Published online Dec 26, 2022. doi: 10.12998/wjcc.v10.i36.13388
Peer-review started: September 4, 2022
First decision: October 12, 2022
Revised: November 5, 2022
Accepted: December 8, 2022
Article in press: December 8, 2022
Published online: December 26, 2022
Processing time: 113 Days and 3.5 Hours
Hip revision surgery is the final treatment option for the failure of artificial hip joints, but it is more difficult than the initial operation. For patients with hip joint loosening around the prosthesis combined with large inflammatory pseudo
Male, 59 years old. The patient underwent left hip replacement 35 years ago and was now admitted to hospital due to massive masses in the left thigh, shortening of the left lower extremity, and pain and lameness of the left hip joint. X-ray, computed tomography and magnetic resonance imaging revealed prosthesis loosening, left acetabular bone defect (Parprosky IIIB type), and a bone defect of the left proximal femur (Parprosky IIIA type). Inflammatory pseudotumours were seen in the left hip and left thigh. Hip revision surgery was performed using a 3D-printed custom acetabular prosthesis was used for hip revision surgery, which was produced by Arcam Electron Beam Melting system with Electron Beam Melting technology. The operation was successful, and the patient was followed up regularly after the operation. The custom-made acetabular prosthesis was well matched, the inflammatory pseudotumour was completely removed, the postoperative hip prosthesis was stable, and the old greater trochanter fracture was well reduced and fixed. The patient was partially weight-bearing with crutches 3 mo after the operation and walked with full weight-bearing after 6 mo. The hip prosthesis was stable, and there was no recurrence of inflammatory pseudotumours at the last follow-up. The Visual Analogue Scale was 3, and the Harris hip score was 90.
The use of 3D-printed personalized custom prostheses for complex hip revision surgery has satisfactory surgical results and has great clinical application value.
Core Tip: We report a case of complex hip joint loosening around a prosthesis combined with a large inflammatory pseudotumor, extensive bone defect and an old fracture of the greater trochanter. A 3D-printed personalized prosthesis for artificial hip revision can be effectively installed. Preoperative planning and successful completion of complex hip revision surgery yielded good results.
- Citation: Wang HP, Wang MY, Lan YP, Tang ZD, Tao QF, Chen CY. Application of 3D-printed prosthesis in revision surgery with large inflammatory pseudotumour and extensive bone defect: A case report. World J Clin Cases 2022; 10(36): 13388-13395
- URL: https://www.wjgnet.com/2307-8960/full/v10/i36/13388.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i36.13388
Prosthesis loosening is one of the main reasons for revision surgery, and the appearance of an inflammatory pseudotumor, especially one with accompanying symptoms, is another[1]. Inflammatory pseudotumor parenchyma is a granulomatous or destructive cystic lesion, also known as a pseudotumor, metal metaplasia or sterile lymphocyte-dominated vasculitis[2], which has adverse reactions to metal fragments[3,4]. It is neither an infection nor a tumor and is prone to occur around total prostheses of the hip, with a tumor-like shape and varying sizes[5]. It can cause progressive pain, swelling, joint subluxation, compression, periprosthetic fractures and soft tissue destruction in the affected extremity[2,6]. Hip revision surgery is the final treatment option for prosthesis failure and for patients with periprosthetic loosening of the hip joint combined with a large inflammatory pseudotumor, extensive bone defects and nonunion of the greater trochanter. However, such surgery is rare in clinical practice and extremely difficult to perform. At present, with the continuous progress of science and technology and the continuous improvement of medicine, the application of 3D printing technology in orthopedics has gradually expanded from initial bone tumor patients to other patients with complex bone diseases, especially those with large bone defects. Due to the continuously improving cooperation between medicine and industry, the accurate 3D printing of materials is gradually being applied. The individualized materials for repair and reconstruction are prepared according to the characteristics of patients' bone defects and combined with 3D printing technology, which can meet the complex needs of patients for bone defect repair and achieve personalized and precise treatment of diseases. Therefore, the treatment of complex diseases is simplified. The successful application of 3D printing technology in the case study presented here fully demonstrates the advantages of this technology and may serve as a reference for its future clinical application. Here, we implanted a 3D-printed personalized acetabular prosthesis, and the long-term follow-up results were satisfactory.
This case report was approved by the Ethics Committee of Panzhihua Central Hospital, and written informed consent was obtained from the patient and his family.
Eight months ago, the patient developed left thigh swelling without obvious reasons, and the swelling gradually extended from the back to the front, accompanied by pain when moving the leg.
Underwent herniorrhaphy 40+ years ago in the local hospital without other diseases or operations. Unfortunately, an intertrochanteric fracture of the left femur was caused by a fall 40 years ago and was treated conservatively, with the presence of ununited fractures later. The patient underwent left hip replacement 35 years ago due to a left intertrochanteric fracture combined with left femoral head necrosis. Eight months ago, the patient developed left thigh swelling without obvious reasons, and the swelling gradually extended from the back to the front, accompanied by pain when moving the leg. The claudication of the left lower limb was aggravated, so he was admitted to our department.
Underwent herniorrhaphy 40+ years ago in the local hospital without other diseases or operations. Unfortunately, an intertrochanteric fracture of the left femur was caused by a fall 40 years ago and was treated conservatively, with the presence of ununited fractures later. The patient underwent left hip replacement 35 years ago due to a left intertrochanteric fracture combined with left femoral head necrosis.
The patient was born in the original place, without industrial poisons, radioactive substances, dust exposure history, no contact history with epidemic water in epidemic areas, smoking history of 40+years, with an average of 20 cigarettes/day, and denied drinking history. Divorce, having a child, healthy family. Deny the history of family hereditary diseases and infectious diseases.
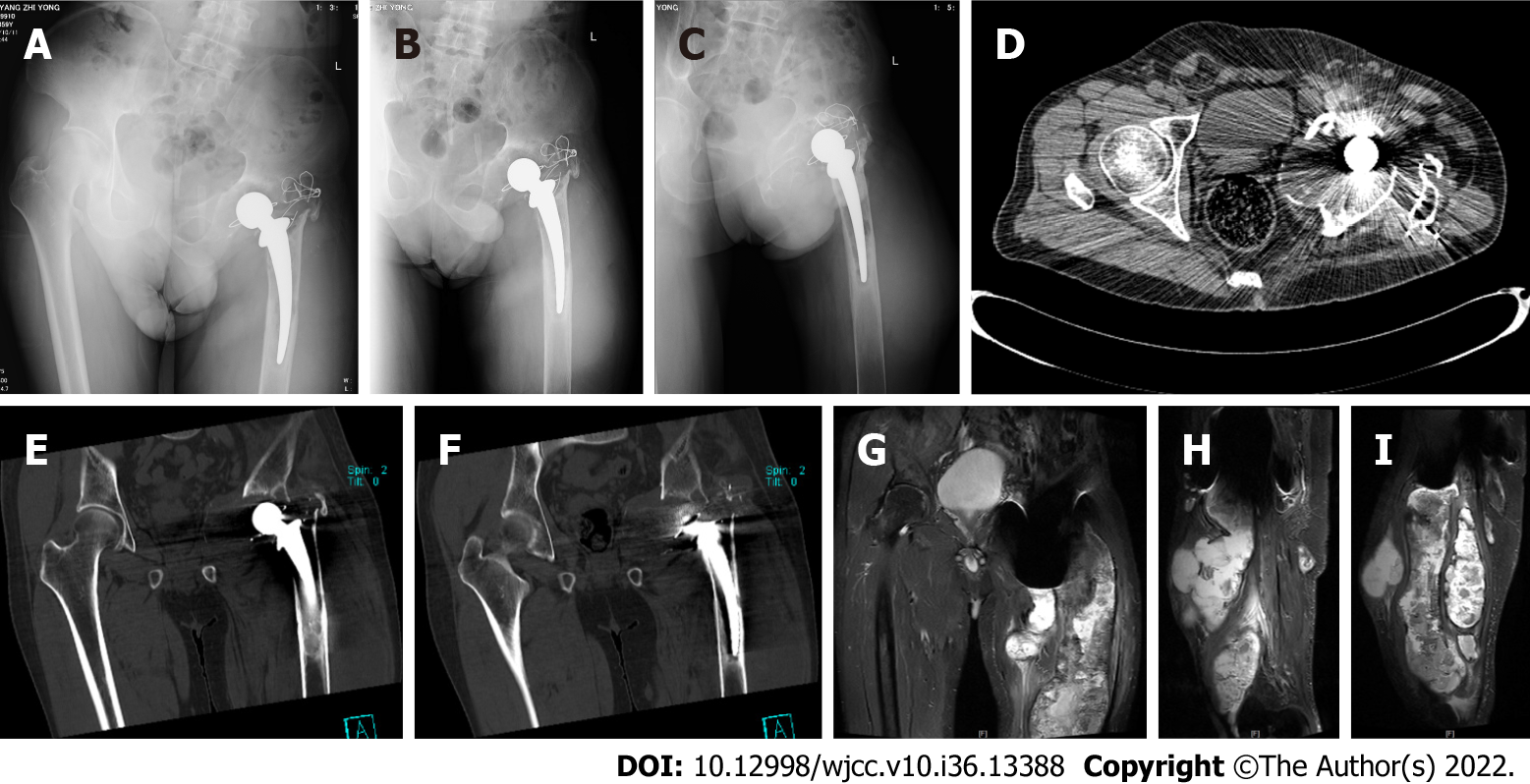
The left lower limb was shortened by approximately 8 cm compared with the right side. A 15-cm-long surgical scar was seen on the left hip, where there was no redness, swelling or exudation. The middle and upper parts of the left thigh were obviously swollen, there were palpable fluctuations, the local skin temperature was normal, and there was no obvious tenderness (Figure 1).
X-ray: Left superior pubic branch - irregular pubic comb bone. Computed tomography (CT): Partial bone absorption of the upper part of the left femur; bone destruction of the left acetabulum; swelling and unclear layers of soft tissue shadows in the upper part of the left thigh and around the hip joint; multiple cystic lesions in the upper part of the left thigh, with multiple cystic necrosis areas in the lesions, of which the posterior subcutaneous necrosis area is a long strip from the subcutaneous buttock to the lower back. Magnetic resonance imaging (MRI): The left upper femur and left hip joint have abnormal bone, with multiple necrosis sites around the hip joint and soft tissue of the left thigh as the main cystic disease. Considering the inflammatory disease, the size of the larger cystic lesion is approximately 8.7 cm × 9.3 cm × 18 cm (Figure 2).
Prosthesis loosening after left hip replacement; Inflammatory pseudotumor of left thigh; Old fracture of left greater trochanter of femur; Shortening deformity of left lower limb.
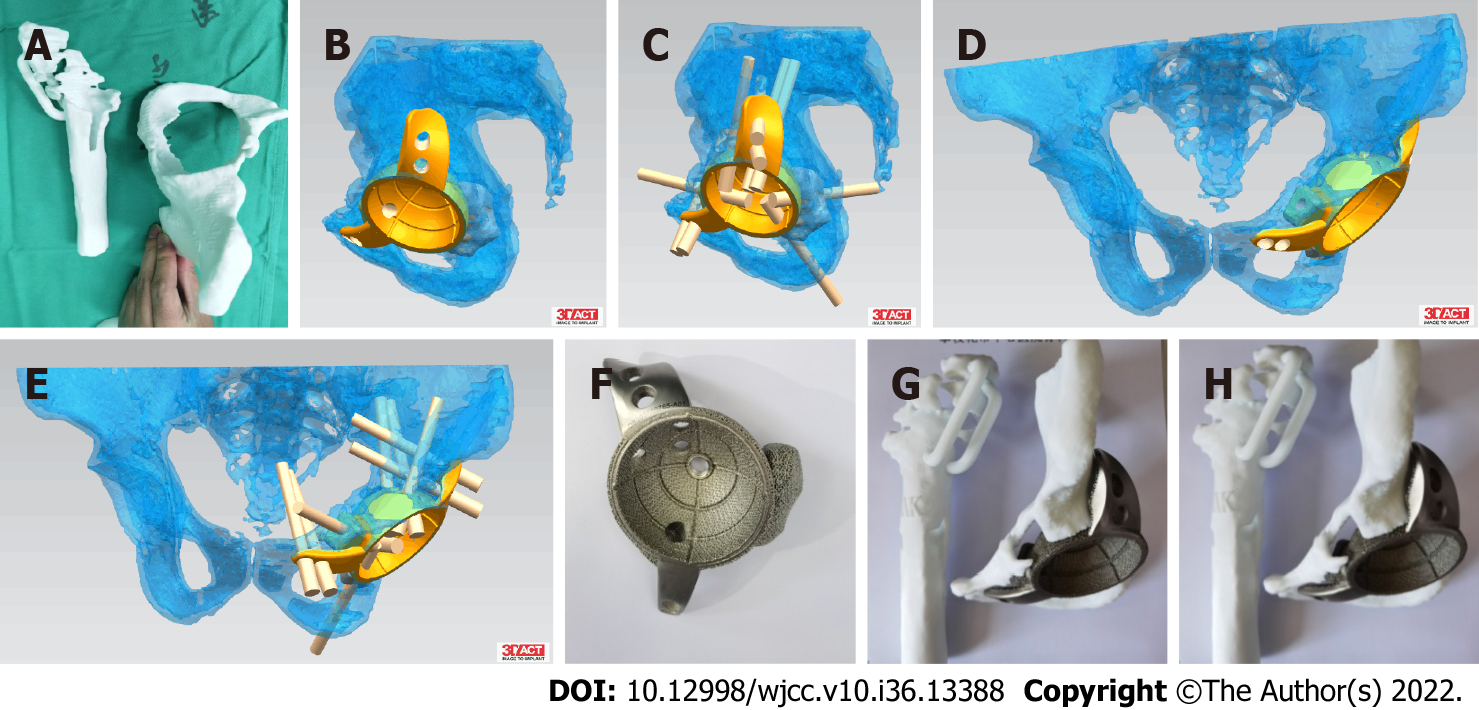
CT examination of the patient's hip joint was performed after admission. The 1:1-sized hip joint model was printed through 3D printing technology (supported by Akcome Medical Co., Ltd.), which we used for preoperative planning and disease communication. Revision surgery is routinely performed to reconstruct acetabular side bone defects, but it is extremely difficult and costly. After fully explaining the scenario to the patient and his family members, the personalized 3D-printed custom acetabular prosthesis was used for hip revision surgery, which was produced by the Arcam EBM system with electron beam melting technology (Figure 3).
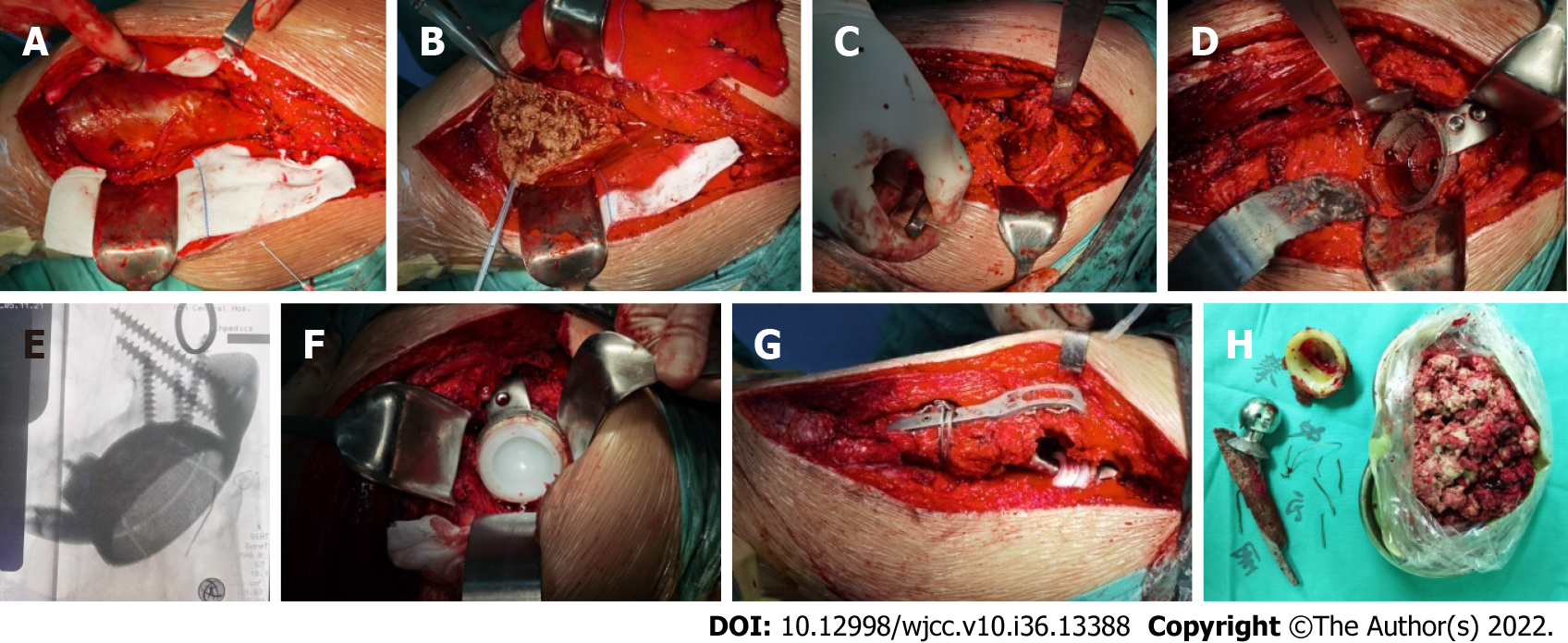
Under general anesthesia, the skin, subcutaneous tissue and scar were incised layer by layer through the posterolateral incision of the left hip, the hip joint was released, and the large inflammatory pseudotumor around the hip joint and thigh was removed. The artificial prosthesis was removed, rinsed with a large amount of normal saline and soaked with iodophor solution. Allograft cancellous bone was implanted into the bone defect of the posterior wall of the acetabulum and pressed tightly. The abduction angle was kept at 45° after the acetabulum was worn down, and the customized 3D-printed Accurate Constructive Technology acetabular prosthesis was installed with an anterior tilt of 20°. The inner lining was installed, the appropriate femoral stem and femoral head were selected and implanted, and the hip joint was reset. The hip joint in all directions was relatively stable, and the tightness was appropriate. The fractured greater trochanter was reduced and fixed with a trochanteric plate after satisfactory reduction. C-arm fluoroscopy showed that the prosthesis was in a good position (Figure 4). Complete hemostasis was performed, and an indwelling drainage tube was placed after repeated rinsing. A peripheral nerve block cocktail was given, tranexamic acid was perfused intraarticularly, and the incision was sutured.
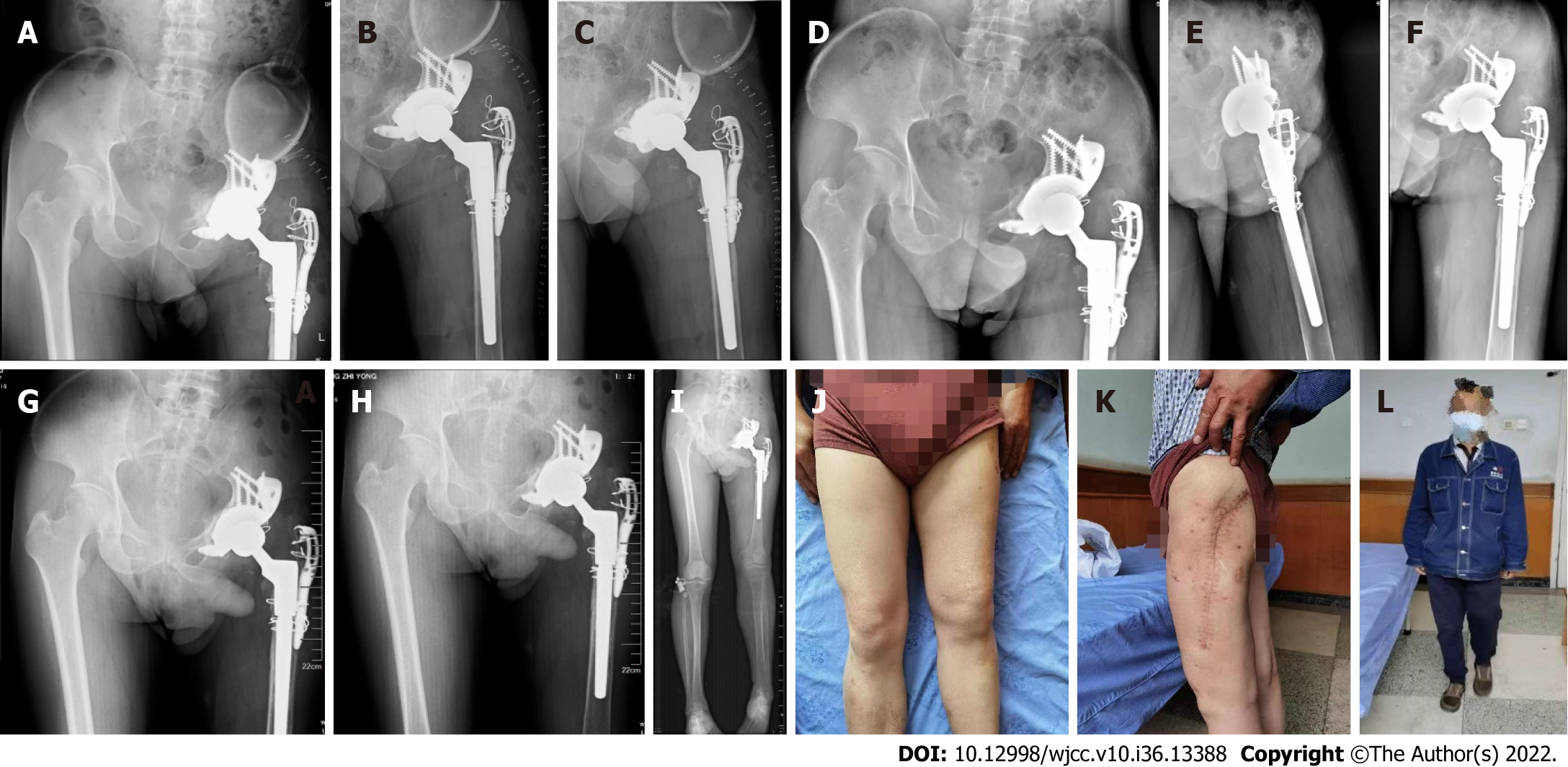
We strove for a fast recovery in the perioperative period. Postoperatively, to prevent thrombosis, cefuroxime sodium was given for anti-inflammation and rivaroxaban was given for anticoagulation. Postoperative bacterial culture was negative, and the pathology showed a small amount of neutrophil and lymphocyte infiltration and no obvious tumor cells. X-ray imaging showed the following: The swelling of the thigh had subsided, the acetabular prosthesis was stable, the greater trochanter fracture was well reduced and fixed, the femoral stem and the greater trochanter were stably held in place, the fixation was effective, and the hip joint position was satisfactory. The patient was kept to strict bed rest after surgery, hip joint activities were performed on the 2nd day after surgery, and the drainage tube was removed on the 3rd day. The patient underwent debridement due to poor incision healing 3 wk after the operation. During the operation, it was found that the residual inflammatory pseudotumor recurred, but the wound recovered well after the residual inflammatory pseudotumor was completely removed. The patient regularly returned to the hospital for follow-up at 1.5 mo, 3 mo, and 6 mo. Partial weight-bearing with crutches was started 3 mo after the operation, and full weight-bearing was started at 6 mo. During the follow-up period, the wound healing was good, the greater trochanter plate and the hip prosthesis were well positioned, and no obvious osteolytic changes or inflammatory tumor recurrence were found around the prosthesis (Figure 5). There was no obvious pain or discomfort in the hip at the last follow-up, the Visual Analogue Scale was 3 points, and the Harris hip joint score was 90 points.
3D printing technology, which is a kind of additive manufacturing, emerged in 1984. It is based on the principle of discrete/accumulation of different 2D cross-sectional shapes. It is a new additive manufacturing technique that builds up materials layer by layer into 3D shapes based on digital models[7]. In recent years, with the development of 3D printing techniques in the medical industry and based on patient CT and MRI image data, reverse molding has been performed to achieve 3D model reconstruction of patient tissues and organs and medical implants, which helps optimize the surgical plan and procedure. Medical planning and surgical implementation methods have become very fast-growing innovations in clinical medicine[8,9]. At present, the application of 3D printing technology in the hip joint can be divided into four categories: (1) Establishment of an anatomical model based on patient images to promote a better understanding of the corresponding anatomy, and at the same time, to facilitate the simulations of surgery and improve the controllability of surgery in each sex; (2) Establishment of patient-specific instruments to improve surgical accuracy[10]; (3) Customizing and producing artificial joint replacement implants; and (4) Customizing the specific implanted prosthesis according to the patient's condition to increase the degree of matching with the specific anatomy of the patient[11,12,15]. How to preserve more bone mass in hip revision surgery is the key to the success of the surgery, especially for revision surgery with large bone defects. Preserving bone mass helps to achieve early full weight-bearing postoperatively, to retain as much range of joint movement as possible, and to maintain long-term prosthesis stabilization[13].
This patient had previously undergone left hip arthroplasty due to intertrochanteric fracture combined with left femoral head necrosis. During the operation, a cement prosthesis (stem and acetabulum) was used, and the intertrochanteric fracture was fixed with wire bundles after reduction. At the time of admission, the patient's left upper thigh was swollen, a local large mass bulged, and the left hip joint was painful when moving, but there were no chills, fever, skin sinus formation or exudation at the local site. White blood cells and inflammatory indicators were normal. No bacteria were found with arthrocentesis. X-ray, CT and MRI examinations showed osteolysis around the prosthesis, bone defects of the left acetabulum and proximal femur, and multiple cystic lesions in the soft tissue of the middle and upper left thigh. It was also found that the femoral trochanteric fixation wire was broken and the fracture was displaced again. The clinical manifestations of this patient are consistent with the diagnosis of an inflammatory pseudotumor, so it is highly likely that it was an inflammatory pseudotumor. According to related reports, the incidence of inflammatory pseudotumor is 40%-60% at the metal-metal interface and 20% at the metal-polyethylene interface. They are less common at ceramic-polyethylene and ceramic-ceramic interfaces[14,15], which is related to the low wear rate and the biological inertness of ceramics. Due to the long medical history of this patient, the friction between the metal femoral head and polyethylene, the micromovement of the bone cement and the bone surface, and the loosened wire continued to produce grinding. Metal ions in the synovial fluid produced by corrosion lead to the formation of inflammatory pseudotumor[14,16-18] and progressively create large defects in the femur and acetabulum.
For this patient, we made a 3D-printed 1:1-sized hip joint model. Along with the difficulty of the imaging examination, the difficulty of the operation was mainly due to the following: (1) The acetabular bone defect was very large, and it was difficult to reconstruct the acetabulum; (2) The inflammatory pseudotumor had spread far, so it was difficult to completely remove it; (3) The greater trochanter of the femur had an old fracture that had not healed, and it was difficult to effectively reduce and fix the greater trochanter; (4) The proximal femoral bone defect made it difficult to maintain the effective fixation of the greater trochanter; and (5) The patient's lower limbs were not equal in length, and it was difficult to restore their length. Based on the above difficulties, we used 3D printing to create a personalized prosthesis. The acetabular cup was fixed on the ilium and pubis by screws. It was stable and ensured effective bone ingrowth later on. A high-molecular-weight polyethylene inner village and ceramic femoral head were used to reduce the recurrence rate of inflammatory pseudotumor induced by metal ions and prolong the service life of the prosthesis. The advantages of this scheme are as follows: (1) It fully preserved the patient’s acetabular bone mass and greatly increased the contact area of the acetabular prosthesis; (2) The 3D printing module was used to repeatedly perform surgical simulation and refine the surgical plan before surgery; and (3) The design of the integrated 3D-printed prosthesis was more conducive to performing the operation and saved operation time. The greater trochanter needs to be effectively fixed to ensure the normal function of the abductor muscles, and it is also important to the future stability of the hip joint. The greater trochanter provides conditions for late healing. There is controversy over whether the inflammatory pseudotumor needs to be completely removed. According to a study, in the natural history of an inflammatory pseudotumor without intervention, 60% of the lesions will increase in volume but can be reduced or regressed in 80% of patients undergoing hip revision surgery. Sassoon et al[4] reported on 5 patients who underwent revision surgery; the inflammatory pseudotumor was partially removed in 2 patients and retained in 3 patients, and the pseudotumor was significantly reduced or regressed in all patients at the 17-mo follow-up. Therefore, in the initial operation, we focused mostly on pseudotumor with large cystic cavities that were associated with the joint and did not give special treatment to the relatively closed and hidden pseudotumor. However, the wound returned due to the recurrence of inflammatory pseudotumor in the early postoperative period. Second-stage surgery was performed for complete debridement. This shows that large inflammatory pseudotumor need to be completely removed during the operation to avoid the adverse effects of repeated inflammatory pseudotumor.
We report a case of complex hip joint loosening around a prosthesis combined with a large inflammatory pseudotumor, extensive bone defect and an old fracture of the greater trochanter. A 3D-printed personalized prosthesis for artificial hip revision can be effectively installed. Preoperative planning and successful completion of the complex hip revision surgery yielded good results. This case provides a reference for the surgical treatment of similar diseases.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Bonartsev A, Russia; Elshazly NEAB, Egypt; Lee T, Malaysia S-Editor: Liu GL L-Editor: A P-Editor: Liu GL
| 1. | Guo L, Yang Y, An B, Shi L, Han X, Gao S. Risk factors for dislocation after revision total hip arthroplasty: A systematic review and meta-analysis. Int J Surg. 2017;38:123-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 62] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 2. | Lash NJ, Whitehouse MR, Greidanus NV, Garbuz DS, Masri BA, Duncan CP. Delayed dislocation following metal-on-polyethylene arthroplasty of the hip due to 'silent' trunnion corrosion. Bone Joint J. 2016;98-B:187-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 3. | Ando W, Yasui H, Yamamoto K, Oinuma K, Tokunaga H, Inaba Y, Kobayashi N, Aihara M, Nakanishi R, Ohzono K. A comparison of the effect of large and small metal-on-metal bearings in total hip arthroplasty on metal ion levels and the incidence of pseudotumour: a five-year follow-up of a previous report. Bone Joint J. 2018;100-B:1018-1024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Sassoon AA, Barrack RL. Pseudotumour formation and subsequent resolution in metal-on-metal total hip arthroplasty following revision: Instructional review and an illustrative case report with revision using a dual mobility design. Bone Joint J. 2016;98-B:736-740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | van der Veen HC, Reininga IH, Zijlstra WP, Boomsma MF, Bulstra SK, van Raay JJ. Pseudotumour incidence, cobalt levels and clinical outcome after large head metal-on-metal and conventional metal-on-polyethylene total hip arthroplasty: mid-term results of a randomised controlled trial. Bone Joint J. 2015;97-B:1481-1487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Waterson HB, Whitehouse MR, Greidanus NV, Garbuz DS, Masri BA, Duncan CP. Revision for adverse local tissue reaction following metal-on-polyethylene total hip arthroplasty is associated with a high risk of early major complications. Bone Joint J. 2018;100-B:720-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 7. | Hughes AJ, DeBuitleir C, Soden P, O'Donnchadha B, Tansey A, Abdulkarim A, McMahon C, Hurson CJ. 3D Printing Aids Acetabular Reconstruction in Complex Revision Hip Arthroplasty. Adv Orthop. 2017;2017:8925050. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 8. | Bruns N, Krettek C. [3D-printing in trauma surgery: Planning, printing and processing]. Unfallchirurg. 2019;122:270-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Wyatt MC. Custom 3D-printed acetabular implants in hip surgery--innovative breakthrough or expensive bespoke upgrade? Hip Int. 2015;25:375-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 10. | Spencer-Gardner L, Pierrepont J, Topham M, Baré J, McMahon S, Shimmin AJ. Patient-specific instrumentation improves the accuracy of acetabular component placement in total hip arthroplasty. Bone Joint J. 2016;98-B:1342-1346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 11. | Li Q, Chen X, Lin B, Ma Y, Liao JX, Zheng Q. Three-dimensional technology assisted trabecular metal cup and augments positioning in revision total hip arthroplasty with complex acetabular defects. J Orthop Surg Res. 2019;14:431. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 12. | Wang S, Wang L, Liu Y, Ren Y, Jiang L, Li Y, Zhou H, Chen J, Jia W, Li H. 3D printing technology used in severe hip deformity. Exp Ther Med. 2017;14:2595-2599. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | Geng X, Li Y, Li F, Wang X, Zhang K, Liu Z, Tian H. A new 3D printing porous trabecular titanium metal acetabular cup for primary total hip arthroplasty: a minimum 2-year follow-up of 92 consecutive patients. J Orthop Surg Res. 2020;15:383. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 14. | Persson A, Eisler T, Bodén H, Krupic F, Sköldenberg O, Muren O. Revision for Symptomatic Pseudotumor After Primary Metal-on-Polyethylene Total Hip Arthroplasty with a Standard Femoral Stem. J Bone Joint Surg Am. 2018;100:942-949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 15. |
Malik HH, Darwood AR, Shaunak S, Kulatilake P, El-Hilly AA, Mulki O, Baskaradas A.
Three-dimensional printing in surgery: a review of current surgical applications |
| 16. | Kilb BKJ, Kurmis AP, Parry M, Sherwood K, Keown P, Masri BA, Duncan CP, Garbuz DS. Frank Stinchfield Award: Identification of the At-risk Genotype for Development of Pseudotumors Around Metal-on-metal THAs. Clin Orthop Relat Res. 2018;476:230-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Urish KL, Hamlin BR, Plakseychuk AY, Levison TJ, Higgs GB, Kurtz SM, DiGioia AM. Trunnion Failure of the Recalled Low Friction Ion Treatment Cobalt Chromium Alloy Femoral Head. J Arthroplasty. 2017;32:2857-2863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 18. | Bayley N, Khan H, Grosso P, Hupel T, Stevens D, Snider M, Schemitsch E, Kuzyk P. What are the predictors and prevalence of pseudotumor and elevated metal ions after large-diameter metal-on-metal THA? Clin Orthop Relat Res. 2015;473:477-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |