Published online Dec 26, 2022. doi: 10.12998/wjcc.v10.i36.13435
Peer-review started: October 20, 2022
First decision: November 11, 2022
Revised: November 22, 2022
Accepted: December 5, 2022
Article in press: December 5, 2022
Published online: December 26, 2022
Processing time: 67 Days and 11.5 Hours
Aortic dissection is a complex and dangerous cardiovascular disease, with many complications in the perioperative period, including severe acute respiratory distress syndrome (ARDS), which affects prognosis and increases mortality. Despite the effect of prone positioning (PP) in improving oxygenation in patients with severe ARDS, reports about PP early after cardiac surgery are few and such an opt
A 40-year-old male patient diagnosed with acute type A aortic dissection on October 22, 2021 underwent ascending artery replacement plus total aortic arch replacement plus stent elephant trunk implantation under cardiopulmonary bypass. Unfortunately, he developed ARDS on postoperative day 1. Despite comprehensive treatment with aggressive pulmonary protective ventilation, fluid management with continuous renal replacement therapy, the condition continued to deteriorate and rapidly progressed to severe ARDS with a minimum oxy
Intermittent short-term PP can improve early postoperative severe ARDS after acute aortic dissection.
Core Tip: Severe acute respiratory distress syndrome (ARDS) is often secondary to cardiac macrovascular surgery. Extracorporeal membrane oxygenation (ECMO) and prone positioning (PP) can improve pulmonary ventilation blood flow ratio and survival rate. We report a case of aortic dissection complicated with severe ARDS, in which intermittent short-term PP successfully improved oxygenation in the absence of ECMO. It is not an absolute contraindication to prone ventilation in the early postoperative period after thoracotomy. The use of intermittent short-term PP can improve the condition and avoid the complications caused by early PP after thoracotomy.
- Citation: Yang JH, Wang S, Gan YX, Feng XY, Niu BL. Short-term prone positioning for severe acute respiratory distress syndrome after cardiopulmonary bypass: A case report and literature review. World J Clin Cases 2022; 10(36): 13435-13442
- URL: https://www.wjgnet.com/2307-8960/full/v10/i36/13435.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i36.13435
Aortic dissection is a complex and dangerous cardiovascular disease, with a high mortality rate, and surgical treatment is an effective way to save life[1-3]. Aortic dissection surgery is traumatic, requiring a long treatment time and deep hypothermia for circulatory arrest[1,2]. A large number of blood transfusions are often required, as well as ischemia-reperfusion due to extracorporeal circulation, so there are many postoperative complications, among which, the incidence of acute respiratory distress syndrome (ARDS) is high, especially in obese patients with acute renal impairment before surgery[1,2,4,5]. ARDS significantly increases postoperative mortality and prolongs ventilator use and intensive care unit (ICU) stay[3]. According to the Berlin definition, ARDS is characterized by acute onset with bilateral lung opacities not explained by cardiac failure and/or fluid overload (Table 1). Although extracorporeal membrane oxygenation (ECMO) and prone positioning (PP) are important parts in the comprehensive treatment plan of severe ARDS[6-10], ECMO can easily cause fatal bleeding in the case of abnormal coagulation. Standardized and timely PP can effectively improve oxygenation and respiratory mechanics, including increasing functional residual volume, reducing lung shunt, promoting pulmonary secretion discharge, and improving ventilation flow ratio[8,11-13], so as to reduce mortality rate[14]. Gu et al[15] used PP to treat severe hypoxemia after aortic dissection and achieved good results. Here, we report a case of successful improvement in oxygenation with postoperative severe ARDS with acute type A aortic dissection treated with PP.
| Diagnostic criteria[5] | Onset within 1 wk of known clinical impairment or new/worsening respiratory symptoms; Bilateral shadows (on CXR or CT scan) not fully explained by effusions, lobar/lung collapse, or nodules; Respiratory failure not entirely explained by heart failure or fluid overload | ||
| Oxygenation impairment[5] | Mild; 200 mmHg < PaO2/FiO2 ≤ 300 mmHg with PEEP or continuous positive airway pressure ≥ 5 cmH2O | Moderate 100 mmHg < PaO2/FiO2 ≤ 200 mmHg with PEEP ≥ 5 cmH2O | Severe PaO2/FiO2 ≤ 100 mmHg with PEEP ≥ 5 |
| Risk factors for ARDS[5,16,17] | Infectious risk factors: Pneumonia, nonpulmonary sepsis | Noninfectious: Aspiration of gastric contents, severe trauma, pulmonary contusion, noncardiogenic shock, inhalation injury, severe burns, pancreatitis, drug overdose, multiple transfusions or TRALI, pulmonary vasculitis, drowning | |
| Oxygen therapy | Intubation/mechanical ventilation (most patients)Noninvasive ventilation for mild ARDS | ||
| Fluid management | Aim for central venous pressure < 4 mmHg or PAOP < 8 mmHg to ↓ pulmonary; Oedema | ||
| Prone positioning | |||
| ECMO | |||
| Decreased oxygen consumption; Increased oxygen delivery[7] | Antipyretics, sedatives, analgesics and paralysis agents; Inotropics to ↑ filling pressure (if no pulmonary edema); Restrict transfusions to maintain hemoglobin to 7–9 g/dL; Inhaled vasodilators (NO, prostacyclin and prostaglandin E1) to ↑ V′/Q′ matching |
A 40-year-old middle-aged man was admitted to hospital with sudden chest and back pain for 5 h.
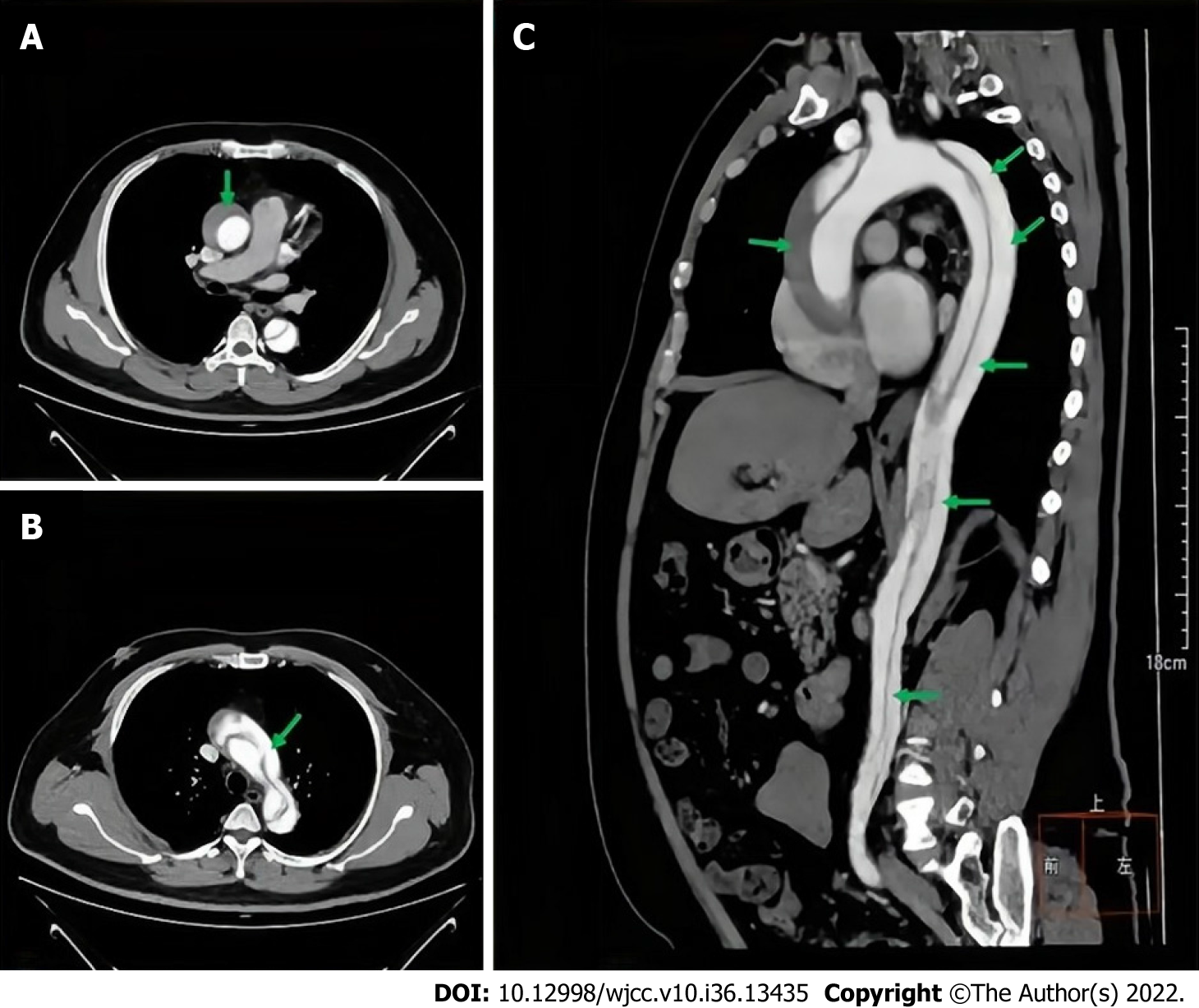
The patient suddenly developed severe chest and back pain 5 h ago. The tearing-like pain continued without relief. Computed tomography angiography (CTA) of the thoracic and abdominal aorta was performed in a large class III general hospital in Chongqing. The examination showed acute type A aortic dissection.
The patient did not have any other medical history other than hypertension.
The patient had a 20-year history of heavy smoking, two packs per day, with no specific family history.
Physical examination revealed persistent tearing pain in the chest and back.
Renal function test showed that creatinine rose to 237.6 mmol/L.
Thoracic and abdominal aorta CTA (Figure 1) showed aortic false lumen formation.
(1) Acute aortic dissection (Standford type A); (2) acute kidney injury (AKI) grade II; (3) coagulation dysfunction; (4) acute myocardial injury; (5) hypoproteinemia; and (6) high-risk stage 3 hypertension.
After preoperative examination, the patient underwent ascending aortic and total aortic arch replacement plus stented elephant trunk implantation under general anesthesia and cardiopulmonary bypass. He was transferred to the ICU in critical condition for continued treatment after surgery. During the operation and on the day of admission to ICU, 4 U of red blood cells, 850 mL of plasma, 20 U of cryoprecipitate, and 2 U of platelets were transfused.
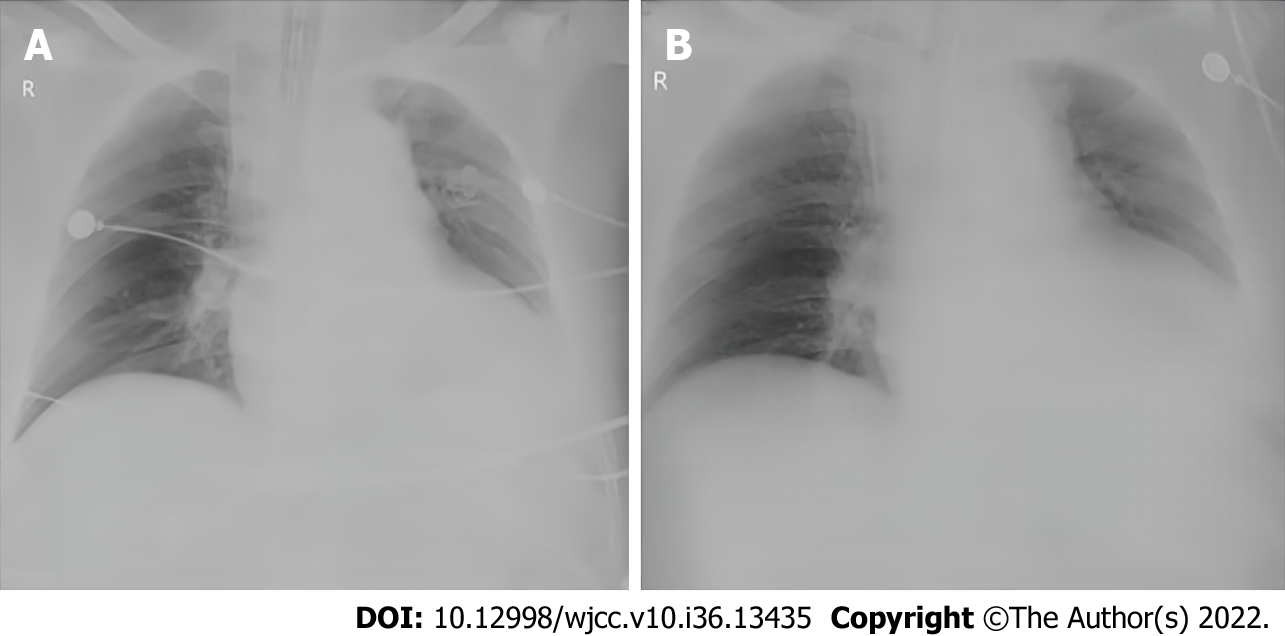
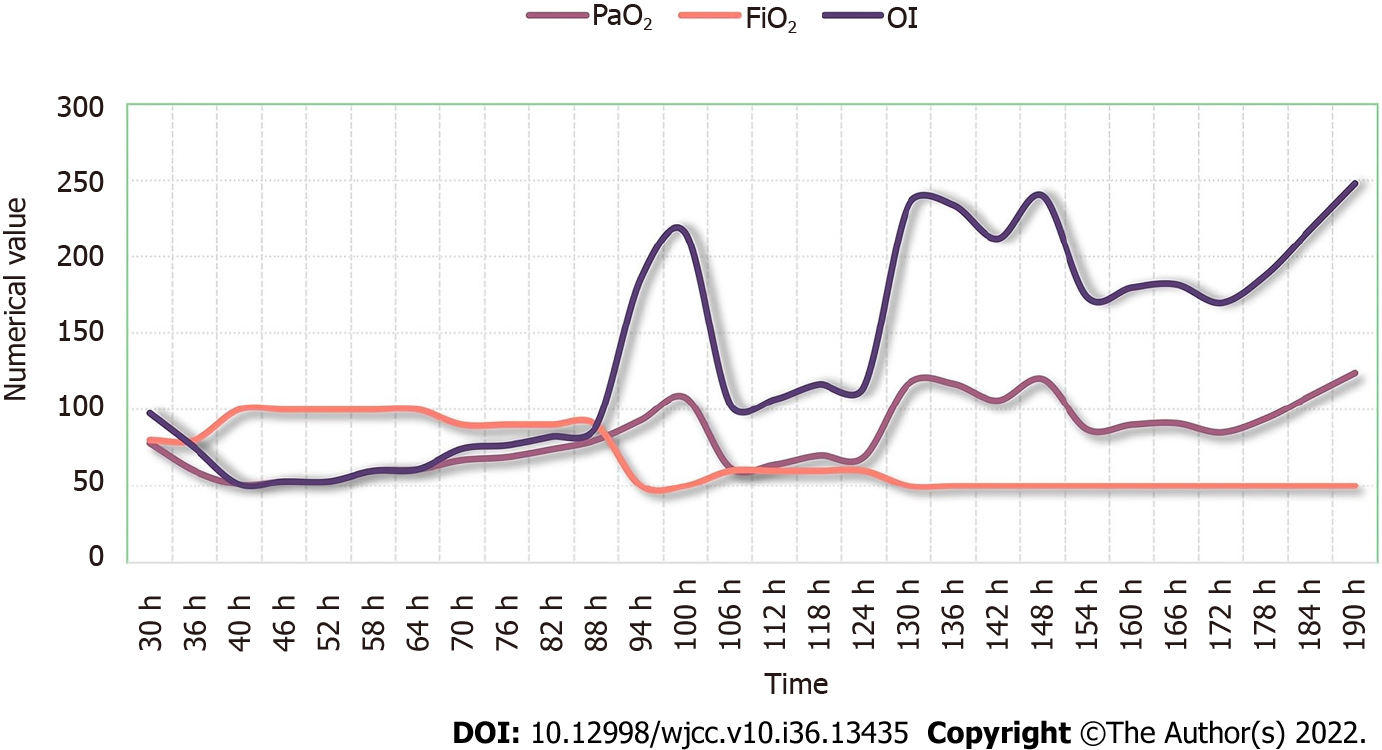
Despite combined treatment with lung protective ventilation, fluid management with continuous renal replacement therapy, and airway secretion clearance, the disease continued to deteriorate and rapidly progressed to severe ARDS. The oxygenation index (OI) dropped from normal to a minimum of 51. We were ready to give emergency rescue measures, including prone ventilation and ECMO, and immediately assessed the feasibility of both approaches. Due to the large amount of drainage from the mediastinal pericardium and chest cavity after thoracotomy, we ruled out ECMO because of the potential risk of massive bleeding. The patient was treated with PP. Prior to treatment, bedside chest radiography was used to assess the lung condition (Figure 2A). The treatment guidelines suggested that PP time should be ≥ 12 h[6]. Although PP has a positive effect on patients with severe ARDS, it may be difficult in cardiac surgery patients because of the recent sternotomy. Because of the patient’s obesity and large amount of mediastinal pericardial and thoracic drainage fluid after thoracotomy, prolonged PP could have increased the risk of drainage tube compression, resulting in poor drainage. Finally, we chose PP for no more than 6 h, and 12 h after the end of PP, the prone position ventilation treatment was performed again. During this period of treatment, we assessed drain patency every hour and monitored circulatory changes in real time to prevent inadequate drainage leading to fatal acute cardiac tamponade. We dynamically followed-up the patient by blood gas analysis. After 4 d of PP, chest X-ray showed that the diffuse exudation from both lungs was significantly reduced (Figure 2B). OI was significantly improved and showed an overall upward trend during PP (Figure 3).
After intermittent short-term PP, the OI improved greatly and the diffuse exudation in both lungs of the patient was significantly reduced.
Surgery is the main treatment for type A aortic dissection[2,16]. Several medical centers have reported that severe hypoxemia is likely to occur after thoracotomy under cardiopulmonary bypass (CPB)[17], especially in the patients with long-term smoking, obesity, early renal damage and prolonged CPB.
Severe hypoxemia rapidly progresses to severe ARDS, with high mortality[4,18-21]. A study from LUNG SAFE (Large observational study to Understand the Global impact of Severe Acute respiratory Failure) showed a mortality as high as 46% for severe forms of ARDS[22]. ARDS can have pulmonary (pneumonia, aspiration, pulmonary contusion, pulmonary embolism, etc.) or extrapulmonary (sepsis, acute severe pancreatitis, cardiopulmonary bypass, severe trauma, burns, etc.) causes[5,22-24], and the prominent clinical feature is hypoxemia. It is believed that ischemia–reperfusion injury and the release of large amounts of inflammatory mediators and circulatory arrest during CPB are responsible for ARDS after cardiac surgery[17,20].
Globally, ARDS accounts for 10% of ICU admissions[25]. Although the pathogenesis of ARDS is gradually being revealed and therapeutic approaches have made significant progress, its morbidity and mortality are still high[7,26]. PP has been proven to effectively improve the prognosis of ARDS patients and reduces ventilator-induced lung injury[14,27]. In addition, PP can shorten the duration of mechanical ventilation and ICU length of stay. When lung protective mechanical ventilation cannot prevent hypoxia or hypercapnia, ECMO may also be considered in patient with severe ARDS[9]. However, even with ECMO support, the mortality rate for severe ARDS is still high. The EOLIA trial showed that in very severe ARDS, the mortality rate was 35% in patients treated with ECMO compared to 46% in patients without ECMO support[28]. Kono et al[29] reported a case that they chose V-V ECMO for Severe Respiratory Failure after Acute Aortic Dissection Surgery. Although PP and ECMO are both options for severe ARDS, ECMO is often not available in general healthcare centers and can easily cause fatal bleeding in patients with abnormal coagulation function. Therefore, PP may be a reliable treatment when ECMO is not an option. Although there are indications and contraindications for the implemen
| Indications | Severe ARDS (PaO2/FiO2 ≤ 100 mmHg with PEEP ≥ 5 cmH2O;); within 48 h after onset of ARDS; mean arterial pressure > 65 mmHg |
| Contraindications (absolute and relative) | Acial/neck trauma or spinal instability; Raised intraocular pressure or recent ophthalmic surgery, facial trauma, or recent oral maxillofacial surgery in last 15 d; Elevated intracranial pressure; Severe hemodynamic instability, unstable cardiac rhythms; Hemoptysis, unstable airway (double lumen endotracheal tube), new tracheostomy < 15 d, lung transplant; Recent sternotomy or more than 20% body surface burn; Grossly distended abdomen; Second or third trimester pregnancy, grossly distended abdomen; Venous thromboembolism treated < 48 h |
| Implementation method[8] | Requires 3-5 people, close attention to ETT and central lines; a demonstration video; and checklist are available; Preparation: Preoxygenation, empty stomach, suction; ETT/oral cavity, remove ECG leads and reattach to back, repeated zeroing of hemodynamic transducers; Support and frequently reposition pressure points: Face, shoulder, anterior pelvis |
| Prone positioning time[31] | 12-16 h per protocol |
| Possible complications | Vascular catheter kinking; Elevated intraabdominal pressure; Facial pressure ulcers, facial edema, brachial plexus injury (arm extension); Cardiac arrest |
| Time to stop | PaO2/FiO2 remained > 150 mm Hg 4 h after supinating (with PEEP < 10 cm H2O and FiO2 < 0.6) |
Therefore, we believe that it is feasible to perform prone ventilation in the early postoperative period in patients with aortic dissection. However, it is necessary to formulate an individualized plan, which not only achieves a better therapeutic effect, but also minimizes the associated potential risks, such as acute cardiac tamponade due to poor drainage of the diaphragmatic drainage tube.
The occurrence of ARDS after aortic dissection is high, and simple lung protective ventilation and fine fluid management are often ineffective. For patients with severe ARDS after CPB for aortic dissection, intermittent short-course PP may be useful when there is no ECMO support or when the risk associated with ECMO is high.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Critical care medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Al-Ani RM, Iraq; Schoenhagen P, United States S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Gawinecka J, Schönrath F, von Eckardstein A. Acute aortic dissection: pathogenesis, risk factors and diagnosis. Swiss Med Wkly. 2017;147:w14489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 108] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 2. | Nienaber CA, Clough RE. Management of acute aortic dissection. Lancet. 2015;385:800-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 443] [Article Influence: 44.3] [Reference Citation Analysis (0)] |
| 3. | Morello F, Santoro M, Fargion AT, Grifoni S, Nazerian P. Diagnosis and management of acute aortic syndromes in the emergency department. Intern Emerg Med. 2021;16:171-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 38] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 4. | Zhou J, Pan J, Yu Y, Huang W, Lai Y, Liang W, Nong L, Liu X, Chen S, Xu Y, He W, Li Y, Huang Y, Sang L. Independent risk factors of hypoxemia in patients after surgery with acute type A aortic dissection. Ann Palliat Med. 2021;10:7388-7397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 5. | Ferguson ND, Fan E, Camporota L, Antonelli M, Anzueto A, Beale R, Brochard L, Brower R, Esteban A, Gattinoni L, Rhodes A, Slutsky AS, Vincent JL, Rubenfeld GD, Thompson BT, Ranieri VM. The Berlin definition of ARDS: an expanded rationale, justification, and supplementary material. Intensive Care Med. 2012;38:1573-1582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1051] [Cited by in RCA: 962] [Article Influence: 74.0] [Reference Citation Analysis (0)] |
| 6. | Griffiths MJD, McAuley DF, Perkins GD, Barrett N, Blackwood B, Boyle A, Chee N, Connolly B, Dark P, Finney S, Salam A, Silversides J, Tarmey N, Wise MP, Baudouin SV. Guidelines on the management of acute respiratory distress syndrome. BMJ Open Respir Res. 2019;6:e000420. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 287] [Cited by in RCA: 295] [Article Influence: 49.2] [Reference Citation Analysis (0)] |
| 7. | Confalonieri M, Salton F, Fabiano F. Acute respiratory distress syndrome. Eur Respir Rev. 2017;26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 141] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 8. | Scholten EL, Beitler JR, Prisk GK, Malhotra A. Treatment of ARDS With Prone Positioning. Chest. 2017;151:215-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 248] [Article Influence: 27.6] [Reference Citation Analysis (0)] |
| 9. | Combes A, Peek GJ, Hajage D, Hardy P, Abrams D, Schmidt M, Dechartres A, Elbourne D. ECMO for severe ARDS: systematic review and individual patient data meta-analysis. Intensive Care Med. 2020;46:2048-2057. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 229] [Cited by in RCA: 240] [Article Influence: 48.0] [Reference Citation Analysis (0)] |
| 10. | Copeland H, Levine D, Morton J, Hayanga JWA. Acute respiratory distress syndrome in the cardiothoracic patient: State of the art and use of veno-venous extracorporeal membrane oxygenation. JTCVS Open. 2021;8:97-103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 11. | Johnson NJ, Luks AM, Glenny RW. Gas Exchange in the Prone Posture. Respir Care. 2017;62:1097-1110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 12. | Munshi L, Del Sorbo L, Adhikari NKJ, Hodgson CL, Wunsch H, Meade MO, Uleryk E, Mancebo J, Pesenti A, Ranieri VM, Fan E. Prone Position for Acute Respiratory Distress Syndrome. A Systematic Review and Meta-Analysis. Ann Am Thorac Soc. 2017;14:S280-S288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 269] [Cited by in RCA: 363] [Article Influence: 51.9] [Reference Citation Analysis (0)] |
| 13. | Alessandri F, Pugliese F, Ranieri VM. The Role of Rescue Therapies in the Treatment of Severe ARDS. Respir Care. 2018;63:92-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 14. | Guérin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, Mercier E, Badet M, Mercat A, Baudin O, Clavel M, Chatellier D, Jaber S, Rosselli S, Mancebo J, Sirodot M, Hilbert G, Bengler C, Richecoeur J, Gainnier M, Bayle F, Bourdin G, Leray V, Girard R, Baboi L, Ayzac L; PROSEVA Study Group. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159-2168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2391] [Cited by in RCA: 2539] [Article Influence: 211.6] [Reference Citation Analysis (0)] |
| 15. | Gu J, Feng Y, Chen S, Cao Y, Li K, Du Y, Li N, Li H. Prone Position in Treatment of Hypoxemia in Patients Who Underwent Type A Aortic Dissection Surgery. Heart Surg Forum. 2022;25:E300-E304. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Sayed A, Munir M, Bahbah EI. Aortic Dissection: A Review of the Pathophysiology, Management and Prospective Advances. Curr Cardiol Rev. 2021;17:e230421186875. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 85] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 17. | Chen MF, Chen LW, Cao H, Lin Y. Analysis of risk factors for and the prognosis of postoperative acute respiratory distress syndrome in patients with Stanford type A aortic dissection. J Thorac Dis. 2016;8:2862-2871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Rong LQ, Di Franco A, Gaudino M. Acute respiratory distress syndrome after cardiac surgery. J Thorac Dis. 2016;8:E1177-E1186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 54] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 19. | Sheng W, Yang HQ, Chi YF, Niu ZZ, Lin MS, Long S. Independent risk factors for hypoxemia after surgery for acute aortic dissection. Saudi Med J. 2015;36:940-946. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 20. | Stephens RS, Shah AS, Whitman GJ. Lung injury and acute respiratory distress syndrome after cardiac surgery. Ann Thorac Surg. 2013;95:1122-1129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 119] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 21. | Kogan A, Segel MJ, Ram E, Raanani E, Peled-Potashnik Y, Levin S, Sternik L. Acute Respiratory Distress Syndrome following Cardiac Surgery: Comparison of the American-European Consensus Conference Definition versus the Berlin Definition. Respiration. 2019;97:518-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 22. | Abe T, Madotto F, Pham T, Nagata I, Uchida M, Tamiya N, Kurahashi K, Bellani G, Laffey JG; LUNG-SAFE Investigators and the ESICM Trials Group. Epidemiology and patterns of tracheostomy practice in patients with acute respiratory distress syndrome in ICUs across 50 countries. Crit Care. 2018;22:195. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 102] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 23. | Laffey JG, Madotto F, Bellani G, Pham T, Fan E, Brochard L, Amin P, Arabi Y, Bajwa EK, Bruhn A, Cerny V, Clarkson K, Heunks L, Kurahashi K, Laake JH, Lorente JA, McNamee L, Nin N, Palo JE, Piquilloud L, Qiu H, Jiménez JIS, Esteban A, McAuley DF, van Haren F, Ranieri M, Rubenfeld G, Wrigge H, Slutsky AS, Pesenti A; LUNG SAFE Investigators; ESICM Trials Group. Geo-economic variations in epidemiology, patterns of care, and outcomes in patients with acute respiratory distress syndrome: insights from the LUNG SAFE prospective cohort study. Lancet Respir Med. 2017;5:627-638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 89] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 24. | Sanfilippo F, Palumbo GJ, Bignami E, Pavesi M, Ranucci M, Scolletta S, Pelosi P, Astuto M. Acute Respiratory Distress Syndrome in the Perioperative Period of Cardiac Surgery: Predictors, Diagnosis, Prognosis, Management Options, and Future Directions. J Cardiothorac Vasc Anesth. 2022;36:1169-1179. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 40] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 25. | Peck TJ, Hibbert KA. Recent advances in the understanding and management of ARDS. F1000Res. 2019;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 46] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 26. | Yadav H, Thompson BT, Gajic O. Fifty Years of Research in ARDS. Is Acute Respiratory Distress Syndrome a Preventable Disease? Am J Respir Crit Care Med. 2017;195:725-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 127] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 27. | Poon WH, Ramanathan K, Ling RR, Yang IX, Tan CS, Schmidt M, Shekar K. Prone positioning during venovenous extracorporeal membrane oxygenation for acute respiratory distress syndrome: a systematic review and meta-analysis. Crit Care. 2021;25:292. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 45] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 28. | Sameed M, Meng Z, Marciniak ET. EOLIA trial: the future of extracorporeal membrane oxygenation in acute respiratory distress syndrome therapy? Breathe (Sheff). 2019;15:244-246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 29. | Kono T, Oda T, Akaiwa K, Nakamura K, Tanaka H. Veno-Venous Extracorporeal Membrane Oxygenation for Acute Lung Injury after Surgery for Aortic Dissection: A Case Report. WJCG. 2017;7:156-163. [DOI] [Full Text] |
| 30. | Guérin C, Albert RK, Beitler J, Gattinoni L, Jaber S, Marini JJ, Munshi L, Papazian L, Pesenti A, Vieillard-Baron A, Mancebo J. Prone position in ARDS patients: why, when, how and for whom. Intensive Care Med. 2020;46:2385-2396. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 113] [Cited by in RCA: 277] [Article Influence: 55.4] [Reference Citation Analysis (0)] |
| 31. | Mitchell DA, Seckel MA. Acute Respiratory Distress Syndrome and Prone Positioning. AACN Adv Crit Care. 2018;29:415-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |