Published online Feb 6, 2022. doi: 10.12998/wjcc.v10.i4.1373
Peer-review started: August 23, 2021
First decision: October 22, 2021
Revised: October 30, 2021
Accepted: December 25, 2021
Article in press: December 25, 2021
Published online: February 6, 2022
Processing time: 153 Days and 18.7 Hours
Gouty tophus is rarely reported in the head and neck areas. To the best of our knowledge, this is the first report on multiple gouty tophi in the head and neck with normal serum uric acid (SUA) levels.
We report a case of multiple gouty tophi in the nasal dorsal and auricle regions with normal SUA levels. The patient was admitted to the hospital with a chief complaint of recurrent nasal swelling and pain for 3 years, which was aggravated for 3 d. The patient’s SUA level had been regularly reviewed in the outpatient department and had been successfully controlled for several years. Resection of the nasal masses was performed. Cartilage from the right ear cavity was used to repair the nasal defects. The pathological report confirmed a nasal gouty tophus. No recurrence or deformity was found after a 1 year follow-up.
Normal SUA cannot completely negate the diagnosis of gouty tophus, especially in some rare regions.
Core Tip: Hyperuricemia is a key factor in the formation of gouty tophus, and it is often detected on the first metatarsophalangeal or first metacarpophalangeal joints of both hands. It is rarely reported in the head and neck areas, such as the throat and auricle. We believe that clinicians should be aware of the possibility of gouty tophus in patients with a history of gout, especially in some rare regions. For surgeons, an accurate preoperative diagnosis can help determine the appropriate operation mode and incision size.
- Citation: Song Y, Kang ZW, Liu Y. Multiple gouty tophi in the head and neck with normal serum uric acid: A case report and review of literatures. World J Clin Cases 2022; 10(4): 1373-1380
- URL: https://www.wjgnet.com/2307-8960/full/v10/i4/1373.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i4.1373
Gout is a clinical syndrome caused by an increase in uric acid production or a weakening of renal excretion function, resulting in a continuous increase in serum uric acid (SUA) level and the deposition of urate in joints, synovium, or other tissues and organs[1,2]. Consequently, complications including gouty arthritis, gouty tophus, uric acid renal stones, and gouty nephropathy may develop. Gouty tophus is a sign of chronic gout, and its formation can lead to bone destruction, joint deformity, joint dysfunction, and even fracture and infection of the tophus[3], which can seriously affect the quality of life of patients. The formation of gouty tophus is a complex process, and many factors can lead to and accelerate its formation. The gold standard for the diagnosis of gout is the detection of birefringent acicular urate crystals in joint fluid or gouty tophus under a polarised light microscope[4].
An increased SUA level is considered as the basis for gout. When a patient presents with an SUA level > 7 mg/dL[5,6], characteristic arthritis, urinary calculi, or renal colic, the clinical diagnosis of gout can be considered. However, most patients with hyperuricemia (HUA) do not develop gout[7]. Further, several patients have normal SUA levels at gout onset and some gout patients have gouty tophus with no acutegout attack or gouty tophus before the attack[7,8], potentially leading to clinical misdiagnosis and mistreatment. Herein, we report a case of multiple gouty tophi in the head and neck, specifically in the auricle and bridge of the nose, with normal SUA level.
A 48-year-old male patient was admitted to the hospital with a chief complaint of ‘recurrent nasal swelling and pain for 3 years’.
Since 2016, the nasal swelling and pain were mild, without nasal congestion, runny nose, epistaxis, fever, headache, trauma, or mosquito bites. In recent years, regular outpatient reviews of SUA had been normal. Drinking alcohol and high purine diet could occasionally aggravate nasal symptoms.
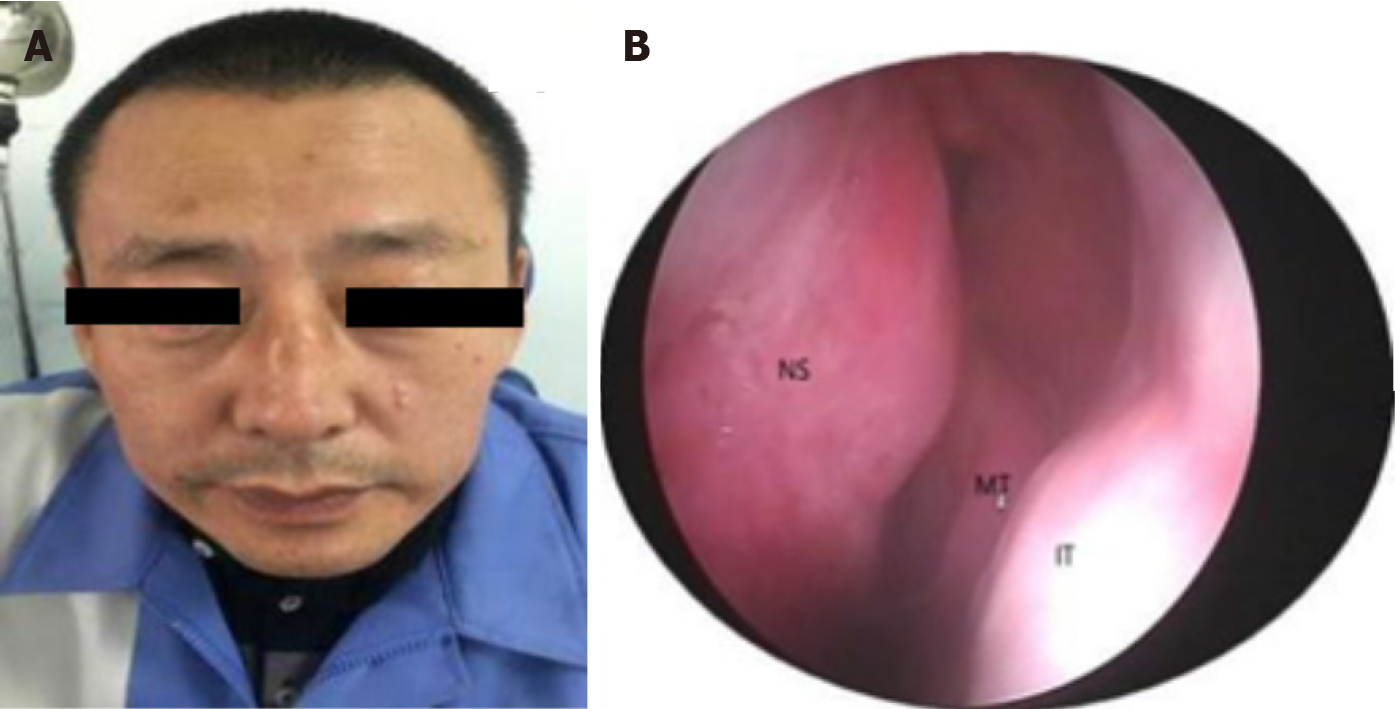
Thirteen years ago, the patient was admitted to another hospital due to swelling and tingling of ankle joints and was diagnosed with gout and hyperuricemia. He regularly received febuxostat. The patient’s SUA level had been regularly reviewed in the outpatient department, and was well controlled for several years (Figure 1). The patient had no history of diabetes mellitus, hypertension, cystic fibrosis and metabolic disorders.
The patient was a male, 48 years old, reported no history of dental surgery, facial trauma, or previous sinus surgery.
Skin swelling with a diameter of 2 cm on the bridge of the nose, obvious tenderness, and nasal deformity. Under the nasal endoscope, the nasal cavity was unobstructed, the nasal septum was in the centre, no obvious bulge or neoplasm was observed in the top wall of the nasal cavity (Figure 2). A new greyish-white creature with a diameter of 5 mm was observed on the outer upper edge of the right auricle.
Laboratory examination revealed a uric acid level of 384 μmol/L (reference value range 208-428 μmol/L). The water sample secretion of rice swill was punctured from the local uplift, and general bacterial and fungal cultures showed no abnormal flora. The patient declined invasive cytological examination.
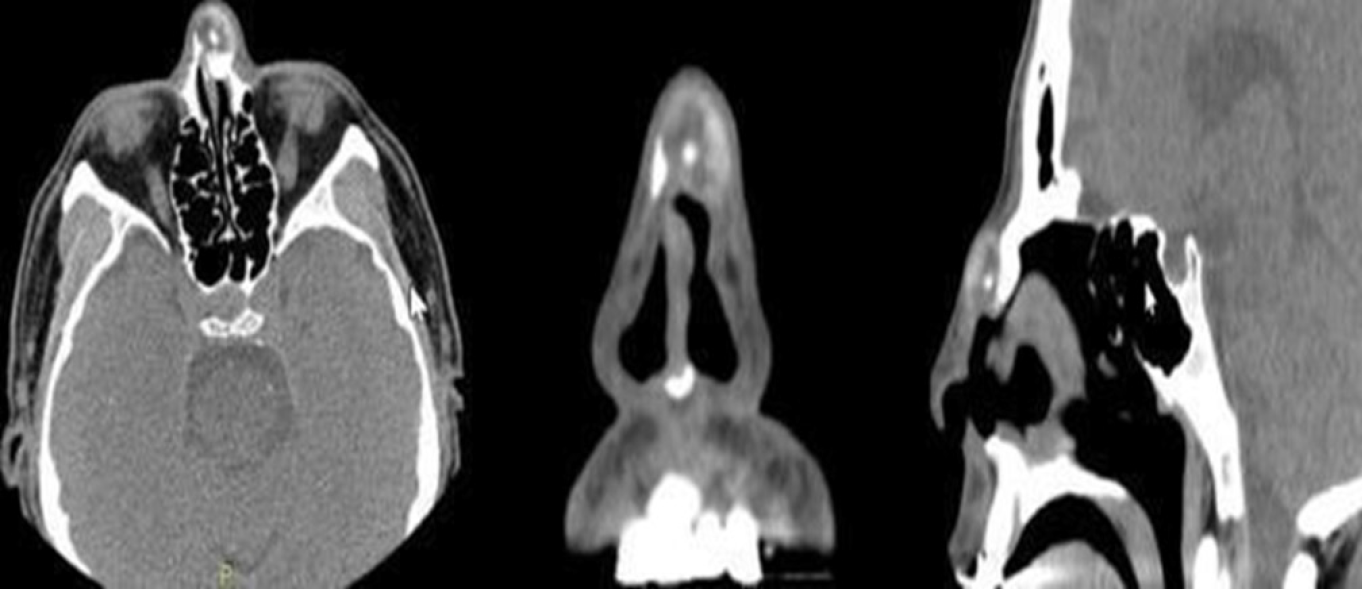
Enhanced computed tomography (CT) imaging revealed a mixed density mass shadow on the left side of the nose (Figure 3).
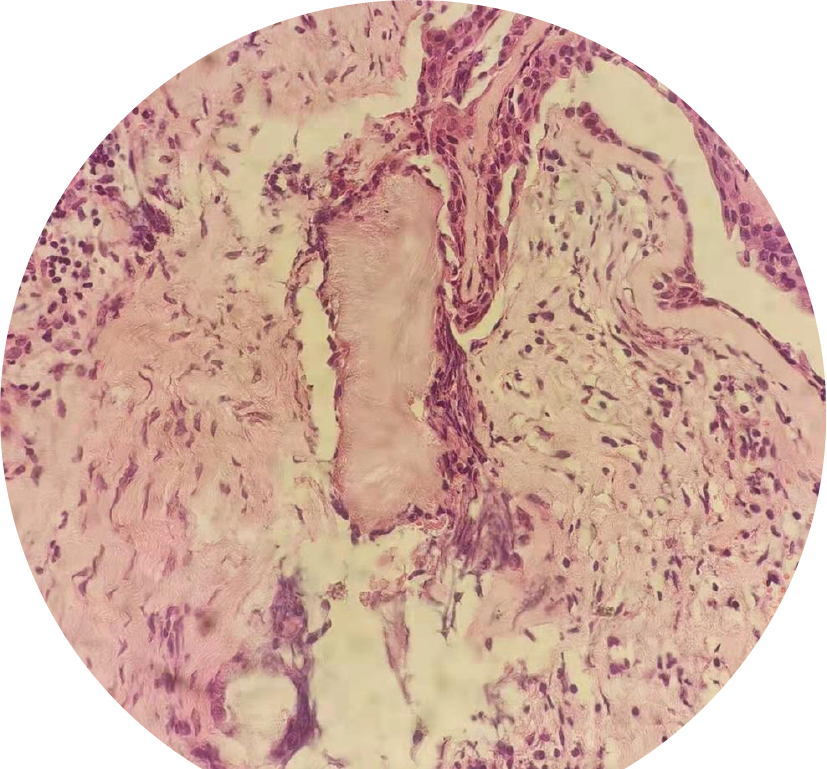
The accurate diagnosis of nasal gouty tophus was confirmed by postoperative histopathological examination (urate crystallized and granulation tissue formed around the tumour) (Figure 4).
The patient underwent nasal lumpectomy and autologous cartilage graft repair under general anaesthesia. During the operation, the skin and subcutaneous tissues were incised. The deep capsule of the mass was incomplete, the left nasal bone compressed and absorbed, the bone defect obvious, and the surface of the right bone not smooth. The tumour was completely removed along the residual bone. Its contents showed yellowish silt-like changes, and 0.5 mL of yellowish viscous caseous secretions were extracted from the tumour. Nasal endoscopy detected no fistula in the nasal cavity. The operative region was flushed with normal saline, and no liquid flowed out of the nose. Cartilage from the left tragus was taken to repair the nasal bone defect, and the skin was continuously sutured subcutaneously with 4-0 absorbable protein thread and bandaged under pressure. Postoperatively, the patient received anti-infection treatment and was advised to relinquish drinking, pay attention to a gout-suitable diet, and engage in active follow-up at the internal medicine department for the regulation of SUA levels.
There was no recurrence in nearly 2 years after operation (Figure 5).
The essence of gout inflammation is the deposition of monosodium urate (MSU) in bone, joint, kidney, and subcutaneous tissue, which leads to tissue damage and inflammation[9]. The development of inflammation depends on changes in the surface protein for MSU crystals. Repeated inflammation depends on the innate immune response mediated by the MSU crystal. Gouty tophus is a granulomatous substance formed by urate crystals encapsulated by monocytes and multinucleated giant cells. Gouty tophus is mainly composed of three layers[3]: (1) MSU crystals forming the centre of the gouty tophus; (2) Monocytes and multinucleated macrophages that are wrapped around the MSU crystal; and (3) Dense connective tissue constituting the outermost layer. Age, sex, genetic susceptibility, SUA level, disease duration, metabolic syndrome, lifestyle, drugs, high purine diet, and drinking are risk factors for gout[10-12]. Gouty tophus is a sign of chronic gout. The formation of gouty tophus can lead to bone destruction, joint deformity, joint dysfunction, fracture, and infection of gouty tophus, seriously affects the quality of life of patients.
The gold standard for the diagnosis of gout is the detection of birefringent acicular urate crystals in joint fluid or gouty tophus under a polarised light microscope. In China, HUA is defined as the condition of a normal purine diet, in which the fasting SUA level is higher than 420 μmol/L (7 mg/dL) in men and 360 μmol/L (6 mg/dL) in women. Nonetheless, the definition of HUA varies widely across published studies in different countries, ranging from 6 to 7 mg/dL[13], and the clinical diagnosis of gout should be considered with the onset of characteristic arthritis, urinary calculi, or renal colic occurrence. In the chronic stage of gout, X-ray and conventional CT examinations can better reveal bone and joint destruction in patients, and can show the characteristic chisel-like and worm-like changes with high specificity; however, they are only suitable for the evaluation of bone destruction in patients with late gout. Magnetic resonance imaging (MRI) has shown that in the early stages of gout, though crystal deposition cannot be observed with the naked eye, the display level is clear, diagnostic sensitivity is high, and the diagnostic value is favourable on MRI. However, because of the high cost and long appointment period, MRI is rarely used in clinical practice. In recent years, the application of dual-energy CT (DECT) in the diagnosis and treatment of gout has become a popular research topic[14-16]. It can identify the chemical composition of urate crystals and the deposition of urate in deep tissues, which can be applied to a patient’s whole body. With the improvement in ultrasound resolution, ultrasound can be used to observe urate crystals, gouty tophus, and bone erosion damage as well as evaluate joint inflammation[17,18]. It has become an effective means of diagnosing gout and monitoring the effect of reducing uric acid levels.
The current patient's SUA level was 384 μmol/L (in China, the reference value is 208–428 μmol/L). He took febuxostat regularly for teen years, and his SUA level was regularly reviewed in the outpatient department. The uric acid level was well under control for several years. When he was diagnosed with gout 13 years ago, gouty tophi appeared in his lower limbs, feet, and ankles. Although his SUA level was reduced to normal by drug treatment, he drank alcohol for a prolonged period and enjoyed consuming seafood with high purine. The patient was convinced that the gout condition was well under control, in recent years, the symptoms of foot and ankle gouty tophus had not been aggravated, and because the occurrence of gouty tophus in the head and neck is extremely rare, the nasal gouty tophus was not considered the main diagnosis before the operation. Nasal ultrasound examination was not performed before the operation, and the patient refused the puncture cytology examination; therefore, it was impossible to make a definite diagnosis before the operation. A CT scan of the nose revealed bone erosion of the tumour, and considering the possibility of a malignant tumour of the nose[19] , we did not perform an external inverted-V incision along the columella, in case of residual tumour. Subsequent to complete exposure of the tumour during the operation, the capsule could be observed surrounding the tumour. There was sand-like filling and rice swill water liquid in the tumour; we considered it a gouty tophus infection that caused exudate formation, although the bacterial and fungal cultures were negative[10]. The diagnosis of gouty tophus lesions was confirmed during the operation and by postoperative pathology. The auricle lesions were mild, and surgery was not performed. Therefore, attention should be directed to the formation of tumours in atypical parts of the body and atypical chondritis in gout patients without HUA as well as to the establishment of a clinical understanding of gouty tophus to prevent misdiagnosis[20].
Gouty tophus can be deposited in different parts of the human body, which can be categorised into typical and atypical parts[21]. Gouty tophus in the head and neck is atypical and rarely observed in the bridge of the nose[22]. In addition, gout often mimics the process of malignant tumours, infections, or other unrelated diseases. A few reports have described the deposition of gout in unusual body parts[23-26]. Therefore, a more systematic, scientific, and comprehensive diagnosis of gout is necessary. In 2015, the American College of Rheumatology/European Alliance Against Rheumatology developed new classification criteria for gout[27]; ultrasound and DECT were included in the gout classification for the first time. If patients met the diagnostic criteria of clinical, laboratory, and imaging examinations, the sensitivity and specificity of diagnosis could be as high as 92%, which also stratified the level of SUA, taking into account that SUA level may not be high during a gout attack. After a definite diagnosis, we further emphasise that drug treatment of patients with gout is particularly important[28-30]. The recommended serum uric acid level is below 6 mg/dL in all gouty patients or 5 mg/dL in severe gout patients to allow more rapid dissolution of the crystals[23].
Why a multiple gouty tophi in the head and neck with normal serum uric acid have been developed in this patient? The possible reason is that although the blood uric acid decreased to normal through drug treatment, the gouty tophus symptoms did not stop developing with the normal blood uric acid due to long-term drinking and eating seafood high purine diet, and gradually occurred in the auricle and nasal, which did not attract enough attention from the patient. Another important reason is that although the patient's blood uric acid is in the normal range, it is still not low enough. The blood uric acid of patients with gout stone should be controlled at 5 mg/dL.
This report describes a case of gouty tophus with normal SUA in an atypical location and atypical symptoms. In clinical settings, especially for patients with normal SUA, the possibility of atypical symptoms and atypical parts of gouty tophus should be considered. Strict control of diet, drinking habits, and SUA levels are needed to avoid the progression of gouty tophus and the development of more serious complications. Surgery is an effective treatment method for gouty tophus.
We would like to thank all the participating departments for their cooperation.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Molla MD S-Editor: Zhang H L-Editor: A P-Editor: Zhang H
| 1. | Dalbeth N, Merriman TR, Stamp LK. Gout. Lancet. 2016;388:2039-2052. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 623] [Cited by in RCA: 727] [Article Influence: 80.8] [Reference Citation Analysis (1)] |
| 2. | Robinson PC, Horsburgh S. Gout: joints and beyond, epidemiology, clinical features, treatment and co-morbidities. Maturitas. 2014;78:245-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 3. | Chhana A, Dalbeth N. The gouty tophus: a review. Curr Rheumatol Rep. 2015;17:19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 84] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 4. | Taylor WJ, Fransen J, Dalbeth N, Neogi T, Schumacher HR, Brown M, Louthrenoo W, Vazquez-Mellado J, Eliseev M, McCarthy G, Stamp LK, Perez-Ruiz F, Sivera F, Ea HK, Gerritsen M, Scire C, Cavagna L, Lin C, Chou YY, Tausche AK, da Rocha Castelar-Pinheiro G, Janssen M, Chen JH, Slot O, Cimmino M, Uhlig T, Jansen TL. Performance of classification criteria for gout in early and established disease. Ann Rheum Dis. 2016;75:178-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Sung KT, Lo CI, Lai YH, Tsai JP, Yun CH, Hsiao CC, Kuo JY, Hou CJ, Hung TC, Su CH, Hung CL, Yeh HI. Associations of serum uric acid level and gout with cardiac structure, function and sex differences from large scale asymptomatic Asians. PLoS One. 2020;15:e0236173. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | McQueen FM, Chhana A, Dalbeth N. Mechanisms of joint damage in gout: evidence from cellular and imaging studies. Nat Rev Rheumatol. 2012;8:173-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 61] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 7. | Lee JS, Kwon OC, Oh JS, Kim YG, Lee CK, Yoo B, Hong S. Clinical features and recurrent attack in gout patients according to serum urate levels during an acute attack. Korean J Intern Med. 2020;35:240-248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 8. | Ragab G, Elshahaly M, Bardin T. Gout: An old disease in new perspective - A review. J Adv Res. 2017;8:495-511. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 299] [Cited by in RCA: 307] [Article Influence: 38.4] [Reference Citation Analysis (0)] |
| 9. | Saccomano SJ, Ferrara LR. Treatment and prevention of gout. Nurse Pract. 2015;40:24-30; quiz 30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Dalbeth N, Bardin T, Doherty M, Lioté F, Richette P, Saag KG, So AK, Stamp LK, Choi HK, Terkeltaub R. Discordant American College of Physicians and international rheumatology guidelines for gout management: consensus statement of the Gout, Hyperuricemia and Crystal-Associated Disease Network (G-CAN). Nat Rev Rheumatol. 2017;13:561-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 66] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 11. | Khanna D, Fitzgerald JD, Khanna PP, Bae S, Singh MK, Neogi T, Pillinger MH, Merill J, Lee S, Prakash S, Kaldas M, Gogia M, Perez-Ruiz F, Taylor W, Lioté F, Choi H, Singh JA, Dalbeth N, Kaplan S, Niyyar V, Jones D, Yarows SA, Roessler B, Kerr G, King C, Levy G, Furst DE, Edwards NL, Mandell B, Schumacher HR, Robbins M, Wenger N, Terkeltaub R; American College of Rheumatology. 2012 American College of Rheumatology guidelines for management of gout. Part 1: systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia. Arthritis Care Res (Hoboken). 2012;64:1431-1446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1168] [Cited by in RCA: 1108] [Article Influence: 85.2] [Reference Citation Analysis (1)] |
| 12. | Towiwat P, Li ZG. The association of vitamin C, alcohol, coffee, tea, milk and yogurt with uric acid and gout. Int J Rheum Dis. 2015;18:495-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 13. | Richette P, Doherty M, Pascual E, Barskova V, Becce F, Castaneda J, Coyfish M, Guillo S, Jansen T, Janssens H, Lioté F, Mallen CD, Nuki G, Perez-Ruiz F, Pimentao J, Punzi L, Pywell A, So AK, Tausche AK, Uhlig T, Zavada J, Zhang W, Tubach F, Bardin T. 2018 updated European League Against Rheumatism evidence-based recommendations for the diagnosis of gout. Ann Rheum Dis. 2020;79:31-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 230] [Article Influence: 46.0] [Reference Citation Analysis (0)] |
| 14. | Shang J, Zhou LP, Wang H, Liu B. Diagnostic Performance of Dual-energy CT Versus Ultrasonography in Gout: A Meta-analysis. Acad Radiol. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 15. | Bongartz T, Glazebrook KN, Kavros SJ, Murthy NS, Merry SP, Franz WB 3rd, Michet CJ, Veetil BM, Davis JM 3rd, Mason TG 2nd, Warrington KJ, Ytterberg SR, Matteson EL, Crowson CS, Leng S, McCollough CH. Dual-energy CT for the diagnosis of gout: an accuracy and diagnostic yield study. Ann Rheum Dis. 2015;74:1072-1077. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 215] [Cited by in RCA: 190] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 16. | Chen J, Liao M, Zhang H, Zhu D. Diagnostic accuracy of dual-energy CT and ultrasound in gouty arthritis : A systematic review. Z Rheumatol. 2017;76:723-729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Ward IM, Scott JN, Mansfield LT, Battafarano DF. Dual-Energy Computed Tomography Demonstrating Destructive Calcium Pyrophosphate Deposition Disease of the Distal Radioulnar Joint Mimicking Tophaceous Gout. J Clin Rheumatol. 2015;21: 314-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | McQueen FM, Doyle A, Dalbeth N. Imaging in gout--what can we learn from MRI, CT, DECT and US? Arthritis Res Ther. 2011;13:246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 55] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 19. | Christiansen SN, Østergaard M, Slot O, Fana V, Terslev L. Ultrasound for the diagnosis of gout-the value of gout lesions as defined by the Outcome Measures in Rheumatology ultrasound group. Rheumatology (Oxford). 2021;60:239-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 20. | Gentili A. The advanced imaging of gouty tophi. Curr Rheumatol Rep. 2006;8:231-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 21. | Wu JC, Chou PY, Chen CH. Nasal gouty tophus: Report a rare case presenting as a nasal hump with nasal obstruction. Biomed J. 2016;39:295-297. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Le Goff B, Berthelot JM, André V, Guillot P, Maugars Y. Ultrasonography for diagnosing atypical gout. Two case reports. Joint Bone Spine. 2008;75:610-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Chen SL, Chen JR, Yang SW. Painless gouty tophus in the nasal bridge: A case report and literature review. Medicine (Baltimore). 2019;98:e14850. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Kim YS, Lee MK, Yi Y. Atypical musculoskeletal manifestations on flexor hallucis longus tendon of gout causing tarsal tunnel syndrome in diabetic patients: A case report. Medicine (Baltimore). 2019;98:e18374. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Saliba J, Sakano H, Friedman RA, Harris JP. Tophaceous Gout of the Middle Ear: Case Reports and Review of the Literature. Audiol Neurootol. 2019;24:51-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 26. | Ministrini S, Baronio G, Zorzi F, Bercich L, Grazioli L, Molfino S, Portolani N. Unusual presentation of gouty tophus in the liver with subsequent appearance in the same site of HCC: a correlate diagnosis? World J Surg Oncol. 2019;17:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 27. | Dhaduk R, Weber S, Fallat LM. Gouty Tophi in Sinus Tarsi of Bilateral Feet Mimicking Synovial Sarcoma:A Case Report. J Foot Ankle Surg. 2019;58:347-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 28. | Neogi T, Jansen TL, Dalbeth N, Fransen J, Schumacher HR, Berendsen D, Brown M, Choi H, Edwards NL, Janssens HJ, Lioté F, Naden RP, Nuki G, Ogdie A, Perez-Ruiz F, Saag K, Singh JA, Sundy JS, Tausche AK, Vaquez-Mellado J, Yarows SA, Taylor WJ. 2015 Gout classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis. 2015;74:1789-1798. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 577] [Cited by in RCA: 532] [Article Influence: 53.2] [Reference Citation Analysis (0)] |
| 29. | Scheepers LEJM, van Onna M, Stehouwer CDA, Singh JA, Arts ICW, Boonen A. Medication adherence among patients with gout: A systematic review and meta-analysis. Semin Arthritis Rheum. 2018;47:689-702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 113] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 30. | Pascart T, Lioté F. Gout: state of the art after a decade of developments. Rheumatology (Oxford). 2019;58:27-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 53] [Article Influence: 8.8] [Reference Citation Analysis (0)] |