Published online Feb 26, 2022. doi: 10.12998/wjcc.v10.i6.1961
Peer-review started: August 15, 2021
First decision: November 6, 2021
Revised: November 16, 2021
Accepted: January 13, 2022
Article in press: January 13, 2022
Published online: February 26, 2022
Processing time: 192 Days and 7.8 Hours
Esophageal foreign body (FB) is a common clinical emergency. Clinically, computed tomography (CT) scans are important in the diagnosis of FBs in the esophagus. Here, we report a case of esophageal perforation and cervical hematoma, caused by a FB, whose uniqueness made rapid diagnosis difficult.
A 42-year-old man was transferred to our hospital with esophageal perforation, which was accompanied by cervical and mediastinal hematoma. CT scans only revealed a black shadow, approximately 2.5 cm in diameter, in the upper esophagus. After multidisciplinary discussion, he was quickly subjected to mediastinal hematoma resection, peripheral nerve compression release, esophageal FB removal and esophagectomy. Eventually, we removed a small crab with a pointed tip from his esophagus.
This was an unusual case of occurrence of sharp polygonal esophageal FBs caused by a small crab. Rapid diagnosis of this FB was difficult, mainly due to its translucent nature. Occurrence of sharp FBs, with cavities that sometimes only appear as black shadows on CT scans, can easily be mistaken for esophageal lumens. More attention should be paid to such sharp polygonal FBs.
Core Tip: Esophageal foreign body (FB) is a common clinical emergency, a man suffered a sharp polygonal FB caused by the small crab. The FB in this patient was more difficult to detect on computed tomography because of its translucent nature, which increased the difficulty of rapid diagnosis. This case is rare and We should pay more attention at the sharp polygonal foreign body.
- Citation: Wang LP, Zhou ZY, Huang XP, Bai YJ, Shi HX, Sheng D. Neck and mediastinal hematoma caused by a foreign body in the esophagus with diagnostic difficulties: A case report. World J Clin Cases 2022; 10(6): 1961-1965
- URL: https://www.wjgnet.com/2307-8960/full/v10/i6/1961.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i6.1961
Esophageal foreign body (FB), which typically presents with dysphagia, is a common clinical emergency. Patients with FBs sometimes attempt inappropriate clearance approaches, such as vigorous swallowing, which may lead to over-tightening or esophageal perforation, accompanied by life-threatening complications such as mediastinal abscess and esophago-aortic fistula bleeding[1]. Here, we report a case of esophageal perforation and cervical hematoma due to a FB in the esophagus. The uniqueness of this FB made rapid diagnosis difficult.
The main complaints were a sudden shortness of breath, neck swelling and dyspnea.
A 42-year-old man, suddenly felt a FB stuck in his throat while eating breakfast (steamed stuffed bun, fried dough stick and seafood soup). Although he tried to clear the obstruction by swallowing steamed stuffed bun and drinking soup, the pharyngeal obstruction was not relieved. Consequently, he developed shortness of breath, neck swelling and dyspnea.
His past medical history was hypertension.
Home medications included hydrochlorothiazide. He denied any family history of lung diseases and esophageal diseases.
Physical examinations revealed presence of neck hematoma and low oxygen saturation.
Laboratory results showed increased white blood cell counts 18.30 × 109/L and elevated levels of C-reactive protein 21.20 mg/L. Nucleic acid-based analysis of the novel coronavirus at the local hospital revealed negative results.
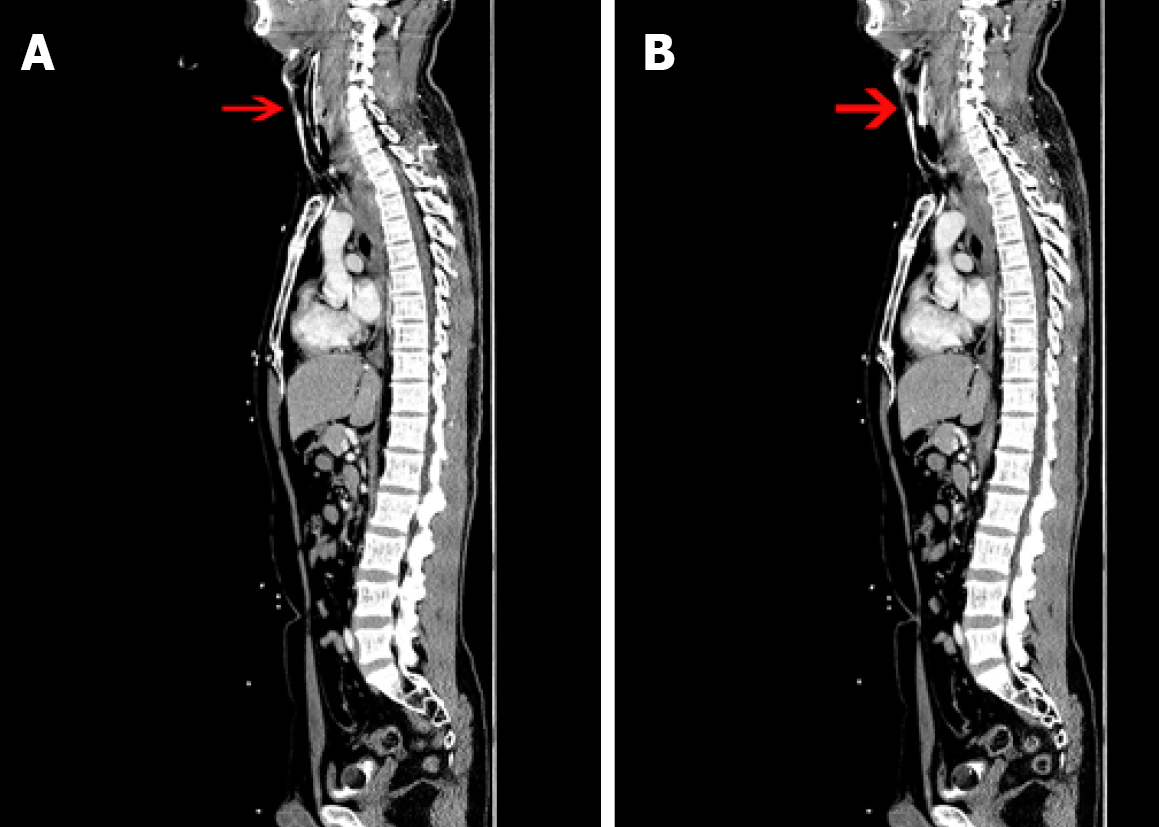
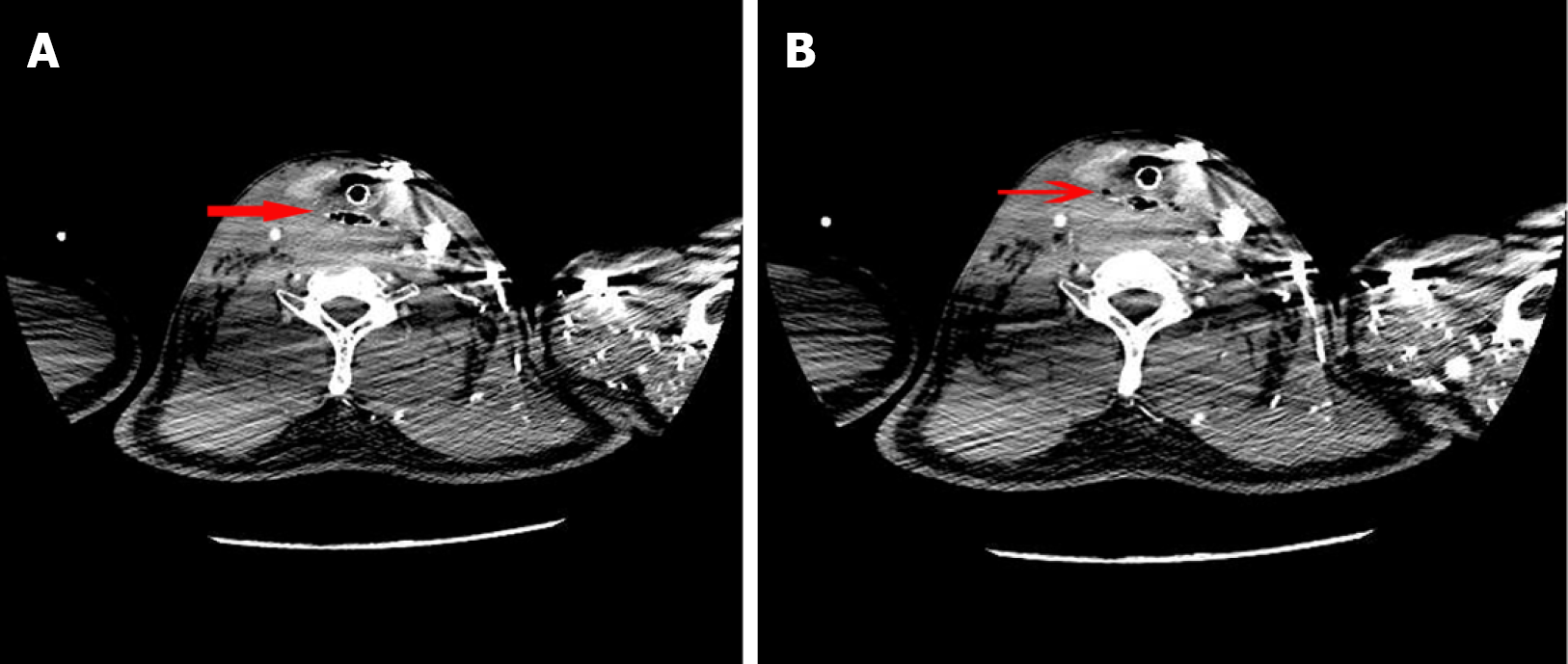
He was immediately taken to the local hospital and subjected to computed tomography (CT) scan, 30 min after onset of his illness. Results revealed presence of a large hematoma in his mediastinum and right neck (Figure 1). Due to the complexity of the problem, he was transferred from the local hospital to our hospital, where he was immediately treated with emergency tracheal intubation and respiratory support (3.5 h after onset of the condition). Results from CT angiography, performed on his thoracic aorta approximately 4 h after onset of the condition, revealed a black shadow of approximately 2.5 cm in diameter in the upper esophagus. The object was surrounded by a sharp end and a faint needle-like high-density shadow around it (Figure 2).
Through a multidisciplinary discussion, we considered that the patient had a cavernous esophageal FB.
He was immediately subjected to mediastinal hematoma removal, peripheral nerve decompression, maxillofacial FB removal and esophageal reconstruction. This was approximately 10 h after onset of the condition. During surgery, an L-shaped incision was made along the sternocleidomastoid muscle of the right neck, followed by release and protection of the right recurrent laryngeal nerve. The posterior pharyngeal space was accessed through the right tracheoesophageal groove to reveal a large hematoma. The hematoma was aspirated, revealing a small arterial injury. Next, the vessel was closed using a surgical suture (ETHICON, polyglactin 910 suture). The wall of the right esophagus was then incised, and the FB at its entrance removed. This FB turned out to be a small crab, 2 cm × 3 cm (Figure 3) with sharp ends that pierced the esophagus and measured 0.5 cm × 0.3 cm. The patient’s esophagus was repeatedly flushed with dilute iodine, then repaired with surgical sutures (ETHICON, polyglactin 910 suture). Next, two drains were placed in the mediastinum, one in the retropharyngeal space, and a vacuum device was placed to drain the nasogastric tube. After successful surgery, the patient was transferred to the intensive care unit. He regained respiratory and circulatory stability, 1 d after surgery, after which the tracheal tube was removed. He was then transferred to the general ward and maintained on antibiotics. Mediastinal and retropharyngeal space catheters were removed on the fifth day, while the nasogastric tube was postoperatively removed after 11 d.
The patient was discharged when he was free of severe symptoms and is being followed up in the outpatient clinic.
Although approximately 20% of all adult patients with esophageal FBs require clinical interventions, most of these FBs will spontaneously pass[2,3]. Esophageal perforation caused by FBs is a relatively rare occurrence, accounting for only 1%-4% of all reported cases. Sharp polygonal or pin-like pointed FBs have been strongly linked with esophageal perforation or rupture, with a risk of up to 35%[4]. Results from a prospective single-center study found that CT was 90%-100% sensitive and 93.7%-100% specific, indicating that it is highly effective in diagnosing accidental ingestions or suspected bone fragments in patients that return negative X-ray results[5-7].
The FB lodged in the esophagus of the patient in the present study was a small crab, a sharp polygonal FB with only a thin shell and a small amount of crab meat inside. Notably, it looked like an air bubble, based on the CT image, which contrasts with solid FBs such as fish and poultry bones that appear as opaque objects on the CT image. This delayed rapid diagnosis of this patient. CT scans revealed the presence of a black shadow, about 2-3 cm in diameter, in the upper esophagus. In general, the gas-bearing shadow is for esophageal lacuna, but the gas shadow was bigger than normal and clear and sharp on both ends; the surrounding was a dimly visible linear high-density shadow, suggesting that it may not be the lacuna esophagus but a sharp FB. Although it was clinically confusing, a closer look at the shaded border revealed a sharp polygonal FB.
Chung et al[8] reported the first case of a crab-induced esophageal FB, albeit with less damage to the esophagus. Here, we report the second case of crab-associated FB lodged in the esophagus, and the first case of crab-associated esophageal perforation. Upon being stuck in the patient’s esophagus, he tried to push it into the stomach by eating steamed bread. However, this improper approach caused the FB to stick deeper in the esophagus. The FB pierced the esophageal wall and damaged blood vessels, thereby causing a huge hematoma and compressing the airway. Consequently, these phenomena resulted in life-threatening dyspnea and respiratory failure. Improper methods for clearance of esophageal FBs, especially sharp ones, are discouraged. Instead, patients are advised to seek timely treatment to reduce the risk of complications. Delayed treatment leads to esophageal necrosis and predisposes patients to general infection, a situation that has been linked to high mortality rates, ranging from 10%-20%[9,10].
Sharp FBs with cavities, which sometimes only appear as black shadows on CT scans, can easily be mistaken for esophageal lumens, thereby making clinical diagnosis difficult. This report elucidates on clinical diagnosis of cavernous FBs. Delayed treatment increases the risk of complications, thus timely performance of clinical management options, such as surgery, are encouraged. We recommend that patients with respiratory distress, caused by lodged FBs, first be subjected to airway stabilization prior to attempting removal or definitive management.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Emergency medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Choe JY, Govindarajan KK S-Editor: Wu YXJ L-Editor: Filipodia P-Editor: Wu YXJ
| 1. | Cobanoglu U, Mergan D, Kemik O, Sayir F. Oesophageal foreign bodies caused by meat consumed during the Sacrifice Feast: Our single-centre experience. J Pak Med Assoc. 2018;68:1193-1198. [PubMed] |
| 2. | Ambe P, Weber SA, Schauer M, Knoefel WT. Swallowed foreign bodies in adults. Dtsch Arztebl Int. 2012;109:869-875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 129] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 3. | Erbil B, Karaca MA, Aslaner MA, Ibrahimov Z, Kunt MM, Akpinar E, Özmen MM. Emergency admissions due to swallowed foreign bodies in adults. World J Gastroenterol. 2013;19:6447-6452. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 40] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | Chirica M, Kelly MD, Siboni S, Aiolfi A, Riva CG, Asti E, Ferrari D, Leppäniemi A, Ten Broek RPG, Brichon PY, Kluger Y, Fraga GP, Frey G, Andreollo NA, Coccolini F, Frattini C, Moore EE, Chiara O, Di Saverio S, Sartelli M, Weber D, Ansaloni L, Biffl W, Corte H, Wani I, Baiocchi G, Cattan P, Catena F, Bonavina L. Esophageal emergencies: WSES guidelines. World J Emerg Surg. 2019;14:26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 187] [Cited by in RCA: 139] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 5. | Ngan JH, Fok PJ, Lai EC, Branicki FJ, Wong J. A prospective study on fish bone ingestion. Experience of 358 patients. Ann Surg. 1990;211:459-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 167] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 6. | Goh BK, Tan YM, Lin SE, Chow PK, Cheah FK, Ooi LL, Wong WK. CT in the preoperative diagnosis of fish bone perforation of the gastrointestinal tract. AJR Am J Roentgenol. 2006;187:710-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 137] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 7. | Brinster CJ, Singhal S, Lee L, Marshall MB, Kaiser LR, Kucharczuk JC. Evolving options in the management of esophageal perforation. Ann Thorac Surg. 2004;77:1475-1483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 520] [Cited by in RCA: 486] [Article Influence: 23.1] [Reference Citation Analysis (0)] |
| 8. | Chung CH. Corrosive oesophageal injury following vinegar ingestion. Hong Kong Med J. 2002;8:365-366. [PubMed] |
| 9. | Young CA, Menias CO, Bhalla S, Prasad SR. CT features of esophageal emergencies. Radiographics. 2008;28:1541-1553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 89] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 10. | Biancari F, D'Andrea V, Paone R, Di Marco C, Savino G, Koivukangas V, Saarnio J, Lucenteforte E. Current treatment and outcome of esophageal perforations in adults: systematic review and meta-analysis of 75 studies. World J Surg. 2013;37:1051-1059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 172] [Article Influence: 14.3] [Reference Citation Analysis (0)] |