Published online Feb 26, 2022. doi: 10.12998/wjcc.v10.i6.1843
Peer-review started: August 18, 2021
First decision: September 29, 2021
Revised: October 4, 2021
Accepted: January 19, 2022
Article in press: January 19, 2022
Published online: February 26, 2022
Processing time: 189 Days and 4.2 Hours
Scientific and effective nursing methods can effectively mitigate negative emotions in patients. Related studies have shown that systematic nursing interventions are beneficial in enhancing the self-efficacy and self-care abilities of patients and improving their physical and mental state, thereby alleviating their fatigue and improving their quality of life.
To explore the effects of systematic nursing intervention on cancer-related fatigue, self-efficacy, self-nursing ability, and quality of life in gastric cancer (GC) patients during the perioperative period.
In this study, sample size was based on the multivariable scale. The sample size was 10 times the acceptable variable, with an additional 20% added to account for an expected loss of patients in follow-up for a final sample size of 168 patients. Conventional nursing measures were used in the control group, while the systematic nursing intervention Adopted Cancer Fatigue Scale (CFS), General Self-Efficacy Scale-Schwarzer (GSES), Self-Care Agency Scale (ESCA), and simple health scale (SF-36) were used in the observation group. The questionnaires were administered on admission and discharge.
At admission, there was no statistically significant difference in the scores on each scale between the groups. At discharge, the CFS and GSES scores in the observation group were 21.56 ± 2.24 and 51.16 ± 11.71, while those in the control group were 29.61 ± 3.48 and 41.58 ± 8.54, respectively, with statistically significant differences. The ESCA score in the observation and control groups was 112.09 ± 11.72 and 97.87 ± 9.26, respectively. Moreover, the scores in all dimensions (self-concept, self-responsibility, health knowledge level, and self-care skills) in the observation group were higher than those in the control group, with statistically significant differences. The SF-36 score in the observation and control groups was 75.51 ± 3.63 and 63.24 ± 3.41, respectively, with statistically significant differences. The scores in all dimensions (mental health, vitality, physical function, physical pain, social function, emotional function, and overall health level) in the observation group were higher than those in the control group, with statistically significant differences.
Systemic nursing intervention for GC patients during the perioperative period could alleviate cancer-related fatigue, improve self-efficacy and self-nursing ability, and improve quality of life, which all have clinical value.
Core Tip: The scores in all dimensions (mental health, vitality, physical function, physical pain, social function, emotional function, and overall health level) in the observation group were higher than those in the control group, with statistically significant differences. Systemic nursing intervention for gastric cancer patients during the perioperative period could alleviate cancer-related fatigue, improve self-efficacy and self-nursing ability, and improve quality of life, which all have clinical value.
- Citation: He F, He RX. Systematic nursing interventions in gastric cancer: A randomized controlled study. World J Clin Cases 2022; 10(6): 1843-1851
- URL: https://www.wjgnet.com/2307-8960/full/v10/i6/1843.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i6.1843
Gastric cancer (GC) ranks fifth for incidence and fourth for mortality globally. There are approximately one million new cases in 2020 and an estimated 769000 deaths[1]. Radical resection is the main treatment for GC, while subtotal gastrectomy with standard D2 lymph node dissection is the main surgical treatment, which is characterized by extensive surgical trauma and slow postoperative recovery[2]. Feeding difficulties are commonly seen in patients with GC, combined with physiological function changes after surgery, which seriously affects the patient’s quality of cancer-related fatigue (CRF). CRF is a persistent and subjective sense of fatigue and activity intolerance caused by cancer itself and surgery, which cannot be alleviated by sleep and rest, and is the most intolerable adverse reaction in patients with cancer[3]. The National Comprehensive Cancer Network believes that anemia, depression, pain, sleep disorders, and nutrition may all be related to CRF based on research on CRF symptoms[4]. Thus, CRF has a significantly negative impact on patients’ quality of life, and comprehensive research has found that the influencing factors of CRF mainly include the following aspects: cancer type and treatment pathways, psychological factors, socioeconomic factors, and cancer complications[4]. CRF is an ever-changing subjective feeling. The recognition and cognition of fatigue during the nursing process will also affect the patients’ expression of CRF. Most patients believe that fatigue is something that must be endured during treatment, and most of them will not actively complain about this symptom. However, fatigue can also be used to predict the occurrence of cancer[5].
GC surgery causes significant surgical trauma and slow postoperative healing. Therefore, effective implementation of nursing interventions is also a key issue in clinical research. Clinically, it is necessary to adopt an active nursing method for patients with GC to eliminate CRF, which will improve the self-efficacy of the patients, which in turn will improve patient prognosis. Scientific and effective nursing methods can effectively mitigate negative emotions in patients. Related studies[6] have shown that systematic nursing interventions are beneficial in enhancing the self-efficacy and self-care abilities of patients and improving their physical and mental state, thereby alleviating their fatigue and improving their quality of life. In this study, systematic nursing interventions were administered to patients with GC during the perioperative period, and their effects on CRF, self-efficacy, self-nursing ability, and quality of life were analyzed. This study also explored the application value of nursing interventions in patients with GC during the perioperative period.
In this study, sample size was based on the multivariable scale. Expecting approximately 20% loss of patients to follow-up, and with 10 times the acceptable variable (which had an expected 140 patients), the final sample size was 168 people. The inclusion criteria were as follows: (1) Clinical or pathological diagnosis of GC; (2) Age ≥ 18 and initial hospitalization; (3) Tumor–node–metastasis (TNM) stages Ⅰ, Ⅱ, IIIa, and IIIb without complications; (4) Patients were aware of their condition and were willing to participate in the study; (5) Patients who could communicate normally; and (6) Patients with no history of mental illness or emotional instability. The exclusion criteria were as follows: (1) Patients who withdrew and transferred for treatment due to personal reasons; (2) Patients who underwent palliative surgery in stage IV; (3) Patients with mental disorders or cognitive impairment; (4) Patients who could not communicate properly; and (5) Patients whose condition was critical and life-threatening. The research subjects were randomly divided into the observation and control groups according to a generated random number table, with 84 cases in each group. This study was approved by the hospital’s medical ethics committee, and the patients and their families understood the content and methods of the study before providing informed consent.
The control group received conventional nursing interventions, were provided guidance on hospital admission, cooperated with the corresponding nursing measures during the perioperative period, and were actively provided life nursing and psychological nursing.
The observation group was treated according to NCCN guidelines for cancer-related fatigue. Based on the patients’ characteristics, systematic nursing interventions were performed. The main contents are as follows: First, on admission, nurses explained the ward environment and system to the patients to eliminate anxiety caused by the unfamiliar environment; second, for establishing a good relationship of trust with the patient, nurses needed to understand the patients’ experience of cancer-related fatigue and related symptoms, including the timing, frequency, severity of fatigue, and distress brought to the patient by fatigue symptoms; third, nurses assisted patients to assess their own available resources and developed personalized, targeted management plans for them, and on the day before the operation, nurses provided the patient with a brochure which included the key points of postoperative care, changes in the patients’ habits, and common complications. At the same time, nurses combined with the form of powerpoint to teach the patients how to correctly use the Fatigue Digital Rating Scale to express their degree of fatigue. Targeted health education was conducted according to the patients’ individual situations to correctly understand the dialectical relationship between their disease, treatment, and psychological conditions. The period after surgery was when nurses had the most contact with patients. Effective nurse–patient communication helped nurses identify patients’ nursing problems and emotional changes over time. When nurses found that the fatigue-related symptoms of the patient worsened, they made the patients listen to music, chatted with family members, and looked for ways to distract the patients’ attention from the fatigue. Nurses urged the patients to move on the bed for early venting. Moderate activities during the day can help ensure that patients sleep better at night. After the patients’ gastric tubes were removed and their diets gradually resumed, nurses used the food model to guide the family members on the issues that need attention while purchasing and cooking food materials. The patients were also encouraged to express their feelings to enhance communication with their families. Nurses listened to the patients’ chief complaints and intervene in the bedside setting. On the third postoperative day, nurses issued a “self-management manual,” and instructed the patients to fill in a daily fatigue diary. Nurses adjusted the nursing measures based on the patients’ fatigue assessment on the previous day and provided patients with a manual on the causes of fatigue and home care tips.
CRF, self-efficacy, self-care ability, and quality of life of the patients were assessed on the day of admission and discharge. Questionnaires were issued by trained nurses, and on-site guidance was provided. The Cancer Fatigue Scale (CFS) evaluated the symptoms related to CRF from three aspects—physical, emotional, and cognitive. The Likert 5 (0–4 points) scoring method was used, with a total score of 0–60 points. The higher the score, the more serious the CRF[7]. The General Self-Efficacy Scale-Schwarzer was used to evaluate the self-efficacy changes of patients in the two groups after nursing using a 4-level scoring method, with each item scoring from 1 to 4[8]. The higher the score was, the better the self-efficacy of patients. Self-care ability was evaluated using the Self-Care Agency Scale, which included 4 dimensions and 43 items, including self-care skills, self-care responsibility, self-concept, and health knowledge level[9]. High scores in all dimensions indicated high self-care ability, and quality of life was evaluated using a simple health scale. The scale comprehensively assessed patients’ quality of life in terms of physiological function, physical pain, general health, physiological ability, social function, emotional function, and mental health, among others, with a total score of 100 points[10]. A higher score indicates a better quality of life.
The data were processed using SPSS 19.0 version, and the measurement data are expressed as mean ± SD, while the count data are expressed as percentage (%). Pairwise comparisons adopted an analysis of variance. The threshold for significance was set at P < 0.05.
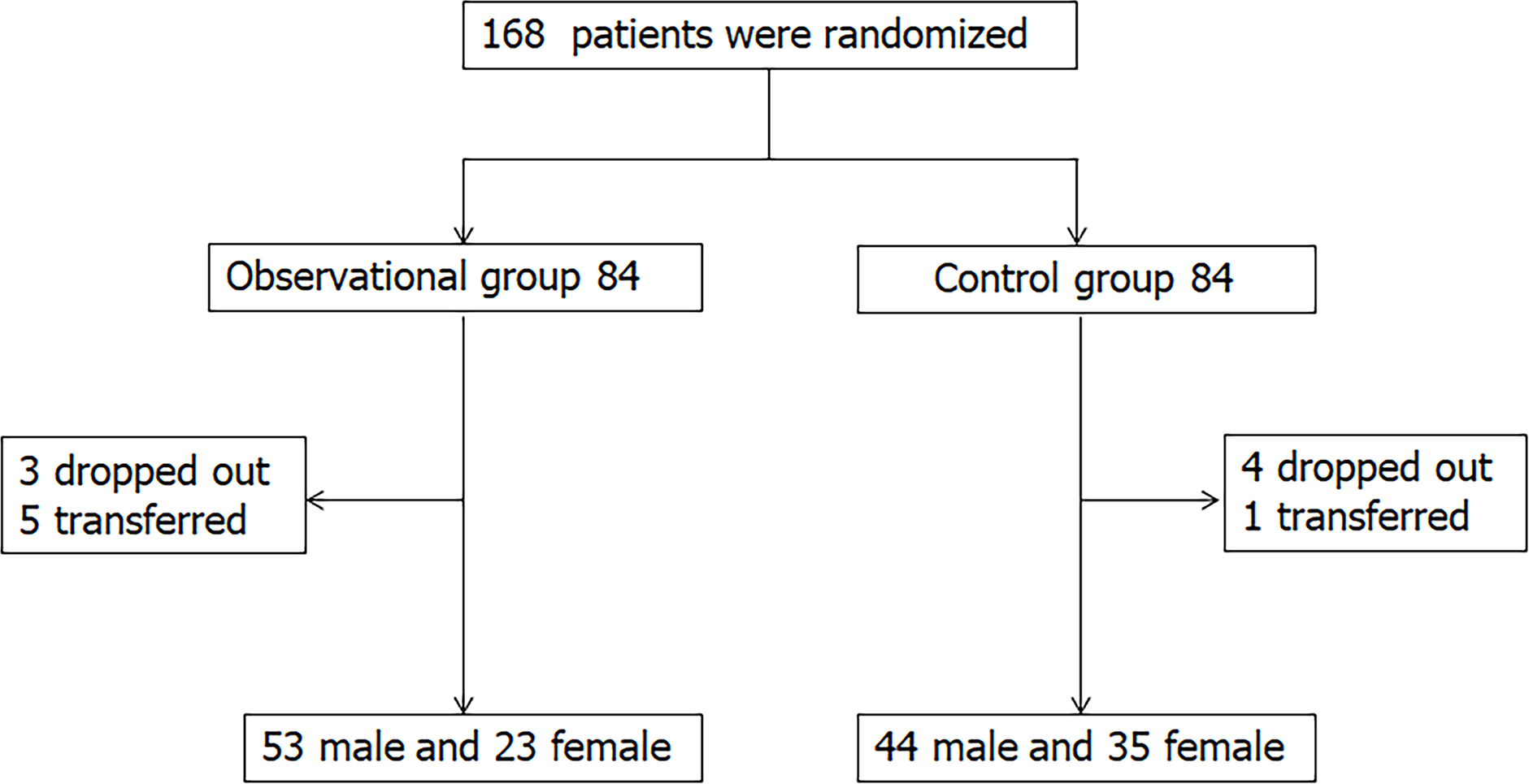
In the observation group, 3 patients dropped out and 5 were transferred. Fifty-three cases were male and 23 cases were female. The average age was (55.14 ± 4.67) years. The TNM stages in 28, 33, and 15 cases were Ⅰ, Ⅱ, and Ⅲ, respectively. The highest educational levels for 1343, 8, and 12 patients were primary school, junior high school, senior high school, and university, respectively. In the control group, 4 patients dropped out and 1 was transferred. Forty-four patients were male and 35 patients were female (Figure 1). The average age was 56.09 ± 4.19 years. The TNM stages in 25, 40, and 14 cases were Ⅰ, Ⅱ, and Ⅲ, respectively. The highest educational levels of 12, 39, 15, and 13 patients were primary school, junior high school, senior high school, and university, respectively. There were no significant differences in age, sex, TNM stage, and educational level between the groups; both groups were comparable (P > 0.05).
Table 1 shows that there was no significant difference in CFS scores between the groups before the intervention (P > 0.05). However, after the nursing intervention, the CFS scores in the two groups were reduced, indicating that the nursing intervention effects were relatively good, but the effects of systematic nursing intervention in the observation group were more obvious than those of conventional intervention in the control group, with a significant difference (P < 0.05).
| Group | Before intervention | After intervention | ||||||
| Observation group | Control group | t value | P value | Observation group | Control group | t value | P value | |
| Body fatigue | 19.02 ± 1.51 | 19.23 ± 1.63 | 0.242 | 0.835 | 10.85 ± 1.22 | 14.63 ± 1.34 | 5.499 | < 0.001 |
| Cognitive fatigue | 9.63 ± 0.85 | 9.71 ± 0.80 | 0.429 | 0.684 | 5.16 ± 0.50 | 7.38 ± 0.57 | 7.181 | < 0.001 |
| Emotional fatigue | 10.70 ± 0.90 | 10.64 ± 0.9 | 0.237 | 0.814 | 6.42 ± 0.43 | 7.92 ± 0.51 | 8.927 | < 0.001 |
| Total score | 40.24 ± 6.47 | 41.47 ± 6.59 | 0.896 | 0.794 | 21.56 ± 2.24 | 29.61 ± 3.48 | 9.983 | < 0.001 |
Table 2 shows that there was no significant difference in self-care ability scores between the two groups before the intervention (P > 0.05). After receiving the nursing interventions, the self-care ability scores of the two groups were increased, indicating that the effects of nursing intervention were relatively good. However, the effects of systemic nursing interventions in the observation group were more obvious than those in the control group, with a significant difference (P < 0.05).
| Group | Before intervention | After intervention | ||||||
| Observation group | Control group | t value | P value | Observation group | Control group | t value | P value | |
| Self-concept | 22.17 ± 4.10 | 21.83 ± 3.41 | 1.897 | 0.825 | 27.91 ± 3.77 | 21.15 ± 3.31 | 9.875 | < 0.001 |
| Self-responsibility | 18.75 ± 7.07 | 18.91 ± 7.38 | 1.612 | 0.795 | 30.22 ± 5.84 | 19.61 ± 6.69 | 10.851 | < 0.001 |
| Health knowledge level | 32.92 ± 5.08 | 33.74 ± 4.64 | 1.472 | 0.814 | 37.08 ± 3.88 | 18.69 ± 2.54 | 9.411 | < 0.001 |
| Self-care skills | 26.56 ± 4.20 | 27.73 ± 3.76 | 1.392 | 0.763 | 40.47 ± 4.14 | 29.50 ± 4.27 | 11.245 | < 0.001 |
| Total score | 87.00 ± 12.52 | 85.83 ± 13.06 | 1.412 | 0.821 | 112.09 ± 11.72 | 97.87 ± 9.26 | 13.417 | < 0.001 |
Table 3 shows that there was no significant difference in self-efficacy scores between the two groups before the intervention (P > 0.05). After nursing interventions, the self-efficacy scores of the two groups were increased, indicating that the nursing intervention effects were relatively good. However, the effects of systemic nursing interventions in the observation group were more obvious than those in the control group, with a significant difference (P < 0.05).
| Group | Observation group | Control group | t value | P value |
| Before intervention | 34.39 ± 10.45 | 35.11 ± 9.60 | 1.335 | 0.813 |
| After intervention | 51.16 ± 11.71 | 41.58 ± 8.54 | 5.53 | < 0.001 |
Table 4 shows the comparison results of the quality of life of the two groups before and after the intervention. The specific indices set were mental health, vitality, physical function, physical pain, social function, health status, and overall health level. After nursing interventions, the scores of all dimensions of quality of life in the observation group were significantly higher than those in the control group, and the difference was significant (P < 0.05).
| Group | Before intervention | After intervention | ||||||
| Observation group | Control group | t value | P value | Observation group | Control group | t value | P value | |
| Mental health | 56.57 ± 6.80 | 56.95 ± 6.86 | 0.349 | 0.728 | 84.61 ± 5.56 | 77.30 ± 4.66 | 7.416 | < 0.001 |
| Vitality | 58.28 ± 9.64 | 58.69 ± 9.43 | 0.412 | 0.734 | 81.68 ± 8.60 | 71.80 ± 8.25 | 11.295 | < 0.001 |
| Physical function | 60.39 ± 7.12 | 60.95 ± 7.25 | 0.499 | 0.692 | 82.71 ± 6.07 | 74.92 ± 5.04 | 9.421 | < 0.001 |
| Physical pain | 55.70 ± 5.05 | 56.14 ± 4.92 | 1.649 | 0.792 | 79.85 ± 6.76 | 67.16 ± 4.44 | 11.292 | < 0.001 |
| Social function | 51.13 ± 3.07 | 51.39 ± 3.13 | 0.301 | 0.702 | 77.92 ± 2.36 | 65.57 ± 2.65 | 12.226 | < 0.001 |
| Emotional function | 42.30 ± 2.66 | 42.59 ± 2.86 | 0.351 | 0.649 | 66.47 ± 2.45 | 51.68 ± 2.51 | 14.261 | < 0.001 |
| Overall health level | 50.38 ± 2.33 | 50.48 ± 2.19 | 0.287 | 0.839 | 75.51 ± 3.63 | 63.24 ± 3.41 | 13.214 | < 0.001 |
Systematic nursing intervention could alleviate symptoms related to CRF in patients with GC during the perioperative period
Systemic nursing intervention was centered on patients based on their negative emotions, wherein nurses implemented multiple interventions, such as knowledge education, psychological and social support, and CRF nursing, and constantly adjusted the care they gave to patients according to their individual situations. The results of this study showed that after intervention, the degree of CRF in the observation group was lower than that in the control group. This was consistent with the results of a previous study[11], which reported that systematic nursing intervention could improve the fatigue state and quality of life of patients with cancer. In this study, nurses and patients established a good relationship of trust. Nurses actively guided patients to correctly face the symptoms and treatment of the disease and improved patients’ cognition of the disease. Patients better followed the nursing measures that could relieve bodily fatigue. In the face of fatigue-related symptoms, nurses guided patients to seek help from family members and friends and, thus, helped the patients get more social support. These measures alleviated patients’ anxiety and depression and relieved patients’ emotional fatigue. From the second day after surgery, nurses instructed patients to move while on the bed to promote venous circulation in the lower extremities. According to the NCCN guidelines, exercise is an effective intervention for CRF[12]. Patients recorded their daily activity levels in a “self-management manual” to encourage them to continue exercising and performed individual movement appropriately to increase muscle strength and stimulate airframe lively sex, which would reduce the feeling of fatigue.
CRF is a series of subjective feelings resulting from patients’ long-term tension and pain caused by GC, such as weakness, activity intolerance, inattention, and reduced motivation or interest, with fatigue being the most distressing of all the related symptoms[13]. Some studies have shown that self-efficacy is negatively correlated with the total score for cancer-related fatigue[14]. The self-efficacy of patients can be improved by alleviating symptoms of cancer-related fatigue. In this study, after instituting the nursing interventions, the self-care ability and self-efficacy scores of the two groups improved, and the systemic nursing intervention in the observation group demonstrated more obvious effects than the conventional nursing intervention in the control group, with the difference being significant (P < 0.05). The reasons are as follows: the researchers used the NCCN guidelines for the management of symptoms of cancer-related fatigue and developed a “self-management manual” for nursing measures for patients, which included general management of fatigue and non-pharmacological measures. Common management practices included monitoring of fatigue levels and the use of diverting attention, including increased exercise, psychological regulation, regulation of sleep disorders, pain self-management, and relaxation therapy. Patients used the nursing measures in the manual for self-regulation, and their self-care ability continued to improve. Self-efficacy refers to a person’s subjective judgment of whether he can successfully conduct a certain achievement behavior[15] and is a degree of confidence that can be gradually developed through learning and cultivation. Positive psychological regulation can improve patients’ cognition of the disease and allow them to calmly face difficulties and adopt positive self-management methods[16]. This increased patients’ confidence in beating cancer and increased their sense of self-efficacy. This was in line with the results reported by Krok et al[17], who reported that the use of a systematic nursing method can greatly alleviate the psychological discomfort of patients with GC and found that after such intervention, the psychological status of the patients improved.
As a major negative life event, cancer causes a significant emotional toll on the family. Sandler et al[18] improved the quality of life of patients with cancer through a combination of cognitive behavioral intervention and physical exercise. The day before the operation, nurses explained patients the function of the stomach and the matters needing attention during the operation to eliminate any unknown facts regarding the disease and the fear of the operation. Before discharge, nurses taught patients how to adapt to changes in diet after gastrectomy. With the advancement of treatment, the patients’ concern gradually shifted to concerns related to radiotherapy and chemotherapy. Nurses dynamically adjusted nursing measures based on the recorded daily in the patients’ “self-management manual.” Nurses fully considered the needs of patients and helped them achieve their subjective initiative. Targeted nursing measures improved patients’ treatment compliance and effectively reduced their symptoms of dysphagia, stomach pain, hiccup, restricted diet, and so on. Therefore, the physical and psychological functions of patients were improved, and the quality of life of patients thereafter also improved. Table 4 shows that the comparison of quality of life between the two groups before and after treatment was statistically significant (P < 0.05).
This study showed that the implementation of systematic nursing interventions in patients with GC during the perioperative period could significantly improve their fatigue state, mental health status, self-nursing ability, self-efficacy, and quality of life, all of which have a positive clinical value. However, the patients included in this study were all from the same specialized oncology hospital, and patients in stage IV who underwent palliative surgery and those with more serious disease were not included. Further studies are needed to clarify whether systematic nursing intervention can be used to improve the CRF and quality of life of patients to elucidate the etiology and pathogenesis of CRF. This would involve other disciplines, such as pharmacy, psychology, and nursing. The creation of a multidisciplinary team, including clinicians, nurses, psychotherapists, and dietitians to comprehensively fulfill organizational and coordinating roles will be optimal in clinical practice.
Systemic nursing intervention for GC patients during the perioperative period could alleviate cancer-related fatigue, improve self-efficacy and self-nursing ability, and improve quality of life, which all have clinical value.
Systematic nursing interventions are beneficial in enhancing the self-efficacy and self-care abilities of patients and improving their physical and mental state, thereby alleviating their fatigue and improving their quality of life.
To explore the effects of systematic nursing intervention.
Gastric cancer (GC) surgery causes significant surgical trauma and slow postoperative healing. Systematic nursing interventions were administered to patients with GC during the perioperative period.
This is a randomized controlled study, sample size was based on the multivariable scale. Ten times of the acceptable variable was determined to be 140 patients, and accounting for 20% loss of patients due to follow-up, the sample size was 168 people. Conventional nursing measures were used in the control group, while the systematic nursing intervention Adopted Cancer Fatigue Scale (CFS), General Self-Efficacy Scale-Schwarzer (GSES), Self-Care Agency Scale (ESCA), and simple health scale (SF-36) were used in the observation group. The questionnaires were administered on admission and discharge.
The scores in all dimensions (mental health, vitality, physical function, physical pain, social function, emotional function, and overall health level) in the observation group were higher than those in the control group, with statistically significant differences.
Systemic nursing intervention for GC patients during the perioperative period could alleviate cancer-related fatigue, improve self-efficacy and self-nursing ability, and improve quality of life, which all have clinical value.
Systemic nursing intervention for GC patients during the perioperative period are beneficial. More large scale randomized controlled studies are needed.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Nursing
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lidoriki I, Yashiro M S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Ma YJ
| 1. | Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75126] [Cited by in RCA: 64636] [Article Influence: 16159.0] [Reference Citation Analysis (176)] |
| 2. | Fugazzola P, Ansaloni L, Sartelli M, Catena F, Cicuttin E, Leandro G, De' Angelis GL, Gaiani F, Di Mario F, Tomasoni M, Coccolini F. Advanced gastric cancer: the value of surgery. Acta Biomed. 2018;89:110-116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 3. | Zou G, Li Y, Xu R, Li P. Resilience and positive affect contribute to lower cancer-related fatigue among Chinese patients with gastric cancer. J Clin Nurs. 2018;27:e1412-e1418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 4. | Berger AM, Mooney K, Alvarez-Perez A, Breitbart WS, Carpenter KM, Cella D, Cleeland C, Dotan E, Eisenberger MA, Escalante CP, Jacobsen PB, Jankowski C, LeBlanc T, Ligibel JA, Loggers ET, Mandrell B, Murphy BA, Palesh O, Pirl WF, Plaxe SC, Riba MB, Rugo HS, Salvador C, Wagner LI, Wagner-Johnston ND, Zachariah FJ, Bergman MA, Smith C; National comprehensive cancer network. Cancer-Related Fatigue, Version 2.2015. J Natl Compr Canc Netw. 2015;13:1012-1039. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 412] [Cited by in RCA: 599] [Article Influence: 66.6] [Reference Citation Analysis (0)] |
| 5. | Pyszora A, Budzyński J, Wójcik A, Prokop A, Krajnik M. Physiotherapy programme reduces fatigue in patients with advanced cancer receiving palliative care: randomized controlled trial. Support Care Cancer. 2017;25:2899-2908. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 77] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 6. | He XL, Cao ZM. Effect of high-quality nursing intervention on the psychological disorder in patients with gastric cancer during perioperative period: A protocol of systematic review and meta-analysis. Medicine (Baltimore). 2020;99:e20381. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Lim EJ, Son CG. Review of case definitions for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). J Transl Med. 2020;18:289. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 109] [Cited by in RCA: 97] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 8. | Selzler AM, Habash R, Robson L, Lenton E, Goldstein R, Brooks D. Self-efficacy and health-related quality of life in chronic obstructive pulmonary disease: A meta-analysis. Patient Educ Couns. 2020;103:682-692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 61] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 9. | Morishita M, Hattori S, Miyai N. Ability for Self-Care among Elderly Patients with Diabetes Mellitus and Its Association with Health Locus of Control and Social Support. Nihon Eiseigaku Zasshi. 2017;72:77-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Doosti-Irani A, Nedjat S, Cheraghi P, Cheraghi Z. Quality of life in Iranian elderly population using the SF-36 questionnaire: systematic review and meta-analysis. East Mediterr Health J. 2019;24:1088-1097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Zhang Q, Li F, Zhang H, Yu X, Cong Y. Effects of nurse-led home-based exercise & cognitive behavioral therapy on reducing cancer-related fatigue in patients with ovarian cancer during and after chemotherapy: A randomized controlled trial. Int J Nurs Stud. 2018;78:52-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 86] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 12. | Berntsen S, Aaronson NK, Buffart L, Börjeson S, Demmelmaier I, Hellbom M, Hojman P, Igelström H, Johansson B, Pingel R, Raastad T, Velikova G, Åsenlöf P, Nordin K. Design of a randomized controlled trial of physical training and cancer (Phys-Can) - the impact of exercise intensity on cancer related fatigue, quality of life and disease outcome. BMC Cancer. 2017;17:218. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 13. | Arring NM, Barton DL, Brooks T, Zick SM. Integrative Therapies for Cancer-Related Fatigue. Cancer J. 2019;25:349-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 14. | Chen HL, Liu K, You QS. Self-efficacy, cancer-related fatigue, and quality of life in patients with resected lung cancer. Eur J Cancer Care (Engl). 2018;27:e12934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 15. | Hamilton CB, Li LC. Measures of Patient Activation and Self-Efficacy. Arthritis Care Res (Hoboken). 2020;72 Suppl 10:645-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Iani L, Quinto RM, Porcelli P, Angeramo AR, Schiralli A, Abeni D. Positive Psychological Factors Are Associated With Better Spiritual Well-Being and Lower Distress in Individuals With Skin Diseases. Front Psychol. 2020;11:552764. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Krok D, Telka E. The role of meaning in gastric cancer patients: relationships among meaning structures, coping, and psychological well-being. Anxiety Stress Coping. 2019;32:522-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Sandler CX, Goldstein D, Horsfield S, Bennett BK, Friedlander M, Bastick PA, Lewis CR, Segelov E, Boyle FM, Chin MTM, Webber K, Barry BK, Lloyd AR. Randomized Evaluation of Cognitive-Behavioral Therapy and Graded Exercise Therapy for Post-Cancer Fatigue. J Pain Symptom Manage. 2017;54:74-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |