Published online Dec 26, 2022. doi: 10.12998/wjcc.v10.i36.13402
Peer-review started: September 7, 2022
First decision: October 12, 2022
Revised: October 28, 2022
Accepted: December 5, 2022
Article in press: December 5, 2022
Published online: December 26, 2022
Processing time: 110 Days and 15.1 Hours
Pyogenic liver abscess (PLA) due to foreign body penetration of the gastrointestinal tract is rare but can lead to serious consequences if not diagnosed and managed properly. We report a case of PLA caused by a fishbone puncture.
This report describes the clinical features, diagnosis and treatment of a 56-year-old male patient who presented with severe pneumonia, acute respiratory failure and septic shock. The main clinical manifestation was a nonspecific recurrent infection. Based on the findings of abdominal computed tomography examination and the detailed medical history, the diagnosis was made as PLA which was caused by fishbone puncture through the stomach wall and into the liver. After active anti-inflammatory treatment, the patient's general condition had improved. The laparoscopic drainage of the liver abscess and the foreign body removal was performed. There was no recurrence of abscess at discharge or during follow-up and the patient’s general condition was satisfactory.
PLA caused by foreign bodies usually requires surgical treatment or percutaneous drainage combined with antibiotics. Our case confirms that a laparoscopic approach is safe and feasible for such cases.
Core Tip: Pyogenic liver abscess (PLA) secondary to perforation of the gastrointestinal tract by a foreign body usually requires surgical treatment. This case report shows that the diagnosis of PLA caused by a foreign body is a medical challenge. Patients usually present with atypical symptoms. Clinicians should make a timely diagnosis and perform surgical intervention promptly.
- Citation: Kadi A, Tuergan T, Abulaiti Y, Shalayiadang P, Tayier B, Abulizi A, Tuohuti M, Ahan A. Laparoscopic treatment of pyogenic liver abscess caused by fishbone puncture through the stomach wall and into the liver: A case report. World J Clin Cases 2022; 10(36): 13402-13407
- URL: https://www.wjgnet.com/2307-8960/full/v10/i36/13402.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i36.13402
Although ingestion of foreign bodies is common, complications are relatively rare in the clinical setting. Pyogenic liver abscess (PLA) due to gastrointestinal perforation by foreign bodies is even rarer, and the diagnosis is challenging due to the nonspecific symptoms and imaging difficulties. Timely diagnosis is very important for improving patient prognosis. If not timely diagnosed, surgical intervention for such cases may not be conducted in time, which may lead to serious consequences. This report presented a case with PLA caused by a fishbone puncture through the stomach wall and into the liver. The clinical features, diagnosis and treatment of this case were described. The report would contribute to the timely and accurate diagnosis and the treatment of PLA caused by foreign bodies.
A 56-year-old male patient presented with complaints of intermittent chest tightness and shortness of breath for 7 d, worsening for 1 d, and was admitted to the intensive care unit of the Emergency Department.
The patient presented with chest tightness and shortness of breath about 1 wk ago. One day prior, the aforementioned symptoms progressed and the patient further developed tremor of the hands, loss of appetite, general malaise and loss of consciousness without obvious cause.
The patient had no history of alcohol consumption, drug abuse or other high-risk behaviors causing PLA. He was in good health and denied any history of hypertension, diabetes and/or heart diseases.
The patient denied any family history of hypertension, diabetes and heart diseases.
The patient’s abdomen was soft with right upper quadrant tenderness but there was no rebound pain or muscle tension. The vital signs were as follows: Body temperature 39.2 °C; blood pressure 98/56 mmHg; heart rate 84 beats per min; respiratory rate 26 breaths per min. There was no obvious abnormalities in other physical examinations.
Laboratory examinations showed that the white blood cell count was 22.22×109/L; neutrophil percentage was 91.7%; platelet count was 26 × 109/L; pH was 7.28; PCO2 was 27 mmHg; PO2 was 64 mmHg; HCO3- was 12.7 mmol/L; BE (Base Excess) was -12.5 mmol/L; C-reactive protein level was > 90 mg/L; interleukin 6 was > 5000 pg/mL; procalcitonin was > 100 ng/mL; and, myoglobin was > 2000 ug/L.
The cranial computed tomography (CT) showed that the soft tissue of the posterior top of the nasopharynx was slightly thicker. The thoracic CT observed that there were bilateral pneumonia, lung air sac in the right lung apex, multiple nodules in bilateral lungs and bilateral pleural effusion. On the abdominal and pelvic CT, there were foci with a slightly lower density in the right lobe of the liver and mixed density in segment IV of the liver near the first porta hepatis.
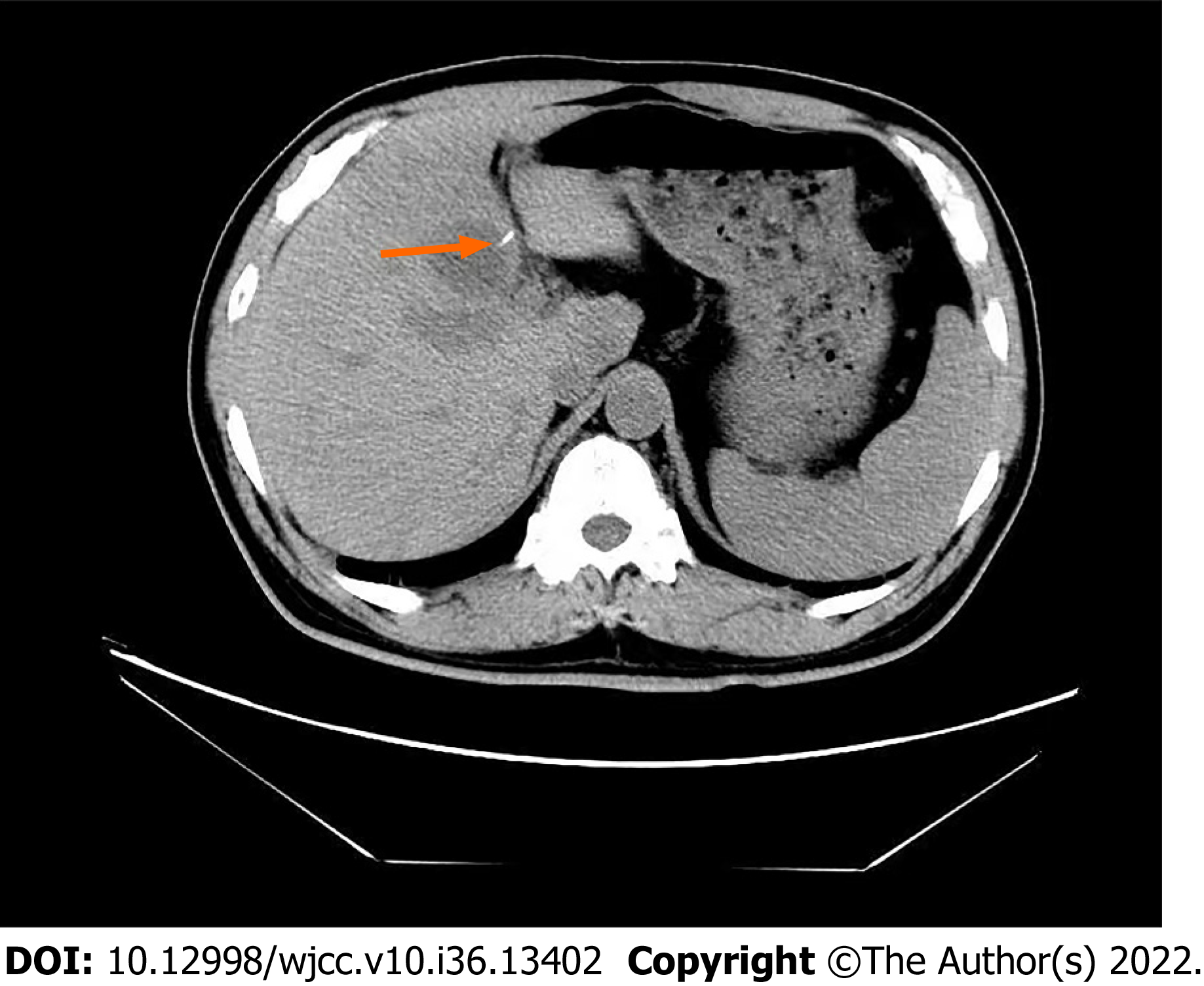
Multidisciplinary team (MDT) discussion results were as follows: On abdominal CT, there was a needle-like high-density shadow in the liver, however, this was missed in the initial report (Figure 1). The drainage from the indwelling gastric tube was brown, which suggests purulent infection. Based on these findings, we presumed that the cause of the PLA may be that the accidentally ingested fishbone may have pierced the pylorus and penetrated the liver, causing local inflammatory reaction, abscess, and the corresponding clinical manifestations. After reviewing the medical history again, it was found that the patient did have a history of eating fish a few days before the onset of disease
The final diagnosis was PLA caused by fishbone puncture complicated with severe pneumonia, acute respiratory failure, and septic shock.
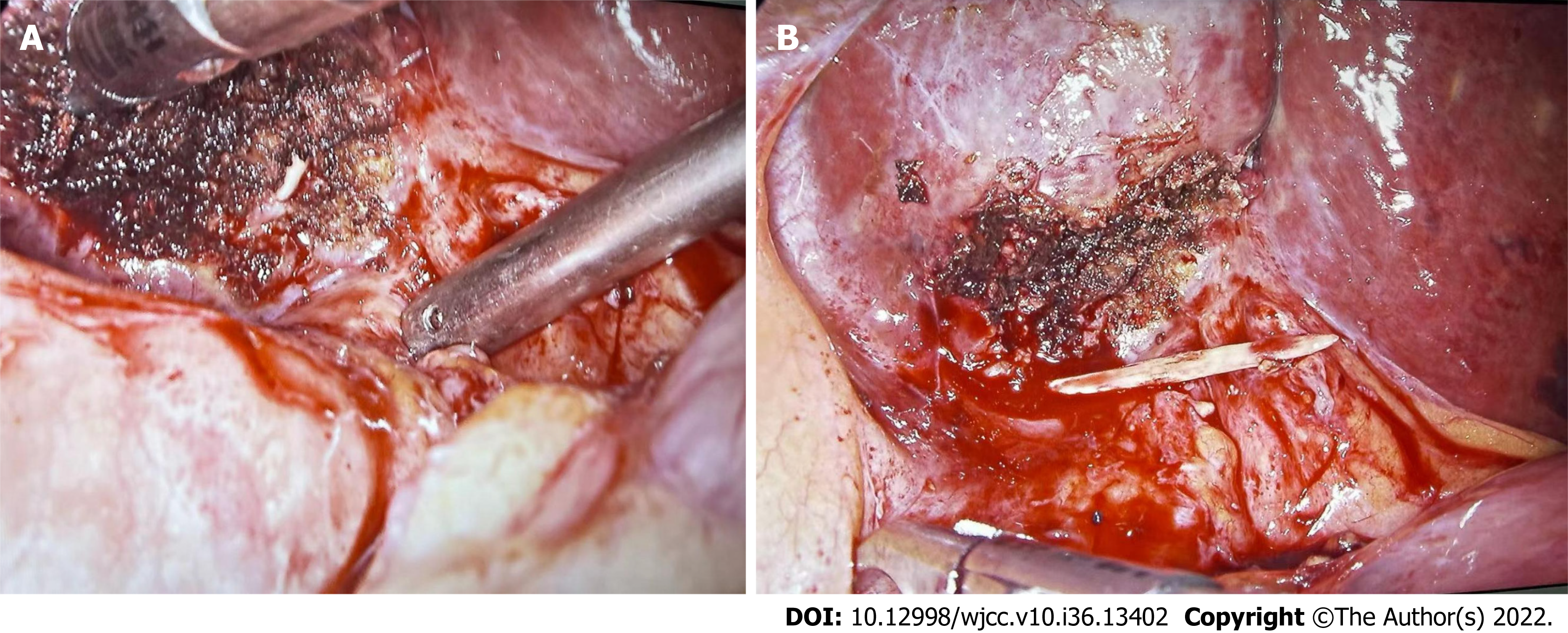
The patient received anti-inflammatory rescue therapy, electrolyte correction, and nutritional support for 8 d in the intensive care unit, and then was transferred back to the general ward. However, the patient had recurrent fever without significant decreases in the inflammatory index and was returned to the intensive care unit again. Repeat abdominal CT showed combined density, and PLA was considered based on the medical history. The diagnosis and cause of PLA were discussed by MDT. Subsequently, the patient was transferred to the Hepatobiliary Surgery Department for laparoscopic exploration. A multiport laparoscope was used. An inspection hole was made above the navel in order to introduce the laparoscope and the remaining three trocars. During the operation, it was found that there were dense adhesions between the pylorus and hepatic hilum and the liver was obviously swollen at the root of the ligamentum teres. After incision, a white foreign body about 2 cm long was found (Figure 2A), which was confirmed to be a fishbone after removal (Figure 2B). An abscess cavity was found by further in-deep exploration, which was incised and the white pus was drained. The abscess cavity was expanded and a drainage tube was placed for adequate drainage.
After the operation, the patient recovered smoothly. A small amount of reddish drainage fluid was observed. After 5 d of observation, the inflammatory indexes were decreased, and the above symptoms and discomfort disappeared. The drainage tube was therefore removed. The patient was discharged in stable condition. Follow-up at 2 wk and 2 mo after discharge was unremarkable.
Liver abscesses are purulent lesions of the liver caused by various pathogens such as bacteria, fungi or Entamoeba histolytica. Biliary route, portal vein route, hepatic artery route, cryptogenic route and direct route to the liver from an open wound are the common infection routes of bacterial liver abscess. Hepatic artery and open wound routes are relatively rare in clinical practice, but cannot be ignored[1]. PLA caused by foreign bodies are rare[2]. It has been reported that the incidence of foreign body penetration of the gastrointestinal tract is less than 1%, and the most common sites of gastrointestinal perforation include the stomach and duodenum. Accidental ingestion of foreign bodies is not uncommon, and the vast majority (80%-90%) of the ingested foreign bodies pass naturally through the gastrointestinal tract within 1 wk. In fact, less than 1% of the patients who ingest foreign bodies could experience symptoms, which are usually secondary to gastrointestinal obstruction or perforation[3]. PLA secondary to foreign body penetration of the gastrointestinal tract are even more rare. Lambert[4] reported the first case in 1898. Since then, there has been an increasing number of studies on such cases, especially over the past 40 years. The duodenum and pylorus may be more prone to perforation[5]. PLA caused by perforation of fishbone through the stomach is relatively hidden and dangerous, which can often bring serious consequences. Theodoropoulou et al[6] reported a high fever in a 46-year-old man without comorbidities, who died of sepsis within 46 h of admission. In the autopsy, a fishbone was found in the liver. Their report points to the level of vigilance clinicians must be aware of in each particular case and this clinical presentation is very similar to our case reported herein. PLA is a disease well known to clinicians and its clinical manifestations are diverse. Some patients present with high fever, right upper quadrant pain, and jaundice. Most patients would be cured after anti-infective treatment, puncture, and drainage. More dangerous and systemic infection with PLA requires the identification of the cause, especially if the patient has no major infectious factors such as biliary tract infection, blood infection or diabetes. In this report, the thickening of the gastrointestinal tract adjacent to the abscess on the preoperative CT examination, as well as the presence of intraoperative adhesions, were clues of PLA secondary to foreign body penetration of the gastrointestinal tract. The clinical manifestations of PLA caused by foreign bodies are usually ambiguous and nonspecific, but abdominal pain (77.3%) and fever (58%) are the most common symptoms[7,8]. Occasionally, acute upper gastrointestinal bleeding may be present[9]. Chen et al[10] have summarized 86 cases of liver abscess caused by foreign bodies such as toothpicks, fishbones, chicken bones, needles, etc. They listed many groups at risk for foreign body perforations, including prison inmates, mentally ill, alcoholics, children, the elderly, carpenters, and tailors. Other conditions included fast food, hot or cold drinks, cognitive impairment, and people wearing dentures. Early identification and extraction of foreign bodies causing gastrointestinal perforation is critical to avoid morbidity and mortality[11,12]. However, early diagnosis is challenging due to the lack of specific findings, the lack of patient awareness of foreign body ingestion, and the low index of suspicion by the medical team for the specific condition. Liver abscess due to foreign body ingestion is still rare and a difficult diagnosis because most patients do not recall foreign body ingestion events and usually present with nonspecific symptoms[13]. Moreover, the foreign bodies are not visible on X-rays and sometimes not even on CT scans.
It is worth noting that there can be a considerable time span of months or even years between the ingestion event and the onset of symptoms of an inflammatory lump or abscess. If foreign body perforation is not properly diagnosed in a timely manner, percutaneous interventional drainage can lead to recurrence or persistence of abscesses, and can even lead to a life-threatening sepsis. Therefore, in refractory abscess after interventional drainage and antibiotics, PLA caused by foreign bodies, although rare, should be considered as the underlying pathogenesis. Clinicians should also be aware that older adults wearing dental prosthetic devices may ingest foreign bodies. CT scans are currently the gold standard for diagnosing foreign body ingestion due to their high resolution and accuracy. Foreign bodies usually appear as high-density linear objects on CT, and CT scans of foreign body ingestion can also determine the presence of perforation, the degree of intra-abdominal inflammation with or without abscess formation, and adjacent organ damage[14]. Contrast-enhanced CT scan is the standard diagnostic modality that provides high resolution and accuracy, followed by abdominal ultrasound[15]. In this report, CT scan was also used for diagnosis. For patients with poor tolerance, unstable vital signs, or contraindications to resection, conservative treatment and supportive treatment can be accepted as the first step, and the situation will improve after re-evaluation. The removal of foreign bodies can be considered at the time of diagnosis. In the 86 cases summarized by Chen et al[10], the foreign bodies in the liver were successfully removed after exploratory laparotomy and 2 cases received laparoscopy for foreign body removal. Comparing the difference between traditional exploratory laparotomy and laparoscopy, it could be concluded that the postoperative hospital stay after laparoscopic surgery is significantly shorter than that of laparotomy. Burkholder and Samant[16] treated a case with fish bone-induced liver abscess with antibiotics and percutaneous drainage, avoiding the need for open surgical intervention. They concluded that percutaneous drainage was the appropriate first line treatment in most cases, even in cases of retained foreign body. When the percutaneous drainage and antibiotics are not effective, removal of foreign bodies causing the PLA is necessary, and laparoscopic surgery is an effective method for the treatment of PLA caused by foreign bodies[17].
Cases of PLA secondary to foreign body penetration of the gastrointestinal tract are extremely rare, the diagnosis of which requires comprehensive analysis and evaluation of the medical history, imaging data, disease progression and systemic condition. Surgery is an effective way to remove the cause, and laparoscopic removal of the foreign bodies is also an effective minimally invasive treatment. Meanwhile, clinicians should improve the understanding of this type of disease, and achieve early detection and early treatment, which is conducive to the prognosis of patients.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Cerwenka H, Austria; Shelat VG, Singapore S-Editor: Xing YX L-Editor: Filipodia P-Editor: Xing YX
| 1. | Huang Y, Zhang W. Research advances in diagnosis and treatment of bacterial liver abscess. J Clin Hepatol. 2018;34:641-644. [DOI] [Full Text] |
| 2. | Venkatesan S, Falhammar H. Pyogenic hepatic abscess secondary to gastric perforation caused by an ingested fish bone. Med J Aust. 2019;211:451-451.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Kanazawa S, Ishigaki K, Miyake T, Ishida A, Tabuchi A, Tanemoto K, Tsunoda T. A granulomatous liver abscess which developed after a toothpick penetrated the gastrointestinal tract: report of a case. Surg Today. 2003;33:312-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 36] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Lambert A. Abscess of the liver of unusual origin. NY Med J. 2022:177-178. [RCA] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Chintamani, Singhal V, Lubhana P, Durkhere R, Bhandari S. Liver abscess secondary to a broken needle migration--a case report. BMC Surg. 2003;3:8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 61] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Theodoropoulou A, Roussomoustakaki M, Michalodimitrakis MN, Kanaki C, Kouroumalis EA. Fatal hepatic abscess caused by a fish bone. Lancet. 2002;359:977. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 42] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Glick WA, Simo KA, Swan RZ, Sindram D, Iannitti DA, Martinie JB. Pyogenic hepatic abscess secondary to endolumenal perforation of an ingested foreign body. J Gastrointest Surg. 2012;16:885-887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Chong LW, Sun CK, Wu CC. Successful treatment of liver abscess secondary to foreign body penetration of the alimentary tract: a case report and literature review. World J Gastroenterol. 2014;20:3703-3711. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 35] [Cited by in RCA: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Leggieri N, Marques-Vidal P, Cerwenka H, Denys A, Dorta G, Moutardier V, Raoult D. Migrated foreign body liver abscess: illustrative case report, systematic review, and proposed diagnostic algorithm. Medicine (Baltimore). 2010;89:85-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 55] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 10. | Chen J, Wang C, Zhuo J, Wen X, Ling Q, Liu Z, Guo H, Xu X, Zheng S. Laparoscopic management of enterohepatic migrated fish bone mimicking liver neoplasm: A case report and literature review. Medicine (Baltimore). 2019;98:e14705. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 11. | Bandeira-de-Mello RG, Bondar G, Schneider E, Wiener-Stensmann IC, Gressler JB, Kruel CRP. Pyogenic Liver Abscess Secondary to Foreign Body (Fish Bone) Treated by Laparoscopy: A Case Report. Ann Hepatol. 2018;17:169-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Cheung YC, Ng SH, Tan CF, Ng KK, Wan YL. Hepatic inflammatory mass secondary to toothpick perforation of the stomach: triphasic CT appearances. Clin Imaging. 2000;24:93-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Hernández-Villafranca S, Qian-Zhang S, García-Olmo D, Villarejo-Campos P. Liver abscess due to a fish bone injury: A case report and review of the literature. Cir Cir. 2020;88:1-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Yu W, Yu H, Ling J, Du J, Yin Z, Li C, Zhou M. Hepatic Abscess Secondary to Stomach Perforation by a Fish Bone: a Rare Cause of Hepatic Abscess. Ann Hepatol. 2018;17:880-883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 15. | Mateus JE, Silva C, Beirão S, Pimentel J. Hepatic Abscess Induced by Fish Bone Migration: Two Case Reports. Acta Med Port. 2018;31:276-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Burkholder R, Samant H. Management of Fish Bone-Induced Liver Abscess with Foreign Body Left In Situ. Case Reports Hepatol. 2019;2019:9075198. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 17. | Carver D, Bruckschwaiger V, Martel G, Bertens KA, Abou-Khalil J, Balaa F. Laparoscopic retrieval of a sewing needle from the liver: A case report. Int J Surg Case Rep. 2018;51:376-378. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |