Published online Feb 6, 2022. doi: 10.12998/wjcc.v10.i4.1441
Peer-review started: September 7, 2021
First decision: November 19, 2021
Revised: November 28, 2021
Accepted: December 23, 2021
Article in press: December 23, 2021
Published online: February 6, 2022
Processing time: 139 Days and 2.2 Hours
Relapsing polychondritis (RP) is a rare inflammatory disease involving the systemic cartilage, such as the auricle, trachea, and bronchiole, among others. A patient with RP shows variable symptoms based on the involved cartilage.
A 72-year-old Japanese woman with a history of redness of the bilateral auricles for 3 d was referred to a clinician. The clinician prescribed antibiotics to the patient; however, the symptoms worsened; thus, she was referred to our hospital. Head and neck magnetic resonance imaging (MRI) showed edematous auricle with remarkable contrast, fluid collection in the bilateral mastoid cells, suggesting otitis media. The eustachian tube (ET) on the right side was also edematous with contrast enhancement. The patient was suspected of RP according to the diagnostic criteria. A biopsy of the auricular cartilage was performed by an otorhinolaryngologist, confirming pathological proof of RP. Treatments with steroids were immediately administered thereafter.
We highlight a rare case of RP with radiologically confirmed involvement of ET in the MRI.
Core Tip: Relapsing polychondritis (RP) is a rare inflammatory disease involving the systemic cartilage. Its diagnostic criteria and clinical manifestations are well established; however, no previous studies have reported the involvement of the eustachian tube (ET) in RP. A 72-year-old Japanese woman with a history of redness of the auricles for 3 d was diagnosed with RP with pathological evidence. The magnetic resonance imaging (MRI) showed edematous ETs with contrast enhan
- Citation: Yunaiyama D, Aoki A, Kobayashi H, Someya M, Okubo M, Saito K. Eustachian tube involvement in a patient with relapsing polychondritis detected by magnetic resonance imaging: A case report. World J Clin Cases 2022; 10(4): 1441-1446
- URL: https://www.wjgnet.com/2307-8960/full/v10/i4/1441.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i4.1441
Relapsing polychondritis (RP) is a rare autoimmune inflammatory disease of the systemic cartilages and proteoglycan-rich structures[1]. The real incidence and prevalence of RP are still unknown. The major inflammatory sites of this disease are the ears, nose, eyes, respiratory tract, and joints[2-5]. The clinical manifestations in the otological area are auricular chondritis, otitis externa, chronic myringitis, eustachian tube (ET) dysfunction, conductive or sensorineural hearing loss, dizziness, and tinnitus[6,7]. The cause of fluid collection in a middle ear of a patient with RP should be derived from ET dysfunction due to ET cartilage inflammation; however, no report has proven the inflammation of an ET itself radiographically. We hereby present a case of a patient with RP confirmed by biopsy of the auricular cartilage, manifesting the involvement of ET detected by magnetic resonance imaging (MRI).
A 72-year-old Japanese woman with a history of redness of the bilateral auricles for 3 d was referred to a clinician.
The clinician prescribed antibiotics to the patient (2 g in a day of cefminox sodium hydrate for 3 d); however, the symptoms worsened, and thus, the patient was referred to our hospital.
The patient’s medical history included hypertension, type 2 diabetes mellitus, lumbar disc hernia, postmenopausal osteoporosis, and reflux esophagitis.
The patient had no family history of similar illnesses.
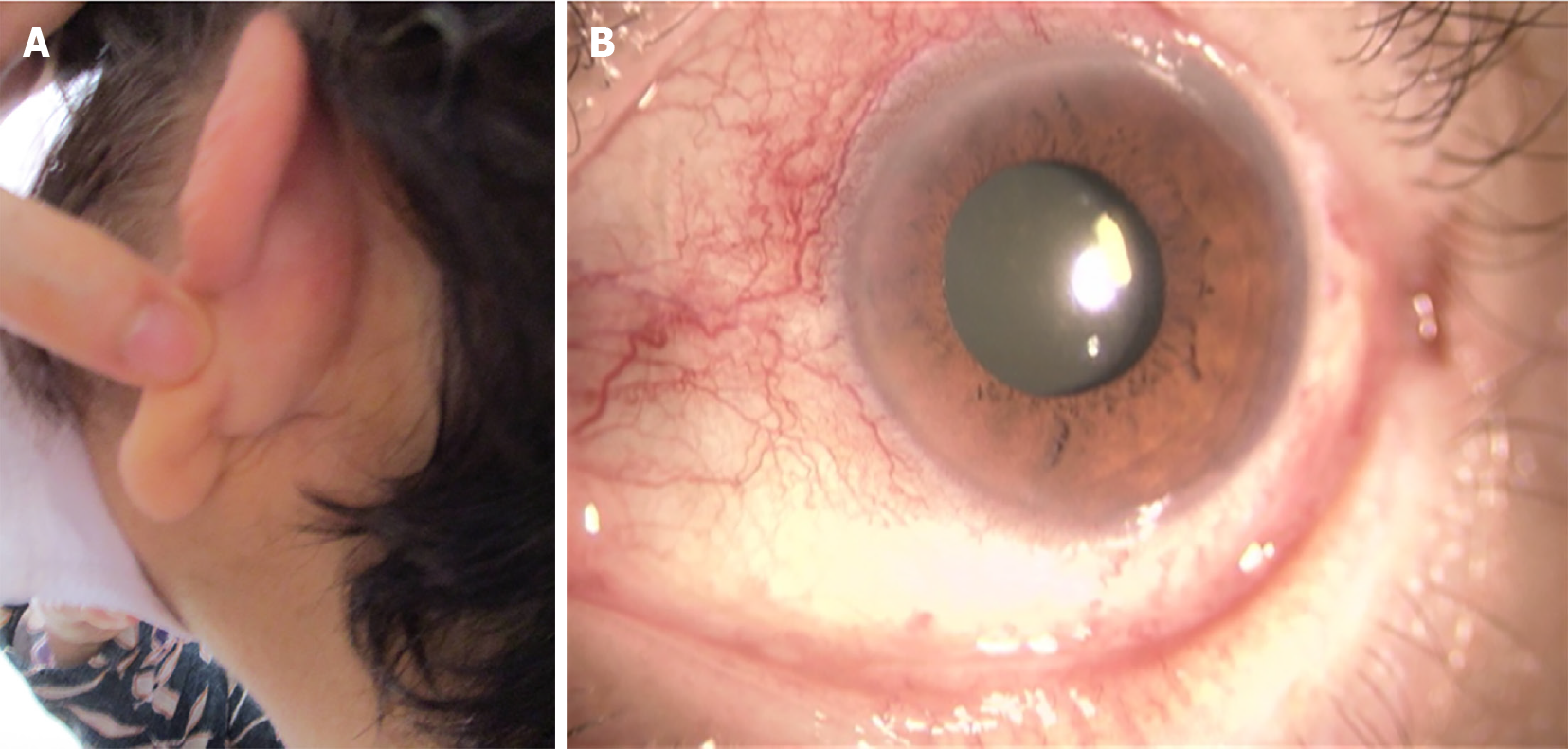
Her body temperature was 37℃. No abnormal chest sound was not heard; however, the patient was suffered from dry cough. Tender, erythematous and edematous bilateral auricles were observed (Figure 1A). Left conjunctival hyperemia was also observed (Figure 1B). Additionally, trismus was observed, which resulted in mastication difficulty. A pure tone audiogram showed sensorineural hearing loss at the high sound area, and the patient complained of tinnitus. Nasal cartilage inflammation or dyspnea was not observed. The patient met four indices of McAdam’s criteria[8]. A tympanic membrane proliferation was not observed.
White blood cell count of 14200/μL (segmented 77.8%), red blood cell count of 383 × 104 /μL, a hemoglobin level of 12.1 g/dL, platelet count of 29.8 × 104 /μL, the total protein level of 7.6 g/dL, albumin level of 3.6 g/dL, total bilirubin level of 0.7 mg/dL, creatinine level of 0.88 mg/dL, eGFR of 48.3 mL/min, C-reaction protein level of 11.03 mg/dL, hemoglobin A1c of 7.0%, and antinucleus antibody level of < 40 U were observed.
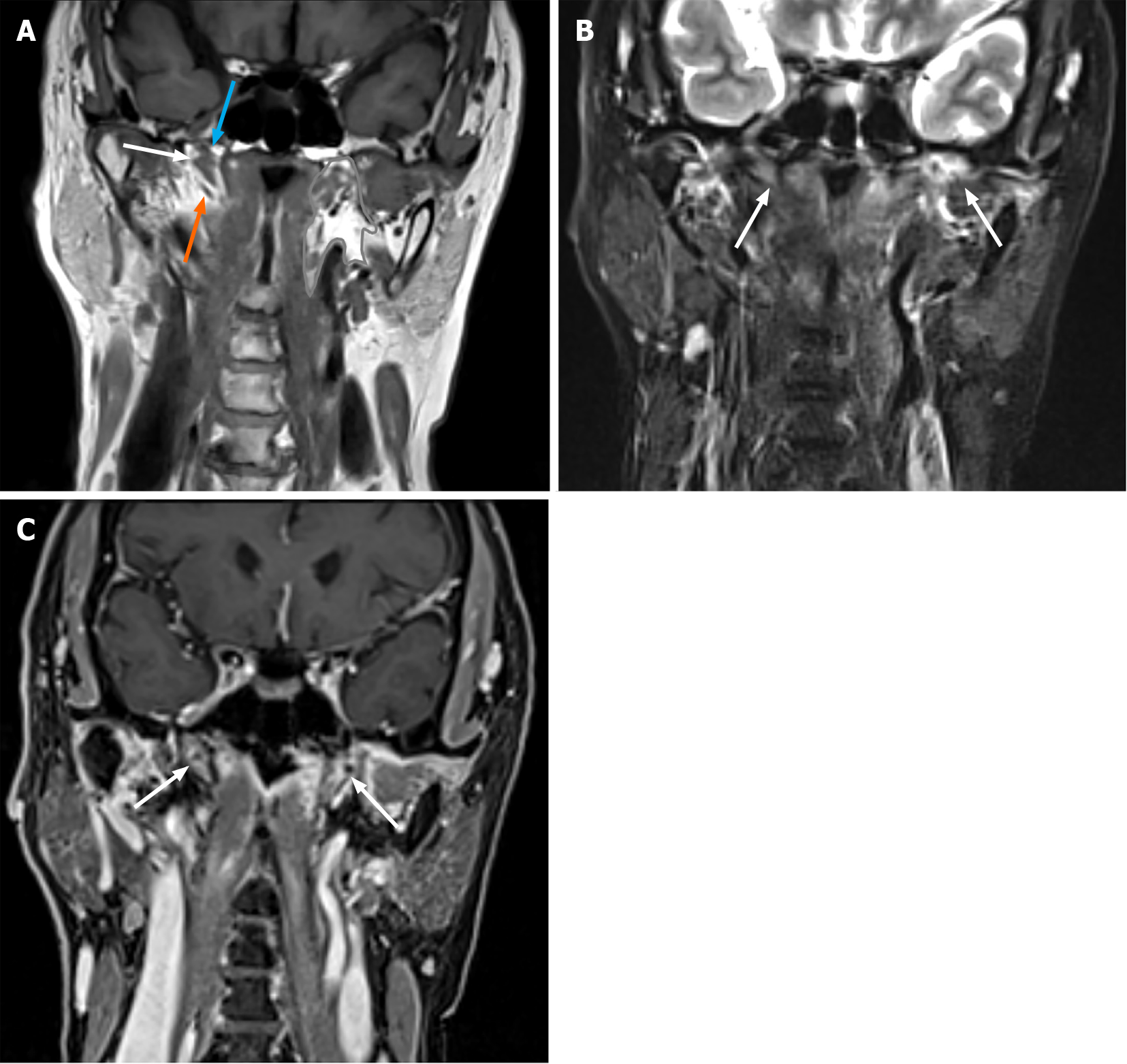
Chest computed tomography showed no subglottal, tracheal, or bronchial swelling. ETs are located in the parapharyngeal space on noncontrast-enhanced 3D T1-weighted image (flip angle, 120; repetition time, 600; echo time, 12; number of excitations, 1; slice thickness, 0.8 mm; and field of view, 25 cm × 28.4 cm). The Merkmal of the ET is the levator veli palatine muscle on the upper side and the tensor veli palatine muscle on the lower side (Figure 2A). Noncontrast-enhanced fat-saturated T2-weighted images (flip angle, 111; repetition time, 6060; echo time, 64; number of excitations, 1; slice thickness, 4 mm; slice space, 4.8 mm; and field of view, 25 cm × 28.4 cm) of the patient demonstrated edematous bilateral ETs (Figure 2B). The contrast-enhanced 3D-volumetric interpolated breath-hold examination T1-weighted image (flip angle, 11; repetition time, 5.5; echo time, 2.46; number of excitations, 2; slice thickness, 1 mm; and field of view, 30 cm × 34.1 cm) demonstrated enhanced bilateral ETs (Figure 2C).
A biopsy from the auricular cartilage, a tissue composed of hyaline cartilage and connective tissue, was performed by an otorhinolaryngologist, and moderate chronic inflammatory cell infiltration including the lymphocytes and plasma cells is observed in the fibrous connective tissue and is partially vitrified. Inflammatory cells have infiltrated part of the hyaline cartilage.
The final diagnosis was RP.
The patient started undergoing steroid therapy using 30 mg/d of prednisolone with preventive antifungal medications as there was no life-threatening symptom. The patient also started taking sulfamethoxazole trimethoprim to prevent Pneumocystis jirovecii pneumonia.
The clinical course of the patient was summarized in Table 1. The patient’s symptoms decreased after drug treatment within 2 wk. Laboratory inflammation markers also decreased. We are following up to see if there is any improvement in sensorineural hearing loss. The edema and contrast enhancement of ETs disappeared in the follow-up MRI at 8 wk.
| Time point | Remarks |
| July 24, 2021 | Redness of the bilateral auricles |
| July 27, 2021 | Antibiotics administration at a clinician |
| August 10, 2021 | Referred to our hospital |
| August 18, 2021 | Non contrast enhanced chest to abdominal CT without significant findings |
| August 20, 2021 | Biopsy for auricular cartilage |
| August 21, 2021 | Contrast enhanced head and neck MRI with presenting figures |
| Prednisolone administration was started | |
| September 1, 2021 | Symptoms and laboratory abnormality improved remarkably |
| October 28, 2021 | Disappeared edema and contrast enhancement of eustachian tubes on MRI |
To the best of our knowledge, this is the first report of a patient with RP manifesting as enhanced and edematous ET on MRI by reviewing previous mass reports and imaging review[3-5,9,10]. The only head and neck lesion other than auricles and nasal cartilage was orbital involvement reported by Moore et al[11]. Otitis media has been known as a common manifestation of a patient with RP; however, the reason behind its occurrence has not been discussed to date. Theoretically, an ET might be involved in a patient with RP as it comprises cartilages, the inflammatory target of RP. Otitis media in adults can be divided into four types of manifestations: microorganism infections in the ET from the nasopharynx to middle ear that manifesting acute otitis media; obstruction of the ET orifice to the nasopharynx due to nasopharyngeal carcinoma, nasopharyngeal inflammation, or ET dysfunction, resulting in a fluid collection in the middle ear manifesting otitis media with effusion (OME); a proliferation of tympanic membrane results in chronic inflammation of the middle ear manifesting chronic otitis media; and cholesteatoma, a keratinized, desquamated epithelial collection in the middle ear. In this patient, infectious symptoms, tympanic membrane proliferation, or cholesteatoma was not observed so that OME was suspected. Fluid collection in the middle ear of patients with RP could be due to ET dysfunction caused by inflammation of the involved cartilages as in this case; however, this has not been proven as a pathological examination at this site.
We experienced a case of patients with RP representing edematous and enhancing ET on MRI accompanying otitis media. Otitis media in patients with RP was suggested to be caused by ET dysfunction through inflammatory changes.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: The Japanese Society of Radiology; The Japanese Society of Interventional Radiology; and The Japanese Society of Nuclear Medicine.
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cao X, He YQ, Xu Y S-Editor: Li X L-Editor: A P-Editor: Li X
| 1. | Lekpa FK, Chevalier X. Refractory relapsing polychondritis: challenges and solutions. Open Access Rheumatol. 2018;10:1-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (1)] |
| 2. | Kent PD, Michet CJ Jr, Luthra HS. Relapsing polychondritis. Curr Opin Rheumatol. 2004;16:56-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 173] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 3. | Chen N, Zheng Y. Characteristics and Clinical Outcomes of 295 Patients With Relapsing Polychondritis. J Rheumatol. 2021;48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Dion J, Costedoat-Chalumeau N, Sène D, Cohen-Bittan J, Leroux G, Dion C, Francès C, Piette JC. Relapsing Polychondritis Can Be Characterized by Three Different Clinical Phenotypes: Analysis of a Recent Series of 142 Patients. Arthritis Rheumatol. 2016;68:2992-3001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 112] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 5. | Shimizu J, Yamano Y, Kawahata K, Suzuki N. Relapsing polychondritis patients were divided into three subgroups: patients with respiratory involvement (R subgroup), patients with auricular involvement (A subgroup), and overlapping patients with both involvements (O subgroup), and each group had distinctive clinical characteristics. Medicine (Baltimore). 2018;97:e12837. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Rampelberg O, Gerard JM, Namias B, Gerard M. ENT manifestations of relapsing polychondritis. Acta Otorhinolaryngol Belg. 1997;51:73-77. [PubMed] |
| 7. | Bachor E, Blevins NH, Karmody C, Kühnel T. Otologic manifestations of relapsing polychondritis. Review of literature and report of nine cases. Auris Nasus Larynx. 2006;33:135-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 41] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | McAdam LP, O'Hanlan MA, Bluestone R, Pearson CM. Relapsing polychondritis: prospective study of 23 patients and a review of the literature. Medicine (Baltimore). 1976;55:193-215. [PubMed] |
| 9. | Lin DF, Yang WQ, Zhang PP, Lv Q, Jin O, Gu JR. Clinical and prognostic characteristics of 158 cases of relapsing polychondritis in China and review of the literature. Rheumatol Int. 2016;36:1003-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 10. | Thaiss WM, Nikolaou K, Spengler W, Spira D, Xenitidis T, Henes J, Horger M. Imaging diagnosis in relapsing polychondritis and correlation with clinical and serological data. Skeletal Radiol. 2016;45:339-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 11. | Moore GH, Rootman DB, Roybal CN, Goldberg RA. Orbital Relapsing Polychondritis: A Unique Presentation, Complication, and Treatment. Ophthalmic Plast Reconstr Surg. 2016;32:e34-e36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |