Published online Dec 26, 2022. doi: 10.12998/wjcc.v10.i36.13337
Peer-review started: August 19, 2022
First decision: October 21, 2022
Revised: November 16, 2022
Accepted: December 5, 2022
Article in press: December 5, 2022
Published online: December 26, 2022
Processing time: 129 Days and 8.6 Hours
Whether it’s better to adopt unilateral pedicle screw (UPS) fixation or to use bilateral pedicle screw (BPS) one for lumbar degenerative diseases is still controversially undetermined.
To make a comparison between UPS and BPS fixation as to how they work efficaciously and safely in patients suffering from lumbar degenerative diseases.
We have searched a lot in the databases through 2020 with index terms such as “unilateral pedicle screw fixation” and “bilateral pedicle screw fixation.” Only randomized controlled trials and some prospective cohort studies could be found, yielding 15 studies. The intervention was unilateral pedicle screw fixation; Primarily We’ve got outcomes of complications and fusion rates. Secondarily, we’ve achieved outcomes regarding total blood loss, operative time, as well as length of stay. Softwares were installed and utilized for subgroup analysis, analyzing forest plots, sensitivity, heterogeneity, forest plots, publication bias, and risk of bias.
Fifteen previous cases of study including 992 participants have been involved in our meta-analysis. UPS had slightly lower effects on fusion rate [relative risk (RR) = 0.949, 95%CI: 0.910 to 0.990, P = 0.015], which contributed mostly to this meta-analysis, and similar complication rates (RR = 1.140, 95%CI: 0.792 to 1.640, P = 0.481), Δ visual analog scale [standard mean difference (SMD) = 0.178, 95%CI: -0.021 to 0.378, P = 0.080], and Δ Oswestry disability index (SMD = -0.254, 95%CI: -0.820 to 0.329, P = 0.402). In contrast, an obvious difference has been observed in Δ Japanese Orthopedic Association (JOA) score (SMD = 0.305, 95%CI: 0.046 to 0.563, P = 0.021), total blood loss (SMD = -1.586, 95%CI: -2.182 to -0.990, P = 0.000), operation time (SMD = -2.831, 95%CI: -3.753 to -1.909, P = 0.000), and length of hospital stay (SMD = -0.614, 95%CI: -1.050 to -0.179, P = 0.006).
Bilateral fixation is more effective than unilateral fixation regarding fusion rate after lumbar interbody fusion. However, JOA, operation time, total blood loss, as well as length of stay were improved for unilateral fixation.
Core Tip: This literature is not strongly conclusive regarding whether bilateral pedicle screw (BPS) fixation or unilateral pedicle screw (UPS) one is more efficacious and safe for patients with lumbar degenerative diseases. While BPS has been considered standard, it has been associated with excessive rigidity and clinically adverse effects clinically, for example, device-related osteoporosis, adjacent segment degeneration, and a higher risk of other complications. This was the first large scale meta-analysis comparing UPS and BPS. We found UPS to have a slightly more poor fusion rate, but significantly improved prognosis regarding several clinical outcomes, possibly associated with minimal invasion.
- Citation: Sun L, Tian AX, Ma JX, Ma XL. Successful outcomes of unilateral vs bilateral pedicle screw fixation for lumbar interbody fusion: A meta-analysis with evidence grading. World J Clin Cases 2022; 10(36): 13337-13348
- URL: https://www.wjgnet.com/2307-8960/full/v10/i36/13337.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i36.13337
Lumbar interbody fusion (LIF) or spinal fusion surgery was independently proposed by Hibbs et al[1] in 1911. To date, this surgical procedure has been used to treat spinal disorders including degenerative vertebral disease, trauma, infection, and tumors for more than a century. The main procedures include discectomy, endplate preparation, bone grafting, cage insertion, pedicle screw placement, or standalone. Patient expectations and the increasing demand for shorter hospital stays have led to more innovative surgical techniques. There are five major surgical approaches: posterior LIF, anterior LIF, lateral LIF, transforaminal LIF, and oblique LIF or anterior to the psoas. The choice of surgical approach is often determined by surgeon preference and patient factors, as there has been no clear or strong evidence regarding which approach is superior[2-5]. The most common internal fixation method for fusion is posterior pedicle screw fixation, and bilateral pedicle screw (BPS) fixation is considered a standard procedure. However, excessive rigidity is suspected to result in clinically adverse effects, such as adjacent segment degeneration, device-related osteoporosis, and a higher risk of other complications[6]. While there is plenty of research exploring two pedicle screw fixations, most studies were limited by their retrospective nature, lack of a comparison group, or inadequate follow-up[7,8]. Previous meta-analyses also included the limitations of not including all prospective studies and incorporating many retrospective studies, and the results may be biased[8,9]. We retrieved all the literature about unilateral and BPS fixation after lumbar fusion in recent years and included the latest randomized controlled trials (RCTs) and prospective cohort studies. The results were meta-analyzed to provide a reference for future clinical work.
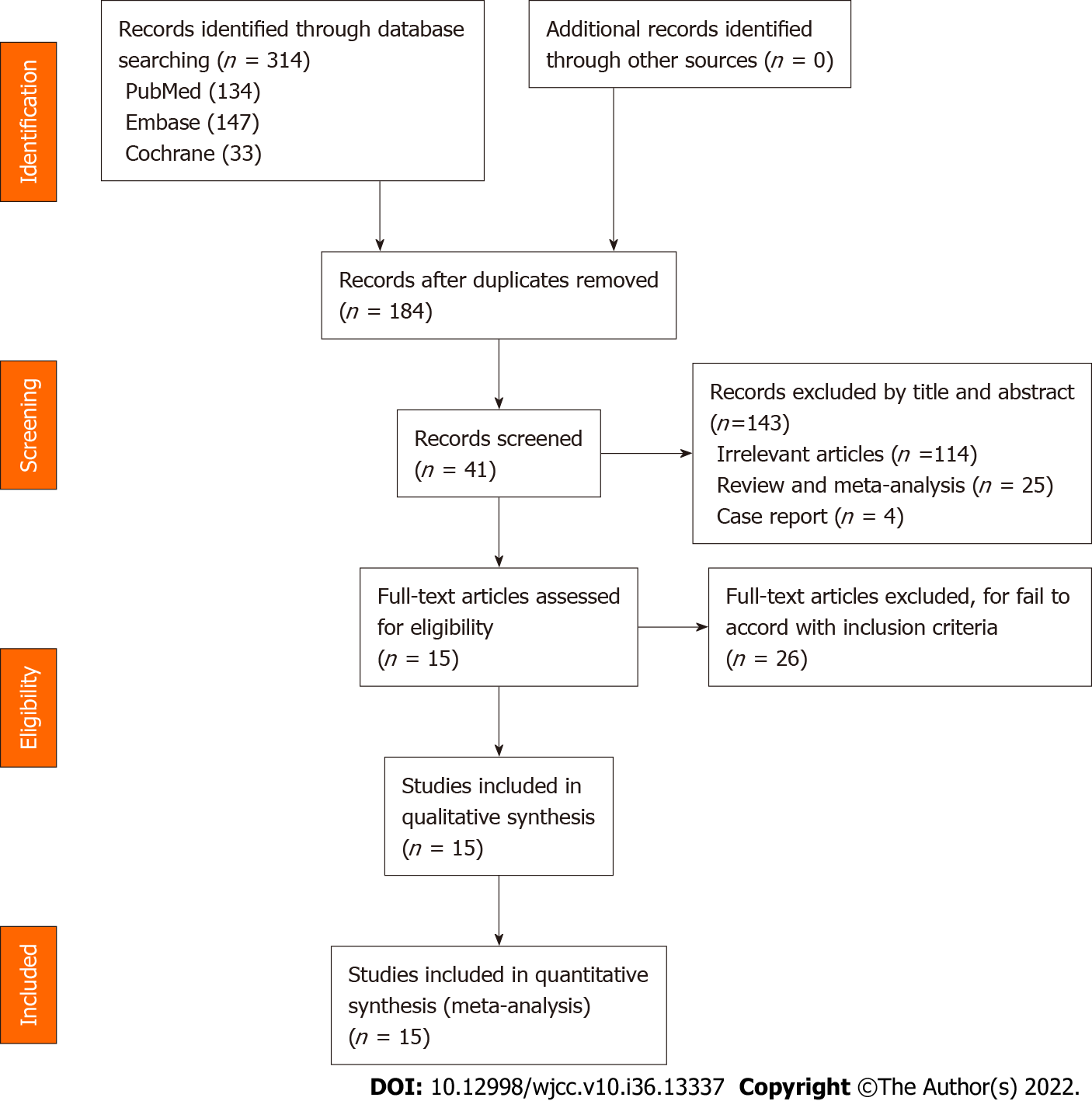
We retrieved relevant studies using “Unilateral Pedicle Screw fixation,” “lumbar interbody fusion,” “lumbar degenerative diseases” along with “Bilateral Pedicle Screw fixation,” as key words with Boolean operators “AND” or “OR” in electronic databases, namely, EMBASE, the Cochrane Library and PubMed as of January 2020. While only prospective cohort studies and RCTs carried out upon human subjects were kept for further use. For presenting the flowchart of the trial selection, Figure 1 has been worked out. PRISMA guidelines, Cochrane Handbook and GRADE system are adopted as well for assessing qualities from involved study so as for convincing that the data herein presented were not only reliable but verifiable as well[10-12].
The PICOS (Population, Intervention, Comparison, Outcome, and Study design) outline was used for including studies in the review. Inclusion criteria: (1) RCTs or prospective cohort studies; (2) The study population was patients with BPS fixation or UPS one after lumbar interbody fusion; (3) The intervention was UPS fixation, UPS fixation was also adopted for comparison; and (4) The primary outcomes were fusion rate and complications such as screw loosening, cage migration, infection, psoas, and neural symptoms. The secondary outcomes included changes in the following: Visual Analog Scale (VAS) score, Oswestry Disability Index (ODI) score, Japanese Orthopedic Association (JOA) score, operation time, total blood loss, as well as in-hospital duration. Exclusion criteria were: (1) No report on fusion rate or complication rate; (2) Study on recurrent lumbar diseases or revision surgeries; and (3) Repeated studies.
Two independent researchers searched the papers independently using the same search strategy, and a third researcher resolved any disagreement. Two reviewers collected the obtainable data from the involved studies independently, and any disagreement between the two reviewers was resolved by a third reviewer. Relevant data consist of names of the authors, dates of publication, types of intervention, ages, sample sizes, outcomes, follow-up duration, and types of reference. we obtained the outcome data, or estimated statistics via the data provided either in tables or in figures if we could not obtain the data directly from the statements of the articles. We present the baseline characteristics of the involved trials in Table 1.
| Ref. | Number of patients (n) | Gender (M/F) | Age (yr, mean ± SD) | Follow-up (mo) | Type of operation | Surgical segments | Reference type | ||||
| UPS | BPS | UPS | BPS | UPS | BPS | UPS | BPS | ||||
| Gu et al[13], 2015 | 35 | 39 | 17/18 | 21/18 | 64.5 ± 8.0 | 66.1 ± 7.1 | 32.1 ± 7.5 | 31.7 ± 8.0 | MI-TLIF | 2 | Prospective cohort |
| Shen et al[14], 2014 | 31 | 34 | 17/14 | 16/18 | 57.3 ± 11.7 | 58.9 ± 10.1 | 26.6 ± 4.5 | 26.6 ± 4.5 | MI-TLIF | 1 | RCT |
| Zhang et al[15], 2014 | 33 | 35 | 14/19 | 10/25 | 59.4 ± 10.2 | 55.7 ± 11.6 | 25.6 ± 4.5 | 25.6 ± 4.5 | TLIF | 2 | RCT |
| Dong et al[16], 2014 | 20 | 19 | 6/14 | 6/13 | 54.0 ± 12.3 | 56.6 ± 14.7 | 24 | 24 | PLIF | 1 | RCT |
| Chen et al[17], 2014 | 15 | 15 | 10/5 | 8/7 | 43.1 ± 5.8 | 44.9 ± 6.5 | 15.2 ± 3.25 | 15.2 ± 3.25 | MI-TLIF | NG | RCT |
| Gologorsky et al[18], 2014 | 40 | 40 | 19/21 | 21/19 | 41.6 | 46.9 | 52 ± 6.5 | 52 ± 6.5 | TLIF | 1 or 2 | Prospective |
| Lin et al[19], 2013 | 43 | 42 | 19/24 | 20/22 | 67 | 65.5 | 26 ± 3.5 | 26 ± 3.5 | MI-TLIF | 1 | RCT |
| Duncan et al[20], 2013 | 46 | 56 | 20/26 | 20/36 | 53.5 ± 14.75 | 55.7 ± 14 | 25.1 | 25.1 | TLIF | 1 or 2 | RCT |
| Dahdaleh et al[21], 2013 | 16 | 20 | 6/10 | 20/36 | 62.2 ± 13.1 | 57.3 ± 11.2 | 11.4 ± 6.1 | 12.4 ± 7.2 | MI-TLIF | 1 | RCT |
| Choi et al[22], 2013 | 26 | 27 | 12/14 | 9/18 | 53.39 ± 14.31 | 56.22 ± 12.62 | 27.52 ± 3.3 | 28.85 ± 4.37 | MI-TLIF | NG | RCT |
| Xie et al[23], 2012 | 56 | 52 | 32/24 | 28/24 | 56.2 ± 8 | 55 ± 8.5 | 36 ± 3 | 36 ± 3 | PLIF | 1 or 2 | RCT |
| Aoki et al[24], 2012 | 25 | 25 | 8/17 | 12/13 | 66.2 ± 8.3 | 65.6 ± 8.8 | 31 ± 3.25 | 31.2 ± 4.5 | TLIF | 1 | RCT |
| Xue et al[25], 2012 | 37 | 43 | 17/20 | 18/25 | 57.1 ± 8.1 | 58.2 ± 7.6 | 25.3 ± 3.5 | 25.3 ± 3.5 | TLIF | 1 or 2 | RCT |
| Feng et al[26], 2011 | 20 | 20 | 12/8 | 10/10 | 53.75 | 53.2 | 24 | 24 | TLIF | 1 | RCT |
| Fernández-Fairen et al[27], 2007 | 40 | 42 | 15/24 | 15/27 | 60.8 ± 5.33 | 61.42 ± 5.47 | 36 | 36 | PLIF | 1 or 2 | RCT |
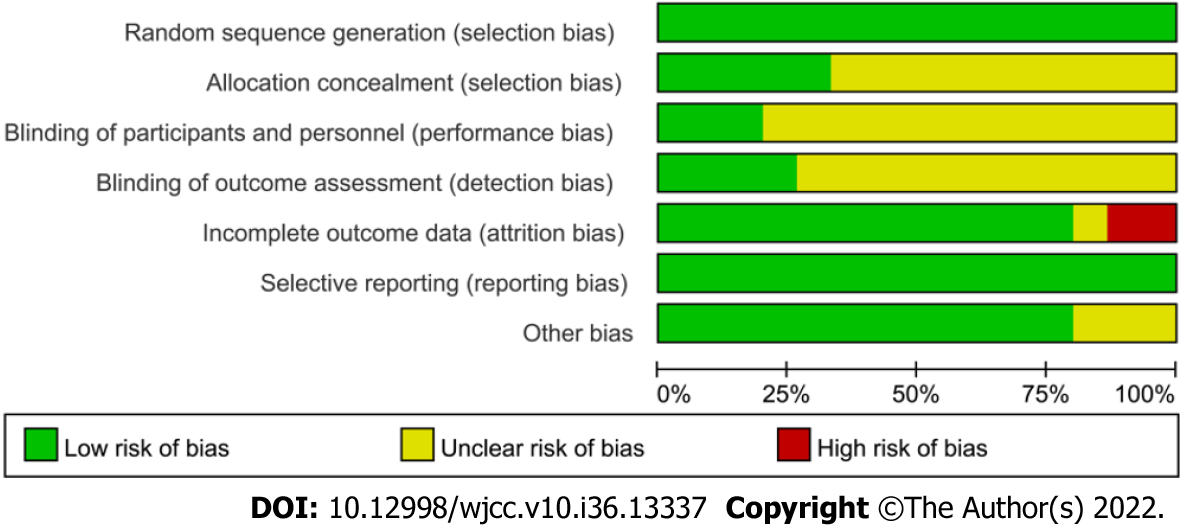
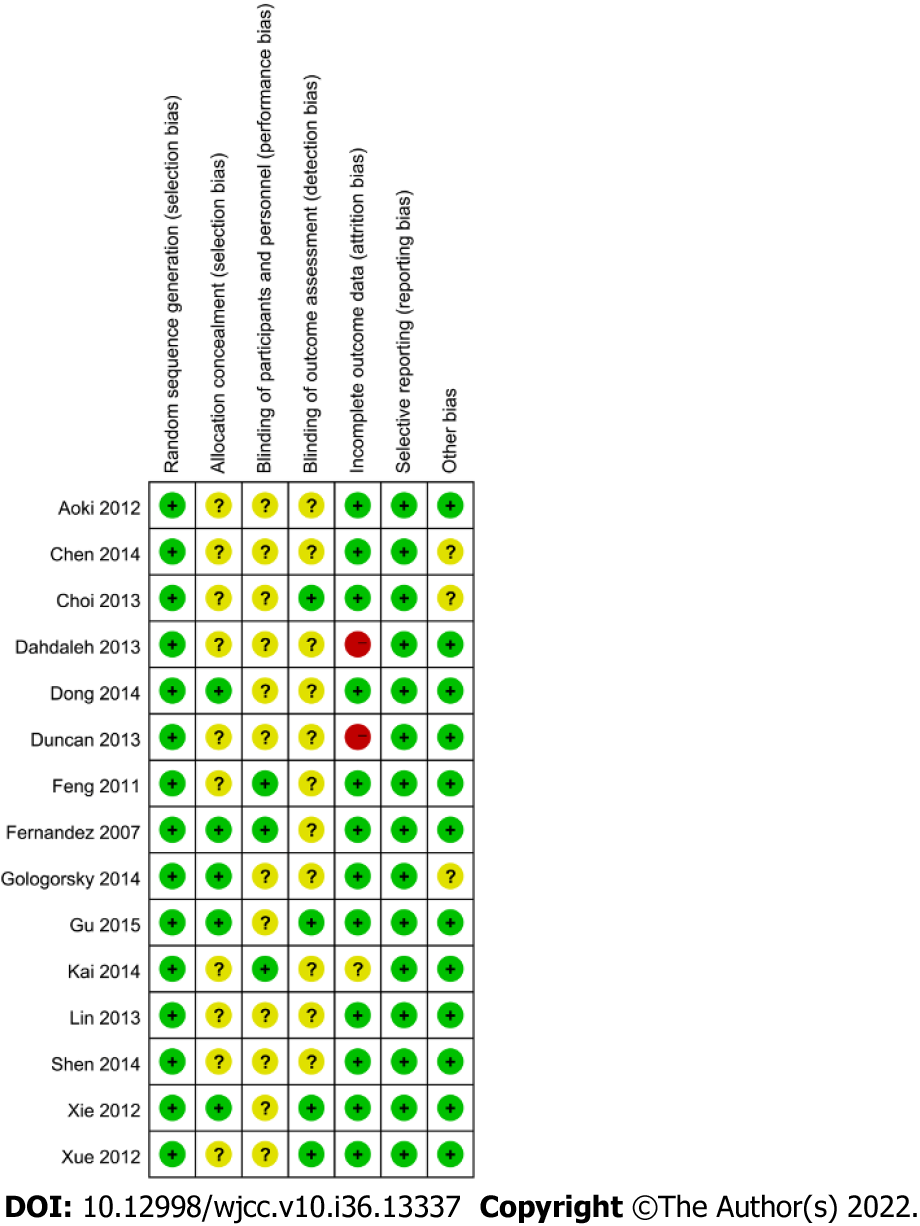
The methodological qualities and foundation of the involved studies were assessed in accordance with the Cochrane Handbook for Systematic Reviews of Interventions. Based on the included literature, the two researchers evaluated adequate sequence generation, allocation concealment, binding, selective reporting, and other bias as being at high, low, or unclear risks of bias. If there were any inconsistency, the third researcher would be consulted to deal with it (Figures 2 and 3).
The GRADE software has been used to conduct evaluation on the convincing level of evidence and strength of recommendations for the involved outcomes. Initially, RCTs were considered to have high confidence, and cohort studies low confidence as for the estimate of effect. Factors which may have decreased the level of confidence level included inconsistency, limitations, imprecision, indirectness, as well as publication bias. Factors that may have raised confidence level consisted of plausible confounding, large effect and dose-response. We present the results of GRADE analysis in Table 2.
| No of studies | Design | Decrease quality of evidence | Increase quality of evidence | Quality | Importance | ||||||
| Limitations | Inconsistency | Indirectness | Imprecision | Publication bias | Large effect | Plausible confounding | Does-response | ||||
| Fusion rate | RCT | No | No | No | No | Unlikely | No | No | No | High (++++) | Critical |
| Complications | RCT | No | No | No | Serious | Very likely | No | No | No | Very low (+---) | Critical |
| -Δ VAS | RCT | No | Serious | No | No | Likely | No | No | No | Low (++--) | Important |
| Δ ODI | RCT | No | Serious | No | No | Likely | No | No | No | Low (++--) | Important |
| Δ JOA | RCT | No | Serious | No | No | Unlikely | No | No | No | Moderate (+++-) | Important |
| Total blood loss | RCT | No | Serious | No | No | Very likely | No | No | No | Very low (+---) | Important |
| Operation time | RCT | No | Serious | No | No | Unlikely | No | No | No | Moderate (+++-) | Important |
| Length of hospital stay | RCT | No | Serious | No | No | Very likely | No | No | No | Very low (+---) | Important |
Meta-analyses have been conducted using RevMan 5.3 software and STATA 13.1. The Standard Mean Difference (SMD) has been applied to make assessment of consecutive outcomes, with 95% Confidence Interval (CI). Relative Risk (RR) with 95%CI was adopted to make assessments of the dichotomous outcomes. The inverse variance, Mantel-Haenszel, and DerSimonian-Laird approaches have been applied to make combination of separated statistics. The results have been considered statistically important at P values < 0.05.
Heterogeneity out of studies has undergone evaluation viaI2 values and and considered high if I2 ≥ 50% or low if I2 < 50%, respectively. An fixed-effects model was adopted when I2 ≥ 50%, whereas an effect model of random type was used when I2 < 50%. Subgroup analyses and sensitivity analysis ones have been conducted to figure out the heterogeneity source, while I2 ≥ 50%. Stata13.1 adopted for evaluation of the publication bias.
According to the index words, 314 citations were identified from the electronic databases. A total of 130 citations were duplicated, and 143 citations were excluded from the title and abstract, such as irrelevant articles, reviews, and case reports. Additionally, 26 retrospective studies were excluded from the analysis. Ultimately, 15 RCTs were included[13-27]. However, the limitation is that not every study included contains every outcome of interest. We summarized the characteristics of the involved studies and presented in Table 1.
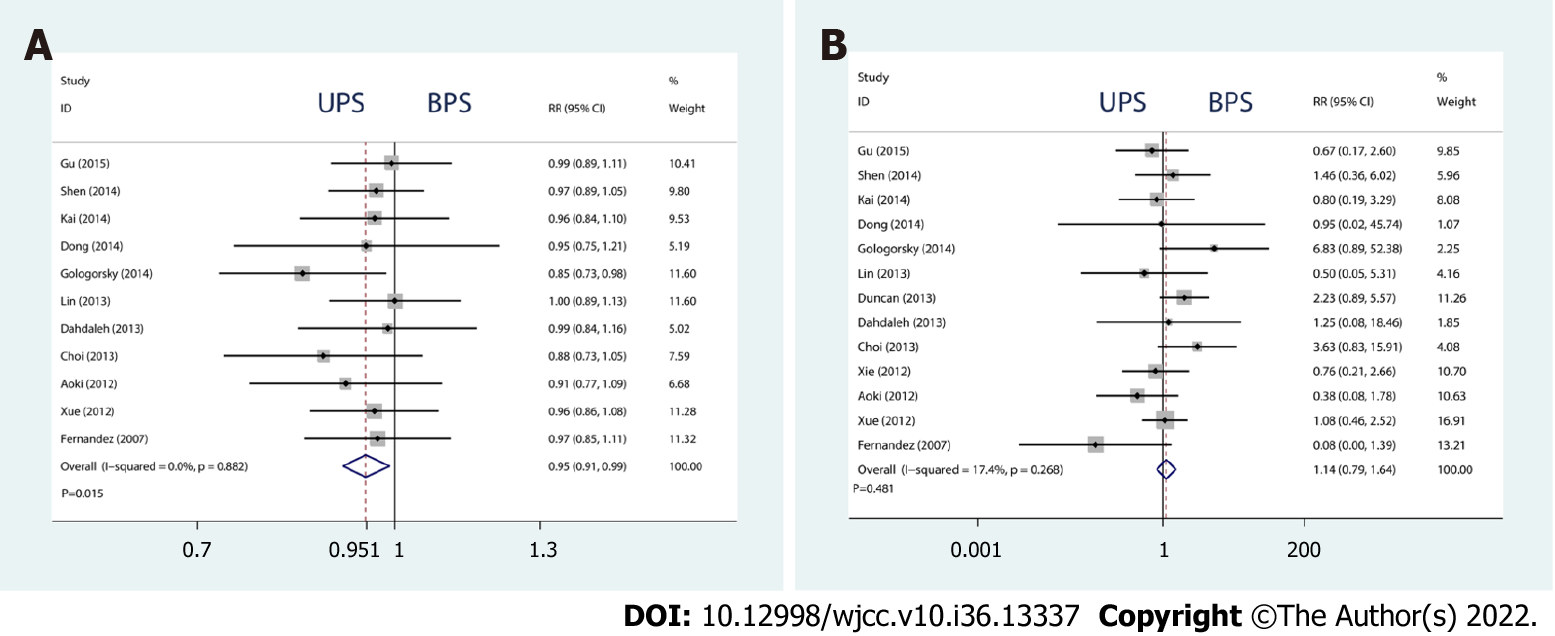
The complications and fusion rate of the two internal fixations were the primary outcomes from the meta-analysis, used for evaluating efficacy and safety.
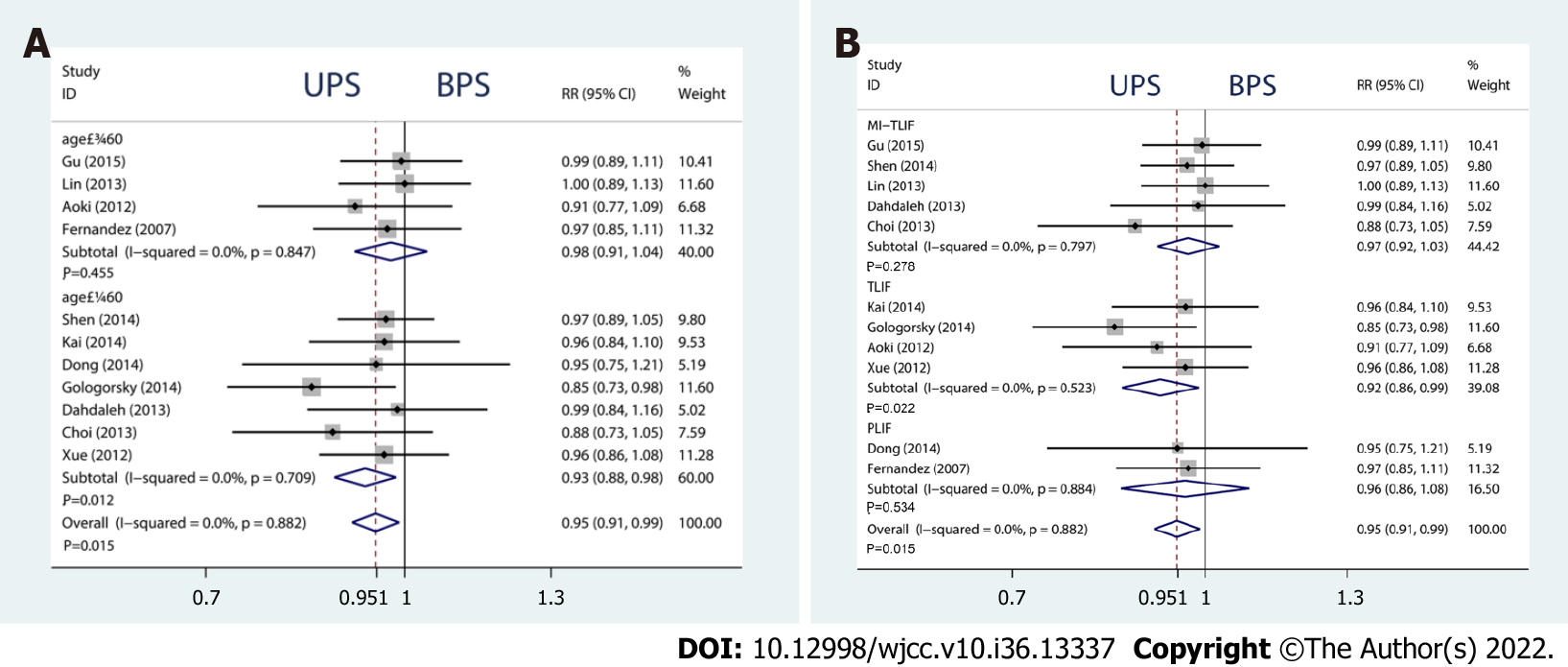
Eleven studies assessed the fusion rate of 708 patients followed up for at least 12 mo. Compared with BPS, UPS had a slightly lower fusion rate (RR = 0.949, 95%CI: 0.910 to 0.990, P = 0.015, Figure 4A). The age subgroup analysis indicated that the significant difference disappeared in patients aged > 60 years (RR = 0.975, 95%CI: 0.914 to 1.041, P = 0.455, Figure 5A). The type of operation subgroup analysis showed that TLIP significantly reduced the fusion rate of the UPS (SMD = 0.921, 95%CI: 0.857 to 0.988, P = 0.022, Figure 5B).
Thirteen studies assessed the fusion cage migration rate of 918 patients followed up for at least 12 mo. No drastic difference has been observed between both internal fixation approaches (RR = 1.140, 95%CI: 0.792 to 1.640, P = 0.481, Figure 4B).
The enhancements in VAS, JOA, and ODI scores were considered subjective. To some extent, operation, blood loss, as well as in-hospital duration depended upon the surgeon’s proficiency. Therefore, these outcomes are secondary but essential indicators of prognosis in clinical practice.
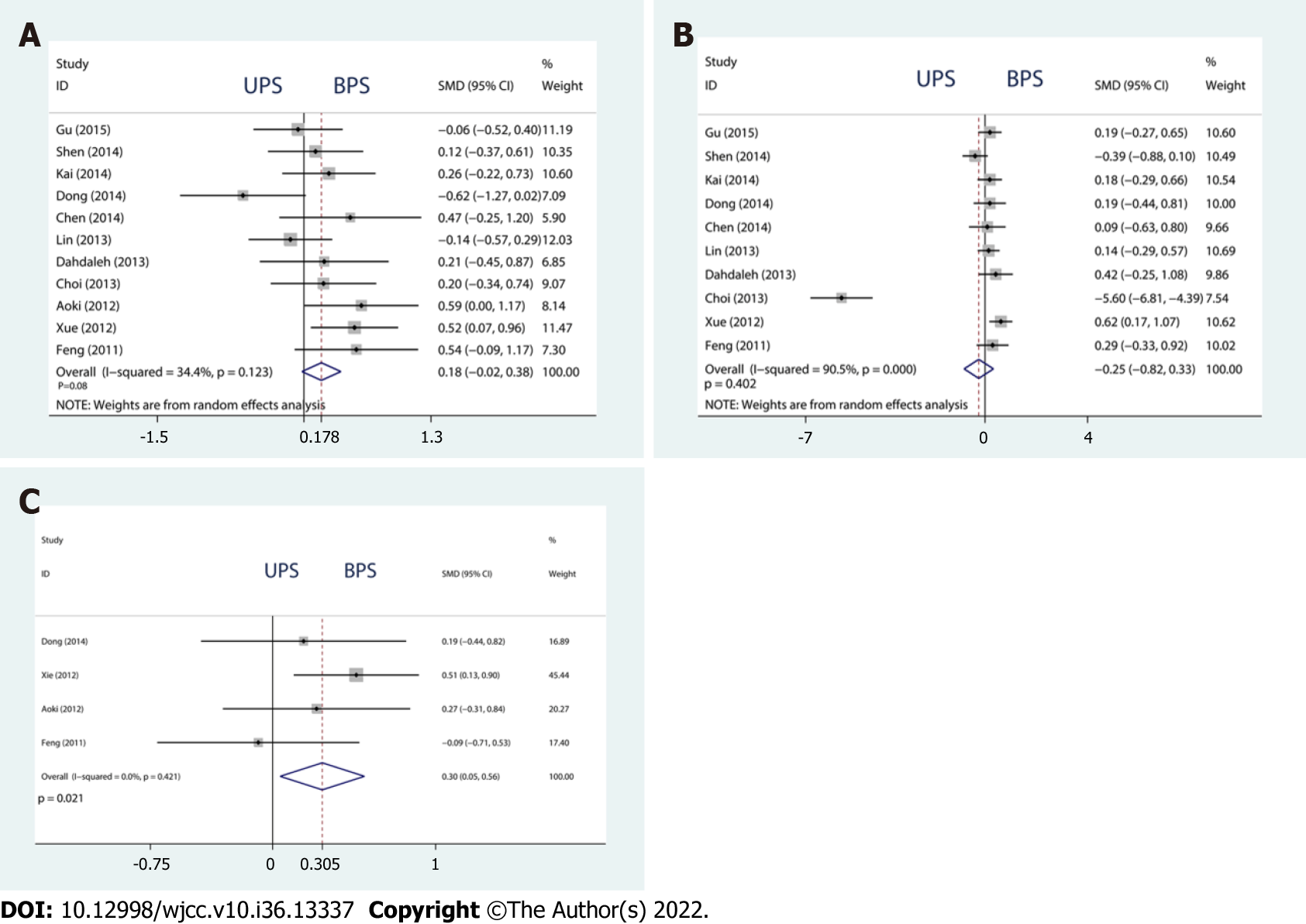
Improvement of VAS, ODI and JOA: There was no significant difference in ΔVAS or ΔODI (ΔVAS, SMD = 0.178, 95%CI: -0.021 to 0.378, P = 0.080; ΔODI, SMD = -0.254, 95%CI: -0.820 to 0.329, P = 0.402, Figure 6A and B). However, compared with BPS, UPS significantly improved ΔJOA (SMD = 0.305, 95%CI: 0.046 to 0.563, P = 0.021, Figure 6C).
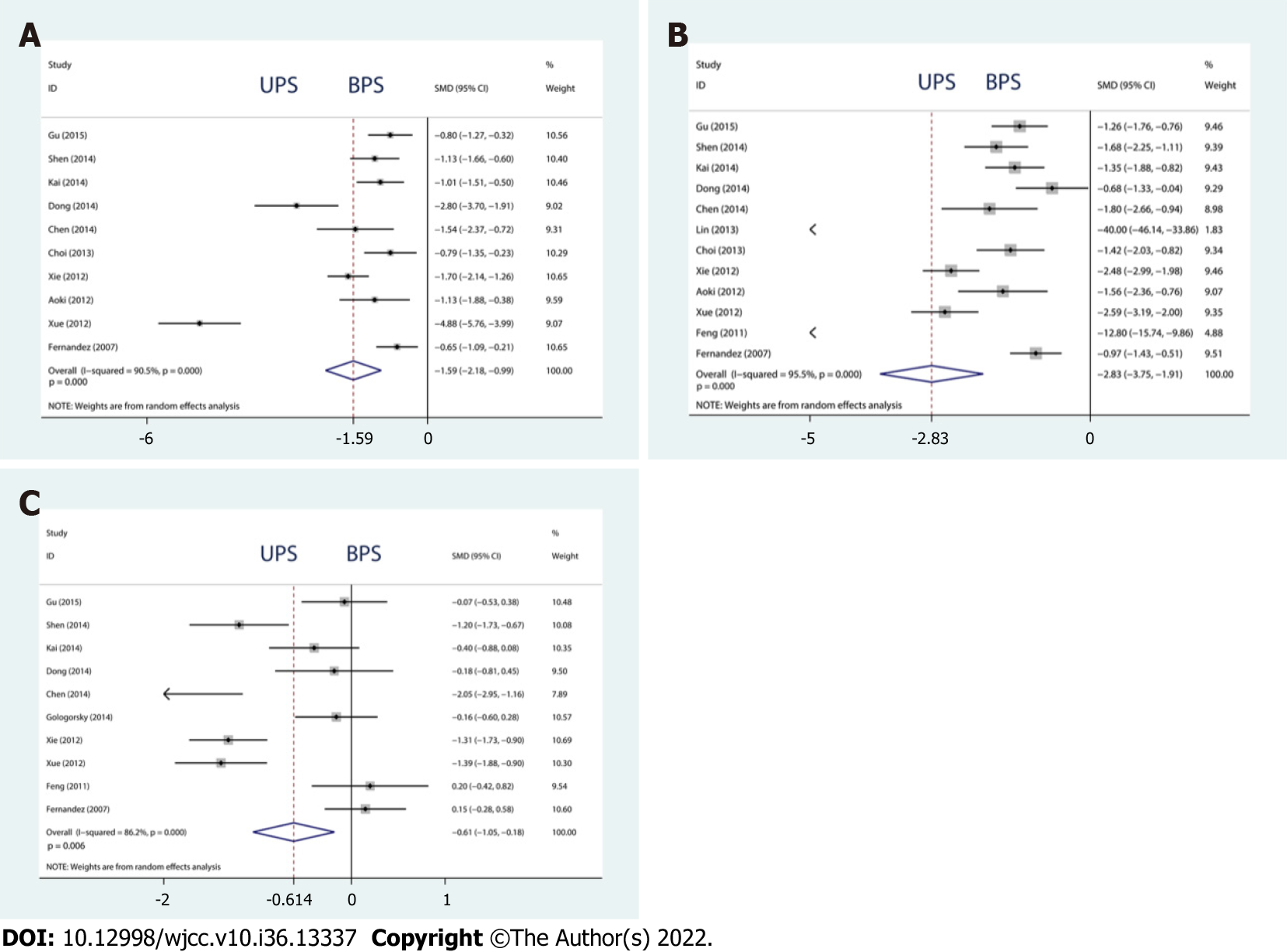
Total blood loss, operation time, as well as in-hospital duration: Compared with BPS, UPS significantly reduced the total blood loss, operation time, and length of hospital stay (total blood loss, SMD = -1.586, 95%CI: -2.182 to -0.990, P = 0.000; operation time, SMD = -2.831, 95%CI: -3.753 to -1.909, P = 0.000; length of hospital stay, SMD = -0.614, 95%CI: -1.050 to -0.179, P = 0.006, Figure 7A-C).
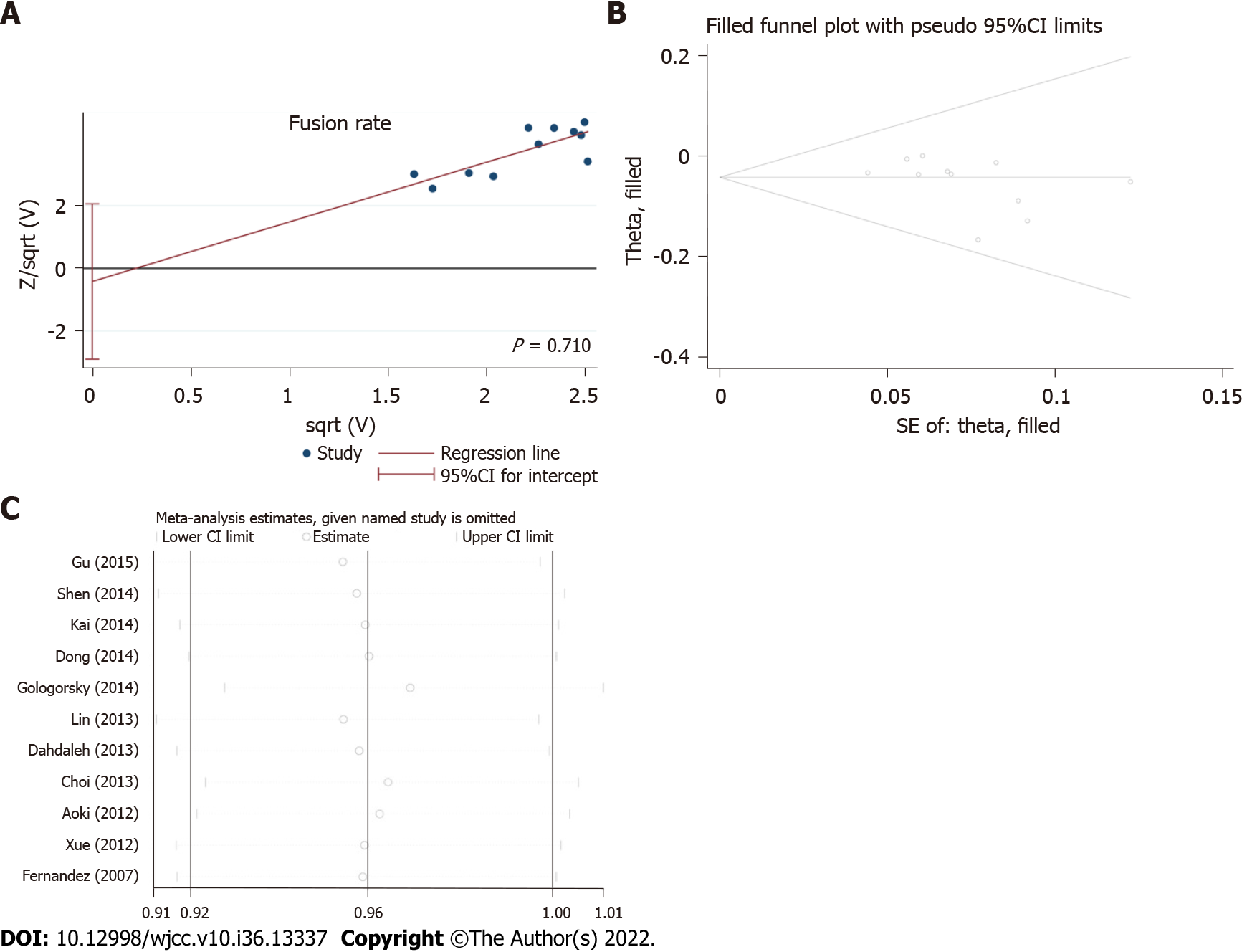
We present baseline characteristics of the involved trials in Table 1, and results of GRADE analysis are presented in Table 2. The included studies met the principles of randomized controlled trials with a high level of evidence (Figures 2 and 3). Given medical ethics and patients’ informed consent rights, these RCTs rarely mention whether to adopt allocation concealment and blind methods, especially single-blind methods. We used the Harbord method and considered that no significant publication bias has been observed in the fusion rate (P = 0.710, Figure 8A). We conducted a sensitivity analysis with metatrim and metaninf and considered the included studies to be steady (Figure 8B and C).
This study suggested that UPS had a poorer fusion rate but significantly improved prognosis regarding several clinical outcomes.
However, the choice between unilateral and BPS fixation after lumbar fusion remains controversial. The BPS provides greater immediate stability, and the UPS significantly decreases the stiffness of the instrumented segment and surgical trauma. In recent years, many clinical follow-up studies and human cadaver studies have shown that UPS is as effective as BPS, and that UPS can achieve biomechanical stability comparable to that of BPS[28-32]. Computer simulation studies, such as finite element studies, also support UPS[33].
However, there are some objections to this approach. Kasai reported that UPS offers only uneven fixation in a human cadaver study, whereas BPS may allow excellent fixation in all directions[34]. Schleicher performed stiffness testing in fresh-frozen human cadaveric lumbar spine motion segments and concluded that BPS offers significantly more stability than UPS in the majority of test modes[35]. Many studies have found no significant difference in only one- or two-level interbody fusion[36]. Our study shows that there is a slightly lower fusion rate in UPS, even with short-segment fixation, which is different from those reported previously[37,38]. In terms of the rate of fusion cage migration, previous studies have found that UPS generates more cage migration than BPS[39]. After synthesizing the newly published studies, our evidence shows no difference in the rate of fusion cage migration between UPS and BPS. In terms of Improvement of VAS, ODI and JOA, there was no difference between UPS and BPS, which was consistent with the conclusion of previous studies[39]. In terms of total blood loss, operation time, and the length of hospital stay, UPS was lower than BPS, which was consistent with the actual clinical situation. Unilateral PS fixation avoided contralateral exposure and reduced trauma. Therefore, UPS fixation can not only shorten the operation time and reduce surgical trauma, but also reduce the recovery time[40]. GRADE is one of the widely adopted approaches in industries of public health and medicine to make assessment of the evidence’s outcome-specific certainty through systematically conducted reviews[41]. Our results show that the level of evidence is high. Therefore, we believe that this is the main contribution of the present meta-analysis. Although UPS has many advantages, BPS is much preferred, assuming there isn’t sufficient stability, such as during long segment fixation. However, current data only provide weak support, if any, favoring BPS over UPS for clinical improvement in fusion rates.
Within aging populations, there is a significant increase in lumbar degenerative diseases (LDD), resulting in great pain and reduced quality of life for patients[42]. Early increase of fusion rate and relief of pain, so that patients can move early, can effectively reduce venous thrombosis, pulmonary infection, pressure sores, and other complications[7,43]. Shortening hospital stay and reducing nosocomial infections are particularly important for the recovery of elderly patients[44]. Thus, it is urgently demanded to explore feasible, secure, and effective treatments for LDD.
Our study also has some limitations. First, all studies were single-center studies with small sizes of samples, which could possibly bring about selection bias. Second, none of the RCTs included in this study used blinding methods. Because of the type of intervention, blinding could not be performed to prevent the placebo effect or observer bias, resulting in low quality of the methodology. Third, different studies had different follow-up times, and the follow-up time of some studies was short. Finally, differences in diagnostic criteria, inclusion and exclusion criteria and details of treatment resulted in heterogeneity in the meta-analysis. Although subgroup and sensitivity analyses have been conducted, confounding statistical outcomes resulted from heterogeneity cannot be excluded to a complete extent.
According to our meta-analysis, UPS had a slightly poorer fusion rate but significantly improved prognosis regarding many important clinical outcomes, possibly associated with minimal invasion. To clarify whether UPS has the same reliability and effectiveness as BPS, longer follow-up and more clinical trials, especially RCTs, are required to provide stronger evidence regarding this observation. Further multicenter studies with more patients are required to obtain more reliable results.
The use of unilateral pedicle screw (UPS) or bilateral pedicle screw (BPS) fixation for lumbar degenerative diseases remains controversial.
To provide objective evidence for the selection of UPS or BPS fixation for lumbar degenerative diseases.
To compare the efficacy and safety of UPS and BPS fixation in patients with lumbar degenerative diseases.
We used meta-analysis to systematically review the current evidence.
UPS had slightly lower effects on fusion rate, which was the main contribution of this meta-analysis, and similar complication rates, Δ visual analog scale, and Δ Oswestry disability index. In contrast, there was a significant difference in Δ Japanese Orthopedic Association (JOA) score, total blood loss, operation time, and length of hospital stay.
Unilateral fixation is less effective than bilateral fixation regarding fusion rate after lumbar interbody fusion. However, JOA, total blood loss, operation time, and length of stay were improved for unilateral fixation.
To clarify whether UPS has the same reliability and effectiveness as BPS, longer follow-up and more clinical trials, especially RCTs, are required to provide stronger evidence regarding this observation. Further multicenter studies with more patients are required to obtain more reliable results.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Chhabra HS, India; Chrcanovic BR, Sweden S-Editor: Zhang H L-Editor: A P-Editor: Zhang H
| 1. | Hibbs RA. An operation for progressive spinal deformities: a preliminary report of three cases from the service of the orthopaedic hospital. 1911. Clin Orthop Relat Res. 2007;460:17-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 58] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 2. | Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015;1:2-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 455] [Reference Citation Analysis (0)] |
| 3. | Li HM, Zhang RJ, Shen CL. Differences in radiographic and clinical outcomes of oblique lateral interbody fusion and lateral lumbar interbody fusion for degenerative lumbar disease: a meta-analysis. BMC Musculoskelet Disord. 2019;20:582. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Cho JY, Goh TS, Son SM, Kim DS, Lee JS. Comparison of Anterior Approach and Posterior Approach to Instrumented Interbody Fusion for Spondylolisthesis: A Meta-analysis. World Neurosurg. 2019;129:e286-e293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 5. | Levin JM, Tanenbaum JE, Steinmetz MP, Mroz TE, Overley SC. Posterolateral fusion (PLF) versus transforaminal lumbar interbody fusion (TLIF) for spondylolisthesis: a systematic review and meta-analysis. Spine J. 2018;18:1088-1098. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 64] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 6. | Virk SS, Niedermeier S, Yu E, Khan SN. Adjacent segment disease. Orthopedics. 2014;37:547-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 115] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 7. | Wen J, Shi C, Yu L, Wang S, Xi Y, Ye X. Unilateral Versus Bilateral Percutaneous Pedicle Screw Fixation in Oblique Lumbar Interbody Fusion. World Neurosurg. 2020;134:e920-e927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Yuan C, Chen K, Zhang H, He S. Unilateral versus bilateral pedicle screw fixation in lumbar interbody fusion: a meta-analysis of complication and fusion rate. Clin Neurol Neurosurg. 2014;117:28-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Hu XQ, Wu XL, Xu C, Zheng XH, Jin YL, Wu LJ, Wang XY, Xu HZ, Tian NF. A systematic review and meta-analysis of unilateral versus bilateral pedicle screw fixation in transforaminal lumbar interbody fusion. PLoS One. 2014;9:e87501. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9207] [Cited by in RCA: 8006] [Article Influence: 533.7] [Reference Citation Analysis (2)] |
| 11. | Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ; GRADE Working Group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924-926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11058] [Cited by in RCA: 14749] [Article Influence: 867.6] [Reference Citation Analysis (0)] |
| 12. | Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, Thomas J. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:ED000142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1361] [Cited by in RCA: 2846] [Article Influence: 474.3] [Reference Citation Analysis (0)] |
| 13. | Gu G, Zhang H, Fan G, He S, Meng X, Gu X, Yan N, Guan X. Clinical and radiological outcomes of unilateral versus bilateral instrumentation in two-level degenerative lumbar diseases. Eur Spine J. 2015;24:1640-1648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 14. | Shen X, Zhang H, Gu X, Gu G, Zhou X, He S. Unilateral versus bilateral pedicle screw instrumentation for single-level minimally invasive transforaminal lumbar interbody fusion. J Clin Neurosci. 2014;21:1612-1616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 15. | Zhang K, Sun W, Zhao CQ, Li H, Ding W, Xie YZ, Sun XJ, Zhao J. Unilateral versus bilateral instrumented transforaminal lumbar interbody fusion in two-level degenerative lumbar disorders: a prospective randomised study. Int Orthop. 2014;38:111-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Dong J, Rong L, Feng F, Liu B, Xu Y, Wang Q, Chen R, Xie P. Unilateral pedicle screw fixation through a tubular retractor via the Wiltse approach compared with conventional bilateral pedicle screw fixation for single-segment degenerative lumbar instability: a prospective randomized study. J Neurosurg Spine. 2014;20:53-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 17. | Chen X, Wu C, Lin H, Zhang G, Li R. Short-term effect of unilateral pedicle screw fixed intervertebral fusion in treatment of degenerative disc disease via MAST QUADRANT minimally invasive system. Cell Biochem Biophys. 2014;70:195-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 18. | Gologorsky Y, Skovrlj B, Steinberger J, Moore M, Arginteanu M, Moore F, Steinberger A. Increased incidence of pseudarthrosis after unilateral instrumented transforaminal lumbar interbody fusion in patients with lumbar spondylosis: Clinical article. J Neurosurg Spine. 2014;21:601-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Lin B, Xu Y, He Y, Zhang B, Lin Q, He M. Minimally invasive unilateral pedicle screw fixation and lumbar interbody fusion for the treatment of lumbar degenerative disease. Orthopedics. 2013;36:e1071-e1076. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Duncan JW, Bailey RA. An analysis of fusion cage migration in unilateral and bilateral fixation with transforaminal lumbar interbody fusion. Eur Spine J. 2013;22:439-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 65] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 21. | Dahdaleh NS, Nixon AT, Lawton CD, Wong AP, Smith ZA, Fessler RG. Outcome following unilateral versus bilateral instrumentation in patients undergoing minimally invasive transforaminal lumbar interbody fusion: a single-center randomized prospective study. Neurosurg Focus. 2013;35:E13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 22. | Choi UY, Park JY, Kim KH, Kuh SU, Chin DK, Kim KS, Cho YE. Unilateral versus bilateral percutaneous pedicle screw fixation in minimally invasive transforaminal lumbar interbody fusion. Neurosurg Focus. 2013;35:E11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 52] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 23. | Xie Y, Ma H, Li H, Ding W, Zhao C, Zhang P, Zhao J. Comparative study of unilateral and bilateral pedicle screw fixation in posterior lumbar interbody fusion. Orthopedics. 2012;35:e1517-e1523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 24. | Aoki Y, Yamagata M, Ikeda Y, Nakajima F, Ohtori S, Nakagawa K, Nakajima A, Toyone T, Orita S, Takahashi K. A prospective randomized controlled study comparing transforaminal lumbar interbody fusion techniques for degenerative spondylolisthesis: unilateral pedicle screw and 1 cage versus bilateral pedicle screws and 2 cages. J Neurosurg Spine. 2012;17:153-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 64] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 25. | Xue H, Tu Y, Cai M. Comparison of unilateral versus bilateral instrumented transforaminal lumbar interbody fusion in degenerative lumbar diseases. Spine J. 2012;12:209-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 94] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 26. | Feng ZZ, Cao YW, Jiang C, Jiang XX. Short-term outcome of bilateral decompression via a unilateral paramedian approach for transforaminal lumbar interbody fusion with unilateral pedicle screw fixation. Orthopedics. 2011;34:364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 27. | Fernández-Fairen M, Sala P, Ramírez H, Gil J. A prospective randomized study of unilateral versus bilateral instrumented posterolateral lumbar fusion in degenerative spondylolisthesis. Spine (Phila Pa 1976). 2007;32:395-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 79] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 28. | Hu Y, Zhu BK, Kepler CK, Yuan ZS, Dong WX, Sun XY. A Comparison Study of Three Posterior Fixation Strategies in Transforaminal Lumbar Interbody Fusion Lumbar for the Treatment of Degenerative Diseases. Indian J Orthop. 2019;53:542-547. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 29. | Chen DJ, Yao C, Song Q, Tang B, Liu X, Zhang B, Dai M, Nie T, Wan Z. Unilateral versus Bilateral Pedicle Screw Fixation Combined with Transforaminal Lumbar Interbody Fusion for the Treatment of Low Lumbar Degenerative Disc Diseases: Analysis of Clinical and Radiographic Results. World Neurosurg. 2018;115:e516-e522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 30. | Liu F, Feng Z, Zhou X, Liang Y, Jiang C, Li X, Li Z, Jiang X, Dong J. Unilateral Versus Bilateral Pedicle Screw Fixation in Transforaminal Lumbar Interbody Fusion: A Monocentric Study of 215 Patients With a Minimum of 4-Year Follow-up. Clin Spine Surg. 2017;30:E776-E783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 31. | Işik HS, Okutan Ö, Yildirim T, Akpinar E, Yilmaz A. Comparison of Unilateral versus Bilateral Pedicle Screw Fixation in Transforaminal Lumbar Interbody Fusion for Single Level Lumbar Degenerative Diseases and Review of Literature. Turk Neurosurg. 2017;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Reference Citation Analysis (0)] |
| 32. | Godzik J, Martinez-Del-Campo E, Newcomb AGUS, Reis MT, Perez-Orribo L, Whiting AC, Singh V, Kelly BP, Crawford NR. Biomechanical Stability Afforded by Unilateral Versus Bilateral Pedicle Screw Fixation with and without Interbody Support Using Lateral Lumbar Interbody Fusion. World Neurosurg. 2018;113:e439-e445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 33. | Li J, Wang W, Zuo R, Zhou Y. Biomechanical Stability Before and After Graft Fusion with Unilateral and Bilateral Pedicle Screw Fixation: Finite Element Study. World Neurosurg. 2019;123:e228-e234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 34. | Kasai Y, Inaba T, Kato T, Matsumura Y, Akeda K, Uchida A. Biomechanical study of the lumbar spine using a unilateral pedicle screw fixation system. J Clin Neurosci. 2010;17:364-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 35. | Schleicher P, Beth P, Ottenbacher A, Pflugmacher R, Scholz M, Schnake KJ, Haas NP, Kandziora F. Biomechanical evaluation of different asymmetrical posterior stabilization methods for minimally invasive transforaminal lumbar interbody fusion. J Neurosurg Spine. 2008;9:363-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 36. | Yücesoy K, Yüksel KZ, Baek S, Sonntag VK, Crawford NR. Biomechanics of unilateral compared with bilateral lumbar pedicle screw fixation for stabilization of unilateral vertebral disease. J Neurosurg Spine. 2008;8:44-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 52] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 37. | Lu P, Pan T, Dai T, Chen G, Shi KQ. Is unilateral pedicle screw fixation superior than bilateral pedicle screw fixation for lumbar degenerative diseases: a meta-analysis. J Orthop Surg Res. 2018;13:296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 38. | Liu H, Xu Y, Yang SD, Wang T, Wang H, Liu FY, Ding WY. Unilateral versus bilateral pedicle screw fixation with posterior lumbar interbody fusion for lumbar degenerative diseases: A meta-analysis. Medicine (Baltimore). 2017;96:e6882. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 39. | Ren C, Qin R, Sun P, Wang P. Effectiveness and safety of unilateral pedicle screw fixation in transforaminal lumbar interbody fusion (TLIF): a systematic review and meta-analysis. Arch Orthop Trauma Surg. 2017;137:441-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 40. | Iwatsuki K, Yoshimine T, Aoki M. Bilateral interlaminar fenestration and unroofing for the decompression of nerve roots by using a unilateral approach in lumbar canal stenosis. Surg Neurol. 2007;68:487-92; discussion 492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 41. | Schwingshackl L, Rüschemeyer G, Meerpohl JJ. [How to interpret the certainty of evidence based on GRADE (Grading of Recommendations, Assessment, Development and Evaluation)]. Urologe A. 2021;60:444-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 42. | Aoki Y, Takahashi H, Nakajima A, Kubota G, Watanabe A, Nakajima T, Eguchi Y, Orita S, Fukuchi H, Yanagawa N, Nakagawa K, Ohtori S. Prevalence of lumbar spondylolysis and spondylolisthesis in patients with degenerative spinal disease. Sci Rep. 2020;10:6739. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 56] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 43. | Zeng ZY, Wu HF. Research progression on unilateral pedicle screw combined with contralateral translaminar facet screw fixation and interbody fusion. J Spinal Surg. 2022;20:279-282, 285. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 44. | Umarji SI, Lankester BJ, Prothero D, Bannister GC. Recovery after hip fracture. Injury. 2006;37:712-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |