Published online Feb 6, 2022. doi: 10.12998/wjcc.v10.i4.1255
Peer-review started: March 14, 2021
First decision: April 23, 2021
Revised: November 15, 2021
Accepted: December 7, 2021
Article in press: December 7, 2021
Published online: February 6, 2022
Processing time: 311 Days and 18.7 Hours
Patella baja is a severe complication after knee injury or surgery, resulting in pain and impaired movement. This disorder is also a substantial challenge for orthopaedic surgeons. Currently, no consensus exists regarding the gold standard management of patella baja. If not appropriately treated, significant dysfunction of the knee joint will occur.
A 46-year-old man with a left patellar fracture was treated with tension band fixation at a local hospital. He had undergone a second operation at the same hospital because of limited knee flexion 6 mo after surgery. Unfortunately, the patellar tendon was ruptured. The patellar tendon was subsequently repaired using an ipsilateral semitendinosus tendon. Two years later, the patient presented to our department with knee pain and loss of range of motion. Autogenous iliotibial band (ITB) enhancement combined with sagittal tendon lengthening plasty was used to improve the symptoms of the knee joint. The patient was followed up for 2 years. The knee joint function of the patient returned to the normal level.
We successfully treated patella baja using autogenous ITB enhancement combined with sagittal tendon lengthening plasty.
Core tip: Patella baja combined with knee dysfunction can be observed in patients with patellar trauma. If not properly managed, joint stiffness and patellofemoral arthritis will occur, seriously affecting quality of life. Various therapeutic approaches are available, but no consensus exists regarding which is the best surgical approach. In this case report, we used our approach to treat patella baja using autogenous iliotibial band enhancement combined with tendon lengthening plasty to restore knee function with remarkable results.
- Citation: Tang DZ, Liu Q, Pan JK, Chen YM, Zhu WH. Autogenous iliotibial band enhancement combined with tendon lengthening plasty to treat patella baja: A case report. World J Clin Cases 2022; 10(4): 1255-1262
- URL: https://www.wjgnet.com/2307-8960/full/v10/i4/1255.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i4.1255
Patella baja is a condition in which the patella is positioned abnormally low relative to the femoral trochlea. Patella baja is normally classified into three types: congenital acquired and mixed[1]. Although the exact pathological mechanism of acquired patella baja remains unclear, several contributing factors have been reported, such as cicatricial hyperplasia of the patellar tendon after total knee arthroplasty, complete resection of the infrapatellar fat pad, chronic injury of the femoral quadriceps, and long-term immobilization after knee surgery[2-4].
Knee pain and dysfunction are the main clinical manifestations of acquired patella baja. If not addressed properly, joint stiffness and patellofemoral arthritis will occur, significantly affecting quality of life[5]. In contrast to conservative treatments, timely and effective surgical interventions play a key role in improving knee function. Although many surgical procedures have been attempted to manage this pathology[6-10], no consensus exists regarding which is the best option. In this case report, we used our method to treat patella baja using autogenous iliotibial band (ITB) enhancement combined with tendon lengthening plasty.
A 46-year-old man was admitted to our hospital because of left knee pain and loss of range of motion (ROM) for 2 years.
The patient had a left patellar fracture and was treated with tension band fixation at a local hospital 2 years prior. He had undergone a second operation at the same hospital because of limited knee flexion 6 mo after the surgery. The surgeon removed the internal fixation and performed manipulation under anaesthesia. Unfortunately, the patellar tendon was ruptured. The patellar tendon was subsequently repaired using an ipsilateral semitendinosus tendon.
No remarkable personal and family history.
No special personal and family history.
Physical examination on admission revealed a longitudinal surgical scar of approximately 15 cm in length on the left knee joint, without obvious skin damage or ulceration. The patient presented with a lameness gait and pain in the knee, left quadriceps atrophy, and knee flexion limited by 45°. The Lysholm score and International Knee Documentation Committee (IKDC) score were 50 and 40, respectively.
The laboratory findings were normal.
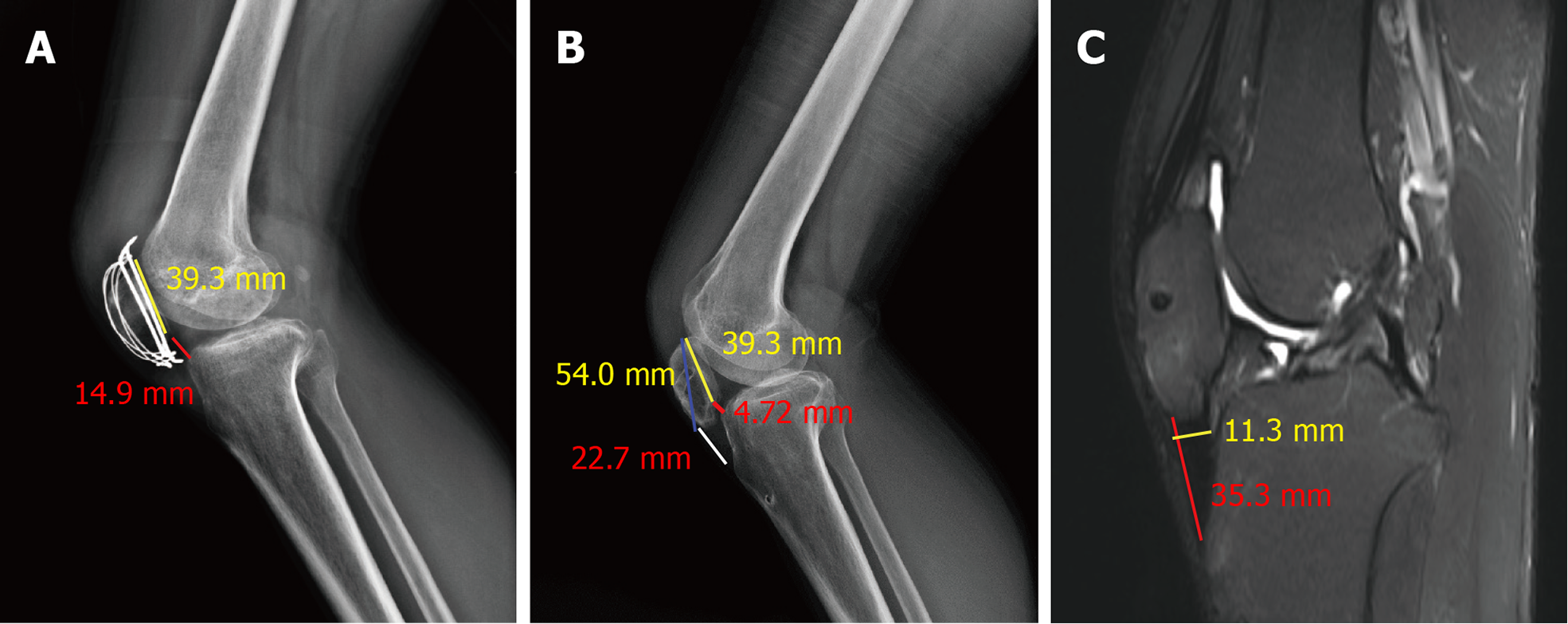
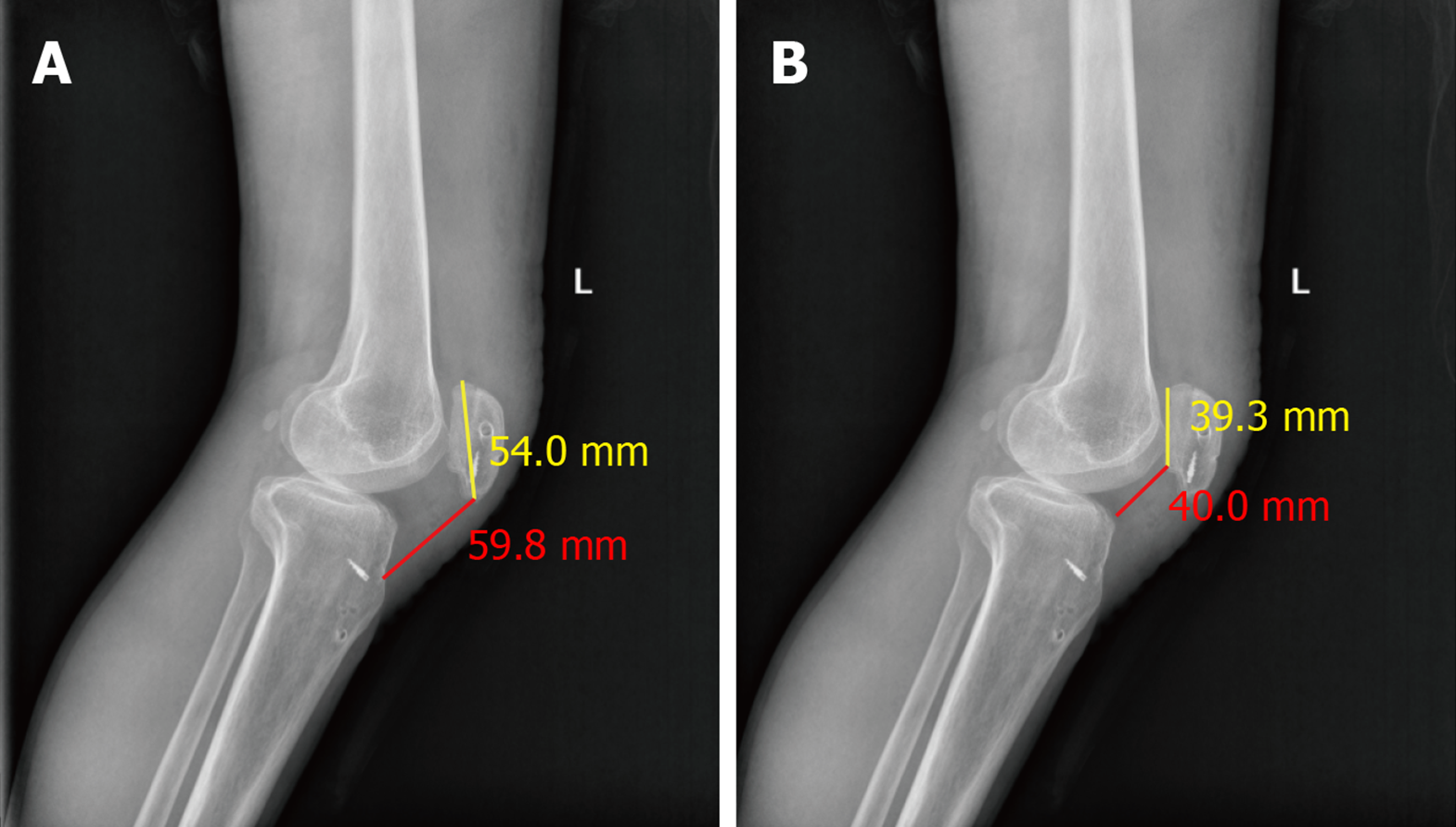
The patient was diagnosed with patella baja using a lateral-view radiograph of his left knee (Figure 1A–1C). Magnetic resonance imaging (MRI) further demonstrated that the patellar tendon was contracted and thickened (Figure 1C).
The final diagnosis was left patella baja and post-traumatic knee dysfunction.
We used our method to treat patella baja using autogenous ITB enhancement combined with tendon lengthening plasty.
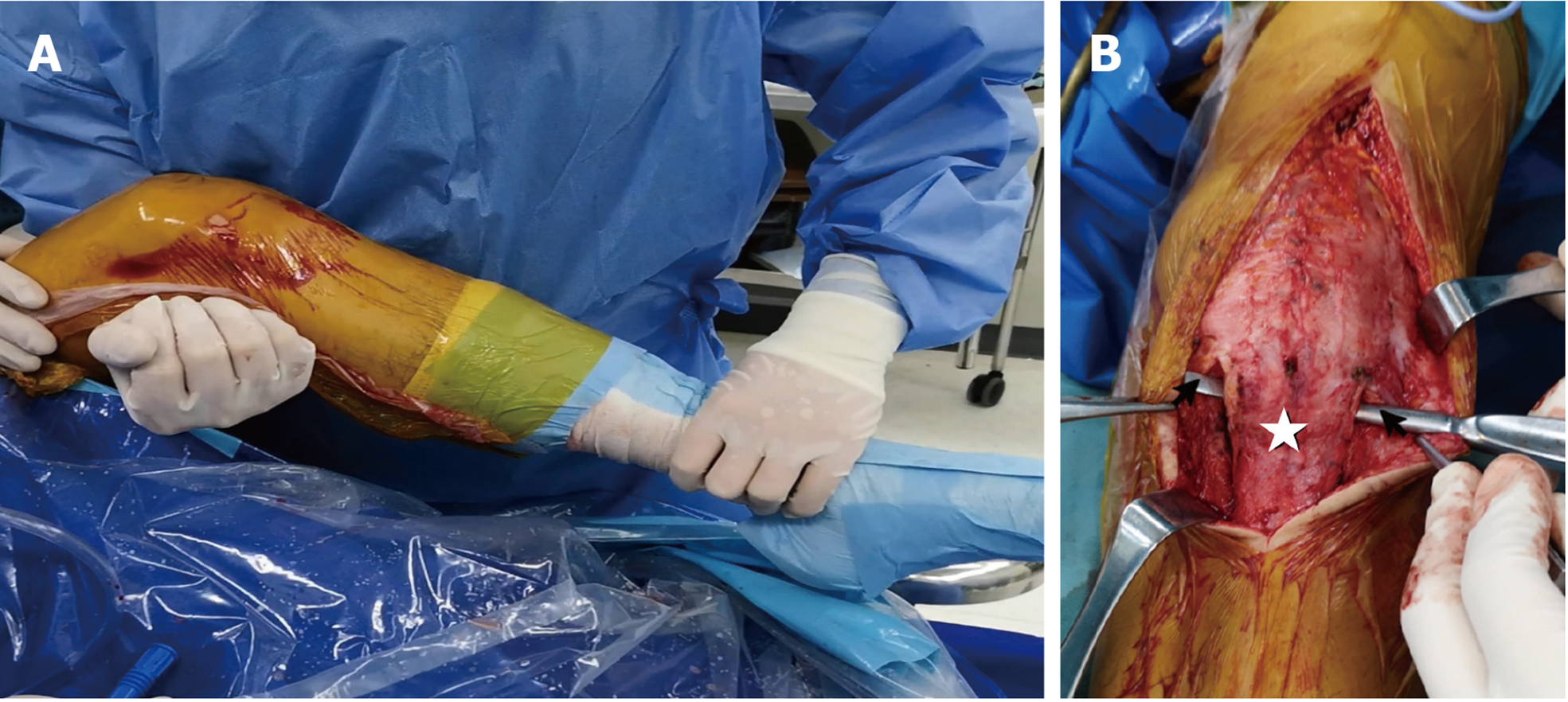
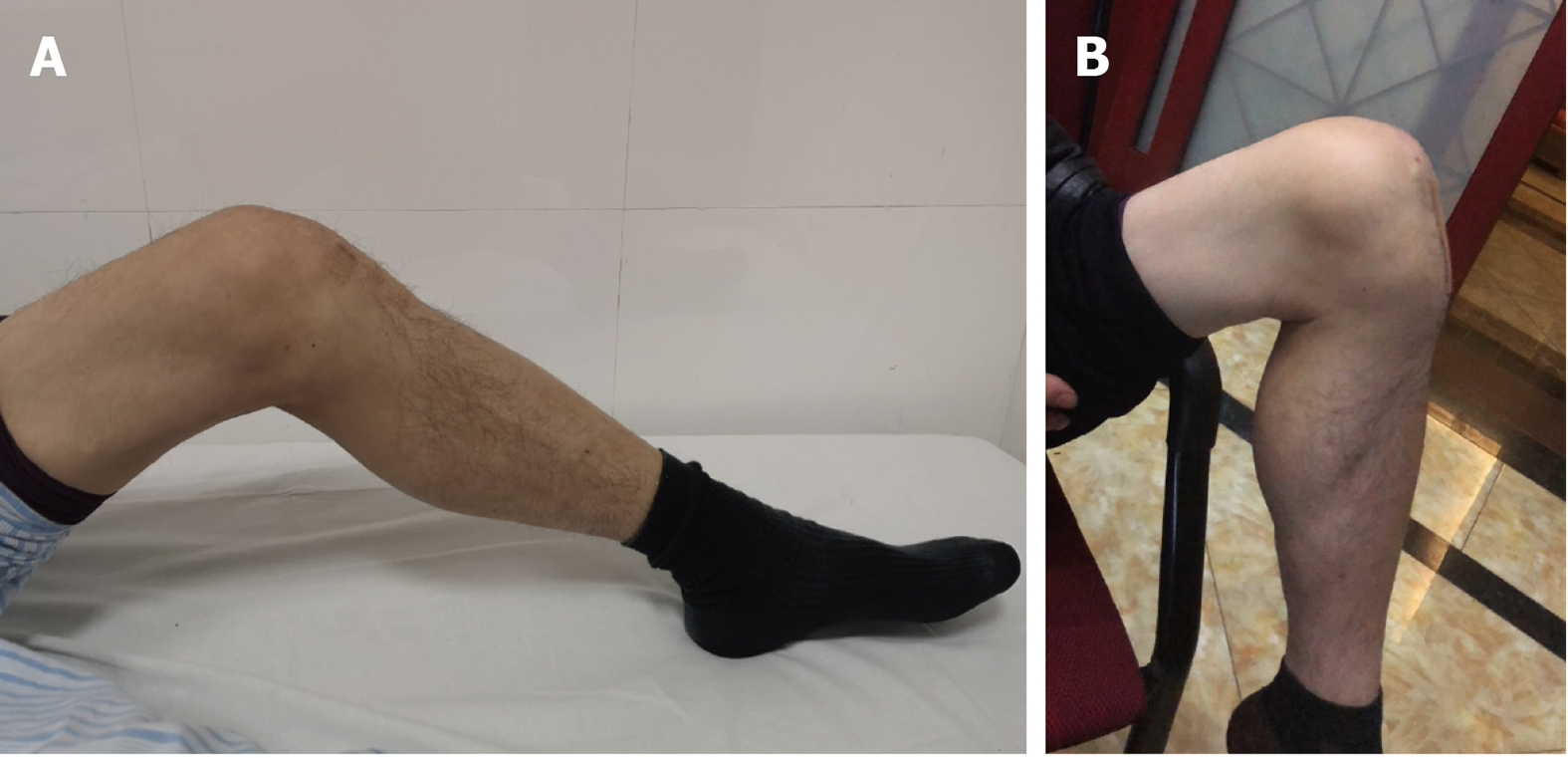
A tourniquet was placed on the left thigh, with the patient in the supine position. Manipulation under anaesthesia was performed. Arthroscopic examination found a large amount of scar tissue and synovial hyperplasia in the joint. Although extensive arthrolysis was then performed by debriding fibrotic scar tissue in the suprapatellar bursa, medial recess, lateral recess, and intercondylar fossa, the ROM of the knee joint was 0°–65° (Figure 2A), and the patellar mobility was not significantly improved. Therefore, open surgery to lengthen the patellar tendon was conducted.
The approach was made along the original incision extending from 5 cm above the superior pole of the patella to the tibial tubercle (Figure 2B). After removing scar tissue surrounding the patella and patellar tendon, a minor increase in ROM was observed. The patellar tendon was subsequently freed and prepared for lengthening.
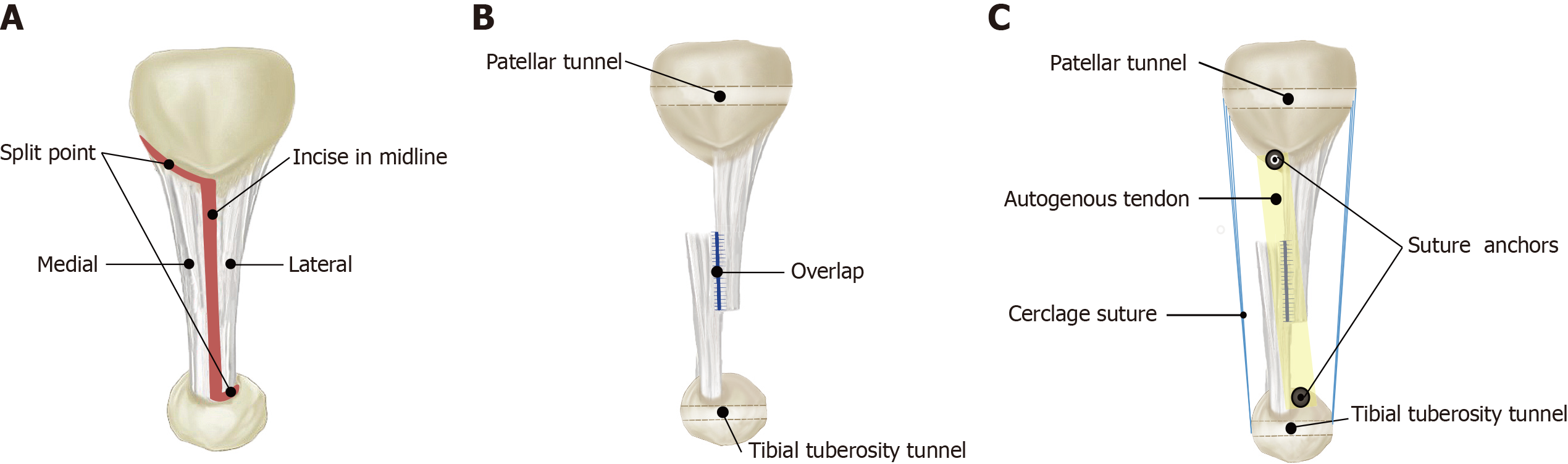
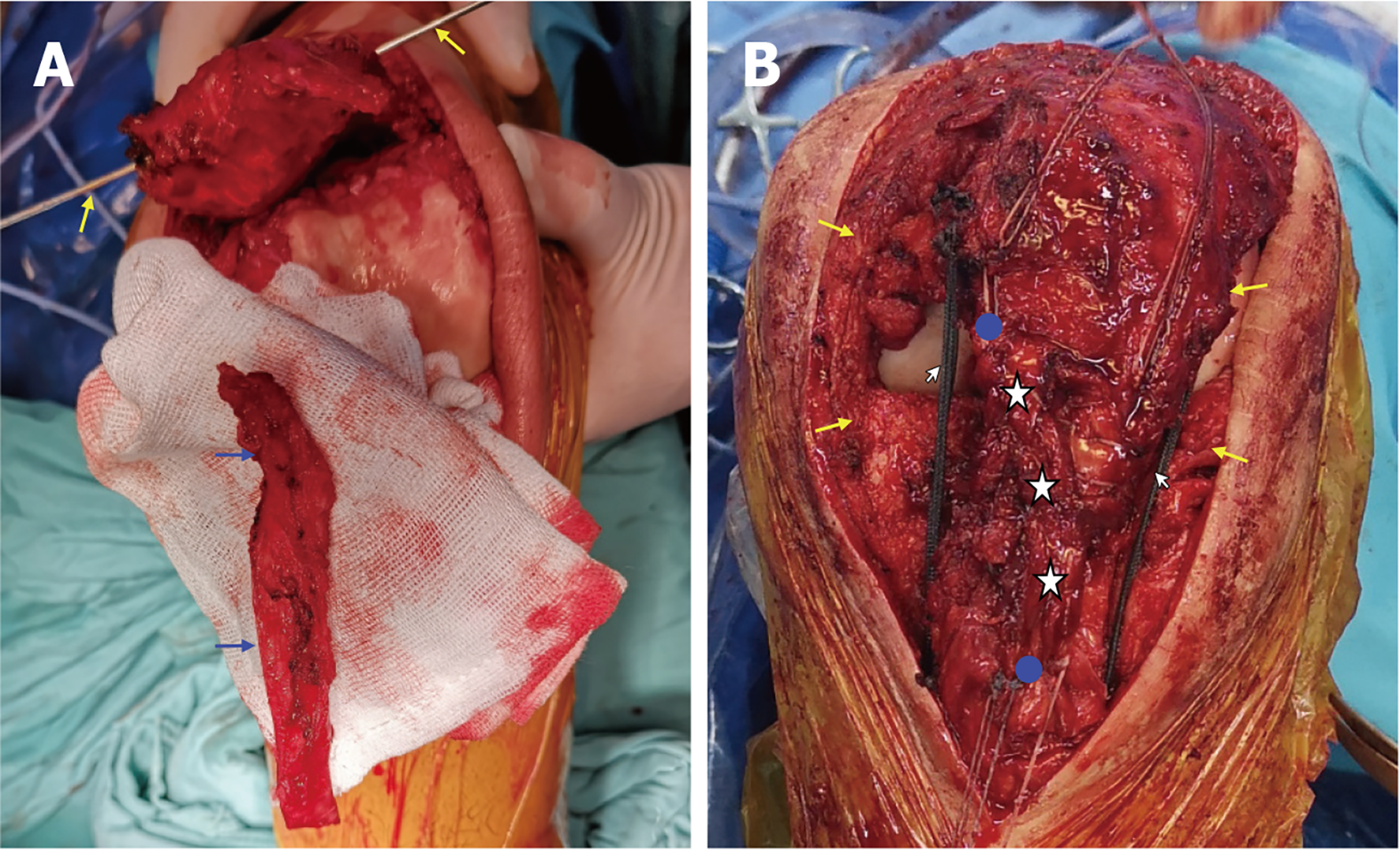
The length of the patellar tendon was approximately 35 mm (Figure 3A). The medial patellar insertion and lateral tibial insertion of the patellar tendon were carefully preserved when splitting along the midline (Figure 3B). Next, the patella was overturned upwards with the knee in 90° of flexion to assess the tendon length. The distance to be prolonged for the patient was approximately 60 mm, and the overlapping distance of the two free tendon ends was approximately 10 mm (Figure 3B). An ultrabraid suture (#2; Smith & Nephew, Andover, FL, USA) was used to overlap the tendon ends in a whipstitch fashion. To enhance the reconstructed patellar tendon, a 60 mm ITB graft was harvested (Figure 4A). The ITB graft was first fixed at the proximal and distal insertion of the patellar tendon by two TWINFIX Ti 3.5 mm suture anchors (Smith & Nephew) (Figure 3C), and then the graft and patellar tendon were sutured together using ultrabraid sutures. The length of the graft was calculated to avoid excess. Three MB66 polyester sutures (#5; Ethicon) were passed through the tibial and patellar bone tunnels as cerclage to avoid high tension when flexing the knee (Figure 4B). The ROM of the knee improved to 100°. Intraoperative fluoroscopy showed that the height of the patella was significantly recovered, with a Carton index of 1.0. After rinsing the wound thoroughly, it was closed normally, and drainage was left.
The patient was allowed partial weight-bearing using crutches with hinged knee brace protection on postoperative day 1. Straight-leg raises, ankle pump exercise and continuous passive motion were started within the first week after surgery. The initial ROM was limited between 0° and 15° for the first week after the procedure. An increment of 15° was allowed every week, and the ROM was increased to 90° by 6 wk. Full weight-bearing and unrestricted ROM were allowed after 2 mo, and the brace was discontinued after 3 mo.
The postoperative radiograph showed that the patellar height was almost normal (Figure 5). The patient was followed up for 2 years. At the final follow-up, the ROM of his knee was 0° to 120° (Figure 6). Additionally, the Lysholm score and IKDC score improved to 92 and 86, respectively.
Patella baja is a severe complication after knee injury or surgery, resulting in pain and impaired movement. The specific aetiology of this disorder remains unknown. Currently, no consensus exists regarding the gold standard management of patella baja. We have successfully treated patients with a history of multiple knee surgeries. Notably, our case had severe scar hyperplasia in the knee and contracture of the patellar tendon, which was of poor quality. The combination of patellar tendon lengthening and ITB enhancement to treat patella baja was suitable for this patient. Additionally, this treatment does not cause additional surgical trauma. Previous studies have attempted various methods to treat patella baja. In et al[8] used the classic Ilizarov technique to prolong the patellar tendon. Although the symptoms of the patient were considerably improved, the affected limb must be fixed for 3 mo, increasing the risk of joint stiffness. The modified Z-shaped plasty used by Guido et al[10] was a successful technique, but these patients did not have rupture of the patellar tendon and did not undergo patellar tendon surgery; thus, the patellar tendon was of relatively good quality. Modified Z-plasty would not be suitable for these patients. Bruhin et al[7] connected the patellar tendon with the quadriceps femoris surface using a transplanted tendon. Although this method does not affect tendon stress distribution and blood supply, it may cause certain restrictions on the quadriceps femoris. Additionally, transposition of the tibial tuberosity is a common technique to address patella baja[6,9]. However, complications were observed such as avulsion of the tibial tubercle and rupture of the patellar tendon. Judet’s quadriceps muscle is the modality applied to describe a surgical procedure of the quadriceps muscle to improve knee flexion in severely ankylosed knees[11,12]. Although Judet’s technique of disinsertion and muscle sliding is a useful technique in fixed knee extension contracture, it has an obvious disadvantage of a long incision and major invasiveness. Here, we reported a complex case of patella baja. A detailed and individualised surgical plan was customised preoperatively: arthroscopic arthrolysis, extensive resection of hyperplastic scar tissue, sagittal Z-plasty for patellar tendon lengthening, autogenous ITB transplantation for enhancement, and suture cerclage for decreased tension. Arthroscopic surgery to treat knee stiffness has been reported with satisfactory results[13,14]. At the beginning of the operation, we performed arthrolysis on the patient’s knee joint under arthroscopy. However, the ROM was not obviously promoted after arthroscopic release; thus, we converted to open surgery. After thoroughly debriding the scar tissue around the patella and patellar tendon, the patellar tendon was equally split and overlapped to ensure a sufficient length when flexing the knee at 90°. To use the contracted patellar tendon more accurately, before surgery, the patellar tendon was evaluated and measured on MRI. After thorough debridement during the operation, the patellar tendon was measured again and compared with the preoperative measurements. Notably, the insertions of the patellar tendon at the patella and tibial tuberosity were well preserved, benefiting the mechanical properties and blood supply of the tendon. Furthermore, we used an autogenous ITB graft to strengthen the lengthened patellar tendon. Autogenous graft transplantation can not only provide mechanical enhancement but may also promote tendon healing[15-17]. Intraoperatively, ITB is used for patellar tendon enhancement, which will not cause additional surgical trauma. Additionally, considering that high-performance suture materials provide better stability[18], we passed three MB66 sutures as cerclage in the bone tunnels to reduce the tension. This suture cerclage may decrease the risk of rupture after surgery.
We analysed the possible reasons for patella baja of our patient. First, the local orthopaedic surgeon left a relatively long end of the K-wire at the index operation. The long end of the K-wire might irritate the patellar tendon and quadriceps tendon, making rehabilitation challenging[19,20]. Second, it is a common phenomenon that patients who were treated at county-level hospitals did not have a systematic rehabilitation protocol in China. Presently, our government is strengthening the construction of a community rehabilitation medical centre. Finally, the patellar tendon ruptured when performing manipulation under anaesthesia during the second surgery. This may be related to the insufficient release of intra-articular adhesion.
This case had several limitations. First, the harvested ITB may cause pain in the graft harvest site, which depends on the intraoperative condition and surgeon’s experience. Second, more cases are needed to verify the effectiveness of our method. Third, the follow-up was short.
Importantly, much knowledge was gained from the patient’s prior surgery. We reviewed the patient’s medical records and radiological data, which helped to plan the detailed surgical procedures and avoid possible intraoperative pitfalls.
We successfully treated patella baja using autogenous ITB enhancement combined with sagittal tendon lengthening plasty. The repair and enhancement of the patellar tendon were achieved effectively and is a worthwhile approach for patients who have had multiple knee surgeries.
We thank our patient for consenting to have his case presented and published.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Yukata K S-Editor: Gong ZM L-Editor: Kerr C P-Editor: Gong ZM
| 1. | Lum ZC, Saiz AM, Pereira GC, Meehan JP. Patella Baja in Total Knee Arthroplasty. J Am Acad Orthop Surg. 2020;28:316-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 2. | Paulos LE, Wnorowski DC, Greenwald AE. Infrapatellar contracture syndrome. Diagnosis, treatment, and long-term followup. Am J Sports Med. 1994;22:440-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 111] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Davies GS, van Duren B, Shorthose M, Roberts PG, Morley JR, Monk AP, Murray DW, Pandit HG. Changes in patella tendon length over 5 years after different types of knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016;24:3029-3035. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 4. | Gwyn R, Kotwal RS, Holt MD, Davies AP. Complete excision of the infrapatellar fat pad is associated with patellar tendon shortening after primary total knee arthroplasty. Eur J Orthop Surg Traumatol. 2016;26:545-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Fiquet C, White N, Gaillard R, Servien E, Neyret P, Lustig S. Combined Patellar Tendon lengthening and partial Extensor Mechanism Allograft reconstruction for the treatment of patella infera: A case report. Knee. 2019;26:515-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Caton JH, Dejour D. Tibial tubercle osteotomy in patello-femoral instability and in patellar height abnormality. Int Orthop. 2010;34:305-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 144] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 7. | Bruhin VF, Preiss S, Salzmann GM, Harder LP. Frontal Tendon Lengthening Plasty for Treatment of Structural Patella Baja. Arthrosc Tech. 2016;5:e1395-e1400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | In Y, Kim SJ, Kwon YJ. Patellar tendon lengthening for patella infera using the Ilizarov technique. J Bone Joint Surg Br. 2007;89:398-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Drexler M, Dwyer T, Marmor M, Sternheim A, Cameron HU, Cameron JC. The treatment of acquired patella baja with proximalize the tibial tuberosity. Knee Surg Sports Traumatol Arthrosc. 2013;21:2578-2583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Guido W, Christian H, Elmar H, Elisabeth A, Christian F. Treatment of patella baja by a modified Z-plasty. Knee Surg Sports Traumatol Arthrosc. 2016;24:2943-2947. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Oliveira VG, D'Elia LF, Tirico LE, Gobbi RG, Pecora JR, Camanho GL, Angelini FJ, Demange MK. Judet quadricepsplasty in the treatment of posttraumatic knee rigidity: long-term outcomes of 45 cases. J Trauma Acute Care Surg. 2012;72:E77-E80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Massè A, Biasibetti A, Demangos J, Dutto E, Pazzano S, Gallinaro P. The judet quadricepsplasty: Long-term outcome of 21 cases. J Trauma. 2006;61:358-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Biggs-Kinzer A, Murphy B, Shelbourne KD, Urch S. Perioperative rehabilitation using a knee extension device and arthroscopic debridement in the treatment of arthrofibrosis. Sports Health. 2010;2:417-423. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Chen MR, Dragoo JL. Arthroscopic releases for arthrofibrosis of the knee. J Am Acad Orthop Surg. 2011;19:709-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 15. | Mihalko WM, Vance M, Fineberg MJ. Patellar tendon repair with hamstring autograft: a cadaveric analysis. Clin Biomech (Bristol, Avon). 2010;25:348-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Black JC, Ricci WM, Gardner MJ, McAndrew CM, Agarwalla A, Wojahn RD, Abar O, Tang SY. Novel Augmentation Technique for Patellar Tendon Repair Improves Strength and Decreases Gap Formation: A Cadaveric Study. Clin Orthop Relat Res. 2016;474:2611-2618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 17. | Larson RV, Simonian PT. Semitendinosus augmentation of acute patellar tendon repair with immediate mobilization. Am J Sports Med. 1995;23:82-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 52] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Westberg SE, Acklin YP, Hoxha S, Ayranci C, Adeeb S, Bouliane M. Is suture comparable to wire for cerclage fixation? Shoulder Elbow. 2019;11:225-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Tian Y, Zhou F, Ji H, Zhang Z, Guo Y. Cannulated screw and cable are superior to modified tension band in the treatment of transverse patella fractures. Clin Orthop Relat Res. 2011;469:3429-3435. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 64] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 20. | Mao N, Liu D, Ni H, Tang H, Zhang Q. Comparison of the cable pin system with conventional open surgery for transverse patella fractures. Clin Orthop Relat Res. 2013;471:2361-2366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |