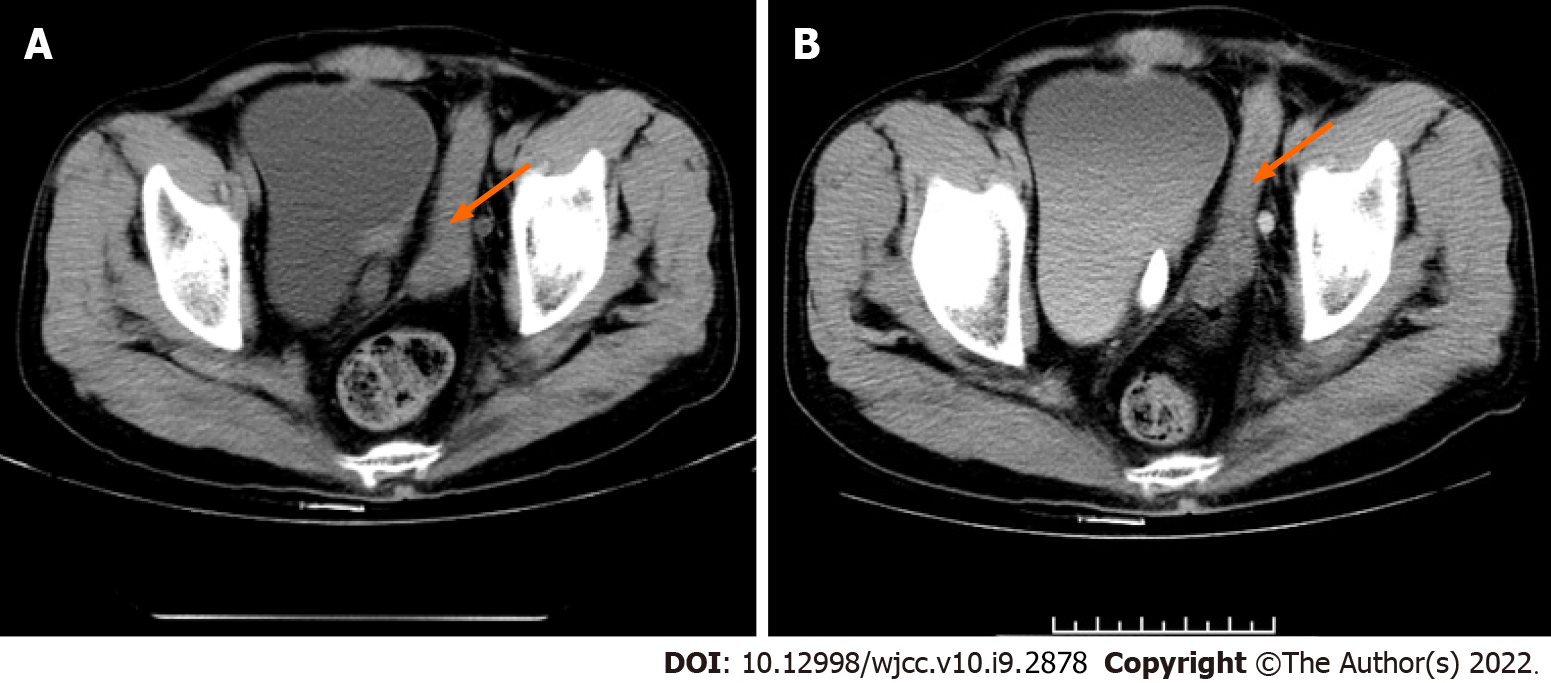
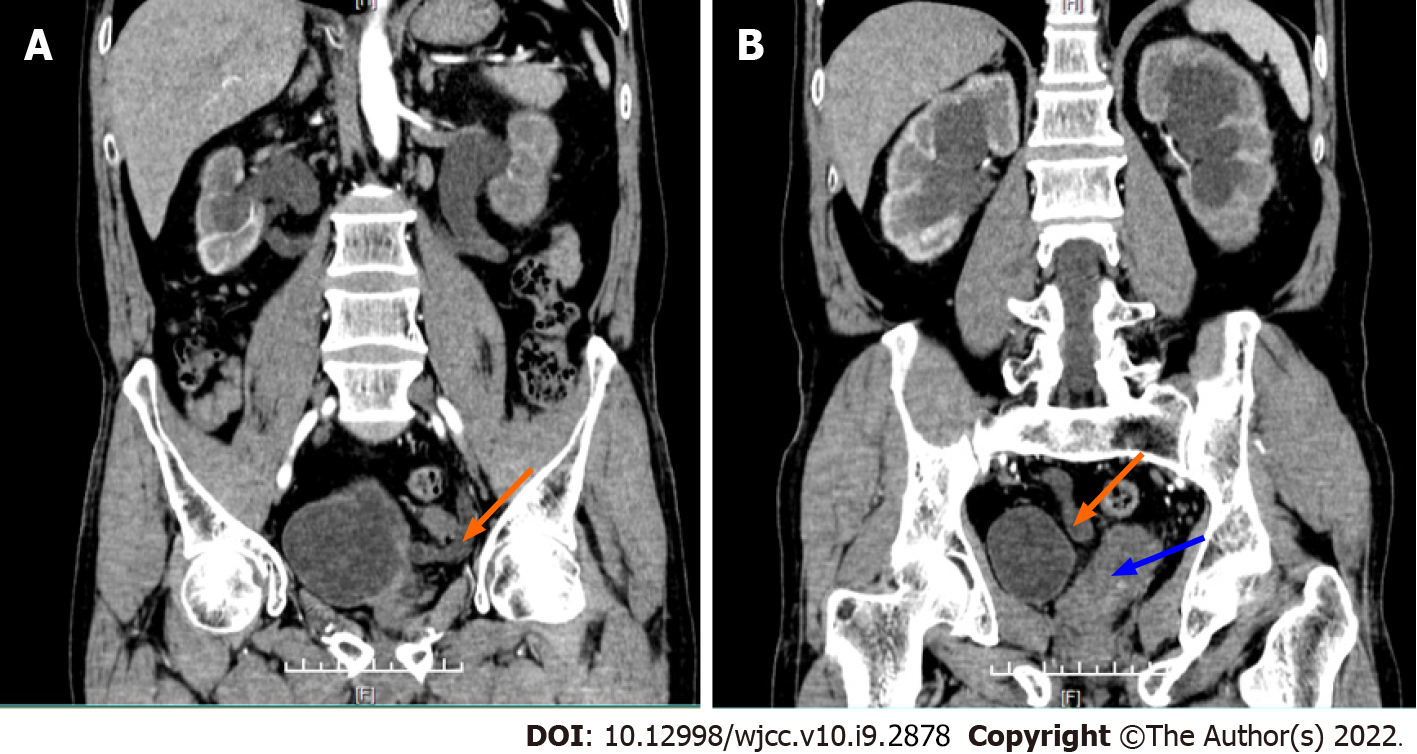
A previous ureteroscopy for bilateral hydronephrosis revealed bilateral ureteral malformation, derangement, and displacement of the seminal vesicle glands to the left side. Urological plain and enhanced computed tomography suggested bilateral hydronephrosis, ureteral dilatation, and ureteral confluence on the left side of the bladder, a malformation opening on the left side of the bladder wall (Figure 1), and an intrapelvic soft tissue shadow on the left side of the bladder, was considered a germline malformation, namely a bipenis (hidden penis in the abdominal cavity) (Figure 2).
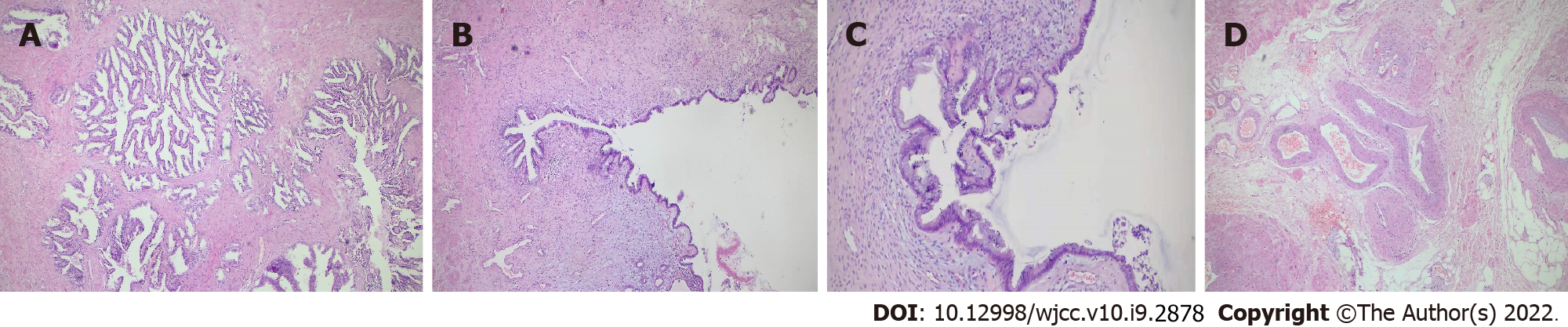
Postoperative pathology suggested that the urethra and urethral and penile corpus cavernosum tissues were visible in the specimen sent for examination, which was consistent with an ectopic penile morphology (Figure 3).
Intraoperative exploration around the bladder revealed 8.0 cm × 2.0 cm columnar solid tissue outside the left posterior wall of the bladder, with tough texture, reaching down to the anterior rectal wall and extending upward to the pelvic wall (Supplementary Figure 1). No seminal vesicle was seen, and the lumen of the left ureter was dilated, with a diameter of about 1.5 cm, passing behind the columnar tissue. The right ureter was carried out in the cysto-rectal space, with a lumen diameter of approximately 1.0 cm; the pelvic columnar neoplasm was considered a repeat ectopic penis. Due to serious adhesions, partial excision of the pelvic mass was performed, with a length of approximately 2.0 cm excised from the middle section, the smooth muscle tissue visible inside, and a tubular channel visible in the middle. The 7-0 silk sutures were wrapped and sutured at the stump, whereas the right and left ureters were loosened. Next, the ureters were cut short at the lowest point and reimplanted on the left and right anterior walls of the bladder, respectively, while bilateral ureteral stents were left in place.
The patient was discharged with no postoperative events. Follow-up was performed for 2 mo, with no reported adverse events. The patient was advised to visit regularly, especially within 1-2 years after surgery.
Penile duplication is an extremely rare congenital anomaly that varies in presentation and location from case to case[1,4]. Existing reports in the literature refer mainly to external penile duplication, whereas intra-abdominal ectopic penis has not been reported to date.
The etiology of diphallia remains unclear; however, there are many possible embryological explanations. Duplication of the penis is caused by a lack of fusion of the paired mesodermal anlagen of the genital tubercle by the 15th week of gestation[5]. Many genetic alterations have been implicated in the development of supernumerary penises, some of which include genes that encode androgen receptors and are linked to the development of male external genitalia[3,4]. Diphalia is not considered familial or hereditary[6].
There are many clinical classifications for these conditions, and some authors[2] classify them as follows: (1) True diphallia, (A) complete or (B) partial; (2) Bifid phallus: (A) partial (a) bifid glans (b) bifid shaft, or (B) complete. In 2017, Jesus et al[7] proposed a new simplified classification based on the clinical and surgical implications of each type: (1) True penile duplication (each duplicate penis has two corpora and one spongiosum); (2) Hemiphalluses (each penis has corpora and a hemiglans); (3) Pseudoduplication (normal penis with accessory penis-like tissue); and (4) Partial duplication (duplication involving only the distal penis). Our case had true penile duplication. True duplication is associated with other congenital defects[4,8,9]. Our case also involved anomalies, such as bilateral ureteral opening malformations, bilateral testicular ectopia, and bilateral epididymal fusion.
In general, ultrasonography helps to confirm the diagnosis by detecting the presence or absence of the corpus cavernosum or spongiosum and its number. It can also detect other associated abnormalities. However, this case was unique because the ectopic penis was located in the abdominal cavity. Furthermore, inexperienced sonographers may not always be able to identify this malformation. Magnetic resonance imaging (MRI) is a valuable method to accurately diagnose diphallia and associated malformations because T2-W images have the appropriate contrast resolution[1,10,11]. One limitation of the study is that no further MRI was performed in this case to confirm the diagnosis.
Our case was first identified by radiologists, and the possibility of an intra-abdominal ectopic penis was considered based on plain and enhanced computed tomography of the urinary tract, which was dependent upon the radiologists' experience in reading the films and provided important information for the physicians.
In general, the associated malformations should be treated first[12]. In the case of actual penile duplication, partial duplication, or pseudo-duplication, most surgeons choose to resect the hypoplastic duplicate penis, glans, or accessory penile-like tissues to maintain the main urethra[13]. In this case, the ectopic penis was located in the abdominal cavity and crossed the left ureter anteriorly, which caused bilateral ureteral dilatation and hydronephrosis. Bilateral ureteral reimplantation is required to further protect renal function, and dissociation of the ectopic penis is also compulsory.
As the patient was a middle-aged male, he had no reproductive needs for the time being, but the status of the patient's sexual activity still requires further attention after surgery.
To date, intra-abdominal ectopic bipenis has not been reported in humans. Penile duplication has a unique presentation in each patient, in which the position of the penis can be either ectopic or orthotopic. Depending on the corporal development and anatomy of the urethra, excision or reconstruction of the duplicate penis is required.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Urology and nephrology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Meglio LD, Singh KP S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Tirtayasa PM, Prasetyo RB, Rodjani A. Diphallia with associated anomalies: a case report and literature review. Case Rep Urol. 2013;2013:192960. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Aleem AA. Diphallia: report of a case. J Urol. 1972;108:357-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Jabali SS, Mohammed AA. Triphallia (triple penis), the first reported case in human. Int J Surg Case Rep. 2020;77:198-200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Frolov A, Tan Y, Rana MW, Martin JR 3rd. A Rare Case of Human Diphallia Associated with Hypospadias. Case Rep Urol. 2018;2018:8293036. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Hollowell JG Jr, Witherington R, Ballagas AJ, Burt JN. Embryologic considerations of diphallus and associated anomalies. J Urol. 1977;117:728-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 55] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Dodat H, Rosenberg D, James-Pangaud I. [Familial association of penoscrotal transposition and diphallia (double penis) with patella aplasia]. Arch Pediatr. 1995;2:241-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Jesus LE, Dekermacher S, Lopes E, Bacon AP. Glans duplication: In-depth review and proposal of a new classification. J Pediatr Urol. 2017;13:172-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Mirshemirani AR, Sadeghyian N, Mohajerzadeh L, Molayee H, Ghaffari P. Diphallus: report on six cases and review of the literature. Iran J Pediatr. 2010;20:353-357. [PubMed] |
| 9. | Karagözlü Akgül A, Uçar M, Çelik F, Kırıştıoğlu İ, Kılıç N. Complete Penile Duplication with Structurally Normal Penises: A Case Report. Balkan Med J. 2018;35:340-343. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Jabali SS, Mohammed AA. Crossed testicular ectopia: Case report with review of literature. Int J Surg Case Rep. 2020;75:189-192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Ghafoori M, Varedi P, Hosseini SJ. MRI in the diagnosis of diphallia. Pediatr Radiol. 2007;37:1298-1300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Corrêa Leite MT, Fachin CG, de Albuquerque Maranhão RF, Francisco Shida ME, Martins JL. Penile duplication without removal of corporal tissue: step by step of an excellent cosmetic result. J Pediatr Urol. 2014;10:567-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Zhang W, Yu N, Liu Z, Wang X. Pseudodiphallia: a rare kind of diphallia: A case report and literature review. Medicine (Baltimore). 2020;99:e21638. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |