Published online Mar 6, 2022. doi: 10.12998/wjcc.v10.i7.2253
Peer-review started: August 9, 2021
First decision: October 17, 2021
Revised: October 25, 2021
Accepted: January 22, 2022
Article in press: January 22, 2022
Published online: March 6, 2022
Processing time: 204 Days and 14.4 Hours
Plexiform fibromyxoma (PF) is a rare mesenchymal tumor, with limited case reports worldwide. Common clinical symptoms are abdominal discomfort and bleeding signs, which frequently present slow-onset in reported cases. Herein, we report a case of gastric PF presenting as acute onset and with pyemia accom-panying tumor rupture. We resected the tumor as well as the distal gastric, bulbus duodeni and gallbladder for treatment in emergency surgery. Notably, before the onset of the disease, the patient received coronavirus disease 2019 (COVID-19) vaccines.
A 26-year-old man was admitted to our hospital, due to abdominal pain and fever after having received COVID-19 vaccines. Laboratory examination indicated severe sepsis. Computed tomography scan revealed a large mass in the abdomen. Deformation of the gastrointestinal tract was seen during gastroscopy. After failure of anti-infective treatment and symptoms of shock developed, he received an emergency surgery. We found a huge and partly ruptured mass, with thick purulence. Microscopically, the mass was composed of spindle cells with clarified cytoplasm, accompanied by myxoid stroma and arborizing blood vessels. Immunohistochemistry showed the tumor cells as positive for smooth muscle actin and succinate dehydrogenase subunit B but negative for DOG-1 and CD117. Finally, the patient was diagnosed with gastric PF and discharged from the hospital.
Gastric PF manifesting as tumor rupture combined with pyemia is rare. Timely surgery is critical for optimal prognosis.
Core Tip: Gastric plexiform fibromyxoma (PF) is a rare mesenchymal tumor, with limited reports worldwide. This may be the first case report worldwide of emergency surgery performed for ruptured gastric PF with severe infection, demonstrating the rarity of the symptoms of this disease. In addition, we noted that the patient had a history of coronavirus disease 2019 vaccination before the onset of the disease. We also conducted a database search of PubMed and Web of Science as of June 2021, determining the number of reported cases to be 134 worldwide. Some new cases and experiences are summarized in this report.
- Citation: Zhang R, Xia LG, Huang KB, Chen ND. Huge gastric plexiform fibromyxoma presenting as pyemia by rupture of tumor: A case report. World J Clin Cases 2022; 10(7): 2253-2260
- URL: https://www.wjgnet.com/2307-8960/full/v10/i7/2253.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i7.2253
Gastric plexiform fibromyxoma (PF) is a rare mesenchymal tumor, most commonly found in the gastric antrum. Only 121 cases of PF have been reported worldwide, according to a review article published in July 2019[1]. This tumor type was first reported in 2007 by Takahashi et al[2] as plexiform angiomyxoid myofibroblastic tumor because of its pathological feature. Miettinen et al[3] later redescribed it as ‘gastric PF’ in 2009, a name which was also adopted by the World Health Organization’s classification of tumors of the digestive system. The clinical manifestations of gastric PF lack specificity and are mainly presented as slow-onset of nonspecific gastrointestinal discomfort. Few of them have required emergency surgery. Because of its low incidence and nonspecific symptoms, gastric PF is not yet fully understood and often misdiagnosed as gastrointestinal stromal tumor (GIST). Herein, we report a case of gastric PF that ruptured and caused sepsis, with the goal of reminding readers of the infrequent symptoms caused by this rare disease and showing a feasible treatment option. We noted that the patient also had a history of coronavirus disease 2019 (COVID-19) vaccinations prior to onset of the disease. In addition, we found more than 13 new cases after reviewing the public literature databases of PubMed and Web of Science[4-15] in Table 1.
| No | Ref. | Population | Age | Sex | Clinical presentation | Ulcer | Location | Size | Diagnosis | Treatment | Prognosis |
| 1 | Magadán Álvarez et al[4]; 2021 | Spain | 41 | M | Vomiting, weight loss | NA | Antrum | NA | PF | Distal gastrectomy | NA |
| 2 | Pei et al[5]; 2020 | China | 45 | M | Incidental | NA | Antrum | 7 cm × 5.5 cm × 5 cm | PF | Radical distal gastrectomy | Uneventful for 3 mo |
| 3 | Nasralla et al[6]; 2020 | Saudi Arabia | 16 | M | Hematemesis | + | Cardia | 5 cm × 5 cm × 4.5 cm | PF | Wedge resection | Uneventful for 3 yr |
| 4 | Martí Gelonch et al[7]; 2021 | Spain | 67 | F | Postprandial fullness, weight loss | NA | Antrum | 18 cm × 10 cm | PF | Local resection | NA |
| 5 | Vieites Branco et al[8]; 2020 | Portugal | 50 | F | Intense epigastric pain | - | Antrum | NA | PF | Distal partial gastrectomy, cholecystectomy | NA |
| 6 | Tang et al[9]; 2020 | China | 56 | M | Dysphagia | - | Esophagus | 6.0 cm × 3.0 cm | PF | Endoscopic submucosal dissection | NA |
| 7 | Hong et al[10]; 2020 | China | 20 | F | Intermittent epigastric pain, tarry stool, weakness and palpitation | + | Antrum | 10.0 cm × 4.0 cm × 3.5 cm | PF | Radical distal gastrectomy | Uneventful for 2 yr |
| 8 | Gan et al[11]; 2020 | United States | 44 | F | Abdominal pain, vomiting, and fatigue | - | Antrum | 6.2 cm × 3.8 cm × 3.6 cm | PF | Subtotal gastrectomy | NA |
| 9 | Arslan et al[12]; 2020 | United States | 16 | F | Gastrointestinal bleeding and outlet obstruction | NA | Antrum | 15.0 cm | Corrected to PF | Surgical resection (specific unknown) | NA |
| 10 | Arslan et al[12]; 2020 | United States | 68 | M | Incidental | NA | Small bowel | 8.0 cm | Corrected to PF | Surgical resection (specific unknown) | NA |
| 11 | Kobori et al[13]; 2019 | Japan | 45 | F | Pharyngeal discomfort | - | Antrum | 1 cm | PF | ESD | Uneventful for 6 mo |
| 12 | Perry et al[14]; 2020 | United States | 39 | M | Weight loss | NA | Antrum | 4.8 cm × 5.9 cm × 5.6 cm | PF | Gastric wedge resection, EGD | Uneventful for 1 mo |
| 13 | Li et al[15]; 2021 | China | 65 | M | Epigastric pain | - | Gastric body | 2.6 cm | PF | NA | Uneventful for 12 mo |
A 26-year-old man was admitted to our hospital with complaint of abdominal pain and fever that had persisted over the past half-month, following receipt of the COVID-19 vaccines.
On January 11, 2021, the patient developed right upper abdominal pain and fever (37.8 °C) 5 h after COVID-19 vaccination. During the first 11 d, he did not receive any treatment for the abdominal pain (deemed ‘tolerable’) nor the intermittent low-grade fever. However, his symptoms progressively worsened, to the extent that his tem-perature rose to 39.5 °C and he experienced melena.
The patient first went to the local hospital for medical treatment on January 22, 2021. Blood panel and computed tomography (CT) examinations were performed. Signs of infection were detected and a mass was found in the gastric antrum. Because the cause of the infection was unclear, the patient did not receive surgery at the local hospital but did receive oral cephalosporin antibiotics and symptomatic treatment. However, his symptoms were not relieved, so he was referred to our hospital on January 26, 2021 for further treatment. After hospitalization, we upgraded the patient’s anti-infective therapy and decided to perform emergency surgery as the care staff noted the patient to have developed a confused state and signs of infectious shock on January 27, 2021.
The patient had no significant medical history.
The patient had no significant family history of any malignancy.
On January 26, 2021, the physical examination made upon admission showed tenderness in the right upper abdomen without rebound pain and no palpable lump. Murphy's sign was positive but no signs of jaundice were noted. Basic clinical findings were temperature of 39.6 °C, blood pressure of 153/84 mmHg, heart rate of 126/min, and respiration of 25/min. Findings from other physical examinations were unre-markable.
On January 22, 2021, the patient’s blood examination (preformed in the local hospital) indicated an increased white cell count [13.01 × 109/L; reference range: (4.0-10.0) × 109/L] and neutrophil ratio (69.6%; reference range: 50%-75%).
On January 23, 2021, a second blood examination found the white cell count to have increased to 25.7 × 109 /L and neutrophil ratio to 82.5%.
On January 26, 2021 (the day of admission to our hospital), the patient’s blood examination indicated a white cell count of 14.61 × 109/L and neutrophil ratio of 84.2%. In addition, we detected remarkable increases in total bilirubin (31.0 mmol/L; reference range: 1.7-20 μmol/L), erythrocyte sedimentation rate (58 mm/h; reference range: 0-15 mm/h), and hs-C-reactive protein (332.41 mg/L; reference range: < 5 mg/L). Blood culture produced no bacterial growth. Tumor markers, such as carcinoembryonic antigen, alpha-fetoprotein, cancer antigen-199 and cancer antigen-125, were all within normal range.
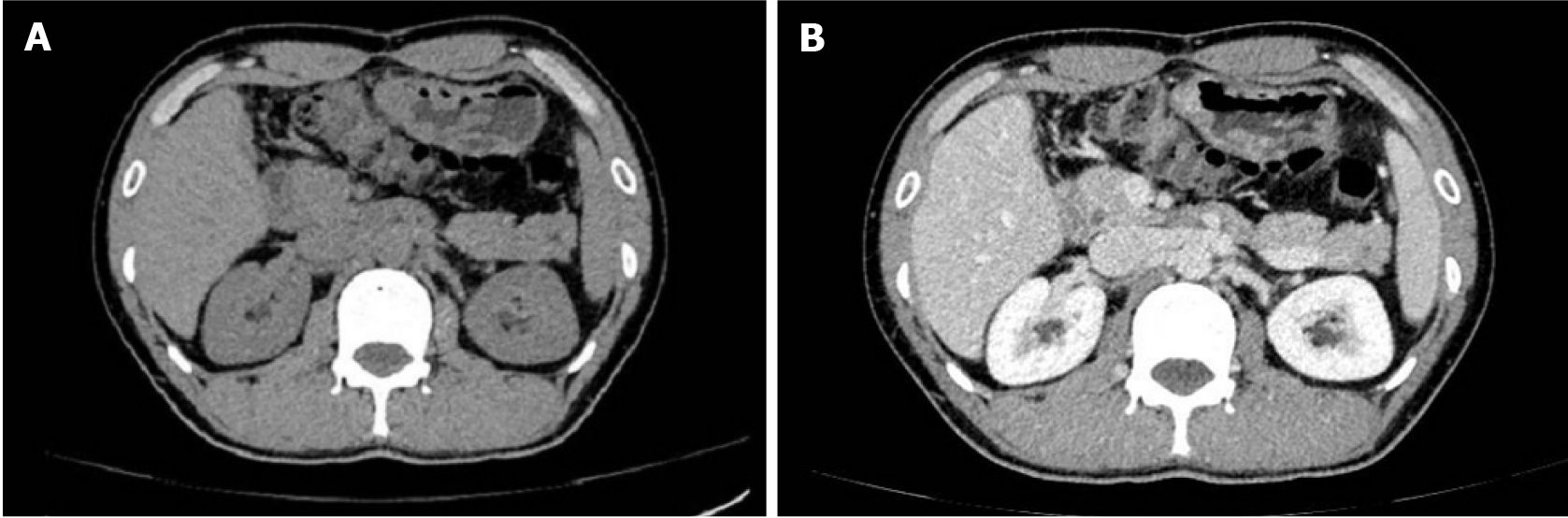
Abdominal CT: On January 25, 2021 (at the local hospital), enhanced CT revealed a huge soft tissue mass near the region of the gastric antrum, pyloric canal, and duodenal bulb. The mass was compressing the surrounding tissues and had unclear boundaries. A portion of the mass (approximately 34 mm × 16 mm) showed an inhomogeneous enhancement in the arterial phase (Figure 1).
After hospitalization, as the abdominal pain and confused state intensified, we reassessed the condition of the abdomen with an emergency CT scan on January 27, 2021. The imaging findings were similar to previous ones, namely a tissue mass (approximately 91 mm × 77 mm × 115 mm) with heterogeneous density was found in the hepatogastric space. It was poorly demarcated from the gastric antrum, and no free air was detected (Figure 1).
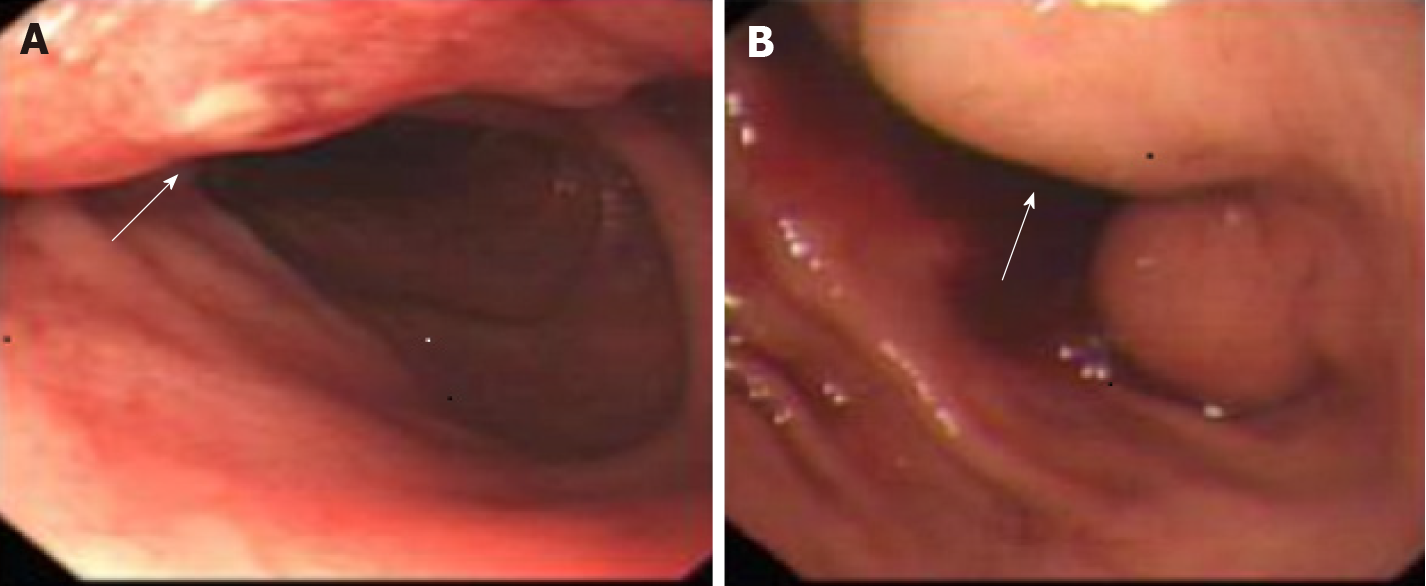
On the day of admission, an ulceration (approximately 1.5 cm × 1.0 cm) was detected in the gastric antrum mucosa during the gastroscopy but no obvious mass was reported. The gastric antrum was deformed and stenosis of bulbus duodeni was observed (Figure 2).
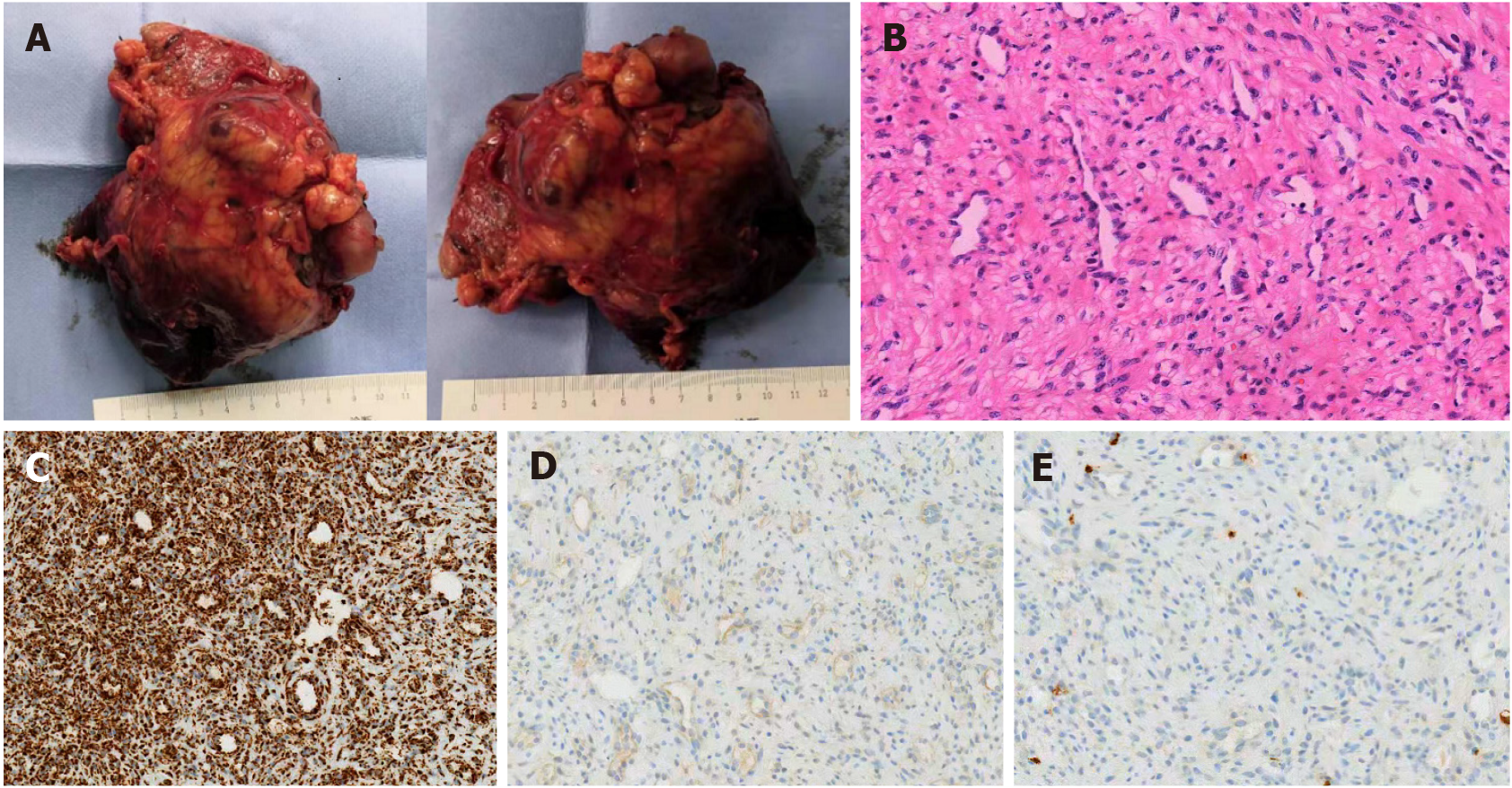
Due to the rarity of this disease, the pathology report was provided for consultation by another tertiary hospital; ultimately, the same opinion was given. On gross pathological examination, an 11 cm × 7 cm × 5 cm tumor could be seen on the serosa of gastro-duodenal junction (Figure 3A). The tumor was elastic in texture and its cut surface was gray-red, with some necrotic rupture and cystic degeneration visible. Also, a rough change was seen on the mucosa where the tumor was located. Microscopically, the hematoxylin/eosin-stained pathological sections’ view revealed the tumor to be composed of spindle cells with clarified cytoplasm, accompanied by myxoid stroma and arborizing blood vessels (Figure 3B). The tumor cells were seen to have infiltrated the mucosa, muscularis, and subserosa, but no apparent atypia of tumor cells was observed. No tumor tissue was found in the resected lymph node (0/1) nor at the gastric and duodenal margins. The pathology of the resected gallbladder showed chronic inflammatory changes without tumor infiltration. Immunohistochemically, the spindle cells were positive for smooth muscle actin and succinate dehydrogenase subunit B (SDHB), and weakly-positive staining was observed for desmin (Figure 3C). Immunohistochemistry staining was negative for S-100, DOG-1, CD10, and β-catenin (Figure 3D). CD34 was positive in the capillary network but was negative in tumor cells. CD117 was positive in mast cells but negative in tumor cells (Figure 3E). The Ki-67 proliferative index was < 1%. In summary, the pathological presentation was deemed to be more consistent with a diagnosis of gastric PF.
After routine preoperative preparation, the patient underwent emergency surgery. During the laparoscopic exploration, it was noted that a huge mass (approximately 9 cm × 12 cm × 5 cm) with thick purulence wrapped the distal stomach and the proximal duodenum. The mass was closely adhered to the gallbladder, with unclear demarcation. Necrotic rupture at the mass and abscess formation were observed intraoperatively. Pus was visible in the pelvic and abdominal cavities. Considering the size of the tumor, we eventually adopted laparotomy to resect the mass, and we performed the distal partial gastrectomy, duodenal bulbectomy, and cholecystectomy. The digestive tract was reconstructed in a Billroth II anastomosis. Repeated flushing of the abdominal cavity with physiological saline was conducted, and a drainage tube was placed before abdomen closure.
Frozen-specimen pathological examination of the resected tissues indicated a spindle cell tumor, consistent with the appearance of GIST cells. The patient received anti-infection therapy and advanced care after surgery but no chemotherapy or radiotherapy.
Following an uneventful recovery, the patient was discharged from the hospital on February 10, 2021. On the 160th day after surgery, he attended follow-up for routine blood test, tumor marker examination, and enhanced CT scan (Figure 4). No signs of tumor recurrence were detected. He was continuing to recover well as of press time.
PF is a rare mesenchymal tumor, with limited reports worldwide. We conducted a database search of PubMed and Web of Science using the terms of “plexiform fibromyxoma” and “plexiform angiomyxoid myofibroblastic tumor”, as of June 2021. at least 13 additional cases were found, published after the review study by Su et al[1], raising the number of reported cases to 134 worldwide. Of the 13 new cases, 9 patients presented with abdominal signs or bleeding symptoms[4,6,7,9-12,15] in Table 1. Others were detected on medical examination performed for other reasons, such as hematuria[12], pharyngeal discomfort[13], and weight loss[14]. From the literature with clinical manifestations available for 108 cases, 86 patients presented as nonspecific gastrointestinal complaints or gastrointestinal hemorrhage, which could indicate that these are the most common symptoms of gastric PF. These manifestations were also reflected in the current case, but the patient’s difficult-to-control infection caused by the ruptured gastric PF was a more notable symptom, which is rare in the disease, causing doctors to face more trouble in the present case. Indeed, it was the infectious shock condition that threatened the patient’s life and forced us to perform emergency surgery.
In known cases, because of the slow-onset process, patients have rarely presented with severe infections or required emergency surgery for gastric PF. We only found a single definitive case[1] of emergency surgery for gastric perforation and a single case[16] showing evident manifestation of infection. As such, this may be the first case report worldwide of emergency surgery performed for ruptured gastric PF with severe infection. The nonspecific and uncommon symptoms of this rare disease pose a challenge in diagnosis and tend to delay treatment. Thus, gastric PF, especially huge gastric PF, may also pose a risk of rupture, necrosis, and serious infection for potentially life-threatening conditions. Timely surgery is the treatment approach that should be considered first. Otherwise, pyemia and abscess, that may prove difficult to control with medication, will follow.
In terms of the auxiliary examination of gastric PF, CT has always been an important examination in most case reports. Of the 13 additional cases, 10 of the 11 underwent CT examinations, excluding the 2 cases of PF found by review of previous pathology reported by Arslan et al[12]. It was also CT that enabled us to find the mass in the case we report herein. Gastroscopy allows direct observation of the gastric mucosa. However, we did not see an observable mass in the patient’s gastric mucosa during gastroscopy. We only observed ulceration and a deformed digestive tract via gastroscopy, while the presence of a large mass was confirmed by CT. The later pathological examination corroborated the gastroscopic findings. This may suggest that PF could grow out of the intestinal wall and form a huge mass but with rare changes in gastric mucosa. Therefore, we should be alert to the possibility of an extra-intestinal neoplasm, even if only tiny changes in the mucosa are observed during the gastroscopy examination of the gastric PF.
As of now, no cases have been found where gastric PF was diagnosed before the pathological examination. In the absence of a specific clinical presentation, path-ological examination remains the only means of confirming the disease. However, the rarity of the disease poses a diagnostic challenge, especially to inexperienced pathologists. In our case, although frozen pathology was routinely performed intraoperatively, we still mistook the mass for a GIST until the paraffin-embedded section pathology report. We need to distinguish between gastric PF and GIST, which is the most common mesenchymal tumor of the gastrointestinal tract. In addition to the characteristic view under the microscope, immunohistochemistry is an important method to differentiate gastric PF from GIST. Including the 13 new cases published after the study by Su et al[1], no detection of DOG-1 or CD117, which are both markers for GIST, were reported for the tumor cells. This case did not overturn the previous immunohistochemical findings of PF. In fact, they still may be the most practical markers to differentiate gastric PF from GIST. Furthermore, it is noteworthy that SDHB was positive in our case, and this test item was the first to be reported in PF cases. Negative SDBH has been identified in SDH-deficient GIST, pheochromocytoma, neuroblastoma[17], and so on. SDHB may also allow PF to be distinguished from some primary tumors, but determination of its significance will require further research.
COVID-19 vaccination has proven to be an effective measure to reduce mortality and contain the spread of COVID-19. In our case, we noted that the patient had a history of COVID-19 vaccination (inactivated vaccine produced by “Beijing Biology”) prior to the acute onset of the disease. We attempted to investigate their connection, if any, but we did not find any evidence of a causal relationship between them. We have also found no reports of abdominal infections among the adverse reactions to this vaccine. We speculate that this may just be a coincidence. We present this pheno-menon here, but whether COVID-19 vaccination was involved in the acute onset of gastric PF deserves further research.
Gastric PF that manifests as tumor rupture combined with pyemia is rare, and timely surgery is critical for optimal prognosis of these patients.
The authors wish to acknowledge the work of staff at The First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China (a tertiary hospital) for their review and confirmation of our patient’s diagnosis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Elpek GO S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Su HA, Yen HH, Chen CJ. An Update on Clinicopathological and Molecular Features of Plexiform Fibromyxoma. Can J Gastroenterol Hepatol. 2019;2019:3960920. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 2. | Takahashi Y, Shimizu S, Ishida T, Aita K, Toida S, Fukusato T, Mori S. Plexiform angiomyxoid myofibroblastic tumor of the stomach. Am J Surg Pathol. 2007;31:724-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 78] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 3. | Miettinen M, Makhlouf HR, Sobin LH, Lasota J. Plexiform fibromyxoma: a distinctive benign gastric antral neoplasm not to be confused with a myxoid GIST. Am J Surg Pathol. 2009;33:1624-1632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 94] [Article Influence: 5.9] [Reference Citation Analysis (1)] |
| 4. | Magadán Álvarez C, Olmos-Martínez JM, Toledo Martínez E, Trugeda Carrera MS, Fernández Díaz MJ, Martín Rivas B, Mazorra Horts R, Mayorga Fernández MM, Arias Pacheco RD. Gastric plexiform fibromyxoma, an uncommon mesenchymal tumor. Rev Esp Enferm Dig. 2021;113:183-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Pei JY, Tan B, Liu P, Cao GH, Wang ZS, Qu LL. Gastric plexiform fibromyxoma: A case report. World J Clin Cases. 2020;8:5639-5644. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Nasralla A, Alwabari M, Alsaif O, Amr SS. Gastric Plexiform Fibromyxoma Arising in the Cardia in an Adolescent Male: A Rare Tumor with an Unusual Location. Case Rep Surg. 2020;2020:9037960. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Martí Gelonch L, Asensio Gallego JI, Eizaguirre Letamendia E, Enríquez-Navascués JM. Giant gastric plexiform fibromyxoma. Cir Esp (Engl Ed). 2021;99:306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Vieites Branco I, Silva JC, Pinto F, Pires F, Almeida A. Rare mesenchymal antral gastric tumors: Case reports of glomus tumor and plexiform fibromyxoma. Radiol Case Rep. 2020;15:71-76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Tang J, Liu F. Plexiform Fibromyxoma: A Rare Mesenchymal Tumor Found in the Esophagus. Am J Gastroenterol. 2020;115:648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Hong YP, Yu J, Wang CY, Su YR, Chen C, Deng WH, Wang WX. Plexiform Fibromyxoma of the Stomach. J Gastrointest Surg. 2020;24:909-912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Gan Y, Hammoud G, Esebua M. A rare case of plexiform fibromyxoma in stomach: FNA diagnosis with histological correlation and differential diagnoses. Ann Diagn Pathol. 2020;44:151453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Arslan ME, Li H, Jennings TA, Lee EC, Nigam A, Lee H. Frequency of Plexiform Fibromyxoma relative to gastrointestinal stromal tumor: A single center study. Ann Diagn Pathol. 2020;48:151568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Kobori I, Katayama Y, Hayashi K, Fujimoto Y, Kaneko M, Kitahama A, Kitagawa T, Imada H, Ban S, Tamano M. Uninodular Fibromyxomatous Gastric Tumor Resected by Endoscopic Submucosal Dissection. Intern Med. 2019;58:2015-2018. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Perry L, McCann C, Schwartz J, Gott M, Senatore P, Slotman G. Plexiform Angiomyxoid Myofibroblastic Tumor of the Stomach. Am Surg. 2020;3134820951487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Li Z, Jiang Q, Guo D, Peng Y, Zhang J, Chen X. Gastric Plexiform Fibromyxoma with Two Different Growth Patterns on Histological Images: a Case Report. J Gastric Cancer. 2021;21:213-219. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Lee PW, Yau DT, Lau PP, Chan JK. Plexiform fibromyxoma (plexiform angiomyxoid myofibroblastic tumor) of stomach: an unusual presentation as a fistulating abscess. Int J Surg Pathol. 2014;22:286-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Zhao T, Mu X, You Q. Succinate: An initiator in tumorigenesis and progression. Oncotarget. 2017;8:53819-53828. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 84] [Article Influence: 10.5] [Reference Citation Analysis (0)] |