Published online Feb 6, 2022. doi: 10.12998/wjcc.v10.i4.1182
Peer-review started: September 16, 2021
First decision: November 7, 2021
Revised: November 20, 2021
Accepted: December 25, 2021
Article in press: December 25, 2021
Published online: February 6, 2022
Processing time: 130 Days and 2.4 Hours
Peritoneal dialysis (PD) catheter migration impedes the efficacy of dialysis. Therefore, several techniques involving additional sutures or incisions have been proposed to maintain catheter position in the pelvis.
To evaluate the efficacy of creating a short musculofascial tunnel beneath the anterior sheath of the rectus abdominis during PD catheter implantation.
Patients who underwent PD catheter implantation between 2015 and 2019 were included in this retrospective study. The patients were divided into two groups based on the procedure performed: Patients who underwent catheter implantation without a musculofascial tunnel before 2017 and those who underwent the procedure with a tunnel after 2017. We recorded patient characteristics and catheter complications over a two-year follow-up period. In addition, postoperative plain abdominal radiographs were reviewed to determine the catheter angle in the event of migration.
The no-tunnel and tunnel groups included 115 and 107 patients, respectively. Compared to the no-tunnel group, the tunnel group showed lesser catheter angle deviation toward the pelvis (15.51 ± 11.30 vs 25.00 ± 23.08, P = 0.0002) immediately after the operation, and a smaller range of migration within 2 years postoperatively (13.48 ± 10.71 vs 44.34 ± 41.29, P < 0.0001). Four events of catheter dysfunction due to migration were observed in the no-tunnel group, and none occurred in the tunnel group. There was no difference in the two-year catheter function survival rate between the two groups (88.90% vs 84.79%, P = 0.3799).
The musculofascial tunnel helps maintain catheter position in the pelvis and reduces migration, thus preventing catheter dysfunction.
Core Tip: We present a simple add-on procedure to the traditional open surgery method of peritoneal dialysis catheter implantation. Our method does not need an additional incision, suture, or change of surgical site. We analyzed images of the catheter and measured its deviation angle, which is related directly to the so-called “migration”. Indeed, patients who underwent the traditional method had a greater initial deviation angle and more angle shift in later images than did those who underwent the modified catheter implantation. This simple modification helps to maintain the catheter in the expected orientation, which will increase the efficacy of dialysis.
- Citation: Lee CY, Tsai MK, Chen YT, Zhan YJ, Wang ML, Chen CC. Importance of the creation of a short musculofascial tunnel in peritoneal dialysis catheter placement. World J Clin Cases 2022; 10(4): 1182-1189
- URL: https://www.wjgnet.com/2307-8960/full/v10/i4/1182.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i4.1182
Peritoneal dialysis (PD) is a widely applied therapy for long-term renal replacement. During PD, a catheter is essential for infusion and drainage of the dialysate. PD catheter implantation is performed by inserting a catheter through the abdominal wall and positioning the tip in the pelvic cavity, which is an ideal drainage site. However, in some patients, the catheter tip may migrate postoperatively, leading to flow dysfunction.
According to the guidelines published by the International Society for Peritoneal Dialysis (ISPD) in 2019[1], a 2.5-cm long musculofascial tunnel beneath the anterior sheath of the rectus abdominis is suggested to orient the catheter tip in the pelvis using the shape-memory of the straight catheter, which was first described in 1981[2]. Nevertheless, there is no current literature comparing the efficacy of this tunneling technique in reducing catheter migration with other procedures. Moreover, several studies[3-5] have described the “traditional” open surgical dissection technique without a musculofascial tunnel. However, those studies reported a higher catheter migration rate in comparison to other modified procedures, in which an additional skin incision[4] or supplementary sutures[5] were needed to “orient” the catheter downward.
In this study, we performed catheter insertion through the abdominal wall without a musculofascial tunnel before 2017 and noticed occasional catheter migration. In the subsequent year, we introduced the musculofascial tunnel technique as a routine procedure in our center. This retrospective study aimed to examine the efficacy of creating a short musculofascial tunnel beneath the anterior sheath of the rectus abdominis in PD implantation by comparing the catheter migration rates with those of PD implantation following the traditional procedure.
We retrospectively analyzed the medical records of patients who underwent PD catheter implantation from 2015 to 2019 at our hospital. The same surgical team performed all of the procedures, and all patients underwent open dissection surgery. Patients were divided into two groups: Patients who underwent catheter implantation without a musculofascial tunnel before 2017 and those who underwent the modified procedure with a tunnel after 2017. This retrospective study was approved by the Research Ethics Committee of NTUH (202106072RINA).
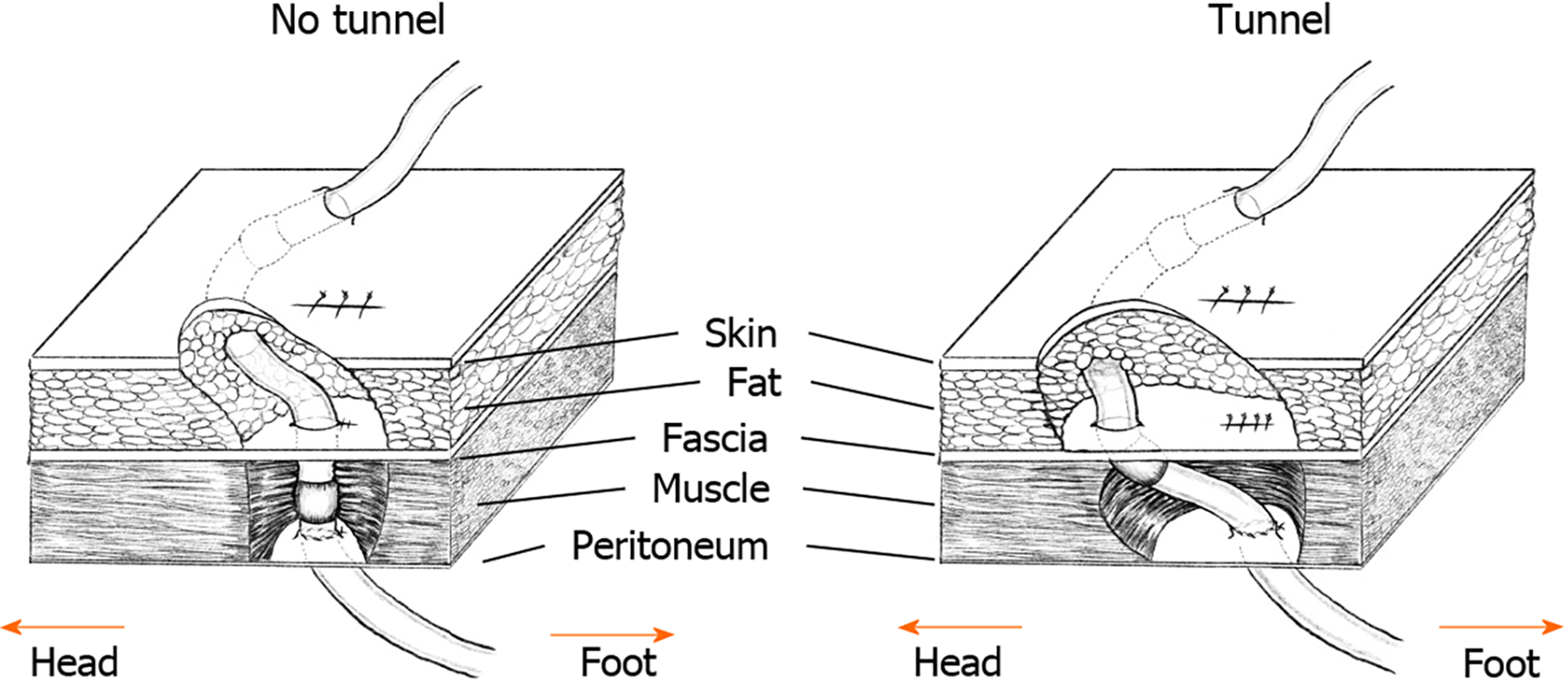
All patients received local anesthesia with intravenous sedation. The left side was preferred for surgery as the patients might be considered for future kidney transplantation using a right-sided approach. A 2–3-cm vertical incision was made over the lower rectus abdominis, and a small opening was created over the anterior sheath at the lower part of the incision. We then split the rectus abdominis bluntly to open the posterior sheath and peritoneum. After placing a purse-string suture, a 41 cm straight catheter with two cuffs (Covidien, Mansfield, United States) was inserted blindly toward the pelvis. In the no-tunnel group, the catheter was extracted from the rectus abdominis via the same opening in the anterior sheath, and the deep cuff was left in the muscle layer (Figure 1, left). In the tunnel group, we pierced the anterior sheath approximately 1-2 cm superior to the previous opening to extract the catheter and left the deep cuff beneath the sheath (Figure 1, right). A subcutaneous tunnel was created similarly in both groups to exit the site and orient the catheter downward.
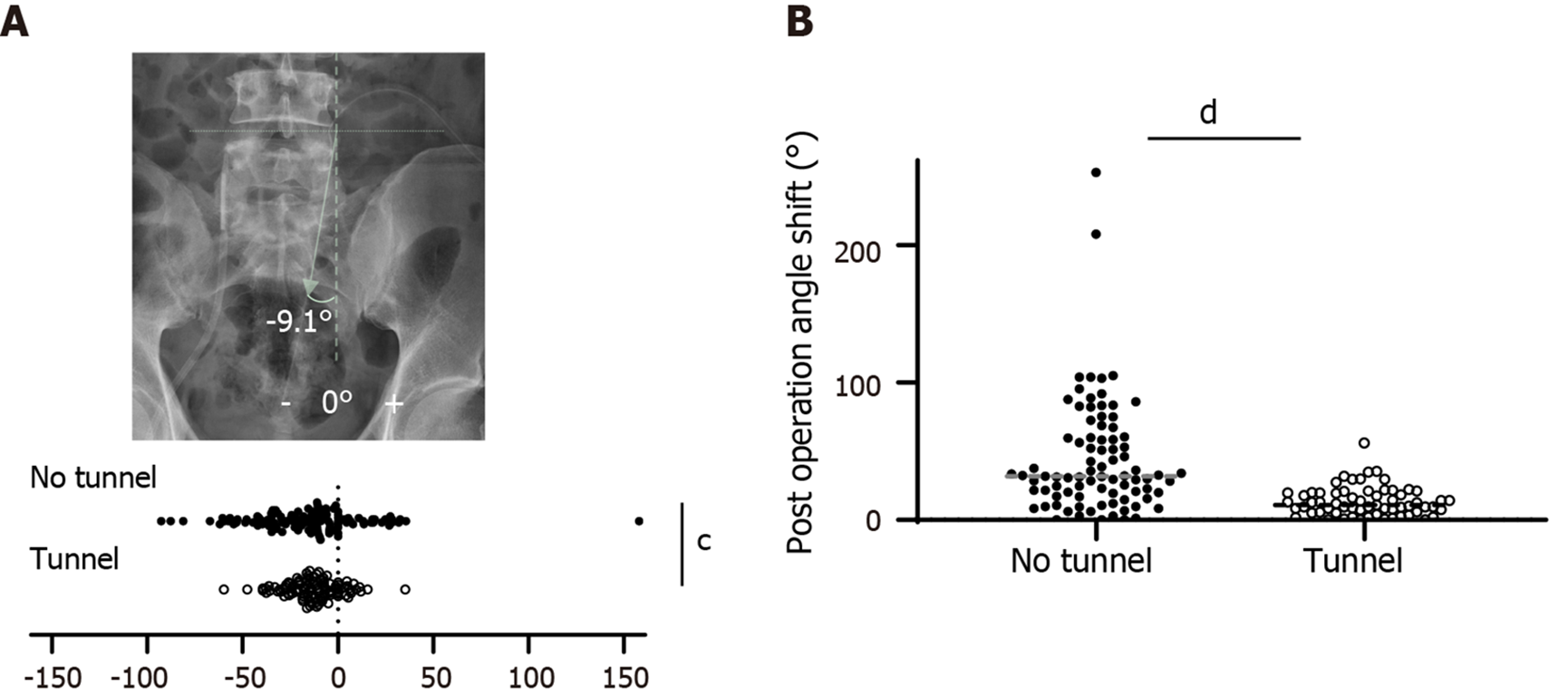
Postoperative plain film radiographs were reviewed to determine the angle of the catheter (Figure 2A). The catheter was placed into the pelvis perpendicularly during the procedure (ideal angle 0º). The angle of the catheter was calculated based on the axis of the catheter 5 cm below the deep cuff. All patients underwent radiography on the same day of the operation. We also reviewed all available radiographs taken within 2 years following the implantation. All angles of the catheter direction were recorded. The maximal migration angle was defined as the maximal disparity between any two measurements within the 2 years.
Overall catheter survival was determined at the time when patients discontinued PD for any reason. Therefore, patients were included if catheter function remained normal, but PD was ceased due to factors not attributed to the catheter itself, such as death, transplantation, personal choice, inguinal hernia, or subsequent abdominal surgery. The data of patients included in this category were censored.
Continuous variables are presented as mean ± SD. A two-sample t-test with Welch’s correction was used to compare nominal data sets. Data proportions were compared using Fisher’s exact test. Two-sided P values < 0.05 were considered statistically significant. We presented the data using Kaplan-Meier curves for the overall and functional catheter survival rates and analyzed them using a log-rank test. Statistical analysis was performed using the software GraphPad Prism 9.1.0 (GraphPad Software, LLC, CA, United States).
This study included 222 patients who underwent PD catheter implantation from 2015 to 2019. Among these patients, 115 underwent the procedure without a musculofascial tunnel before July 2017, and 107 underwent the modified procedure with a tunnel starting from August 2017. There was no difference in age, sex ratio, or primary renal disease incidence between the no-tunnel and tunnel groups (Table 1). In addition, no differences in body mass index or abdominal surgery history were observed between the two groups.
| No-tunnel (n = 115) | Tunnel (n = 107) | P value | |
| Age (yr, mean ± SD) | 57.03 ± 17.88 | 58.49 ± 16.38 | 0.4093 |
| Male, n (%) | 64 (55.65) | 67 (62.62) | 0.3395 |
| BMI (kg/m2, mean ± SD) | 23.85 ± 4.27 | 24.16 ± 4.07 | 0.5884 |
| Cause of ESRD, n (%) | 0.1434 | ||
| GN | 26 (22.61) | 23 (21.50) | |
| Polycystic kidney | 2 (1.74) | 5 (4.67) | |
| Diabetes mellitus | 17 (14.78) | 26 (24.30) | |
| Others | 70 (60.87) | 53 (49.52) | |
| History of abdominal surgery, n (%) | 22 (19.13) | 18 (16.82) | 0.7279 |
The absolute value of the catheter angle was significantly smaller in the tunnel group than in the no-tunnel group (15.51 ± 11.30 vs 25.00 ± 23.08º, P = 0.0002). Moreover, there were fewer cases of catheter migration greater than 45 in the tunnel group than in the no-tunnel group (1.87% vs 13.04%, P = 0.0018).
All patients had at least one radiograph taken in the two-year period following catheter placement. Patients who underwent catheter placement with an associated musculofascial tunnel displayed a significantly lower shift in the catheter angle than the patients who underwent catheter placement without a tunnel (Figure 2B, 13.48 ± 10.71 vs 44.34 ± 41.29º, P < 0.0001), implying that the catheter tip remained more stable in the pelvic cavity when the musculofascial tunnel was created.
Dysfunction of the catheter due to migration was observed in four patients over the two-year follow-up period, and all affected patients were in the no-tunnel group. In addition, both groups had two cases of catheter obstruction due to omental wrapping. PD was resumed successfully in all four patients following laparoscopic omentectomy.
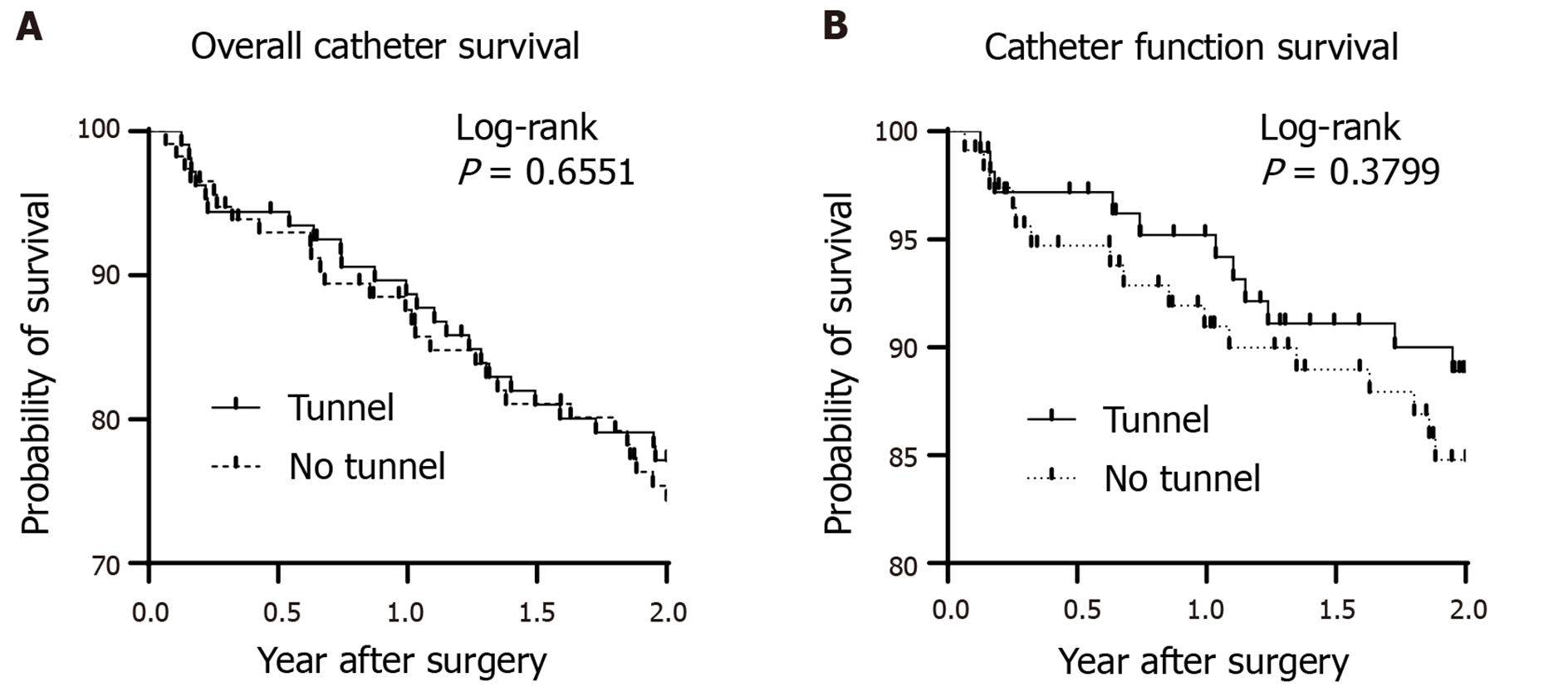
At the end of the two-year follow-up period, more than 70% of patients in both groups continued PD (Figure 3). The most common reasons for discontinuation were peritonitis and death (Table 2). After censoring the causes of discontinuation that were not attributed to the catheter (mentioned above), we performed a “function” survival analysis of the catheter, which revealed a two-year survival rate of 88.90% and 84.79% in the tunnel and no-tunnel groups, respectively. Although the survival curve seemed superior in the tunnel group, the difference was not statistically significant (P = 0.3799).
| No-tunnel (n = 115), n (%) | Tunnel (n = 107), n (%) | P value | |
| Low efficiency | 4 (3.48) | 2 (1.87) | 0.6845 |
| Peritonitis | 11 (9.57) | 6 (5.61) | 0.3186 |
| Abdominal wall leak | 1 (0.87) | (0.93) | > 0.9999 |
| Abdominal surgery | 1 (0.87) | 0 (0.00) | > 0.9999 |
| Inguinal hernia | 0 (0.00) | 2 (1.87) | 0.2312 |
| Personal choice | 2 (1.74) | 0 (0.00) | 0.4984 |
| Transplantation | 4 (3.48) | 2 (2.80) | > 0.9999 |
| Death | 4 (3.48) | 10 (9.35) | 0.0975 |
Catheter migration is a common complication following catheter implantation, with a reported incidence of 10%-30%[6,7]. This retrospective study demonstrated that PD catheter orientation was improved by creating a short musculofascial tunnel. Further, this tunnel helped maintain catheter position within the pelvis of all patients throughout a two-year follow-up period. In contrast, four patients in the no-tunnel group (3.4%) experienced catheter dysfunction due to migration.
Various current modifications for open surgery[4,5] involve performing additional incisions or sutures to extend the catheter route, reducing malfunction episodes, and prolonging catheter survival. However, our musculofascial tunnel modification required only a brief extension of surgical time and did not necessitate a significant procedure alteration. In addition, according to our experience, there is no need to make a long skin incision for the tunnel.
Laparoscopic surgery is also a practical method for rectus sheath tunneling or pre-peritoneal tunneling[8] to prevent catheter migration. However, general anesthesia with a muscle relaxant is necessary for laparoscopy, increasing anesthesia-related risk and prolonging perioperative preparation. Moreover, laparoscopic surgery is associated with additional costs for anesthesia and surgical instruments.
We suggest placing the catheter approximately 1.5 cm outside the purse-string suture of the peritoneum with the inner cuff just beneath the anterior fascia. This placement allows the catheter to be well fixed away from the peritoneum, thus preventing possible peritonitis induced by a tissue reaction around the deep cuff[9]. In addition, when discontinuing the use of the catheter, it is easier to remove the inner cuff in the presence of a musculofascial tunnel because the cuff lies superior to the rectus abdominis. On the contrary, the inner cuff is buried deeply in the rectus abdominis near the peritoneum in the no-tunnel method. Thus, increasing the risk of injuring the peritoneum and intestines during removal of the cuff due to extensive dissection.
This study had several limitations. First, this was a retrospective study conducted in a single center. As patients underwent different procedures in two separate periods, bias in patient selection and care was inevitable. However, we compared the patient characteristics between the two groups, and there were no significant differences in terms of kidney disease status and factors related to surgical concerns. In addition, all operations were performed by the same surgical team (Lee CY and Chen CC). Therefore, perioperative preparation and surgical materials remained unchanged throughout the study; thus, we believe that bias was minimal although present. Second, the patients in the study had an average body mass index of 24 kg/m2, which is similar to that of most Asians but lower than those of Europeans and Americans[10]. The thickness of subcutaneous adipose tissue is critical for determining incision length, and deep subcutaneous adipose tissue may result in technical difficulty during open surgery. Further investigation involving patients with a high body mass index is needed in the future.
The results from this study provide evidence supporting the ISPD guideline for improving the quality of PD care. However, the addition of a short musculofascial tunnel, a simple but usually neglected step in catheter implantation, helped tilt the catheter and orient it downward toward the pelvis, which reduced catheter migration and prevented catheter dysfunction. This preemptive modification does not require specialized training, and therefore, can be readily adopted by surgical teams.
Creation of a musculofascial tunnel is usually neglected in the procedure of peritoneal dialysis catheter implantation.
We would like to see if the tunnel reduces catheter migration.
Patients undergoing peritoneal dialysis implantation with or without a musculofascial tunnel were retrospectively reviewed.
Plain film after catheter implantation were reviewed to compare the migration angle.
Patients with the musculofascial tunnel had lower migration rate.
Creating of a musculofascial tunnel is an important step for reducing catheter migration.
Long term follow up is need for the function survival benefit.
The authors would like to acknowledge the peritoneal dialysis team for providing clinical support with the surgical procedures. In addition, we thank Mr. Shi-Yi Yang for his assistance with the statistics used in this report.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Wankowicz Z, Zhu C S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | Crabtree JH, Shrestha BM, Chow KM, Figueiredo AE, Povlsen JV, Wilkie M, Abdel-Aal A, Cullis B, Goh BL, Briggs VR, Brown EA, Dor FJMF. Creating and Maintaining Optimal Peritoneal Dialysis Access in the Adult Patient: 2019 Update. Perit Dial Int. 2019;39:414-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 201] [Article Influence: 33.5] [Reference Citation Analysis (0)] |
| 2. | Helfrich GB, Winchester JF. Questions, Answers. Perit Dial Int. 1981;2:132-133. [RCA] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 3. | Peppelenbosch A, van Kuijk WH, Bouvy ND, van der Sande FM, Tordoir JH. Peritoneal dialysis catheter placement technique and complications. NDT Plus. 2008;1:iv23-iv28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 4. | Jiang C, Xu L, Chen Y, Yan X, Sun C, Zhang M. A modified open surgery technique for peritoneal dialysis catheter placement decreases catheter malfunction. Perit Dial Int. 2014;34:358-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 5. | Li Y, Zhu Y, Liang Z, Zheng X, Zhang H, Zhu W. A simple modified open peritoneal dialysis catheter insertion procedure reduces the need for secondary surgery. Int Urol Nephrol. 2019;51:729-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Ma Y, Liu S, Yang M, Zou Y, Xue D, Liu Y, Wang Y, Xie X, Chen H. Association between different peritoneal dialysis catheter placement methods and short-term postoperative complications. BMC Nephrol. 2021;22:151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Esagian SM, Sideris GA, Bishawi M, Ziogas IA, Lehrich RW, Middleton JP, Suhocki PV, Pappas TN, Economopoulos KP. Surgical vs percutaneous catheter placement for peritoneal dialysis: an updated systematic review and meta-analysis. J Nephrol. 2021;34:1681-1696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 8. | Modaghegh MH, Kazemzadeh G, Rajabnejad Y, Nazemian F. Preperitoneal tunneling-a novel technique in peritoneal dialysis catheter insertion. Perit Dial Int. 2014;34:443-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Dimitriadis A, Antoniou S, Toliou T, Papadopoulos C. Tissue reaction to deep cuff of Tenckhoff's catheter and peritonitis. Adv Perit Dial. 1990;6:155-158. [PubMed] |
| 10. | WHO. Global status report on noncommunicable diseases 2014. Available from: http://www.who.int/nmh/publications/ncd-status-report-2014/en/. |