Published online Dec 26, 2022. doi: 10.12998/wjcc.v10.i36.13458
Peer-review started: October 17, 2022
First decision: October 27, 2022
Revised: November 5, 2022
Accepted: November 22, 2022
Article in press: November 22, 2022
Published online: December 26, 2022
Processing time: 70 Days and 8.1 Hours
Hoffa's fracture is a coronal-oriented fracture of the femoral condyle. It is rarely observed in pediatric patients that isolated coronal fracture of the medial femoral condyle accompanies an intact lateral femoral condyle. Only a few cases involving Hoffa's fracture of the medial femoral condyle have been reported in patients with undeveloped skeletons. Such a fracture cannot be observed by routine imaging examinations, thus resulting in possible misdiagnosis and further treatment challenges.
A 5-year-old boy with Hoffa's fracture of the medial femoral condyle suffered from right knee pain and severe swelling after being hit by a heavy object. The patient was misdiagnosed and initially treated in a local primary healthcare center. No improvement in his right knee’s extension was observed following conservative treatment for 2 wk. The patient was transferred to our hospital, re-diagnosed using arthroscopy, and underwent open reduction and internal fixation. The therapeutic outcome was satisfactory with the screws removed 7 mo after fixation. At the final follow-up of 40 mo, the range of motion in the knee had recovered. There was no varus-valgus instability.
Hoffa's fracture is rarely seen in children aged 5 years, let alone in the medial condyle, and can easily be misdiagnosed due to limited physical and imaging examinations. Suspected Hoffa's fracture in preschool children should be confirmed based on arthroscopic findings. Open reduction and internal fixation should be performed to protect the articular surface and prevent long-term complications.
Core Tip: Hoffa’s fracture is a rare fracture pattern of femoral condyle, it has special coronal fracture slice. When it happens in children, this fracture is very easy to be missed. The medial condyle Hoffa’s fractures are especially uncommon. We report Hoffa’s fracture of the medial condyle in a 5-year-old child, the youngest patient ever reported, who was misdiagnosed in the first place. Eventually, we diagnosed the disease with arthroscopy and completed the operation with its assistance, successfully avoiding the radiation damage caused by computed tomography scans to toddler. Meanwhile, a clear and concise review of literature is also included in our study.
- Citation: Chen ZH, Wang HF, Wang HY, Li F, Bai XF, Ni JL, Shi ZB. Hoffa's fracture in a five-year-old child diagnosed and treated with the assistance of arthroscopy: A case report. World J Clin Cases 2022; 10(36): 13458-13466
- URL: https://www.wjgnet.com/2307-8960/full/v10/i36/13458.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i36.13458
Hoffa's fracture, named after Albert Hoffa in 1904 following his detailed research on this disease[1], is an unusual fracture type on the coronal plane of the femoral condyle. Hoffa's fractures of the lateral femoral condyle are commonly seen, while Hoffa's fractures of the medial femoral condyle are rare, especially in individuals with undeveloped skeletons. The latest case was a 16-year-old girl with Hoffa's fracture of the medial femoral condyle reported by Jiang et al[2] in 2022. This type of fracture is an intra-articular fracture and is clinically treated under the same principles as a typical intra-articular fracture. But this type of injury is often misdiagnosed due to a lack of clinical suspicion and radiographic examinations. In this report, we present the case of a 5-year-old boy with unusual type of injury misdiagnosed in a local hospital. Arthroscopy was performed to confirm the medial Hoffa's fracture. Later, open reduction and internal fixation were successfully applied to the patient for treatment.
A 5-year-old boy was transferred to the Department of Orthopedics in our hospital due to right knee pain and swelling, and an inability to bear weight and extend the right knee.
The patient had right knee pain and an inability to extend the knee following 2 weeks of conservative treatment.
The boy had no history of severe diseases, surgery or long-term medication.
The patient’s family had no related diseases.
His right knee was swollen, skin was intact with tenderness on palpation, and limited mobility. No distal neurovascular deficits were observed. He was alert, articulate, and a reliable reporter. No other weakness, stiffness, or edema was found.
Results of laboratory examinations were unremarkable.
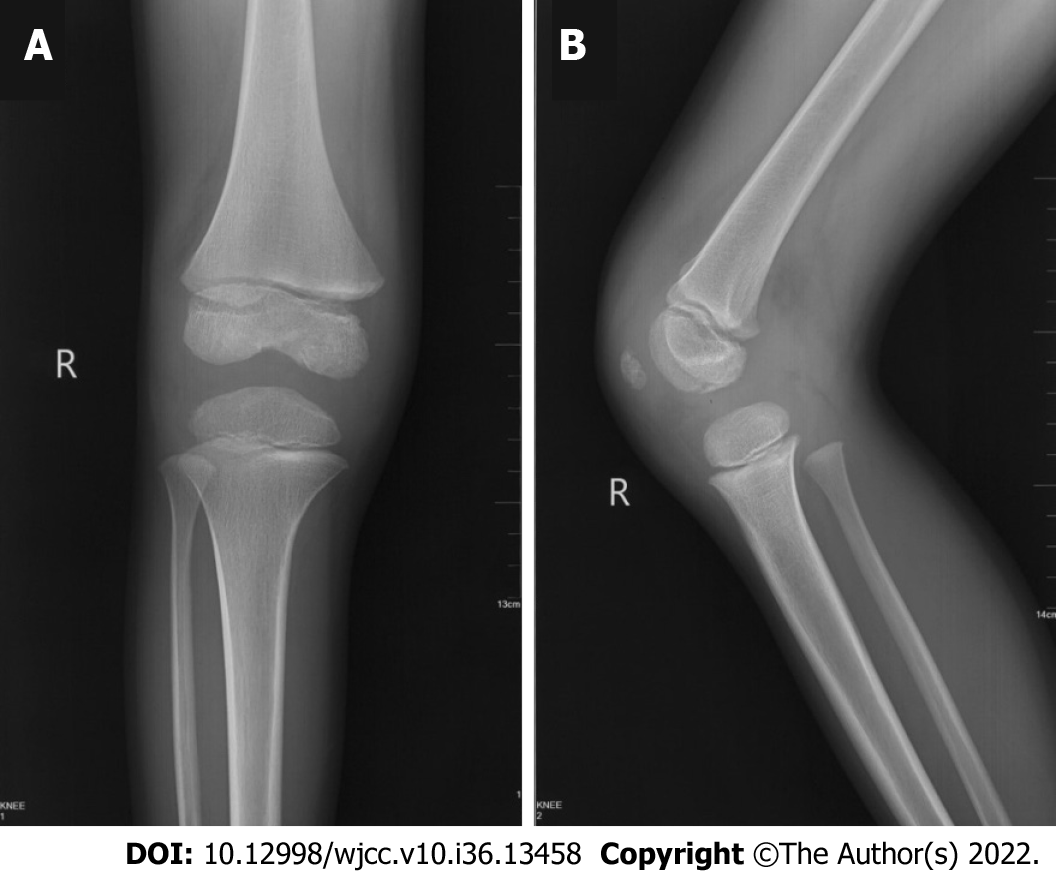
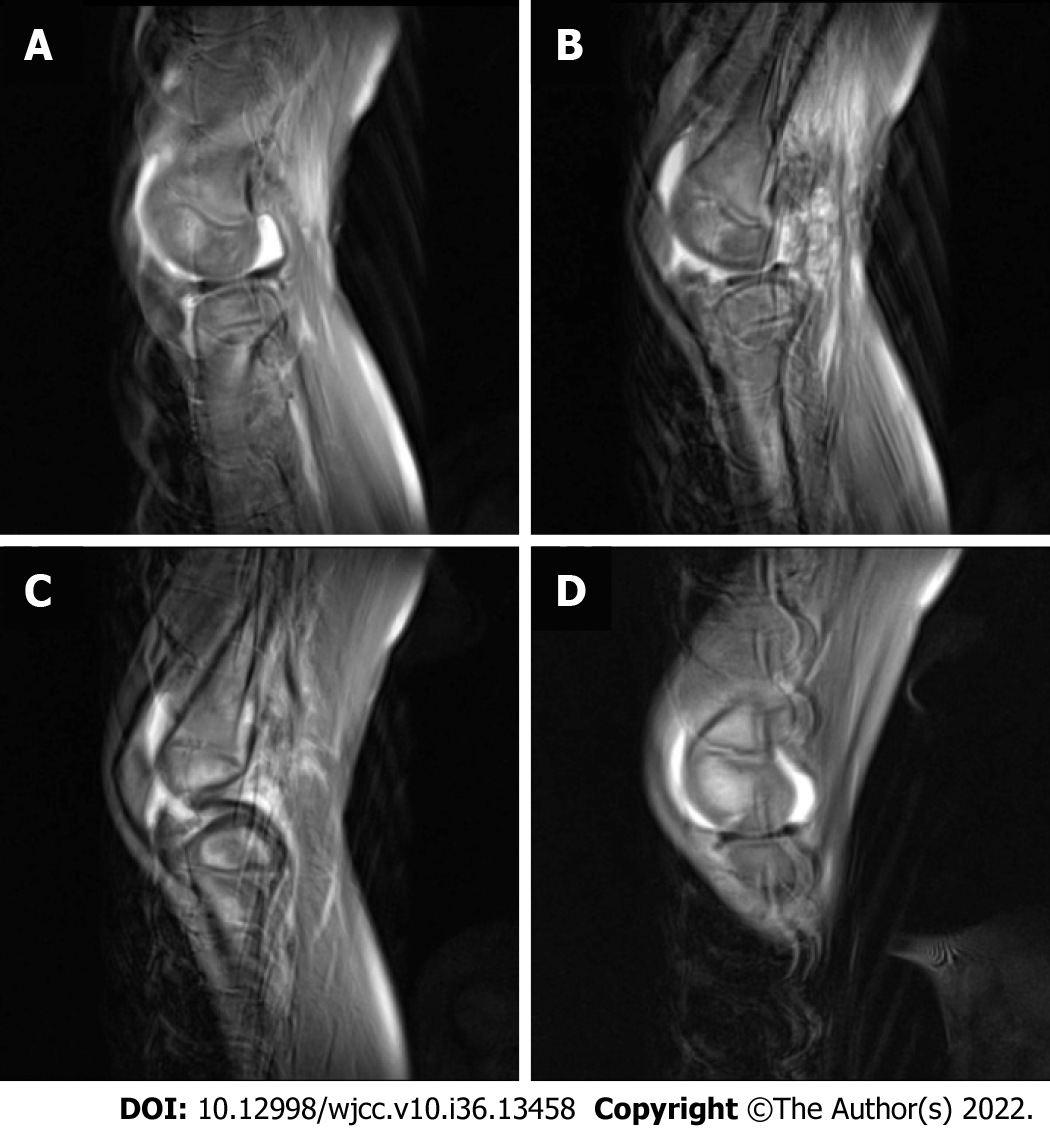
X-Ray showed a stable fracture in the medial femoral condyle with no displacement (Figure 1). A local orthopedist suggested conservative treatment. Computed tomography (CT) is considered efficient in the diagnosis of adult Hoffa's fracture. However, in this case, the thick cartilage of the distal femoral epiphyseal area made it difficult to evaluate the fracture[1,3,4]. The area of high signal on magnetic resonance imaging (MRI) also indicated no severe displacement (Figure 2).
Arthroscopy was performed to confirm the diagnosis. Different from the findings on the imaging examinations, obvious fracture displacement of the cartilage was found (Figure 3).
Hoffa's fracture of the medial femoral condyle.
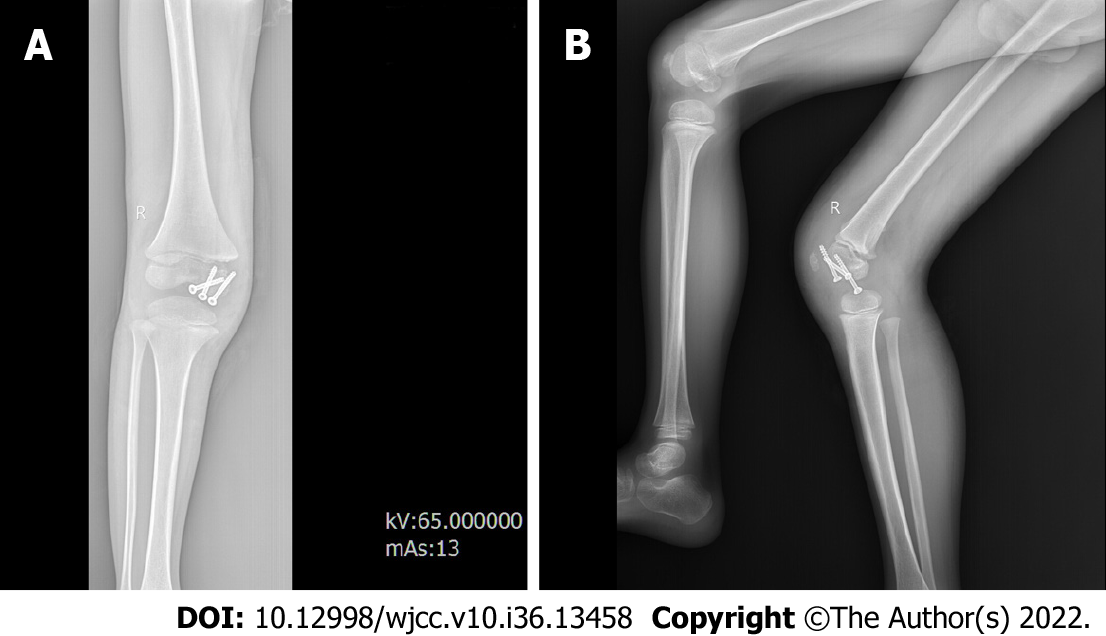
Arthroscopic exploration and diagnosis were performed at the beginning of the operation. The presence of steps and micromovement at the fracture ends could be seen during arthroscopy. However, due to instability of the bone mass caused by the now old injury (more than 2 wk), it was difficult to achieve a satisfactory reduction via arthroscopy. Therefore, open reduction was scheduled (Figure 4). Two 3.0 mm partially-threaded cancellous screws placed perpendicular to the fracture line were used to reduce the fracture. To avoid epiphyseal injury, a screw of appropriate length was placed through the metaphysis. Countersunk screws were also placed through the articular cartilage.
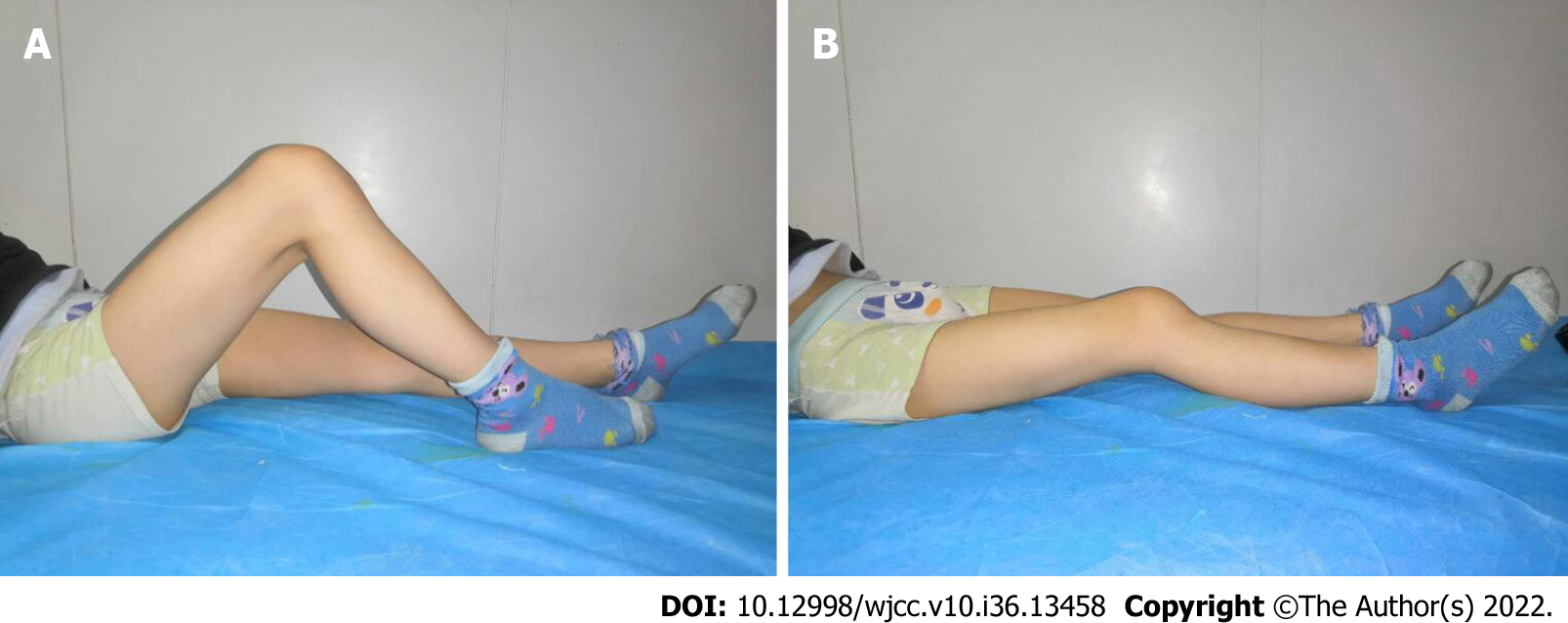
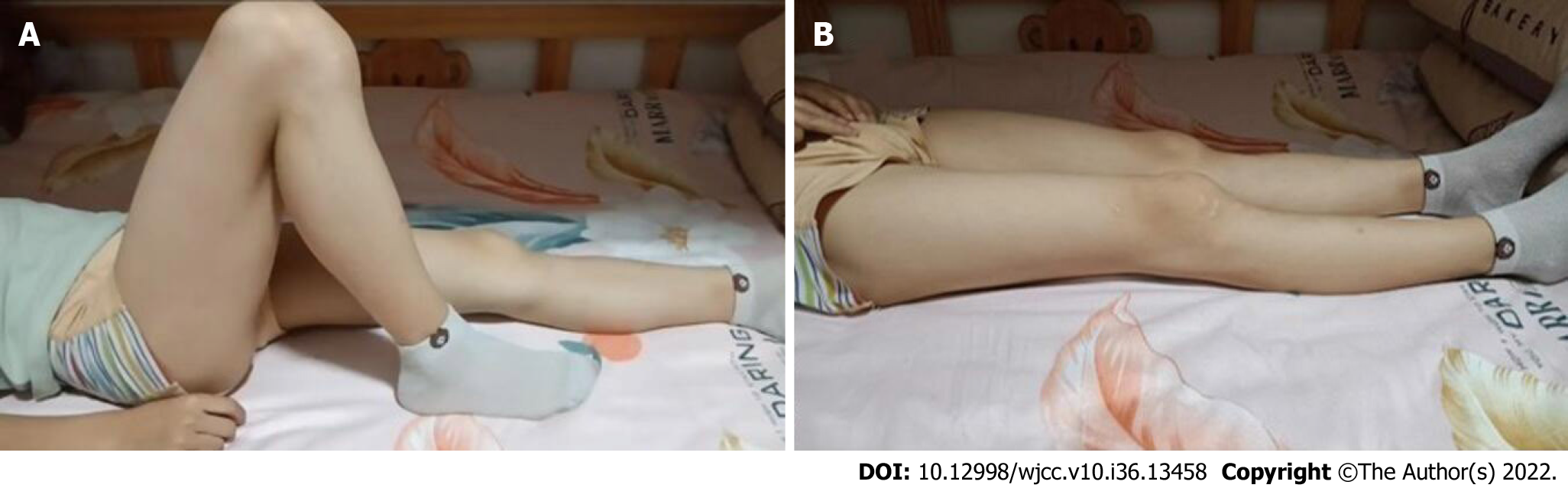
Following open reduction and internal fixation, the patient wore a knee brace with 30° of knee flexion for approximately 2 wk. Afterwards, gradually begin to work on the range of motion of the knee. The patient was strictly instructed to avoid any weight-bearing bending until the sixth week, in order to minimize the shear force on his coronation. Partial weight-bearing began after the sixth week, then progressing to full weight-bearing (FWB) by the tenth week. At the six-month follow-up, he could walk without support. The knee range of motion was 5° to 100° (Figure 5). No angular deformity or limb-length discrepancy was observed. X-ray showed that the fracture healed well and there was no sign of femoral condyle collapse (Figure 6). The screws were removed after 7 mo. At the final follow-up of 40 mo, the KSS score was 100. The patient had full range of motion, with no varus-valgus instability (Figure 7).
Coronal plane fracture of the femoral condyle was named after Hoffa following his detailed research on this fracture in 1904[3]. Letenneur et al[5] classified this fracture into three different types. Accordingly, our patient developed a Type III fracture. This rare injury can also be classified into a medial, lateral and conjoint Hoffa's fracture based on the location of the fracture[6]. According to a review of the literature on Hoffa’s fracture in the pediatric population (Table 1), 16 cases of Hoffa’s fracture in pediatric patients were reported. Only 5 were located on the medial femoral condyle. Bali et al[7] first described an isolated Hoffa's fracture of the medial condyle in a patient with an undeveloped skeleton. Ranjan et al[6] described a Hoffa’s fracture of the medial condyle in a 6-year-old girl. To date, only four cases of Hoffa’s fracture of the medial condyle in pediatric patients has been reported. We aimed to report the fifth case in a 5-year-old patient, the youngest ever diagnosed.
| No. | Ref. | Sex | Age (yr) | Injury | Diagnostic tool | Location of fracture | Approach | Outcome |
| 1 | Agrawal et al[8], 2021 | M | 18 | Road side accident | X-ray, CT | Conjoint | Medial parapetallar approach, with 2 (6.5 mm) PTCS in 1 condyle and one 6.5 and 4.5 mm PTCS in another condyle | 0°-130° ROM |
| 2 | Kondreddi et al[9], 2014 | - | 17 | Road traffic accident | X-ray | Lateral parapatellar arthrotomy, with four 4-mm cancellous screws (2 for each condyle) introduced antero-posteriorly through the non-articular surface, in a di-rection perpendicular to the fracture line | 120° ROM | |
| 3 | Julfiqar et al[20], 2019 | M | 12 | Fall from height when his left knee was in the flexed position | X-ray | Open reduction and intraepiphyseal internal fixation using a 4.5 mm cannulated cancellous screw | 0°-120° ROM | |
| 4 | Chaudhary et al[12], 2020 | M | 11 | Fall from a tree | X-ray | Open reduction and internal fixation using the Swashbuckler approach, lag screw technique with two 4 mm cancellous screws placed antero-posteriorly in the lateral condyle and one antero-posterior 4 mm cancellous screw and one Herbert screw placed postero-anteriorly in the medial condyle | 0°-120° ROM | |
| 5 | Lal et al[15], 2011 | - | 9 | Fall from height | X-ray | Arthroscopy assisted internal fixation, with 4.5-mm cannulated cancellous screws, inserted from anterior to posterior just distal to the femoral physis | Cure | |
| 6 | Harna et al[22], 2017 | M | 7 | Hit by a speeding motor vehicle | CT | Swashbuckler approach, with 2.9 mm Herbert screws for compression | 0°-130° ROM | |
| 7 | Kumar et al[13], 2001 | F | 17 | Fall from ladder | X-ray | Lateral femoral condyle | Reduction and fixation with two antero-posterior lag screws | Full ROM |
| 8 | Flanagin et al[10], 2011 | M | 14 | Wrestling | Arthroscopy | Headless compression screws | Full ROM | |
| 9 | Potini et al[14], 2015 | M | 14 | Direct blow over knee | X-ray | Open reduction and rigid fixation with countersunk interfragmentary screws | 5°–110° ROM | |
| 10 | Tripathy et al[19], 2013 | M | 12 | Fall while playing | CT | Open reduction and fixation with two partially threaded cancellous lag screws | Cure | |
| 11 | Ashraf[16], 2019 | M | 12 | Motor vehicle accident | X-ray, CT | Evaluation of the cruciateligaments and antero-posterior stability with arthroscopy, open reduction and internal fixation using two cannulated screws | Full ROM | |
| 12 | McDonough et al[11], 2000 | M | 8 | Road traffic accident | X-ray | Open reduction and internal fixation using two partially threaded cancellous lag screws | Full ROM | |
| 13 | Jiang et al[2], 2022 | F | 16 | Knee injury in a sprint race | X-ray, CT | Medial femoral condyle | Open reduction and fixation using three 3.5 mm partially threaded cancellous screws | 0°-135° ROM |
| 14 | AlKhalife et al[3], 2018 | M | 12 | Object dropped | CT | Open reduction and internal fixation through a medial parapatellar approach with the aid of a bone clamp and two 4.0 mm partially threaded cancellous screws, the screw heads placed through the articular cartilage were countersunk | 15°–130° ROM | |
| 15 | Bali et al[7], 2011 | M | 12 | Traffic accident | CT | Open reduction and internal fixation with two large-fragment cannulated screws, which were buried under the articular surface of the knee | Cure | |
| 16 | Ranjan et al[6], 2021 | F | 6 | Fall | CT | Open reduction and fixation through the medial approach with two 4.5 mm partially threaded cannulated cancellous screws | 0°–110° ROM | |
| 17 | Current Study, 2022 | M | 5 | Hit by object | Arthroscopy | Open reduction and internal fixation through the medial parapatellar approach, using two 3.0 mm partially threaded cancellous screws | Full ROM |
Hoffa’s fractures are mostly triggered by high-energy damage[8,9], and are more commonly seen in young adults. This injury is mainly caused by axial shear force affecting the posterior part of the femoral condyle when the knee is flexed[6]. Due to the anatomical features of the ectropion angle at the distal femur, when high-energy violence acts on the distal femur, it often acts firstly on the lateral condyle. As a result, lateral condyle fractures are more common than medial condyle fractures. Commonly, the cause of Hoffa's fractures in adults is vehicle accidents[7] while in pediatric Hoffa's fracture are usually caused by trivial injury or sports injury[10]. In this case, the injury was caused by a heavy object falling on the right knee. Since only a few cases have been reported, little is known about Hoffa's fractures in children, and McDonough et al[11] reported the first case of a non-healing Hoffa's fracture in an eight-year-old boy. According to our research (Table 1), X-ray is the most effective diagnostic tool for confirming pediatric Hoffa’s fracture, followed by CT[12-14]. However, as the fracture is barely visible on routine anteroposterior radiographs, misdiagnosis often occurs even in the lateral view. The fracture can be obscured by the intact anterior condyle in the anterior and posterior projections, if it is minimally displaced[15-17]. Therefore, it is wiser to carry out the gold standard investigation, which is CT[18]. However, in pediatric patients, the fracture line can be easily ignored, even on CT and MRI due to thick cartilage. In young patients, the diagnosis of Hoffa’s fracture is often omitted based on past clinical experience. Three cases of misdiagnosed Hoffa’s fracture in eight-year-old and two twelve-year-old boys were identified in previous literature, which were fixed with cannulated screws and successfully treated[11,16,19]. In this study, we report another case of nonunion of Hoffa’s fracture in the medial condyle in a five-year-old boy who was initially misdiagnosed as having a stable fracture with no displacement. The patient was finally diagnosed with Hoffa’s fracture by arthroscopy. Therefore, it is noteworthy that arthroscopy is critical in the diagnosis of pediatric Hoffa’s fracture with inconclusive radiographs[10]. In our case, a CT scan was not performed on the injured knee due to difficulty in evaluating the fracture, thick cartilage of the distal femoral epiphysis and the patient’s immature skeleton[1,3,4]. Avoiding CT exams can also prevent greater radiation exposure during CT scans than X-rays[20].
Conservative treatment of these fractures is unsatisfactory as the reduction in fracture fragments is difficult to achieve and to maintain by closure. This may lead to multiple complications such as avascular necrosis, nonunion, and malunion[4,15,21]. Therefore, as the ideal treatment[19], surgical stabilization and internal fixation are required to achieve a satisfactory clinical outcome. There is also controversy regarding the surgical approaches for pediatric Hoffa’s fracture. The approaches described in previous literature include the lateral, medial and Swashbuckler approach (Table 1). It is generally accepted that surgical stabilization is necessary for a satisfactory clinical outcome after the treatment of Hoffa’s fracture. The reason for this is that, closure reduction and cast/traction techniques are difficult to achieve and sustain the reduction of fracture fragments without soft tissue attachment. Therefore, this kind of injury is also prone to vascular necrosis and bone nonunion, which should be prevented by stable anatomical compression reduction and internal fixation. This can only be achieved by open/arthroscopic approaches[15]. In our case, we performed open reduction and internal fixation with the assistance of arthroscopy using a medial parapatellar approach. The outcome was satisfactory. The advantages of the guidance of arthroscopy include avoidance of soft tissue, decreased blood loss, and intraarticular visualization. Acute Hoffa’s fracture with minimal communition and large fragments can also get benefit from arthroscopic fixation[21,22].
We report Hoffa’s fracture of the medial condyle in a 5-year-old child, the youngest patient ever reported, who was diagnosed and treated with the assistance of arthroscopy. We maintain that this rare fracture can be misdiagnosed easily. Healthcare practitioners should note of this when dealing with children’s knee fractures. It is better to diagnose this fracture by arthroscopy in patients with skeletal immaturity. Treatment of this fracture with open reduction and internal fixation can prevent further long-term complications. However, arthroscopy-guided reduction and internal fixation may be a good option for patients who have a fresh fracture.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anatomy and morphology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hakimi T, Afghanistan; Paparoupa M, Germany S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Hoffa A. Lehrbuch der Frakturen und Luxationen. Stuttgart: Verlagvon Ferdinand Enke. 1904; 451. Available from: https://www.abebooks.fr/Lehrbuch-Frakturen-Luxationen-Hoffa-Albert/30696933697/bd. |
| 2. | Jiang ZX, Wang P, Ye SX, Xie XP, Wang CX, Wang Y. Hoffa's fracture in an adolescent treated with an innovative surgical procedure: A case report. World J Clin Cases. 2022;10:1410-1416. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | AlKhalife YI, Alshammari AN, Abouelnaga MA. Hoffa's fracture of the medial femoral condyle in a child treated with open reduction and internal fixation: A case report. Trauma Case Rep. 2018;14:20-26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Lewis SL, Pozo JL, Muirhead-Allwood WF. Coronal fractures of the lateral femoral condyle. J Bone Joint Surg Br. 1989;71:118-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 107] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Letenneur J, Labour PE, Rogez JM, Lignon J, Bainvel JV. [Hoffa's fractures. Report of 20 cases (author's transl)]. Ann Chir. 1978;32:213-219. [PubMed] |
| 6. | Ranjan R, Kumar R, Jeyaraman M, Jain R, Chaudhary D, Kumar S. Hoffa Fracture in Skeletally Immature Patients: A Case Report and Review of Literature. J Orthop Case Rep. 2021;11:112-118. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 7. | Bali K, Mootha AK, Prabhakar S, Dhillon MS. Isolated Hoffa fracture of the medial femoral condyle in a skeletally immature patient. Bull NYU Hosp Jt Dis. 2011;69:335-338. [PubMed] |
| 8. | Agrawal P, Kumar A, Teja KVC, Razek MRA. A Case Report of Adolescent Bicondylar Conjoint Hoffa Fracture with Patellar Fracture and Dislocation: A Rare Combination. J Orthop Case Rep. 2021;11:57-61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | Kondreddi V, Yalamanchili RK, Ravi Kiran K. Bicondylar Hoffa's fracture with patellar dislocation - a rare case. J Clin Orthop Trauma. 2014;5:38-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Flanagin BA, Cruz AI, Medvecky MJ. Hoffa fracture in a 14-year-old. Orthopedics. 2011;34:138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | McDonough PW, Bernstein RM. Nonunion of a Hoffa fracture in a child. J Orthop Trauma. 2000;14:519-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Chaudhary SD, Raghuwanshi SR. Complex Variant of Paediatric Conjoint Bicondylar Hoffa Fracture: A Rare Entity. Indian J Orthop. 2020;54:408-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Kumar R, Malhotra R. The Hoffa fracture: Three case reports. J Orthop Surg (Hong Kong). 2001;9:47-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 35] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Potini VC, Gehrmann RM. Intra-Articular Dislocation of the Patella With Associated Hoffa Fracture in a Skeletally Immature Patient. Am J Orthop (Belle Mead NJ). 2015;44:E195-E198. [PubMed] |
| 15. | Lal H, Bansal P, Khare R, Mittal D. Conjoint bicondylar Hoffa fracture in a child: a rare variant treated by minimally invasive approach. J Orthop Traumatol. 2011;12:111-114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Ashraf E. Missed Hoffa Fracture in Skeletally Immature Patient Complicated by Non-union Pseudoarthrosis: Case Report and Review of Literature. Ortho & Rheum Open Access J. 2019;15:555916. [DOI] [Full Text] |
| 17. | Allmann KH, Altehoefer C, Wildanger G, Gufler H, Uhl M, Seif el Nasr M, Langer M. Hoffa fracture--a radiologic diagnostic approach. J Belge Radiol. 1996;79:201-202. [PubMed] |
| 18. | Dhillon MS, Mootha AK, Bali K, Prabhakar S, Dhatt SS, Kumar V. Coronal fractures of the medial femoral condyle: a series of 6 cases and review of literature. Musculoskelet Surg. 2012;96:49-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 19. | Tripathy SK, Aggarwal A, Patel S, Goyal T, Priya N. Neglected Hoffa fracture in a child. J Pediatr Orthop B. 2013;22:339-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Julfiqar, Huda N, Pant A. Paediatric conjoint bicondylar Hoffa fracture with patellar tendon injury: An unusual pattern of injury. Chin J Traumatol. 2019;22:246-248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Holmes SM, Bomback D, Baumgaertner MR. Coronal fractures of the femoral condyle: a brief report of five cases. J Orthop Trauma. 2004;18:316-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 67] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 22. | Harna B, Goel A, Singh P, Sabat D. Pediatric conjoint Hoffa's fracture: An uncommon injury and review of literature. J Clin Orthop Trauma. 2017;8:353-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |