Published online Feb 26, 2022. doi: 10.12998/wjcc.v10.i6.1991
Peer-review started: August 23, 2021
First decision: November 7, 2021
Revised: November 12, 2021
Accepted: January 19, 2022
Article in press: January 19, 2022
Published online: February 26, 2022
Processing time: 184 Days and 12.3 Hours
Median arcuate ligamentum syndrome (MALS) is a disease entity with unclear pathogenesis. If it is not considered in advance, the clinical diagnosis of the disease is very difficult because patients complain of digestive discomfort including pain. However, this characteristic is not specific to MALS. There have been no studies to assist in making a quick diagnosis. The aim of this case series was to recognize that MALS must be considered as a differential factor in the cause of abdominal pain.
We described cases in which four patients complained of abdominal pain over a long period but in whom a diagnosis of MALS could not be made. If the gastroenterologist does not take into account abdominal pain in advance, the patient is considered an asymptomatic gallstone patient and has their gallbladder removed despite imaging evaluation. The patient may also be considered a psychiatric patient and may be administered psychiatric drugs over a long period. In all four cases in this report, the patients experienced abdominal pain. In three cases, the diagnosis was possible by the clinician’s judgment considering both clinical symptoms and imaging techniques shortly after the onset of symptoms. However, in one case that lasted over 20 years, a clear diagnosis was not possible. Even after complaining of colicky pain and performing a cholecystectomy, the diagnosis was made only after the symptoms persisted. In all four cases, the symptoms were relieved by neuromodulators.
MALS is a rare disease and it is easy to miss because it is not malignant, but patients can suffer from pain over a long period. For the accurate diagnosis of a patient complaining of abdominal pain, the diagnosis must be differentiated. In addition, as there are asymptomatic patients, patients who need treatment should be carefully selected, and improvement with medical treatment can be expected. Large-scale studies are also needed.
Core Tip: A considerable number of median arcuate ligamentum syndrome patients are overlooked in the diagnosis of patients complaining of abdominal pain. They are unable to lead a normal life due to severe excruciating pain. However, without an accurate diagnosis, they are misunderstood as symptomatic gallstone patients and have their gallbladder removed or experience pain for a long time. In addition, as the currently known treatment involves surgery based on a mechanistic hypothesis, there are concerns about its complications. Therefore, medical drug treatment should be prioritized to determine whether improvement occurs.
- Citation: Kim JE, Rhee PL. Median arcuate ligamentum syndrome: Four case reports. World J Clin Cases 2022; 10(6): 1991-1997
- URL: https://www.wjgnet.com/2307-8960/full/v10/i6/1991.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i6.1991
Median arcuate ligamentum syndrome (MALS) is a disease entity with unclear pathogenesis[1,2]. If it is not considered in advance, the clinical diagnosis of the disease is very difficult because patients complain of digestive discomfort including pain, but this characteristic is not specific to MALS[3-6]. Most of the studies conducted through a retrospective analysis of incidental celiac artery compression in asymptomatic patients have been imaging studies[7-10], but the data are difficult to apply in actual clinical practice. This is because accidental image discovery does not require treatment. In addition, the surgical cases experienced by many surgeons only concern surgical methods for diseases that have already been diagnosed through complex processes[11,12], and no studies have been conducted to help make a quick diagnosis in these patients.
Therefore, it is necessary to introduce MALS as a causal disease, which should be considered in patients complaining of digestive symptoms at the gastroenterology department. Here, we present four patients diagnosed with MALS.
Case 1: A 63-year-old male patient with no specific medical history visited our clinic complaining of epigastric pain with heartburn symptoms that started 2 years earlier.
Case 2: A 64-year-old female patient, complaining of indigestion for 20 years had been treated for stress-induced gastritis, irritable bowel syndrome with constipation, and reflux esophagitis.
Case 3: A 62-year-old female patient with an underlying alcohol-related disorder complained of indigestion 3 d earlier and took digestive medicines, but there was no improvement.
Case 4: A 47-year-old female patient was admitted with severe abdominal pain that started several years ago.
Case 1: The location of the pain was in the upper abdomen, and the pain lasted for 2 to 3 min. The patient mentioned that the pain intensity sometimes even woke him up and that it subsided when he walked and slightly improved when he bent over. Although he had been administered a proton pump inhibitor (PPI), motility-increasing agent, and mucosal protective agent at local clinics for several years, there was no improvement. Endoscopy and a computed tomography (CT) were already done at other hospitals. The CT readings at the other hospitals showed normal findings and malignancy was excluded.
Case 2: She underwent cholecystectomy at another hospital because of colicky pain, but she was still complaining of unbearable abdominal pain and came to our hospital. Endoscopy and a CT scan were performed again and normal findings were reported.
Case 3: She visited the emergency room for severe abdominal pain but returned home without any specific findings on the CT scan. An outpatient clinic history was done again. Her squeezing pain persisted for more than 10 min at one time and was sometimes accompanied by chills.
Case 4: She felt excruciating pain in the upper abdomen that lasted several minutes to hours and the pain was not related to eating or defecation. Extreme pain even woke her up at night. It occurred once or twice a year, and PPI and prokinetics administration had no effect. The pain intensity decreased when leaning forward or breathing in.
The patients had a free previous medical history.
The patients’ abdomen was soft and had no tenderness.
Blood analyses were normal.
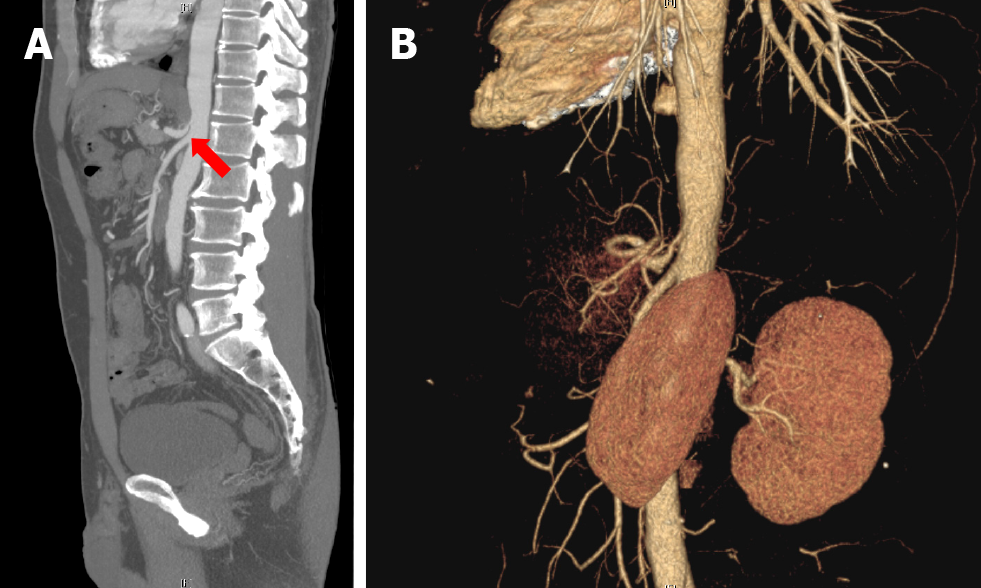
Case 1: We reviewed the medical history based on the characteristics of pain and the CT again, and a focal point of CT stenosis in the celiac axis was suspected (Figure 1A). Therefore, CT angiography (CTA) was performed. On the CTA, it was observed that the celiac trunk originating from the upper abdominal aorta was compressed by the diaphragmatic crus (Figure 1B). As a result, the origin of the celiac trunk showed focal tight narrowing, and along with clinical symptoms, the diagnosis could be made.
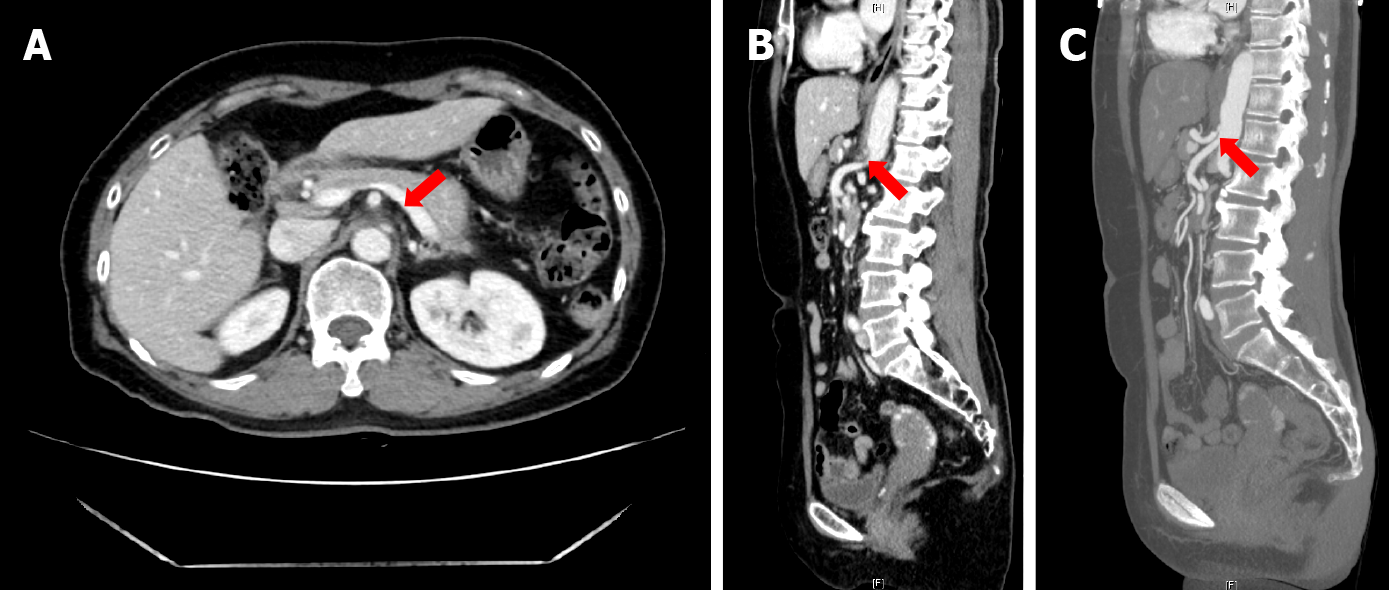
Case 2: Considering the patient's clinical features, we thought of diseases that could be missed by imaging techniques. Celiac artery compression was confirmed by reviewing the imaging studies (Figure 2A-C). This time, the collateral vessels around the pancreas were reviewed for narrowing of the celiac artery.
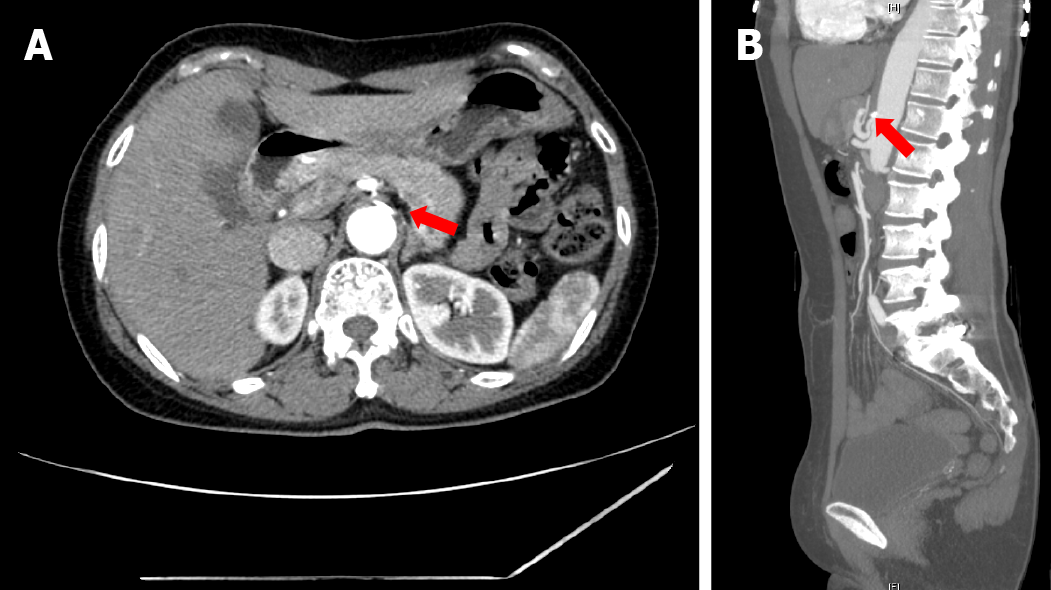
Case 3: CTA was performed based on clinical suspicion and celiac luminal narrowing was found due to focal calcification in the imaging tests (Figure 3A and B).
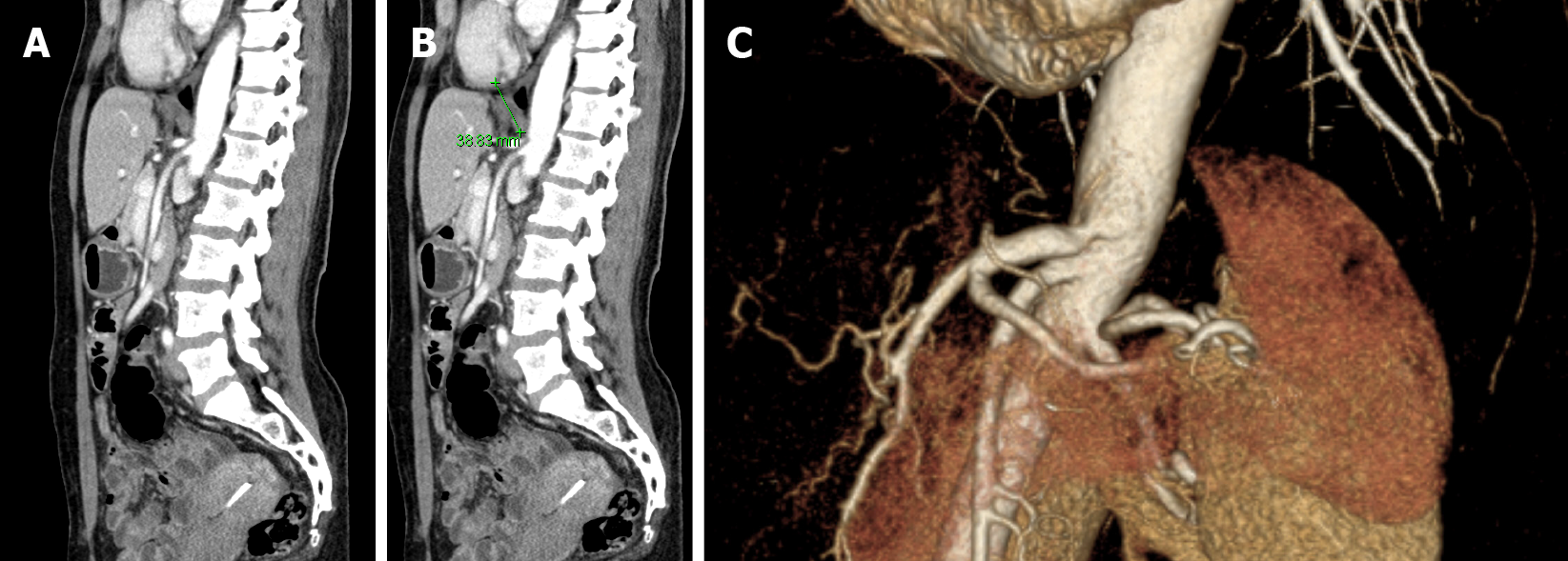
Case 4: There were no specific findings on endoscopy and abdominal ultrasonography, so based on clinical symptoms, an abdominal CT was performed, and MALS was diagnosed (Figure 4A-C).
The final diagnosis of the presented four cases is median arcuate ligamentum syndrome.
The patient’s condition improved after the administration of amitriptyline 10 mg to treat visceral neurologic symptoms and Tegoprazan 50 mg. The patient showed an immediate symptom improvement response to amitriptyline before active analgesic administration. Thus, even before active treatment, through diagnosis alone, improvement was already demonstrated. During follow-up, if any pain remains after observation for more than 3 mo, a pain relief agent and an active agent for reducing neurotransmitters will be used.
Neuropathic pain was relieved after the administration of gabapentin 100 mg, meloxicam 20 mg, and famotidine 20 mg b.i.d.
Gabapentin 100 mg, meloxicam 7.5 mg b.i.d, and esomeprazole were prescribed. She was due for an outpatient visit in 3 mo. The patient was asked to visit our hospital again if the symptoms worsened. She has been living without recurrence for a month after being prescribed medications.
She was prescribed gabapentin 100 mg, meloxicam 7.5 mg, and famotidine 20 mg b.i.d, and her symptoms improved significantly.
The symptoms of all 4 patients were much relieved with medical treatment, and they are being followed up on an outpatient clinics.
In all four cases, the patients experienced abdominal pain. In three cases, the diagnosis was possible by the judgment of the clinician shortly after the onset of symptoms. However, in one case that lasted over 20 years, a clear diagnosis was not possible. Even after complaining of colicky pain and performing a cholecystectomy, the diagnosis was made only after symptoms persisted. In all four cases, the symptoms were relieved by neuromodulators.
There are two current common hypotheses of MALS, which have been defined through several studies. The first one is neurologic pain caused by the compression of the celiac plexus and the other one is defined by compression of the celiac artery[2,10]. However, most hypotheses are based on images that were retrospectively analyzed and a defined protocol for making a diagnosis has not been developed. If this is due to ischemic arteriality, collateral vessels may develop, but the pain caused regardless of the produced collateral vessels. Importantly, ischemia cannot be reversible when the pain is maintained for a long time.
Therefore, the imaging diagnosis is only an auxiliary diagnosis. If the clinician does not suspect this diagnosis, the latter will happen very late. Most of the patients who came to the outpatient clinic of the department of gastroenterology at the tertiary hospital for indigestion and abdominal pain underwent an endoscopy and CT. However, it is not easy to identify rare diseases without providing clinical information from tens of thousands of still images. In addition, since the focus is on the exclusion of malignant tumors related to mortality pain is often considered a psychological disease despite its chronic nature, and is ignored.
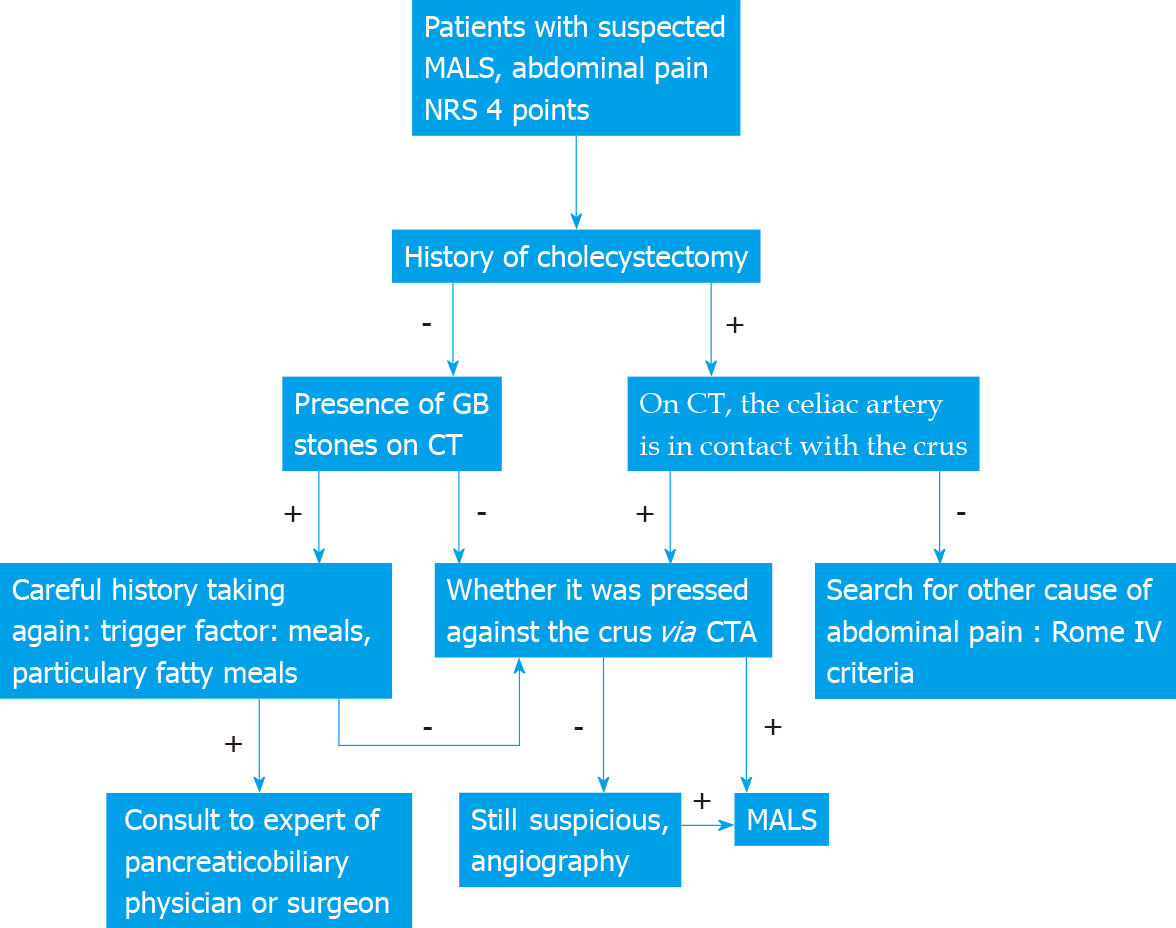
A report in 2017 reported only one case[13]. Other case reports that dealt with diagnosed cases relied on images and explained the pathological mechanisms for bowel ischemia, but they could not explain the absence of symptoms of intestinal damage due to ischemia[14]. Surgical treatments, such as ganglionectomy along with arterial reconstruction, have been proven to be effective[11], but considering that there are no symptoms even when pressed, physical removal may not be the only solution. This case is very novel because no cases have reported the outcomes of medical treatment and it raises awareness about a diagnosis that should not be missed. This case was written to suggest that a gastroenterologist must make a differential diagnosis. And since the gastroenterologist judges all the clinical results together, the evaluation is performed after confirming these. The following algorithm illustrates this process (Figure 5).
A limitation of this study was that the number of cases studied was too small. However, given that numerous MALS diagnoses have been missed, it is necessary to review many patients in the future and establish the diagnostic flow, considering the possibility that the etiology itself may be wrong. Since considering only four cases is insignificant, it will be necessary to review patients experiencing abdominal pain who have numerous missed diagnoses in the future. A common diagnostic flow is also required.
MALS is a rare disease and it is easy to miss because it is not malignant, but patients experience pain over a long period. For the accurate diagnosis of a patient complaining of abdominal pain, the diagnosis must be differentiated. In addition, as there are asymptomatic patients, patients who need treatment should be carefully selected, and improvement with medical treatment can be expected. Large-scale studies are also needed.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Baryshnikova NV, Ghannam WM, Martínez-Pérez A S-Editor: Zhang H L-Editor: A P-Editor: Zhang H
| 1. | Goodall R, Langridge B, Onida S, Ellis M, Lane T, Davies AH. Median arcuate ligament syndrome. J Vasc Surg. 2020;71:2170-2176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 90] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 2. | Kim EN, Lamb K, Relles D, Moudgill N, DiMuzio PJ, Eisenberg JA. Median Arcuate Ligament Syndrome-Review of This Rare Disease. JAMA Surg. 2016;151:471-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 175] [Article Influence: 21.9] [Reference Citation Analysis (1)] |
| 3. | Ghulam QM, Bredahl KK, Axelsen T, Hvolris LE, Kristiansen VB, Schulze S, Jørgensen LG, Schroeder TV, Eiberg JP. [Median arcuate ligament syndrome]. Ugeskr Laeger. 2015;177:V03150284. [PubMed] |
| 4. | Camacho N, Alves G, Bastos Gonçalves F, Abreu R, Ferreira R, Catarino J, Correia R, Ferreira ME. Median Arcuate Ligament Syndrome of Diaphragm - Literature Review and Case Report. Rev Port Cir Cardiotorac Vasc. 2017;24:57-61. [PubMed] |
| 5. | Fernstrum C, Pryor M, Wright GP, Wolf AM. Robotic Surgery for Median Arcuate Ligament Syndrome. JSLS. 2020;24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 6. | Santos Seoane SM, Izquierdo Romero M, Fernández Pantiga A, García Antuña E. Median arcuate ligament syndrome as a cause of intestinal angina. Rev Esp Enferm Dig. 2019;111:397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Cernigliaro J, Chen F, Bhatt S. The "Hook" sign of median arcuate ligament syndrome on ultrasound. Abdom Radiol (NY). 2021;46:2251-2252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Xiang H, Han J, Ridley WE, Ridley LJ. Fish hook coeliac: Median arcuate ligament syndrome. J Med Imaging Radiat Oncol. 2018;62 Suppl 1:74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Horton KM, Talamini MA, Fishman EK. Median arcuate ligament syndrome: evaluation with CT angiography. Radiographics. 2005;25:1177-1182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 264] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 10. | Heo S, Kim HJ, Kim B, Lee JH, Kim J, Kim JK. Clinical impact of collateral circulation in patients with median arcuate ligament syndrome. Diagn Interv Radiol. 2018;24:181-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 11. | San Norberto EM, Romero A, Fidalgo-Domingos LA, García-Saiz I, Taylor J, Vaquero C. Laparoscopic treatment of median arcuate ligament syndrome: a systematic review. Int Angiol. 2019;38:474-483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Usta S, Karabulut K, Artaş H. Median arcuate ligament syndrome during pancreaticoduodenectomy. Turk J Surg. 2018;1-2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Kuruvilla A, Murtaza G, Cheema A, Arshad HMS. Median Arcuate Ligament Syndrome: It Is Not Always Gastritis. J Investig Med High Impact Case Rep. 2017;5:2324709617728750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Bagley J, Stamile E, Berry JL, DiGiacinto D. Case report: median arcuate ligament syndrome diagnosed with computed tomography and Doppler ultrasonography. Radiol Technol. 2015;86:238-245. [PubMed] |