Published online Mar 26, 2022. doi: 10.12998/wjcc.v10.i9.2721
Peer-review started: October 10, 2021
First decision: December 10, 2021
Revised: December 24, 2021
Accepted: February 12, 2022
Article in press: February 12, 2022
Published online: March 26, 2022
Processing time: 163 Days and 10.3 Hours
Spinal anesthesia is superior to general anesthesia for postoperative recovery in older patients (≥ 65 age). However, evidence for this is lacking.
To evaluate the effect of anesthesia on postoperative complications in older patients undergoing hip surgery.
This is a retrospective, propensity score-matched, cohort study. Patients ≥ 65-years-old who underwent hip surgery at the Traditional Chinese Medicine of Guangdong Provincial Hospital in China from October 2016 to June 2020 were included. The operative methods were femoral fracture’s internal fixation and hip replacement. The orthopedic doctors in different hospitals of our group have varied requirements for patients’ out-of-bed time after surgery. Therefore, spinal anesthesia or general anesthesia was selected according to the requirements of the orthopedic doctors. The primary outcome of this study was complications during the hospitalization of the postoperative patient. The length of hospital stay, postoperative blood transfusion, routine blood analysis, renal function, co
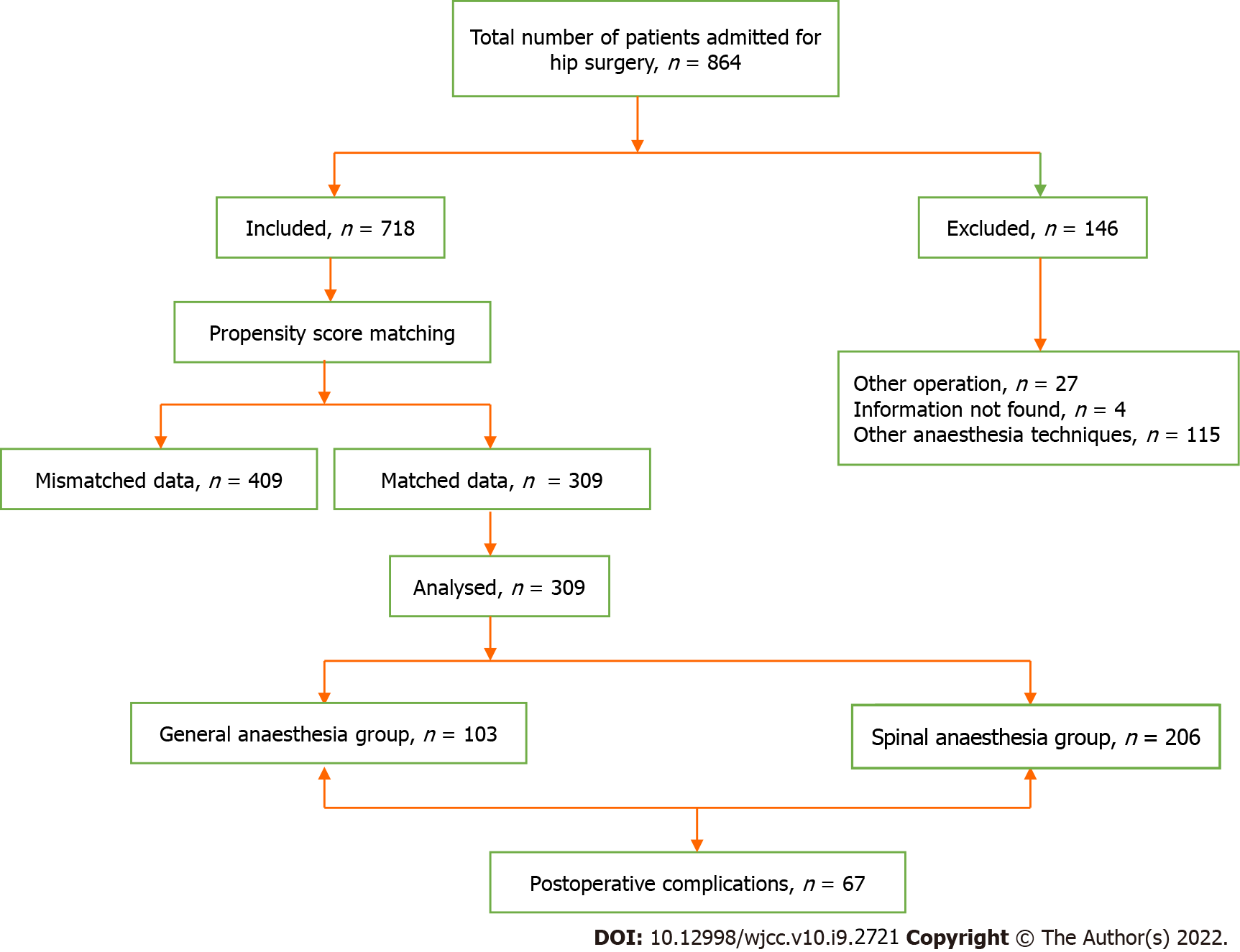
Among the 864 patients identified from the electronic medical record data database, we screened out those with incomplete medical record data. After PSM of the baseline values of the two groups of patients, data of 309 patients (206 patients in spinal anesthesia group and 103 patients in general anesthesia) were utilized in this study. 67/309 patients had complications, including postoperative limb dysfunction, pulmonary infection, delirium, lower extremity venous thrombosis, and shock. The incidence of complications was not related to anesthesia methods (P > 0.05), but the levels of D-Dimer (P = 0.017), fibrinogen (P = 0.005), and high-sensitivity C-reactive protein (hsCRP) (P = 0.002) in the spinal anesthesia group were significantly higher than those in the general anesthesia group.
Anesthesia technology is not a risk factor for postoperative complications of hip surgery. The levels of D-Dimer and hsCRP were higher in the spinal anesthesia group.
Core Tip: This is a retrospective cohort study. We used the propensity score matching to compare the preoperative data of retrospectively selected patients between groups. A total of 309 patients were selected to evaluate whether different anesthesia methods affect the incidence of postoperative complications of hip surgery in elderly patients. The current results showed no difference in postoperative complications between elderly patients undergoing hip surgery under spinal anesthesia and general anesthesia.
- Citation: Guo LS, Wang LN, Xiao JB, Zhong M, Zhao GF. Association between anesthesia technique and complications after hip surgery in the elderly population. World J Clin Cases 2022; 10(9): 2721-2732
- URL: https://www.wjgnet.com/2307-8960/full/v10/i9/2721.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i9.2721
Globally, the population is aging rapidly, increasing the demand for hip surgery, especially in older patients susceptible to bone mass loss. Successful surgery and postoperative functional recovery in the older population are yet challenging. The latter has a long-term effect on the quality-of-life post-discharge. Some potential serious complications during the perioperative period are observed in older patients, although advances in anesthesia and surgical nursing have recently minimized these events. Nonetheless, common complications are critical factors affecting the quality of life of older patients. Therefore, addressing and avoiding these complications is crucial in the older population undergoing hip surgery[1].
Several studies have posited that spinal anesthesia (SA) is superior to general anesthesia (GA) in surgery for older individuals. Among these studies, we observed that GA increases the risk of death, prolongs hospitalization, and increases the possibility of readmission and the risk of pulmonary complications[2,3]. However, evidence regarding whether the selected anesthesia affects post-hip surgery complications in older patients is lacking[4]. Large-scale studies have found that SA is independently associated with better outcomes[5]. In contrast, Kehlet et al[6] demonstrated that GA reduces the incidence of postoperative bladder dysfunction and severe neurological complications. Further evidence is needed to verify the effects of the choice of anesthesia for hip surgery in older patients. Thus, this propensity score-matched (PSM)-pair cohort study was designed to assess whether the type of anesthesia effectuated the complications after hip surgery. Subsequently, the postoperative outcomes, including length of hospitalization, postoperative pain, blood transfusion, routine blood analysis, renal function, coagulation function, and inflammatory reactions, were assessed.
This is a retrospective, PSM cohort study. The inclusion criteria were as follows: patients ≥ 65-years-old who had a history of hip surgery, including internal fixation of femoral fractures and hip replacement, at the Traditional Chinese Medicine of Guangdong Provincial Hospital in China between October 2016 and June 2020. The exclusion criteria included patients who underwent any other lower limb surgery, those who had anesthesia other than GA or SA, and whose medical records could not be located. The ethics approval for this study (Ethics approval number: ZE2020-288-01) was obtained from the Ethics Committee of Guangdong Provincial Chinese Hospital, Guangzhou, China (Chairperson Prof J. Liu) on November 11, 2020 prior to data collection. Informed consent was waived due to the retrospective design.
The independent variable examined in this study was the anesthesia technique (GA or SA) utilized during hip surgery. GA included propofol and sufentanil venous administration, rocuronium relaxant, and tracheal intubation. Sevoflurane inhalers were used for maintenance. SA involved the administration of 1% ropivacaine. Dexmedetomidine was used when necessary during surgery. Perioperative antibiotics were routinely administered to prevent infection. If patient-controlled analgesia post-surgery was insufficient, then multimodal administration was administered.
Data were extracted from the electronic Surgery Anesthesia Database System. General patient information, laboratory data, and clinical medical records were collected, and a comprehensive history was classified according to the disease system. Demographic data, including age, sex, and classification by the American Society of Anaesthesiologists (ASA) grade, were collected. Baseline data, such as Charlson comorbidity index (CCI), surgery site, duration, anesthesia time, intraoperative blood loss, hematocrit level, National nosocomial infection surveillance risk index, systematically recorded medical history, and preoperative renal function tests, were extracted[7,8].
The primary outcome of this study was the occurrence of complications during the hospitalization of the postoperative patient. These patients received our call-back visit 90 days after discharge from the hospital. Thus, two physicians manually reviewed medical records of patients diagnosed with postoperative complications, such as postoperative limb dysfunction, lung infection, delirium, deep venous thrombosis, and shock. The multiple complication classification system of Clavien-Dindo was adopted for severity grading of the reported complications. Data were collected to assess the secondary outcomes, including the length of hospital stay, postoperative blood transfusion, routine blood analysis, renal function, coagulation function, and inflammatory reactions[9].
The statistical methods of this study were reviewed by Lingnsong Guo from Guangdong Hospital of Traditional Chinese Medicine.Shapiro–Wilk test was used to evaluate the normality of variable distribution. Continuous variables were described as means ± SD, while categorical variables were described as frequency (%). If continuous variables were nonparametric, data were presented using median and range, quartiles, or confidence intervals. Mann-Whitney U, Pearson’s chi-square test, and Fisher’s exact tests were used to compare the baseline characteristics. Spearman’s correlation analysis was used to analyze the correlation between high-sensitivity C-reactive protein (hsCRP) and pulmonary infection.
To address the possible confounders, PSM was utilized to verify the basic principles and methods in large observational studies[10]. For PSM, demographic and baseline clinical data were included that could influence the incidence rate of complications. The ratio of the GA group to the SA group was 1:2. Specifically, age, position type, anesthesia time, ASA grade, blood loss, anesthesia level, inflammation level, and CCI score were matched between the groups.
A multivariate logistic regression model was established to estimate the individual propensity score of the GA group. Variables with significant standardization differences were included in the model a priori. In each iteration, standardized differences were used to assess the balance between queues, and unbalanced variables were included in the subsequent model. All baseline variables were balanced between the two queues by repeating the above steps.
P < 0.05 indicated a statistically significant difference. All analyses were performed using SPSS 20.0 (IBM, Armonk, NY, United States) and Stata 13.0 (Stata Corporation, College Station, TX, United States).
A total of 864 patients were identified in the medical record system; among them, 718 patients fulfilled the inclusion/exclusion criteria for selection. According to baseline data, PSM identified 309 cases. A flowchart of the study participant selection process is shown in Figure 1.
The cohort of 718 older patients underwent hip surgery at our institution during the study period, of which 139 (19.4%) received GA and 579 (80.6%) received SA (Table 1). Statistically significant differences were observed in some baseline characteristics prior to matching (Table 1). Patients in the SA group were more likely to be older, have a higher ASA grade, shorter operative time, longer anesthesia time, more intraoperative blood loss, higher infection grade, and higher CCI scores than those in the GA group.
| Total (n = 718) | Spinal anaesthesia (n = 579) | General anaesthesia (n = 139) | Standardised difference | P value | ||||
| n/mean | %/SD | n/mean | %/SD | n/mean | %/SD | |||
| Age (yr)1 | 84.76 | 5.38 | 85.23 | 5.33 | 82.82 | 5.15 | -0.529 | < 0.001 |
| Sex | -0.023 | 0.521 | ||||||
| Female | 532 | 74.1 | 426 | 73.6 | 106 | 76.3 | ||
| Male | 186 | 25.9 | 153 | 26.4 | 33 | 23.7 | ||
| ASA1 classification | -0.322 | < 0.001 | ||||||
| 1 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| 2 | 85 | 11.8 | 56 | 9.7 | 29 | 20.97 | ||
| 3 | 575 | 80.1 | 473 | 81.7 | 102 | 73.4 | ||
| 4 | 55 | 7.7 | 47 | 8.1 | 8 | 5.8 | ||
| 5 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Position type1 | -0.619 | < 0.001 | ||||||
| Lateral decubitus position | 282 | 39.3 | 199 | 34.5 | 83 | 59.7 | ||
| Prone position | 9 | 1.3 | 8 | 1.4 | 1 | 0.7 | ||
| Supine position | 134 | 18.7 | 106 | 18.4 | 28 | 20.1 | ||
| Traction position | 285 | 39.7 | 258 | 44.8 | 27 | 19.4 | ||
| Others | 5 | 0.7 | 5 | 0.9 | 0 | 0 | ||
| Operation time (min)1 | 69.80 | 35.34 | 67.10 | 31.47 | 80.98 | 46.70 | 0.322 | 0.001 |
| Anaesthesia time (min)1 | 117.48 | 45.84 | 113.13 | 42.50 | 135.54 | 54.22 | 0.458 | < 0.001 |
| Blood loss (mL)1 | 68.85 | 82.86 | 60.71 | 61.96 | 102.55 | 134.55 | 0.402 | < 0.001 |
| NNIS1 | -0.292 | < 0.001 | ||||||
| 0 | 214 | 29.8 | 155 | 26.8 | 59 | 42.4 | ||
| 1 | 496 | 69.1 | 420 | 72.5 | 76 | 54.7 | ||
| 2 | 8 | 1.1 | 4 | 0.7 | 4 | 2.9 | ||
| CCI1 | 5.14 | 1.47 | 5.23 | 1.48 | 4.77 | 1.41 | -0.368 | 0.001 |
| Comorbidities | ||||||||
| Respiratory system | 88 | 12.3 | 77 | 13.3 | 11 | 7.9 | -0.265 | 0.085 |
| Circulatory system | 533 | 74.2 | 429 | 74.1 | 104 | 74.8 | 0.027 | 0.914 |
| Digestive system | 91 | 12.7 | 72 | 12.4 | 19 | 13.7 | 0.069 | 0.695 |
| Urogenital system | 67 | 9.3 | 56 | 9.7 | 11 | 7.9 | -0.008 | 0.627 |
| Blood system | 20 | 2.8 | 14 | 2.4 | 6 | 4.3 | 0.098 | 0.248 |
| Endocrine system | 207 | 28.8 | 167 | 28.8 | 40 | 28.8 | -0.000 | 1.000 |
| Autoimmune system | 7 | 1 | 5 | 0.9 | 2 | 1.4 | -0.020 | 0.626 |
| Nervous system | 20 | 2.8 | 14 | 2.4 | 6 | 4.3 | 0.067 | 0.248 |
| Cerebrovascular system | 193 | 26.9 | 162 | 28 | 31 | 22.3 | -0.108 | 0.201 |
| Facial features | 8 | 1.1 | 7 | 1.2 | 1 | 0.7 | -0.020 | 1.000 |
| Mental disorders | 10 | 1.4 | 9 | 1.6 | 1 | 0.7 | -0.073 | 0.696 |
| Osteoporosis | 13 | 1.8 | 10 | 1.7 | 3 | 2.2 | 0.031 | 0.724 |
| Tumour | 62 | 8.6 | 51 | 8.8 | 11 | 7.9 | -0.001 | 0.744 |
| Operation | 272 | 37.9 | 216 | 37.3 | 56 | 40.3 | 0.035 | 0.559 |
| Blood transfusion | 26 | 3.6 | 20 | 3.5 | 6 | 4.3 | 0.015 | 0.801 |
| Laboratory examination | ||||||||
| Urea | 7.71 | 6.18 | 7.78 | 6.05 | 7.43 | 6.71 | -0.039 | 0.581 |
| Creatinine1 | 90.13 | 66.24 | 91.95 | 71.04 | 82.40 | 39.20 | -0.161 | 0.049 |
| e-GFR | 64.82 | 21.16 | 64.07 | 21.36 | 67.96 | 20.07 | 0.194 | 0.075 |
In the GA group, 74.1% (n = 103) were matched with twice as many patients in the SA group (n = 206) (Table 2). None of the covariates were significantly different after matching (all P > 0.05). No significant differences were detected in the incidence of postoperative complications between the SA and GA groups (Table 3).
| Total (n = 309) | Spinal anaesthesia (n = 206) | General anaesthesia (n = 103) | Standardised difference | P value | ||||
| n/mean | %/SD | n/mean | %/SD | n/mean | %/SD | |||
| Age (yr) | 84.23 | 5.12 | 84.33 | 5.21 | 84.04 | 4.95 | -0.128 | 0.644 |
| Sex | -0.021 | 0.401 | ||||||
| Female | 239 | 77.3 | 158 | 76.7 | 81 | 78.6 | ||
| Male | 70 | 22.7 | 48 | 23.3 | 22 | 21.4 | ||
| ASA classification | -0.117 | 0.873 | ||||||
| 1 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| 2 | 33 | 10.7 | 20 | 9.7 | 13 | 12.6 | ||
| 3 | 260 | 84.1 | 178 | 86.4 | 82 | 79.6 | ||
| 4 | 16 | 5.2 | 8 | 3.9 | 8 | 7.8 | ||
| 5 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Position type | -0.114 | 0.261 | ||||||
| Lateral decubitus position | 150 | 48.5 | 95 | 46.1 | 55 | 53.4 | ||
| Prone position | 5 | 1.6 | 4 | 1.9 | 1 | 1.0 | ||
| Supine position | 56 | 18.1 | 34 | 16.5 | 22 | 21.4 | ||
| Traction position | 97 | 31.4 | 72 | 35 | 25 | 24.3 | ||
| Others | 1 | 0.3 | 1 | 0.5 | 0 | 0 | ||
| Operation time (min) | 76.10 | 33.1 | 77.23 | 31.90 | 73.81 | 35.50 | -0.033 | 0.391 |
| Anaesthesia time (min) | 125.05 | 39.8 | 124.31 | 38.84 | 126.41 | 41.94 | -0.034 | 0.672 |
| Blood loss (mL) | 75.71 | 67.0 | 72.48 | 62.96 | 82.18 | 74.22 | -0.032 | 0.230 |
| NNIS | 0.050 | 0.635 | ||||||
| 0 | 40 | 12.9 | 6 | 29.6 | 34 | 33 | ||
| 1 | 213 | 68.9 | 143 | 69.4 | 67 | 65 | ||
| 2 | 4 | 1.3 | 2 | 1.0 | 2 | 1.9 | ||
| CCI | 5.05 | 1.4 | 5.09 | 1.39 | 4.97 | 1.39 | 0.033 | 0.470 |
| Comorbidities | ||||||||
| Respiratory system | 37 | 12.0 | 28 | 13.6 | 9 | 8.7 | 0.062 | 0.266 |
| Circulatory system | 232 | 70.1 | 153 | 74.3 | 79 | 76.7 | 0.026 | 0.678 |
| Digestive system | 40 | 12.9 | 24 | 11.7 | 16 | 15.5 | -0.046 | 0.370 |
| Urogenital system | 26 | 8.4 | 18 | 8.7 | 8 | 7.8 | 0.055 | 0.832 |
| Blood system | 10 | 3.2 | 6 | 2.9 | 3.9 | -0.025 | 0.736 | |
| Endocrine system | 83 | 26.9 | 55 | 26.7 | 28 | 27.2 | -0.025 | 1.000 |
| Autoimmune system | 3 | 1.0 | 2 | 1.0 | 1 | 1.0 | 0.024 | 1.000 |
| Nervous system | 9 | 2.9 | 5 | 2.4 | 4 | 3.9 | 0.014 | 0.488 |
| Cerebrovascular system | 80 | 25.9 | 55 | 26.7 | 25 | 24.3 | 0.079 | 0.681 |
| Facial features | 4 | 1.3 | 3 | 1.5 | 1 | 1.0 | 0.047 | 1.000 |
| Mental disorders | 3 | 1.0 | 2 | 1.0 | 1 | 1.0 | 0.062 | 1.000 |
| Osteoporosis | 8 | 2.6 | 6 | 2.9 | 2 | 1.9 | 0.076 | 0.723 |
| Tumour | 23 | 7.4 | 14 | 6.8 | 9 | 8.7 | 0.008 | 0.646 |
| Operation | 117 | 37.9 | 77 | 37.4 | 40 | 38.8 | 0.189 | 0.901 |
| Blood transfusion | 14 | 4.5 | 8 | 3.9 | 6 | 5.8 | -0.220 | 0.562 |
| Laboratory examination | ||||||||
| Urea | 7.30 | 4.8 | 7.49 | 5.43 | 6.90 | 3.27 | 0.060 | 0.360 |
| Creatinine | 8.64 | 65.4 | 91.85 | 76.31 | 81.92 | 31.79 | 0.018 | 0.143 |
| e-GFR | 64.45 | 21.2 | 63.5 | 21.69 | 66.37 | 20.24 | -0.036 | 0.313 |
| Spinal anaesthesia (n = 206) | General anaesthesia (n = 103) | P value | |||
| n | % | n | % | ||
| Hip joint dysfunction | 14 | 6.8 | 3 | 2.9 | 0.159 |
| Deep vein thrombosis | 3 | 1.5 | 0 | 0.0 | 0.219 |
| Delirium | 9 | 4.4 | 3 | 2.9 | 0.532 |
| Pneumonia | 25 | 12.1 | 7 | 6.8 | 0.147 |
| Shock | 2 | 1.0 | 1 | 1.0 | 1.000 |
PSM was used for all patients. Thus, the present analysis included 718 patients, of which 579 received SA and 139 received GA. Subsequently, 67 patients experienced postoperative complications during hospitalization. The model adjusted for several complications and preoperative characteristics of patients, including age, sex, ASA grade, CCI score, operation position, operative time, anesthesia time, intraoperative blood loss, infection grade, and history of complications. Bivariate analysis after PSM analysis showed that the anesthesia technique was not related to the incidence of postoperative complications. The specific postoperative complications are listed in Table 3. Interestingly, although the two matched cohorts had a similar incidence rate of complications, the postoperative fibrinogen, D-Dimer, and hsCRP levels in the SA group were significantly higher than those in the GA group. Additionally, the GA group demonstrated higher brain natriuretic peptide levels than the SA group (Table 4).
| Spinal anaesthesia (n = 206) | General anaesthesia (n = 103) | P value | |||
| n/mean | %/SD | n/mean | %/SD | ||
| Length of hospital stay (d) | 12.54 | 4.58 | 13.31 | 5.05 | 0.212 |
| 90-d readmission | 20 | 9.7 | 11 | 10.7 | 0.789 |
| Clavien-Dindo score | 0.583 | ||||
| 1 | 126 | 61.2 | 65 | 63.1 | |
| 2 | 69 | 33.5 | 30 | 29.1 | |
| 3 | 1 | 0.5 | 0 | 0 | |
| 4 | 10 | 4.9 | 8 | 7.8 | |
| 5 | 0 | 0 | 0 | 0 | |
| Renal function | |||||
| GLU (mmoL l-1)1 | 8.06 | 2.77 | 7.40 | 2.36 | 0.006 |
| Urea (mmoL l-1) | 7.34 | 3.27 | 7.46 | 3.73 | 0.943 |
| Cr (μmoL l-1) | 92.43 | 59.39 | 83.47 | 36.25 | 0.822 |
| eGFR (mL min-1/1.73 m2) | 63.87 | 21.54 | 65.67 | 20.54 | 0.656 |
| ALB (g) | 31.28 | 3.28 | 32.01 | 3.92 | 0.148 |
| Routine blood | |||||
| WBC (109 l-1)1 | 10.76 | 3.16 | 10.00 | 2.77 | 0.033 |
| NEUT (%) | 82.41 | 6.08 | 81.38 | 6.16 | 0.170 |
| RBC (1012 l-1) | 3.31 | 0.55 | 3.84 | 5.57 | 0.753 |
| Hb (g l-1) | 95.07 | 15.17 | 95.98 | 15.41 | 0.624 |
| HCT (%) | 29.15 | 4.84 | 29.60 | 4.71 | 0.437 |
| PLT (109 l-1) | 234.14 | 110.26 | 225.33 | 88.61 | 0.486 |
| PCT (%) | 0.33 | 0.40 | 0.19 | 0.15 | 0.187 |
| Coagulation | |||||
| PT (s) | 14.02 | 1.20 | 14.48 | 1.99 | 0.233 |
| PT% (%) | 88.54 | 11.54 | 85.59 | 16.74 | 0.170 |
| INR (R) | 1.09 | 0.09 | 1.13 | 0.20 | 0.420 |
| FIB (g l-1)1 | 5.10 | 1.11 | 4.70 | 1.26 | 0.029 |
| APTT (s) | 40.04 | 5.34 | 40.04 | 5.86 | 0.925 |
| DDi (ng l-1 FEU)1 | 5.9 | 4.07 | 4.25 | 3.98 | 0.003 |
| Others | |||||
| TnT (μg l-1) | 28.08 | 280.69 | 2.54 | 2.94 | 0.521 |
| BNP (pg m l-1)1 | 187.98 | 286.26 | 340.96 | 457.10 | 0.009 |
| NTProBNP (pg m l-1) | 1250.66 | 1361.23 | 1067.31 | 1920.33 | 0.233 |
| hsCRP (mg l-1)1 | 84.71 | 46.71 | 60.39 | 40.72 | 0.002 |
| ERS (mm h-1) | 52.78 | 29.49 | 51.21 | 69.59 | 0.214 |
Hip arthroplasty is common among geriatric patients. Most of these patients have multiple comorbidities with high rates of postoperative complications and mortality. We used a 25-G pen-point SA needle (diameter 0.5 mm) to address the risk of postoperative complications in older patients. Compared to conventional needles, the use of this 25-G needle in older people results in fewer injuries and reduces the risk of lower back pain and headaches[11]. Previous studies have shown that SA is more favorable than GA for postoperative recovery. A retrospective study of 2591 patients who had undergone hip surgery showed that the use of SA improved the postoperative outcomes by reducing the number of pulmonary embolisms, bleeding, and length of hospital stay[12]. A large-scale study relying on a large national database of patients from approximately 400 hospitals determined that SA had a more positive effect on the outcomes in primary hip arthroplasty than GA[5]. However, a large sample retrospective study of 16695 patients reported no difference in the risk of complications, including hospitalization, readmission, deep vein thrombosis, pulmonary embolism, myocardial infarction, and pneumonia, between the two anesthesia techniques[2]. Additionally, a 2016 retrospective Cochrane study demonstrated that the anesthesia technique had an effect only on the incidence of deep vein thrombosis but not on other key outcome indicators, including mortality, pneumonia, myocardial infarction, cerebrovascular accidents, acute psychiatric disorders, and discharge, which are consistent with the current findings[13].
Similarly, a prospective study, which included patients > 65-years-old undergoing hip surgery randomly assigned to GA or SA, suggested that the choice of anesthesia did not affect postoperative cognitive dysfunction[14]. Another retrospective study of 196 older patients who underwent hip arthroplasty found that the use of GA or SA did not affect postoperative recovery[15].
In the present study, our results suggested that the choice of anesthesia technique is not associated with the risk of complications after hip surgery in older patients. Notably, no significant difference was detected in the Clavien–Dindo score or common postoperative complications between the groups. Moreover, no significant difference was observed in the length of stay and 90-day readmission rates. Thus, our results suggested that the anesthesia technique is not the key factor affecting the postoperative rehabilitation in older patients undergoing hip surgery.
Differences were noted in laboratory indices, renal function, routine blood analysis, coagulation function, and inflammatory markers (including hsCRP) recorded before and after surgery after removing the confounding effects of covariates by PSM. Fibrinogen, D-Dimer, and hsCRP remained higher in the SA group, while the brain natriuretic peptide level was higher in the GA group after surgery. Although the incidence of common complications was not significant in either group, the incidence of common complications in the SA group was higher than that in the GA group.
Choice selection bias is one of the most obvious limitations of observational studies, and the results could be unreliable if this effect is not reduced appropriately. The two common statistical methods employed to reduce selection bias are multivariate logistic regression and PSM[16]. PSM is a method of data processing used for the control of confounding factors in observational and retrospective studies and commonly used in orthopedic research[17]. In the current study, we collected the information of 816 cases, and finally, 718 patients were obtained according to the inclusion and exclusion criteria. However, the general conditions of these patients, such as age, gender, course of the disease, and history, are different in the two groups. Among the 309 patients screened out after PSM, the differences in general information and preoperative conditions between the two groups were not statistically significant.
Another study comparing 52044 Taiwanese participants using a PSM sample found that the anesthesia technique had no significant effect on the incidence rates of 30-day mortality, pneumonia, acute myocardial infarction, delirium, or renal failure[18]. However, this study focused on the incidence of severe complications after hip arthroplasty and did not consider common complications that affect the quality of life after discharge. The study also emphasized that the findings could be more reliable if the definition of the outcome indicators were standardized and reported that some patients wanted to die at home, which is a local custom, and thus early discharge was listed as a cause of death[19].
Nonetheless, in the current study, some patients were prematurely discharged for financial reasons, leading to delayed complications that may not have been recorded and could have affected the analysis. Therefore, future studies could be improved by standardizing the definition of observation indicators.
Although our results showed that the anesthesia technique had no significant effect on complications, D-Dimer, fibrinogen, white blood cell count, glucose, brain natriuretic peptide, and hsCRP were significantly increased in the SA group. D-Dimer is the product of fibrinogen lysis after activation and is used to reflect the blood coagulation function. Although previous studies have suggested that D-Dimer is a predictor of postoperative deep vein thrombosis[20], recent studies did not show any significant differences in deep vein thrombosis diagnosis. The receiver operating characteristic curve analysis revealed that levels above a threshold of 1.75 mg/L for D-Dimers are independently associated with deep vein thrombosis[21]. Therefore, in the present study, the difference between GA and SA was not considered significant, as the D-Dimer levels in both groups were > 1.75 mg/L. Another study in Japan also showed that compared to GA, SA is associated with a significant increase in the risk of deep vein thrombosis, at about 48%. The study recorded patients with deep vein thrombosis, symptomatic or asymptomatic, by venous color Doppler ultrasound examination 10 days after the operation[22]. In the current study, we recorded symptomatic patients with deep vein thrombosis after surgery. A large deviation was noted in the occurrence of deep vein thrombosis events. Therefore, even our results showed that different anesthesia methods are not effective for elderly hip surgery. However, according to the changes in D-Dimer and fibrinogen levels, the high-risk surgery patients, such as those with a hypercoagulable state, perennial bedridden, and malignant tumors, avoided SA.
The differences in white blood cell count and glucose levels between the two groups were not clinically significant. Unfortunately, brain natriuretic peptide data were missing for many patients (n = 148), and the residual range was large (13.3-2397.19 ng/L) for meaningful comparison.
The SA group showed significantly higher levels of hsCRP after surgery than the GA group, while no statistically significant difference was observed in the diagnosis of lung infections in this study. The changes in hsCRP reflected postoperative recovery and postoperative stress levels related to surgical injury[23]. Due to the increase in oxidative stress reaction after the operation, the risk of postoperative complications increases, and the recovery time of patients after the operation is prolonged[24]. In the current study, SA patients were conscious during surgery, and GA patients were not, and changes in the psychological status of SA patients during the surgery might have led to differences in surgical stress between the two groups, resulting in differences in postoperative hsCRP, white blood cell counts, and glucose levels. Thus, reducing the stress response during surgery may be beneficial to the prevention of postoperative cognitive dysfunction in elderly patients[25]. We speculated that in elderly hip surgery patients who have to receive SA, drugs could be administered during the operation to reduce the degree of stress response caused by the operation and the environment.
In a retrospective study, Nouvenne et al[26] found that serum hsCRP levels > 61 mg/L were independently associated with a 3.59-fold increased risk of pneumonia, while other studies showed that the anesthesia technique had no obvious effect on CRP[27,28]. Thus, we evaluated the correlation between hsCRP and pulmonary infection and found a significant but weak correlation with the risk of pulmonary infection (r = 0.089, P = 0.179). Although no diagnostic difference was observed in the incidence of postoperative pulmonary infection between the two groups, and the incidence of postoperative pulmonary infection in the SA group (12.1%) was higher than that in the GA group (6.8%). These results suggested that older patients with severe coexisting pulmonary disease or those with risk factors, such as obesity, a history of chronic smoking, abuse of antibiotics, and long-term corticosteroid use, should be treated cautiously.
The current study has two distinct advantages. Firstly, we included 25 preoperative baseline indicators, utilized a propensity score model for balanced matching between groups, and included eight independent variables with significant differences between groups to reduce selection bias. Secondly, we incorporated the surgical location into the model to minimize potential confounding effects during surgery.
Nevertheless, the present study has some limitations. This was a single-center study, which restricts the generalizability of our findings to other institutions that may not be comprised of similar demographic and nursing processes. Also, we did not collect data on several variables that might affect the outcomes, including body mass index (BMI), drinking history, and the specific type of surgery. High BMI is associated with surgical site infection after total hip arthroplasty[29], and BMI classification is a predictor of early postoperative complications[30]. A history of alcohol consumption is an independent risk factor for blood transfusion after hip surgery[31]. Since our data were obtained from electronic medical records, it was not feasible to obtain these variables. Finally, other unknown factors, including inconsistent pre-recorded data, may have residual confounding effects. Also, the selection bias could not be ignored. Different surgical teams have varied requirements for anesthesia and surgical methods. Anesthesiologists have personal preferences for the choice of anesthesia methods, and the outcome indicators of adverse reactions after surgery are not uniform; these offsets cannot be calibrated by matching analysis. Therefore, to conclusively determine the preferred anesthesia for application in clinical hip arthroplasty practice, a multicenter, large-scale randomized trial is essential.
The anesthesia technique utilized in this study was not identified as a risk factor for common complications after hip surgery in the older population. The increase in hsCRP and D-Dimer levels was smaller in patients who underwent hip surgery under GA than SA, indicating the need for prudent selection of patients. This increase in hsCRP and D-Dimer requires further investigation in specific populations.
Successful surgery and postoperative functional recovery in the elderly remain challenging. Some studies believe that spinal anesthesia is superior to general anesthesia in surgery in the older patients. However, there is a lack of evidence on whether the selected anesthesia affects the complications after hip surgery in elderly patients.
The present study aimed to evaluate the effect of anesthesia on postoperative complications in older patients undergoing hip surgery.
Anesthesia technique is not a risk factor for postoperative complications of hip surgery, but it should be carefully selected for some patients.
Patients included patients over 65 years old who underwent hip surgery in Traditional Chinese Medicine of Guangdong Provincial Hospital in China from October 2016 to June 2020. The main outcome of this study was postoperative complications during hospitalization. Hospital stay, postoperative blood transfusion, blood routine analysis, renal function, coagulation function and inflammation were secondary results. Propensity score matching was performed by logistic regression.
67/309 patients had complications, including postoperative limb dysfunction, pulmonary infection, delirium, lower extremity venous thrombosis and shock. The incidence of complications was not related to anesthesia methods (P > 0.05), but the levels of D-Dimer (P = 0.017), fibrinogen (P = 0.005) and high-sensitivity C-reactive protein (P = 0.002) in spinal anesthesia group were significantly higher than those in general anesthesia group.
Anesthesia technology is not a risk factor for postoperative complications of hip surgery. The levels of D-Dimer and hsCRP were higher in the spinal anesthesia group.
To conclusively determine the preferred anesthesia for application in clinical hip arthroplasty practice, a multicenter, large-scale randomized trial is essential.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anesthesiology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Amornyotin S, El-Gendy HA S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | McIsaac DI, MacDonald DB, Aucoin SD. Frailty for Perioperative Clinicians: A Narrative Review. Anesth Analg. 2020;130:1450-1460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 159] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 2. | Desai V, Chan PH, Prentice HA, Zohman GL, Diekmann GR, Maletis GB, Fasig BH, Diaz D, Chung E, Qiu C. Is Anesthesia Technique Associated With a Higher Risk of Mortality or Complications Within 90 Days of Surgery for Geriatric Patients With Hip Fractures? Clin Orthop Relat Res. 2018;476:1178-1188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 3. | Smith LM, Cozowicz C, Uda Y, Memtsoudis SG, Barrington MJ. Neuraxial and Combined Neuraxial/General Anesthesia Compared to General Anesthesia for Major Truncal and Lower Limb Surgery: A Systematic Review and Meta-analysis. Anesth Analg. 2017;125:1931-1945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 79] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 4. | Association of Anaesthetists of Great Britain and Ireland; Griffiths R, Alper J, Beckingsale A, Goldhill D, Heyburn G, Holloway J, Leaper E, Parker M, Ridgway S, White S, Wiese M, Wilson I. Management of proximal femoral fractures 2011: Association of Anaesthetists of Great Britain and Ireland. Anaesthesia. 2012;67:85-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 171] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 5. | Memtsoudis SG, Sun X, Chiu YL, Stundner O, Liu SS, Banerjee S, Mazumdar M, Sharrock NE. Perioperative comparative effectiveness of anesthetic technique in orthopedic patients. Anesthesiology. 2013;118:1046-1058. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 320] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 6. | Kehlet H, Aasvang EK. Regional or general anesthesia for fast-track hip and knee replacement - what is the evidence? F1000Res. 2015;4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Roffman CE, Buchanan J, Allison GT. Charlson Comorbidities Index. J Physiother. 2016;62:171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 201] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 8. | Emori TG, Culver DH, Horan TC, Jarvis WR, White JW, Olson DR, Banerjee S, Edwards JR, Martone WJ, Gaynes RP. National nosocomial infections surveillance system (NNIS): description of surveillance methods. Am J Infect Control. 1991;19:19-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 564] [Cited by in RCA: 550] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 9. | Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18532] [Cited by in RCA: 24844] [Article Influence: 1183.0] [Reference Citation Analysis (0)] |
| 10. | Schulte PJ, Mascha EJ. Propensity Score Methods: Theory and Practice for Anesthesia Research. Anesth Analg. 2018;127:1074-1084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 137] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 11. | Arevalo-Rodriguez I, Muñoz L, Godoy-Casasbuenas N, Ciapponi A, Arevalo JJ, Boogaard S, Roqué I Figuls M. Needle gauge and tip designs for preventing post-dural puncture headache (PDPH). Cochrane Database Syst Rev. 2017;4:CD010807. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Malhas L, Perlas A, Tierney S, Chan VWS, Beattie S. The effect of anesthetic technique on mortality and major morbidity after hip fracture surgery: a retrospective, propensity-score matched-pairs cohort study. Reg Anesth Pain Med. 2019;44:847-853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Guay J, Parker MJ, Gajendragadkar PR, Kopp S. Anaesthesia for hip fracture surgery in adults. Cochrane Database Syst Rev. 2016;2:CD000521. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 89] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 14. | Tzimas P, Samara E, Petrou A, Korompilias A, Chalkias A, Papadopoulos G. The influence of anesthetic techniques on postoperative cognitive function in elderly patients undergoing hip fracture surgery: General vs spinal anesthesia. Injury. 2018;49:2221-2226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 60] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 15. | Rashid RH, Shah AA, Shakoor A, Noordin S. Hip fracture surgery: does type of anesthesia matter? Biomed Res Int. 2013;2013:252356. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Austin PC, Jembere N, Chiu M. Propensity score matching and complex surveys. Stat Methods Med Res. 2018;27:1240-1257. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 115] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 17. | Kane LT, Fang T, Galetta MS, Goyal DKC, Nicholson KJ, Kepler CK, Vaccaro AR, Schroeder GD. Propensity Score Matching: A Statistical Method. Clin Spine Surg. 2020;33:120-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 189] [Article Influence: 37.8] [Reference Citation Analysis (0)] |
| 18. | O'Donnell CM, McLoughlin L, Patterson CC, Clarke M, McCourt KC, McBrien ME, McAuley DF, Shields MO. Corrigendum to 'Perioperative outcomes in the context of mode of anaesthesia for patients undergoing hip fracture surgery: systematic review and meta-analysis' [Br J Anaesth 2018; 120: 37-50]. Br J Anaesth. 2018;120:1442-1444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Chu CC, Weng SF, Chen KT, Chien CC, Shieh JP, Chen JY, Wang JJ. Propensity Score-matched Comparison of Postoperative Adverse Outcomes between Geriatric Patients Given a General or a Neuraxial Anesthetic for Hip Surgery: A Population-based Study. Anesthesiology. 2015;123 136-147 [PMID:25955981 DOI: 10.1097/ALN.0000000000000695. |
| 20. | Bongard O, Wicky J, Peter R, Simonovska S, Vogel JJ, de Moerloose P, Reber G, Bonameaux H. D-dimer plasma measurement in patients undergoing major hip surgery: use in the prediction and diagnosis of postoperative proximal vein thrombosis. Thromb Res. 1994;74:487-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 46] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 21. | Li J, Zhu Y, Chen W, Zhao K, Zhang J, Meng H, Jin Z, Ye D, Zhang Y. Incidence and locations of deep venous thrombosis of the lower extremity following surgeries of tibial plateau fractures: a prospective cohort study. J Orthop Surg Res. 2020;15:605. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 22. | Nakamura M, Kamei M, Bito S, Migita K, Miyata S, Kumagai K, Abe I, Nakagawa Y, Nakayama Y, Saito M, Tanaka T, Motokawa S. Spinal anesthesia increases the risk of venous thromboembolism in total arthroplasty: Secondary analysis of a J-PSVT cohort study on anesthesia. Medicine (Baltimore). 2017;96:e6748. [PubMed] |
| 23. | Watt DG, Horgan PG, McMillan DC. Routine clinical markers of the magnitude of the systemic inflammatory response after elective operation: a systematic review. Surgery. 2015;157:362-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 246] [Article Influence: 24.6] [Reference Citation Analysis (0)] |
| 24. | Tsuchiya M, Shiomoto K, Mizutani K, Fujioka K, Suehiro K, Yamada T, Sato EF, Nishikawa K. Reduction of oxidative stress a key for enhanced postoperative recovery with fewer complications in esophageal surgery patients: Randomized control trial to investigate therapeutic impact of anesthesia management and usefulness of simple blood test for prediction of high-risk patients. Medicine (Baltimore). 2018;97:e12845. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 25. | Kotekar N, Shenkar A, Nagaraj R. Postoperative cognitive dysfunction - current preventive strategies. Clin Interv Aging. 2018;13:2267-2273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 178] [Cited by in RCA: 197] [Article Influence: 28.1] [Reference Citation Analysis (0)] |
| 26. | Nouvenne A, Ticinesi A, Folesani G, Cerundolo N, Prati B, Morelli I, Guida L, Lauretani F, Maggio M, Aloe R, Lippi G, Meschi T. The association of serum procalcitonin and high-sensitivity C-reactive protein with pneumonia in elderly multimorbid patients with respiratory symptoms: retrospective cohort study. BMC Geriatr. 2016;16:16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 27. | Kahveci K, Ornek D, Doger C, Aydin GB, Aksoy M, Emre C, Deveci A, Bozkurt M, Ozgun G. The effect of anesthesia type on stress hormone response: comparison of general vs epidural anesthesia. Niger J Clin Pract. 2014;17:523-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 28. | Buyukkocak U, Caglayan O, Daphan C, Aydinuraz K, Saygun O, Agalar F. Similar effects of general and spinal anaesthesia on perioperative stress response in patients undergoing haemorrhoidectomy. Mediators Inflamm. 2006;2006:97257. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 29. | Liu X, Dong Z, Li J, Feng Y, Cao G, Song X, Yang J. Factors affecting the incidence of surgical site infection after geriatric hip fracture surgery: a retrospective multicenter study. J Orthop Surg Res. 2019;14:382. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 30. | Peters RM, van Steenbergen LN, Stewart RE, Stevens M, Rijk PC, Bulstra SK, Zijlstra WP. Patient Characteristics Influence Revision Rate of Total Hip Arthroplasty: American Society of Anesthesiologists Score and Body Mass Index Were the Strongest Predictors for Short-Term Revision After Primary Total Hip Arthroplasty. J Arthroplasty. 2020;35:188-192.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 31. | You Y, Zhang Y, Qiang L, Sun Y, Zhang J, Bou E, Yan M, Dai K, Ding M. Prevalence and risk factors for perioperative complications of CKD patients undergoing elective hip surgery. J Orthop Surg Res. 2019;14:82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |