Published online Mar 6, 2022. doi: 10.12998/wjcc.v10.i7.2229
Peer-review started: August 26, 2021
First decision: October 22, 2021
Revised: November 29, 2021
Accepted: January 22, 2022
Article in press: January 22, 2022
Published online: March 6, 2022
Processing time: 187 Days and 19 Hours
Patients with severe periodontitis often require multidisciplinary treatment to achieve healthy periodontal tissue, normal occlusion, and optimal aesthetics. In the present study, we aimed to evaluate the efficacy of multidisciplinary non-surgical treatment in a patient with stage IV/ grade C periodontitis, malocclusion, and dentition defects.
A 47-year-old woman visited our periodontology department due to teeth mobility problems and difficulties chewing food. The patient had no history of drug allergies or systemic disease. Initial therapy involved scaling and root planning with a Gracey scaler and periodontal ultrasonic therapeutic apparatus using a periodontal endoscope (Perioscopy, Zest Dental Solutions, United States) to control the periodontal inflammation prior to treatment. Five months later, orthodontic treatment was then performed to treat occlusion and overall aesthetics. After completion, a Maryland bridge was used to restore Nos. 22, 31, and 41 teeth. Florida probing (Florida probe, United States) was performed every 2-3 mo to evaluate the periodontal condition throughout treatment. Overall, multidisciplinary non-surgical treatment resulted in satisfactory aesthetic results with healthy periodontal tissue and stable occlusion.
In some patients with stage IV/grade C periodontitis, systematic and sequential non-surgical treatment can provide excellent therapeutic results.
Core Tip: We present a case of severe periodontitis treated with standardized multidisciplinary therapy, with excellent therapeutic effects. This case report offers new insight into the treatment of patients with stage IV/ grade C periodontitis, highlighting the potential of a systematic and sequential non-surgical approach.
- Citation: Li LJ, Yan X, Yu Q, Yan FH, Tan BC. Multidisciplinary non-surgical treatment of advanced periodontitis: A case report. World J Clin Cases 2022; 10(7): 2229-2246
- URL: https://www.wjgnet.com/2307-8960/full/v10/i7/2229.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i7.2229
Periodontitis is a chronic inflammatory disease caused by plaque microorganisms that can lead to periodontal tissue inflammation and alveolar bone loss. If untreated, periodontitis increases the risk of loose teeth and subsequent tooth loss[1]. Global epidemiological studies have shown a high prevalence of periodontitis in various countries including China, America, and Britain[2,3]. In addition to initial treatment, periodontal surgery is often required to completely remove local inflammatory stimulation and restore the normal appearance of periodontal soft and hard tissue[4]. However, in patients with severe periodontitis, sequential periodontal treatment usually requires a range of periodontal surgery and high expenditure, which many patients cannot afford. Meanwhile, studies have also shown that subgingival scaling and root debridement with periodontal endoscopy can have a similarly positive therapeutic effect[5].
Occlusion disorder problems often occur in patients with severe periodontitis, while secondary occlusal trauma can aggravate the destruction of periodontal tissue; however, both can be treated orthodontically[6]. Sim et al[6] and Angelina et al[7] have both reported that orthodontic treatment will not exacerbate periodontal destruction if the periodontal inflammation and plaque are initially controlled. Moreover, postoperative stable occlusion was found to promote periodontal tissue recovery.
However, in patients with advanced periodontitis, choosing an appropriate prosthetic treatment plan can be difficult when considering restoration of the denture deficiency, minimization of damage to the abutment teeth, and increasing the stability of the periodontal tissue. A recent study showed that fixed prosthodontic treatment in compliant patients is highly successful after 20 years of supportive periodontal care[8]. Moreover, several studies have also demonstrated that prosthodontics need to be designed according to the periodontal conditions of the patient, with different fixed dental prostheses having an effect on the periodontium[9-12]. The Maryland bridge has also been suggested in such cases, providing restoration of missing teeth with long-term stability[13].
In this case report, we present a patient with stage IV/ grade C periodontitis who achieved a good treatment outcome following nonsurgical periodontal treatment, orthodontic treatment, and prosthodontic treatment with a Maryland bridge, bringing new insight into the treatment of advanced periodontal disease.
A 47 year old woman with no medical history presented to our hospital for teeth mobility problems.
While collecting detailed medical history, the patient complained of long-term problems with tooth loss and difficulties chewing. The patient had undergone no previous oral therapy, and sought treatment due to recent worsening of her chewing difficulties. The patient had mild halitosis and occasional bleeding during tooth brushing.
The patient had no significant medical history.
The patient had no significant personal or family history.
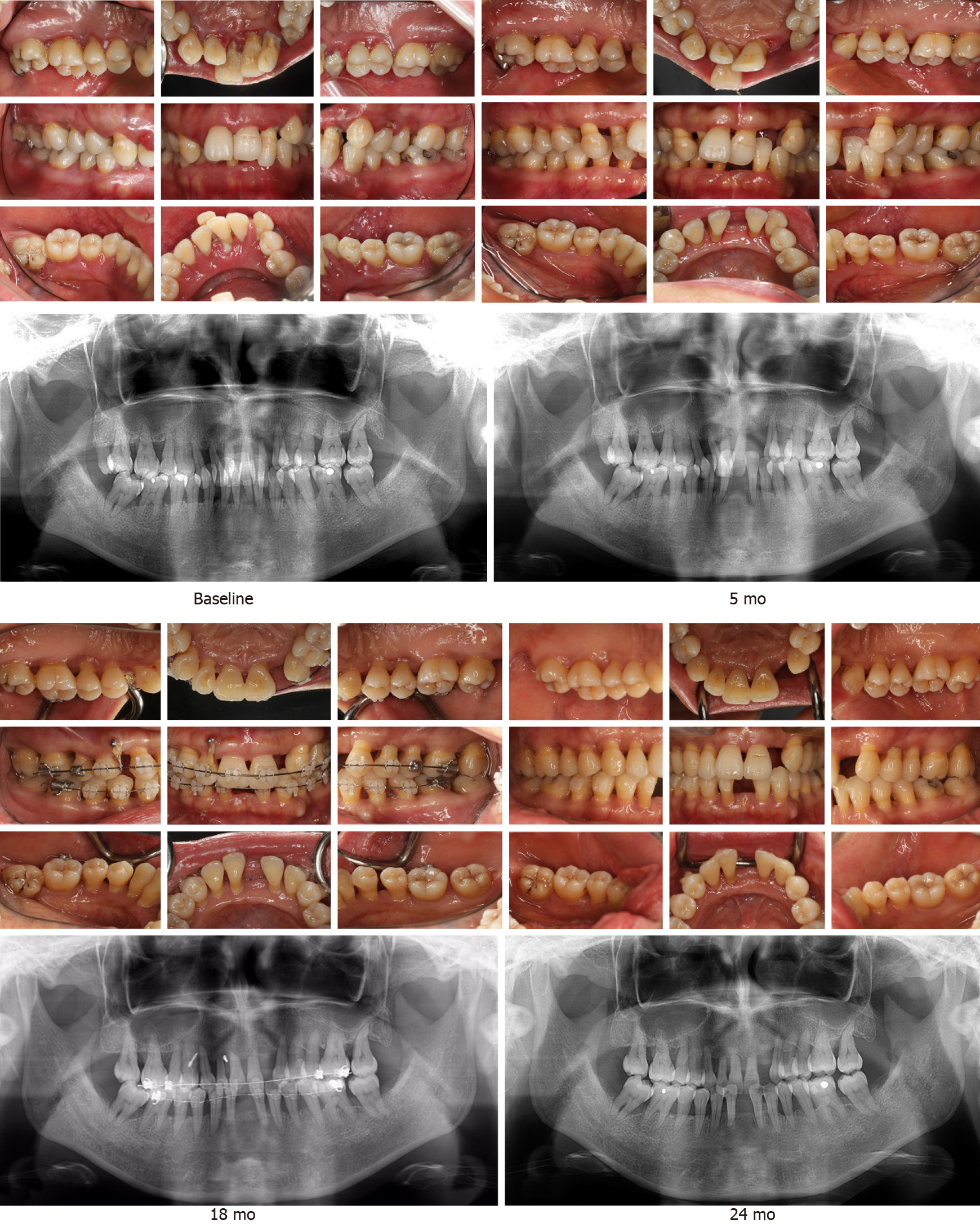
In the clinical examination, we identified poor oral hygiene with a large amount of dental calculus and obvious plaque retention. The gingiva tissues appeared tender and edematous (Figure 1). No. 21 tooth was distinctly labially inclined, while Nos. 31 and 41 were extremely loose. Overall, 83% of her teeth (25 teeth) showed mobility ≥ I°, and more than 50% presented a probing depth (PD) of > 4 mm with positive bleeding on probing (BOP). According to the “Classification of Periodontal and Peri-Implant Diseases and Conditions” in 2017[14] and the Angle classification[15], the patient was diagnosed with: (1) Periodontitis stage IV/ grade C; (2) angle class III skeletal malocclusion, with maxillary and mandibular prognathism; and (3) moderate crowded malocclusion. A therapeutic plan was subsequently proposed by a team of periodontists, orthodontists, and a prosthodontist. In view of her periodontal condition and dental calculus, supragingival ultrasonic scaling was carried out ahead of detailed examination in order to provide a baseline level 1 wk later.
Preoperative panoramic radiographs (Figure 1 baseline) revealed that the full mouth alveolar bone was absorbed to varying degrees into the middle 1/2 and apical 1/3 of the root, with Nos. 22 and 31 teeth absorbed into the apical region.
The patient approved the treatment plan and provided signed informed consent for inclusion in this case report. The report was reviewed and approved by the Ethics Committee of Nanjing Stomatological Hospital, Medical School of Nanjing University (Nanjing, China).
Oral hygiene (plaque assessment): Oral hygiene and the amount of plaque near the gingival margin were examined by visual inspection and probing.
Florida probe: The Florida probe, a computerized system that transfers periodontal pressure-sensitive probing and charting systems into a graphical representation, was used throughout periodontal treatment. The system stores digital records of each periodontal treatment session, allowing the effectiveness of a course of treatment to be monitored.
Periodontal pocket depth: A periodontal probe was inserted into the periodontal pocket parallel to the long axis of the tooth. The periodontal pocket was then probed to determine the depth of central, mesial, and distal sites on the labial/buccal and lingual/palatal sides of the tooth, respectively.
Tooth mobility assessment: Forceps were placed around the incisal margins of the anterior teeth and then closed around the posterior teeth. The teeth were then moved in a buccal-lingual or mesial-distal direction with the forceps tip against the occlusal fossa and graded as follows: Ⅰ°, mobility within 1 mm or only in a buccal-lingual direction; Ⅱ°, mobility within a range of 1-2 mm or in buccal-lingual and mesial-distal directions; Ⅲ°, mobility greater than 2 mm in buccal-lingual, mesial-distal, and vertical directions.
Bleeding on probing: A probe was inserted into the base of the periodontal pocket or the sulcus then removed, and the gingival margin was observed for bleeding.
X-ray evaluation: Periodontal hard tissues, notably the alveolar bone, was visualized using panoramic and apical radiographs.
Based on the clinical and imaging examinations, a final periodontal diagnosis of periodontitis (stage Ⅳ, grade C)/extensively severe chronic periodontitis and a final orthodontic diagnosis of Angle class Ⅰ neutroclusion were made.
Intraoral images obtained at the first visit showed a poor level of oral hygiene, a large amount of dental calculus, and obvious plaque retention (Figure 1). No. 21 tooth was distinctly labially inclined and Nos. 31 and 41 were extremely loose.
The overall aim was to improve the periodontal condition and encourage efficient oral hygiene habits and plaque control. The aesthetic needs of the patient and problems with occlusion were also considered.
At the beginning of treatment, the patient showed a desire to maintain her teeth and refused periodontal surgery. The therapeutic plan therefore consisted of: (1) Non-surgical initial periodontal therapy, with supra- and subgingival scaling, and root debridement using a periodontal endoscope; (2) orthodontic treatment aimed at improving occlusion and aesthetics; and (3) suitable prosthodontic treatment (i.e., Maryland fixed bridge restoration). The patient’s clinical index was continuously monitored and risk assessment was carried out throughout treatment, which lasted 38 mo. The treatment plan is shown in Figure 2.
Initial periodontal therapy was based on mechanical removal of bacterial plaque via nonsurgical treatment, with standardized supra and subgingival scaling plus root planning (SRP). During the second visit, Nos. 22, 31, and 41 teeth were subsequently extracted. To achieve total calculus removal, SRP was carried out using a periodontal endoscope in sites with pockets ≥ 5 mm. Two weeks later, the patient underwent a session of professional plaque control, including reinforcement of oral hygiene processes via monthly checks and the use of plaque disclosing agents to facilitate daily examinations. Twelve weeks after completion of active therapy, the periodontal inflammation was deemed under control. Positive BOP sites were reduced by 86%-39%, and the plaque index showed that the plaque accumulation markedly decreased by 100%-17%, with a reduction in deep pockets ≥ 5 mm of 63%-2%. Orthodontic treatment was therefore initiated, with thorough examination and risk assessment using a Florida probe (Figure 3). A marked reduction in periodontal pockets was observed while probing; however, her risk assessment level remained high before orthodontic treatment, decreasing to moderate after 13-mo treatment (Figure 3A and B). The patient was recalled for periodontal maintenance every 3 mo throughout orthodontic therapy, at which point her periodontal parameters were examined and any changes in her condition were recorded. Positive therapeutic effects with a low risk assessment level and overall improvements in PD were ultimately achieved (Figure 4).
After systematic periodontal therapy, a stable periodontal condition was achieved despite some teeth remaining mobile. We therefore consulted orthodontics for a critical evaluation, which highlighted that no tooth movement to the labial-buccal side was required during orthodontics, and therefore, there was no increased risk of loosening. Instead, the plan was considered beneficial in terms of stabilization following improvements to the occlusal relationship.
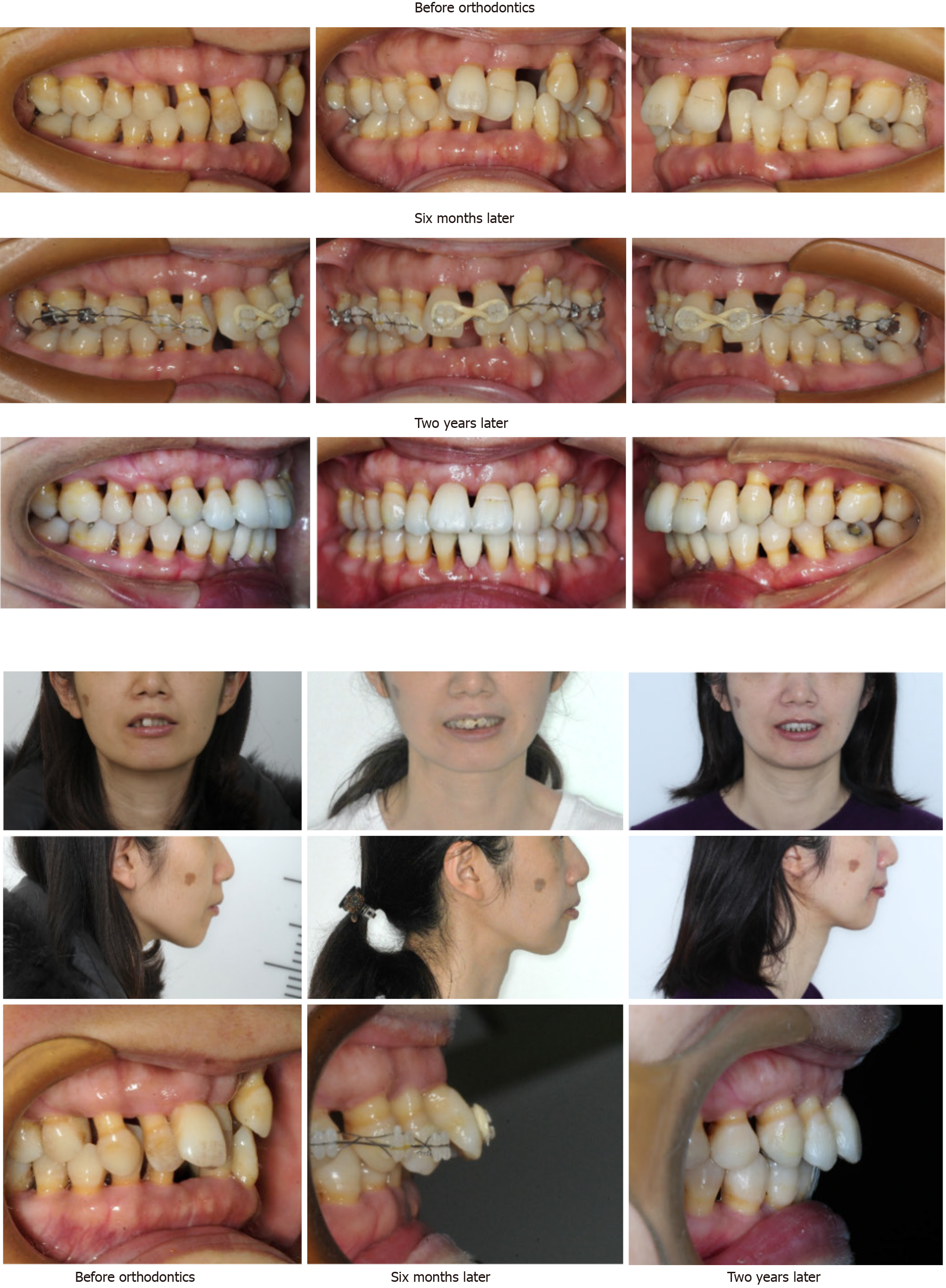
In order to correct the malocclusion and achieve a satisfactory occlusal relationship, orthodontic treatment was performed to initially align the teeth and then straighten the maxillary anterior teeth. Nickel titanium wires were used for alignment of the arches and interactive traction elastics were used for correction of the incisor position. The final duration of orthodontic treatment was 19 mo. The aesthetic profile was enhanced and the radiographic bone density increased in the molar region following periodontal and orthodontic treatment (Figure 5). Figure 6 shows intraoral and extraoral images obtained during treatment.
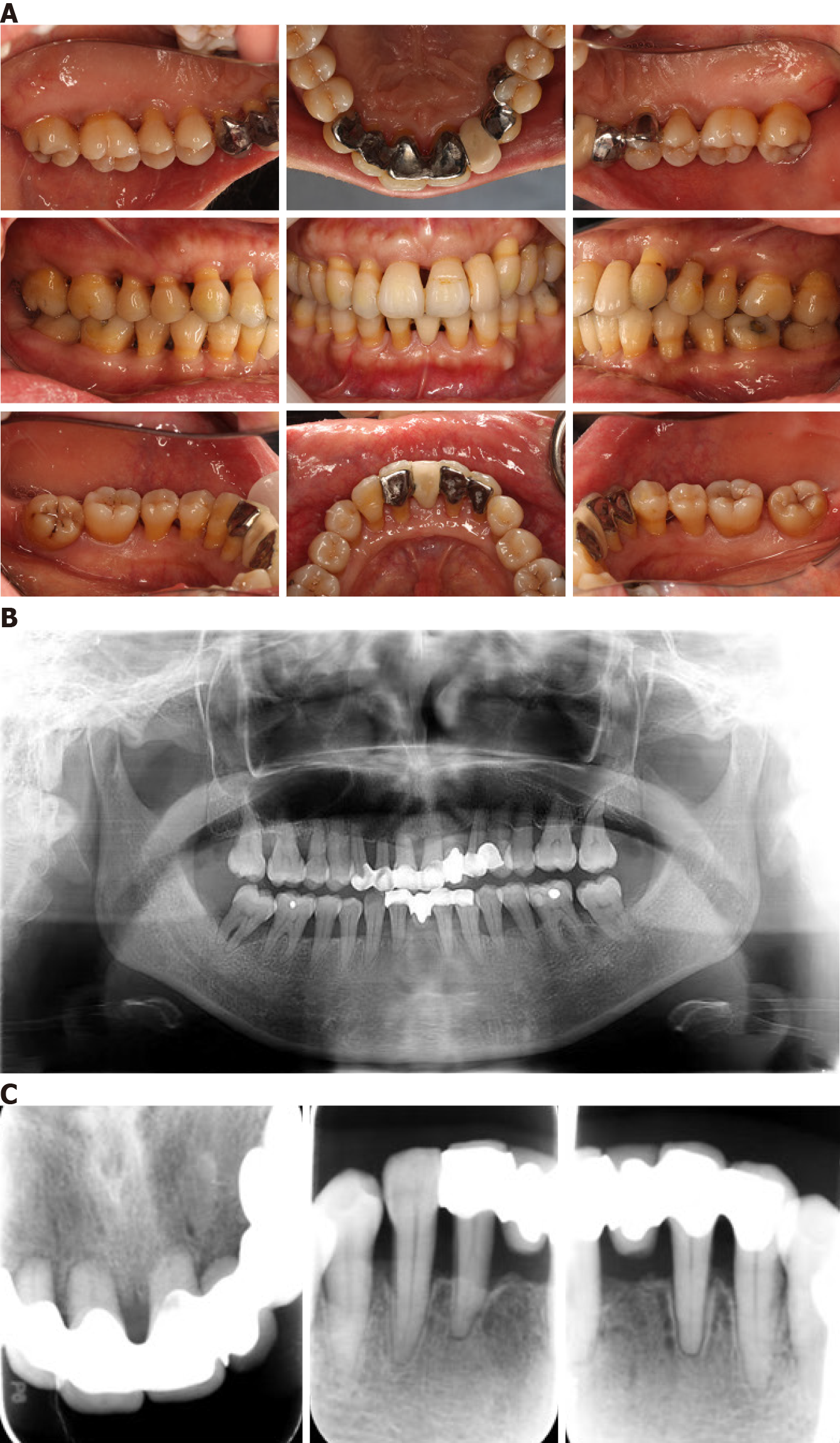
After the completion of non-surgical periodontal and orthodontics treatment, the patient was referred to the department of prosthodontics for establishment of a prosthodontic treatment plan. Considering the compromised periodontal situation and tooth mobility problems, a Maryland bridge was selected on one side to provide full dentition, while on the other side, dental splints were used to fix the loose teeth (Figure 7). Eight months after treatment, the periodontal condition remained satisfactory and stable (Figure 8).
After completing prosthodontic treatment, the patient was called for follow-up visits every 3 mo, with intraoral images obtained after 8 mo. Periodontal examination with risk assessment was also performed using a Florida probe (Figure 8), revealing a stable periodontal condition and good plaque control. Another 6 mo later, radiographic data and additional intraoral images were obtained (Figure 9), revealing a continuous stable periodontal condition with no additional alveolar bone loss.
Supra- and subgingival scaling with root planning was initially performed using a periodontal endoscope, which took 5 mo. An obvious improvement in the patient’s periodontal condition was revealed in terms of BOP and PD, and the high-risk assessment result decreased remarkably to low risk after 2-year treatment. Subsequently, based on the patient’s desire for straightening teeth, consultation with the orthodontic doctor, and evaluation of the risk of orthodontic treatment, 19 mo of orthodontic treatment was commenced, providing excellent treatment effects. Obvious root absorption in the upper anterior teeth was observed in addition to an unusual root morphology.
Traditional periodontal treatment usually consists of four stages: Initial therapy, periodontal surgery, restorative therapy, and supportive periodontal therapy[16]. The aim of the second stage, periodontal surgery, is thorough debridement and restoration of the physiological morphology and function of the periodontal tissue. In this case study, we initially carried out supra- and subgingival scaling with root planing using a periodontal endoscope for 5 mo. Compared with general treatment, subgingival scaling and debridement with the aid of a periodontal endoscope are more thorough, offering a more efficient and minimally invasive approach for controlling periondontal inflammation. The main advantage of periodontal endoscopy is subgingival treatment with real-time image support[5], which directly displays the subgingival scaling process and therapeutic effect. This support is impractical with traditional treatment of, for example, deep periodontal pocket bottoms and multiple root bifurcations[17]. Periodontal endoscopic techniques can also reduce the risk of periodontal surgery and associated complications[18].
After completing initial treatment, re-evaluation is important, especially with severe periodontitis. In this case study, obvious improvement in the patient’s periodontal condition was revealed, both in terms of BOP and PD, and the high-risk assessment result decreased remarkably to low risk after 2-year treatment. Moreover, the patient adopted a greatly improved oral hygiene routine. These re-assessment results are pivotal in determining the subsequent treatment plan. At present, the commonly accepted indicators representing the so-called "treatment endpoint" include: (1) No BOP; and (2) a PPD ≤ 4 mm[8]. A large number of long-term clinical studies have shown that patients with severe periodontitis who show good plaque control and receive only normative non-surgical periodontal treatment can achieve notable improvements in their periodontal condition[19]. For example, Barros et al[20] showed that non-surgical periodontal treatment alone could result in improvements in alveolar bone density.
In our case, 19 mo of orthodontic treatment provided excellent treatment effects. Orthodontic treatment can re-arrange the dentition, eliminate occlusal trauma, restore stability, and disperse the occlusal force, all of which are crucial in gaining healthy periodontal soft and hard tissue[6]. The precondition of orthodontic treatment is control of periodontal inflammation, which, if not achieved, can result in treatment failure or even accelerate periodontal destruction[21]. In patients with moderate to severe periodontal disease, periodontal-orthodontic treatment can not only correct malocclusion, but also significantly improve periodontal health[22]. Findings suggest that the performance of PD, plaque index, clinical attachment level, and the sulcus bleeding index of patients treated with combined orthodontic-periodontic treatment were much better than those treated with basic periodontics[23]. Notably, patients with periodontal disease must follow the principle of light force correction. Orthodontic forces are transmitted through periodontal fibers, which are the basis of tooth movement. The amount of orthodontic force depends on the periodontal ligament area of the teeth. If the alveolar bone height is reduced by 50%, the periodontal ligament area is reduced by 75%, leaving only 25%, and the orthodontic force should therefore be reduced to 25 rather than 50%. The orthodontic forces should therefore be determined according to the amount of residual alveolar bone[24]. In this case study, obvious root absorption in the upper anterior teeth was observed in addition to an unusual root morphology. It was previously reported that pointed and tapered apical morphologies are more likely to result in increased root absorption during orthodontic treatment[25,26].
It is often challenging to decide an appropriate prosthodontic treatment plan for patients with periodontitis resulting from a poor periodontal condition. However, with the development of oral prosthetics and manufacturing processes, even patients with severe periodontitis can undergo fixed denture restoration if the periodontal condition of the abutment teeth remains stable and meets the standard of clinical fixed denture abutment[8]. Fixed denture repair is more comfortable than removable dentures, and can improve periodontal tissue repair and the prognosis of loose teeth. Adhesive fixed dentures result in less teeth grinding and cutting, and do less harm to the abutment teeth. Corrente et al[27] carried out a 10-year observational study of patients with periodontitis treated with bonded dentures, and revealed a cumulative denture survival rate of 76.2%. The Maryland bridge is widely used due to the minimal tooth preparation and subsequent reduction in pain. It is important to consider abutment teeth as much as possible during design since they act as periodontal splints, avoiding occlusal trauma and working as an entirety to restore the function and appearance of the missing teeth[28].
Overall, through multidisciplinary therapy lasting 38 mo and consisting of periodontal, orthodontic, and prosthodontic treatment, excellent therapeutic results were obtained in terms of aesthetics and occlusion. This case report highlights, therefore, that even in patients with severe periodontitis, by following serialized treatment and strict plaque control, non-surgical periodontal treatment can dramatically improve the overall periodontal condition and provide satisfactory therapeutic results.
In practice, to improve the treatment success of advanced periodontitis, a multidisciplinary approach involving orthodontics, prosthodontics, and endodontics is required. This case report offers new insight into the treatment of patients with advanced periodontitis, highlighting the potential of systematic and sequential non-surgical therapy.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Nanjing Stomatological Hospital, Medical School of Nanjing University.
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ghaffar KA, Heboyan A, Meqa K S-Editor: Ma YJ L-Editor: Wang TQ P-Editor: Ma YJ
| 1. | Borgnakke WS. Does Treatment of Periodontal Disease Influence Systemic Disease? Dent Clin North Am. 2015;59:885-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 50] [Article Influence: 5.0] [Reference Citation Analysis (1)] |
| 2. | Martins MD, Jiao Y, Larsson L, Almeida LO, Garaicoa-Pazmino C, Le JM, Squarize CH, Inohara N, Giannobile WV, Castilho RM. Epigenetic Modifications of Histones in Periodontal Disease. J Dent Res. 2016;95:215-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 87] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 3. | GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1211-1259. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5428] [Cited by in RCA: 5098] [Article Influence: 637.3] [Reference Citation Analysis (0)] |
| 4. | Rios HF, Lin Z, Oh B, Park CH, Giannobile WV. Cell- and gene-based therapeutic strategies for periodontal regenerative medicine. J Periodontol. 2011;82:1223-1237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 87] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 5. | Kuang Y, Hu B, Chen J, Feng G, Song J. Effects of periodontal endoscopy on the treatment of periodontitis: A systematic review and meta-analysis. J Am Dent Assoc. 2017;148:750-759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (1)] |
| 6. | Sim HY, Kim HS, Jung DU, Lee H, Lee JW, Han K, Yun KI. Association between orthodontic treatment and periodontal diseases: Results from a national survey. Angle Orthod. 2017;87:651-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (1)] |
| 7. | Gorbunkova A, Pagni G, Brizhak A, Farronato G, Rasperini G. Impact of Orthodontic Treatment on Periodontal Tissues: A Narrative Review of Multidisciplinary Literature. Int J Dent. 2016;2016:4723589. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 8. | Di Febo G, Bedendo A, Romano F, Cairo F, Carnevale G. Fixed prosthodontic treatment outcomes in the long-term management of patients with periodontal disease: a 20-year follow-up report. Int J Prosthodont. 2015;28:246-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Vliegenthart JF. Studies on glycoprotein-derived carbohydrates. Biochem Soc Trans. 1994;22:370-373. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 10. | Uccella R, Zibetti E, Gaiazzi M. [Major histocompatibility complex antigens in a population of insulin-dependent diabetics living in the Province of Varese]. Minerva Med. 1994;85:71-76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 11. |
Heboyan A, Manrikyan M, Markaryan M, and Vardanyan I, Changes in the Parameters of Gingival Crevicular Fluid in Masticatory Function Restoration by Various Prosthodontic Constructions.
|
| 12. | Freeman S. Occupational skin disease. Curr Probl Dermatol. 1995;22:80-85. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 13. | Kathariya R, Devanoorkar A, Golani R, Shetty N, Vallakatla V, Bhat MY. To Splint or Not to Splint: The Current Status of Periodontal Splinting. J Int Acad Periodontol. 2016;18:45-56. [PubMed] |
| 14. | Papapanou PN, Sanz M, Buduneli N, Dietrich T, Feres M, Fine DH, Flemmig TF, Garcia R, Giannobile WV, Graziani F, Greenwell H, Herrera D, Kao RT, Kebschull M, Kinane DF, Kirkwood KL, Kocher T, Kornman KS, Kumar PS, Loos BG, Machtei E, Meng H, Mombelli A, Needleman I, Offenbacher S, Seymour GJ, Teles R, Tonetti MS. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol. 2018;89 Suppl 1:S173-S182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 660] [Cited by in RCA: 1237] [Article Influence: 176.7] [Reference Citation Analysis (1)] |
| 15. | Du SQ, Rinchuse DJ, Zullo TG. Reliability of three methods of occlusion classification. Am J Orthod Dentofacial Orthop. 1998;113:463-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 16. | Bartold PM, Gronthos S, Ivanovski S, Fisher A, Hutmacher DW. Tissue engineered periodontal products. J Periodontal Res. 2016;51:1-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 80] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 17. | Ganesh PR, Karthikeyan R, and Malathi K. Perio-Scopy: A New Paradigm in Periodontal Therapy. International Journal of Dental and Medical Research 2015; 1: 168-171. |
| 18. | Sanz I, Alonso B, Carasol M, Herrera D, Sanz M. Nonsurgical treatment of periodontitis. J Evid Based Dent Pract. 2012;12:76-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 97] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 19. | Aimetti M. Nonsurgical periodontal treatment. Int J Esthet Dent. 2014;9:251-267. [PubMed] |
| 20. | de Barros FC, Braga FF, Fischer RG, Figueredo CM. Effects of nonsurgical periodontal treatment on the alveolar bone density. Braz Dent J. 2014;25:90-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | Kloehn JS, Pfeifer JS. The effect of orthodontic treatment on the periodontium. Angle Orthod. 1974;44:127-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 22. | Re S, Corrente G, Abundo R, Cardaropoli D. Orthodontic treatment in periodontally compromised patients: 12-year report. Int J Periodontics Restorative Dent. 2000;20:31-39. [PubMed] |
| 23. | Maeda S, Maeda Y, Ono Y, Nakamura K, Sasaki T. Interdisciplinary treatment of a patient with severe pathologic tooth migration caused by localized aggressive periodontitis. Am J Orthod Dentofacial Orthop. 2005;127:374-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.1] [Reference Citation Analysis (1)] |
| 24. | Christensen L, Luther F. Adults seeking orthodontic treatment: expectations, periodontal and TMD issues. Br Dent J. 2015;218:111-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 48] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 25. | Dindaroğlu F, Doğan S. Root Resorption in Orthodontics. Turk J Orthod. 2016;29:103-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (1)] |
| 26. | Krishnan V. Root Resorption with Orthodontic Mechanics: Pertinent Areas Revisited. Aust Dent J. 2017;62 Suppl 1:71-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (1)] |
| 27. | Corrente G, Vergnano L, Re S, Cardaropoli D, Abundo R. Resin-bonded fixed partial dentures and splints in periodontally compromised patients: a 10-year follow-up. Int J Periodontics Restorative Dent. 2000;20:628-636. [PubMed] |
| 28. | Prathyusha P, Jyoti S, Kaul RB, Sethi N. Maryland Bridge: An Interim Prosthesis for Tooth Replacement in Adolescents. Int J Clin Pediatr Dent. 2011;4:135-138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |