Published online Mar 6, 2022. doi: 10.12998/wjcc.v10.i7.2281
Peer-review started: July 28, 2021
First decision: October 25, 2021
Revised: November 5, 2021
Accepted: January 25, 2022
Article in press: January 25, 2022
Published online: March 6, 2022
Processing time: 217 Days and 3.1 Hours
Posterior reversible encephalopathy syndrome (PRES) is a neurotoxic encephalopathic state with clinical symptoms such as headache, altered consciousness, visual disturbances, and seizures. Vasogenic edema occurs predominantly in the posterior occipital and parietal lobes of the brain. PRES is caused by various diseases, and its mechanism remains unclear. However, it can be easily diagnosed based on characteristic lesions on magnetic resonance imaging.
A 51-year-old woman with unremarkable past medical history presented with progressively worsening back pain since 2 mo. Physical examinations revealed paralumbar muscle tenderness, a large lesion on the right breast and several mass-like lesions on both breasts. The blood pressure (BP) was elevated (150/90 mmHg), and did not respond to antihypertensive medication. On the seventh day of hospitalization, she exhibited a confused mental status and generalized tonic-clonic seizures. On magnetic resonance imaging, bilateral cortical and subcortical edema of the occipital lobes, suggestive of PRES, was observed. The serum calcium was 15.8 mg/dL. After two days of treatment with nicardipine, elcatonin, and zolendronic acid, her BP was 130/91 mmHg and serum calcium was 10.1 mg/dL. The patient regained consciousness and her mental status improved. Fluorodeoxyglucose-positron emission tomography revealed right breast cancer with extensive metastases.
Although rare, hypercalcemia can lead to PRES by causing uncontrolled hypertension. Prompt diagnosis can help prevent severe mental disturbances and even death.
Core Tip: Posterior reversible encephalopathy syndrome (PRES) is a treatable but pot
- Citation: Song CH, Lee SJ, Jeon HR. Posterior reversible encephalopathy syndrome in a patient with metastatic breast cancer: A case report. World J Clin Cases 2022; 10(7): 2281-2285
- URL: https://www.wjgnet.com/2307-8960/full/v10/i7/2281.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i7.2281
Posterior reversible encephalopathy syndrome (PRES) is a neurotoxic encephalopathic state with clinical features such as headache, vomiting, altered consciousness, visual disturbances, and seizures. The radiologic findings demonstrate vasogenic edema in the posterior occipital and parietal lobes of the brain[1]. The pathogenesis of PRES remains unclear, but it is likely related to cerebral autoregulatory failure and end
Hypertension is the most common cause of PRES. Post-transplantation, immune suppression, infection, or autoimmune disease are also risk factors for PRES. In cancer patients, wide use of chemotherapy and targeted agents can be associated with PRES. Hypercalcemia rarely causes PRES, but there have been few reports on hypercalcemia-induced PRES[2].
Hypercalcemia is a common finding in patients with advanced stage cancer. Hypercalcemia develops in cancer patients via parathyroid hormone-related peptide (PTHrP) production, osteolytic metastasis, excessive calcium release from the bone, ectopic 1-alpha-hydroxylase activity, and 1,25-dihydroxycholecalciferol formation[3].
We present a case of PRES caused by hypercalcemia and hypertension in a patient with advanced breast cancer with multiple bone metastasis who had never received chemotherapy.
A 51-year-old woman with unremarkable medical history was admitted to the hospital via the emergency room for lower back pain.
She complained of worsening back pain after lifting a heavy object two months ago. The numeric rating scale (NRS) score for back pain was seven points.
The patient had an unremarkable medical history.
The patient had an unremarkable personal and family history.
Physical examination revealed paralumbar muscle tenderness, a 5 cm × 8 cm skin ulcer on her right breast, and several mass-like lesions on both breasts. We planned to evaluate the multiple breast masses under the impression of breast cancer while treating her lumbar pain.
Her blood pressure on admission was 150/90 mmHg despite no history of hypertension. When the patient complained of severe pain, the blood pressure elevated to 170-180 mmHg, and when the pain was relieved, it decreased to 150 mmHg. Therefore, we concluded that the increased blood pressure was likely due to the uncontrolled pain, since the patient did not have a history of hypertension. Attempts to alleviate the pain included physical therapy, trigger point injection, and medication (intravenous nefopam and methocarbamol, as well as oral acetaminophen and tramadol). However, the pain and elevated blood pressure persisted (systolic BP, 160–180 mmHg). On the 4th day of admission, the patient continued to complain of severe pain (NRS score 8-9), and the patient's blood pressure was measured up to 186/106 mmHg. Therefore, we added oral and intravenous antihypertensive drugs to control her BP, but no improvement was observed.
On the 7th day of hospitalization, the patient had an altered mental status with generalized tonic-clonic seizures lasting for 1 min.
Her serum calcium level was 15.8 mg/dL.
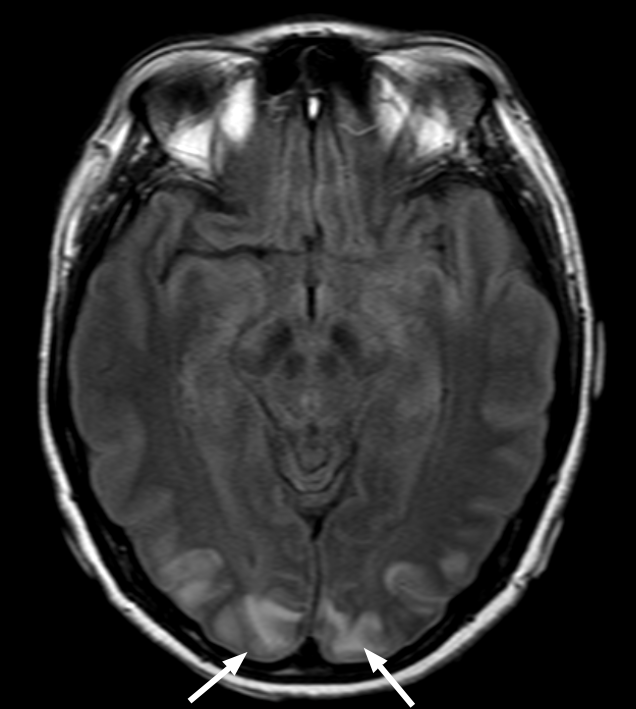
Electroencephalography showed repetitive seizures localized in the bilateral posterior region that were more prominent on the left side. Brain magnetic resonance imaging showed bilateral cortical and subcortical edema of the occipital lobes suggesting PRES lesions (Figure 1).
The final diagnosis of the presented case was PRES due to uncontrolled hypertension and hypercalcemia.
Her high BP was controlled using intravenous nicardipine, while the hypercalcemia was treated using normal saline, elcatonin, and zoledronic acid.
After two days of treatment, she had a BP of 130/91 mmHg and a serum cacium level of 10.1 mg/dL. Moreover, her mental status improved. After regaining consciousness, she experienced a partial visual field defect for a few days because of the occipital lobe involvement of PRES.
After the patient regained consciousness, fluorodeoxyglucose-positron emission tomography (FDG-PET) imaging was performed to evaluate the cancer status. FDG-PET imaging suggested right large breast cancer with extensive metastatic lesions, including the left breast, right axillary lymph node, and multiple bones (Figure 2). In addition, a biopsy for histopathological examination of the breast lesion, confirmed invasive ductal carcinoma.
The pathophysiology of PRES remains unclear, but there are two leading theories. First, when the blood pressure exceeds the upper limit of cerebral blood flow autoregulation, cerebral hyperperfusion occurs, and the blood-brain barrier breaks, allowing interstitial extravasation, which may cause vascular leakage and vasogenic edema[1]. The posterior brain areas are particularly susceptible to hyperperfusion due to the lack of sympathetic innervation. The second theory suggests that the syndrome is triggered by endothelial dysfunction, caused by circulating endogenous or exogenous toxins. The excessive release of pro-inflammatory cytokines results in endothelial activation, enhancing the release of vasoactive agents, and increasing vascular permeability and edema formation, which can also cause hypertension[1].
In this case, the patient had uncontrolled progressive hypertension after admission. Her systolic BP reached ≥ 180 mmHg. Her elevated BP was one of the leading causes of PRES.
Another consideration was her high calcium level, associated with her advanced breast cancer and multiple bone metastasis. Hypercalcemia is common in breast cancer patients, especially those with advanced-stage and multiple skeletal metastases[3]. The intervention of osteoclasts is the main mechanism of hypercalcemia in patients with extensive osteolytic bone metastases[4]. Excessive osteoclast activation, resulting from RANKL/RANK interaction and malignancy-secreted cytokines, leads to enhanced bone resorption and hypercalcemia.
Although the precise mechanism remains unclear, the pathophysiology of PRES can be correlated with increased calcium levels. Hypercalcemic conditions impair endothelial function by inhibiting the activation of nitric oxide released from endothelial cells. This has a vasodilating effect and increases systolic blood pressure[5]. In this case, the patient's high blood pressure was not controlled by antihypertensive drugs but was controlled after hypercalcemia was corrected. Another hypothesis is that hypercalcemia-induced hypomagnesemia results in hypertension. Based on the antagonism between calcium and magnesium, and the vasodilating properties of magnesium elevated calcium levels lower magnesium concentration. Thus, a magnesium deficit contributes to the development of vasoconstriction. The patient had slight hypomagnesemia (0.72 mmol/L, reference value 0.77-1.03 mmol/L). Based on this, the excessive calcium level of the patient made her vulnerable to developing PRES.
PRES has been reported in cancer patients who have undergone chemotherapy of targeted agents[6,7]. However, herein we focused on the pathophysiology found in advanced cancer in a case of PRES in an untreated breast cancer patient.
This was a rare case of PRES caused by hypertension and hypercalcemia. Although hypercalcemia is a rare cause of PRES, it can, directly and indirectly, result in uncontrolled hypertension, which can lead to PRES. Thus, it is essential to recognize diseases that induce hypercalcemia because PRES has been associated with severe consciousness disturbances and can be fatal. A prompt diagnosis is essential for adequate treatment.
Provenance and peer review: Unsolicited Manuscript; Externally peer reviewed.
Specialty type: Clinical neurology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hasan A S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Fugate JE, Rabinstein AA. Posterior reversible encephalopathy syndrome: clinical and radiological manifestations, pathophysiology, and outstanding questions. Lancet Neurol. 2015;14:914-925. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 580] [Cited by in RCA: 718] [Article Influence: 71.8] [Reference Citation Analysis (0)] |
| 2. | Bolanthakodi N, Vidyasagar S, Varma M, Holla A. Posterior reversible encephalopathy syndrome due to hypercalcaemia: a rare cause. BMJ Case Rep. 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Mirrakhimov AE. Hypercalcemia of Malignancy: An Update on Pathogenesis and Management. N Am J Med Sci. 2015;7:483-493. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 130] [Cited by in RCA: 150] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 4. | Feldenzer KL, Sarno J. Hypercalcemia of Malignancy. J Adv Pract Oncol. 2018;9:496-504. [PubMed] |
| 5. | Nilsson IL, Rastad J, Johansson K, Lind L. Endothelial vasodilatory function and blood pressure response to local and systemic hypercalcemia. Surgery. 2001;130:986-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 44] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Cacho-Díaz B, Lorenzana-Mendoza NA, Salmerón-Moreno K, Reyes-Soto G, Castillo-Rangel C, Corona-Cedillo R, Escobar-Ceballos S, Garza-Salazar JG. Chemotherapy-induced posterior reversible encephalopathy syndrome: Three case reports. Medicine (Baltimore). 2019;98:e15691. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Ladwa R, Peters G, Bigby K, Chern B. Posterior Reversible Encephalopathy Syndrome in Early-Stage Breast Cancer. Breast J. 2015;21:674-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |