Published online Dec 6, 2022. doi: 10.12998/wjcc.v10.i34.12717
Peer-review started: August 29, 2022
First decision: September 26, 2022
Revised: October 5, 2022
Accepted: October 31, 2022
Article in press: October 31, 2022
Published online: December 6, 2022
Processing time: 93 Days and 4.2 Hours
Tension pneumoperitonium is a rare complication during bronchoscopy that can cause acute respiratory and hemodynamic failure, with fatal consequences. Isolated pneumoperitonium during bronchoscopy usually results from ruptures of the abdominal viscera that need surgical repair. Non-surgical pneumoperitoneum (NSP) refers to some pneumoperitoneum that could be relieved without surgery and only by conservative therapy. However, the clinical experience of managing tension pneumoperitonium during bronchoscopy is limited and controversial.
A 51-year-old female was admitted to our hospital for cough with bloody sputum of seven days. On the 8th day of her admission, a bronchoscopy was arranged for bronchial-alveolar lavage to detect possible pathogens in the lower respiratory tract, as oxygen was delivered via a 12 F nasopharyngeal cannula, approximately 5-6 cm from the tip of the catheter, with a flow rate of 5-10 L/min. After four minutes of bronchoscopy, the patient suddenly vomited 20 mL of water, followed by severe abdominal pain, while physical examination revealed obvious abdominal distension, as well as hardness and tenderness of the whole abdomen, which was considered pneumoperitonium, and the bronchoscopy was terminated immediately. A computer tomography scan indicated isolated tension pneumoperitonium, and abdominal decompression was performed with a drainage tube, after which her symptoms were relieved. A multidisciplinary expert consultation discussed her situation and a laparotomy was suggested, but finally refused by her family. She had no signs of peritonitis and was finally discharged 5 d after bronchoscopy with a good recovery.
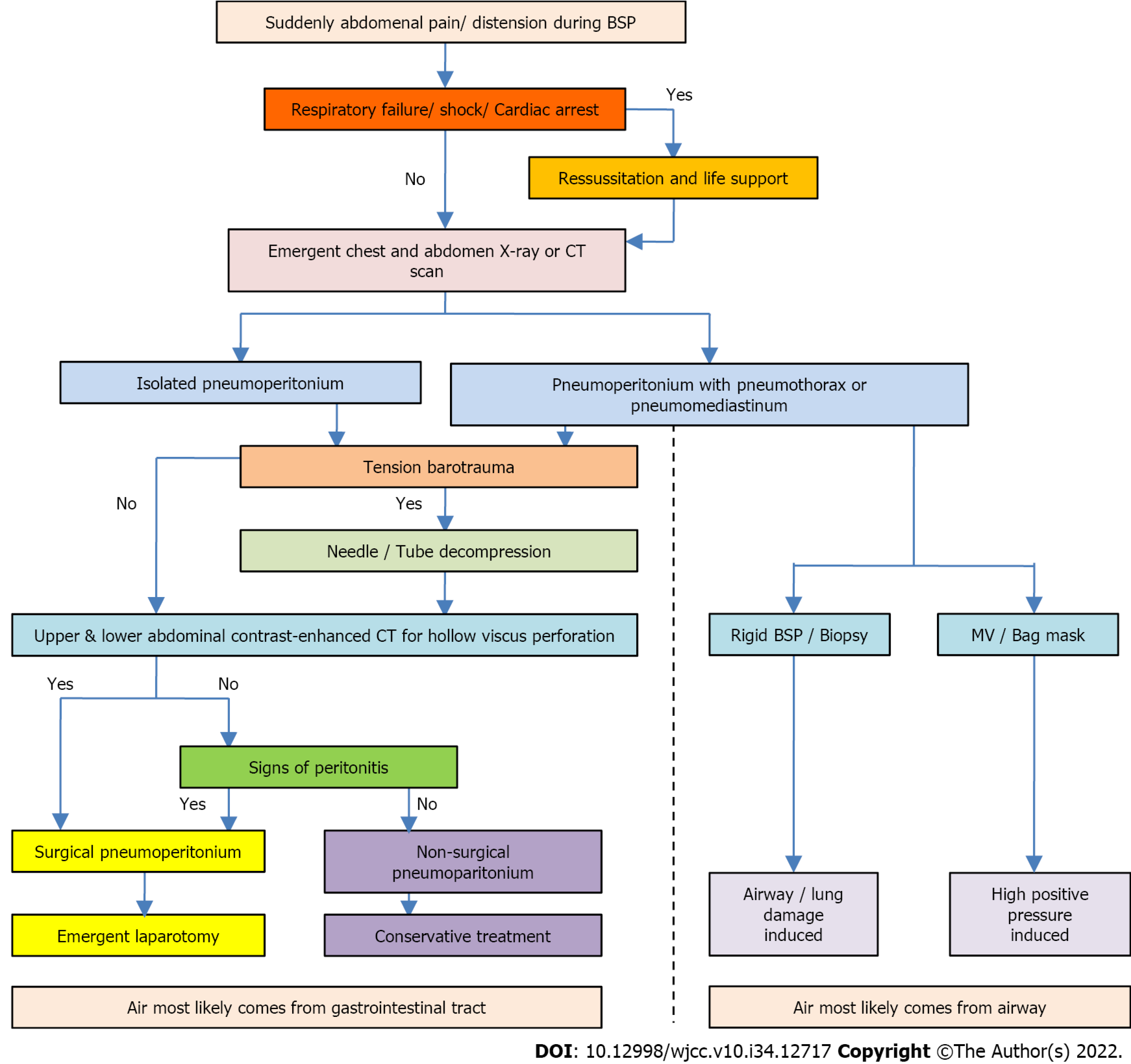
The possibility of tension pneumoperitonium during bronchoscopy should be guarded against, and given its serious clinical consequences, cardiopulmonary instability should be treated immediately. Varied strategies could be adopted according to whether it is complicated with pneumothorax or pneumomediastinum, and the presence of peritonitis. When considering NSP, conservative therapy maybe a reasonable option with good recovery. An algorithm for the management of pneumoperitonium during bronchoscopy is proposed, based on the features of the case series reviewed and our case reported.
Core Tip: Tension pneumoperitonium is a rare complication during bronchoscopy that can cause serious consequences. Isolated pneumoperitonium during bronchoscopy usually results from ruptures of the abdominal viscera that need surgical repair. Nonsurgical pneumoperitoneum (NSP) refers to some pneumoperitonium that could be relieved without surgery and only by conservative therapy. However, the clinical experience of managing tension pneumoperitonium during bronchoscopy is limited and controversial. Herein, we describe a rare case of isolated tension pneumoperitonium during bronchoscopy, which was recovered with no signs of peritonitis by conservative therapy. An algorithm for the management of pneumoperitonium during bronchoscopy is proposed.
- Citation: Baima YJ, Shi DD, Shi XY, Yang L, Zhang YT, Xiao BS, Wang HY, He HY. How to manage isolated tension non-surgical pneumoperitonium during bronchoscopy? A case report . World J Clin Cases 2022; 10(34): 12717-12725
- URL: https://www.wjgnet.com/2307-8960/full/v10/i34/12717.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i34.12717
Pneumoperitonium is a rare complication during bronchoscopy[1,2]. Tension pneumoperitonium may cause acute respiratory and hemodynamic failure[1,2], and can give rise to fatal consequences[3,4]. When pneumoperitonium is complicated with pneumothorax or pneumomediastinum, it is usually due to high positive pressure ventilation or airway/alveolar rupture[2,5]. Isolated pneumoperitonium during bronchoscopy is usually caused by ruptures of the abdominal viscera that need surgical repair[3,6]. Some pneumoperitonium could be relieved without surgery and only by conservative therapy, which is known as non-surgical pneumoperitoneum (NSP)[6]. When tension pneumoperitonium occurs during bronchoscopy, prompt diagnosis and life support should be performed, and whether it is an NSP should be confirmed, which may help the patient avoid surgical procedures and get a good recovery with conservative treatment[7]. However, given the limited and controversial clinical experience in the management of tension pneumoperitonium during bronchoscopy, we recount a rare case of isolated tension pneumoperitonium during bronchoscopy that was relieved by conservative therapy.
A 51-year-old female was admitted to our hospital for cough with bloody sputum of seven days.
A 51-year-old female was admitted to our hospital for cough with bloody sputum for 7 d, with chest pain, dyspnea after exercise, and with no fever.
Her past medical history includes right knee arthroplasty one month before admission, and tubal ligation for twenty-seven years.
She had no trauma history, no other special diseases, or family genetic history.
Vital signs at admission: Temperature 36.3 ℃, Pulse 98 bpm, respiratory rate (RR) 20 bpm, blood pressure (BP) 131/96 mmHg, pulse oxygen saturation (SPO2) 81% (at room air), body mass index 28. She was alert, with moist rales in both lower lobe.
At admission, her C reactive protein was 189.66 mg/L, Arterial Blood Gas showed pH 7.44, PaCO2 32.2 mmHg, PaO2 45 mmHg; Fibrinogen 5.59 g/L, D-dimer 2.41 mg/L. Her blood cell count, procalcitonin and brain natriuretic peptide were in normal range.
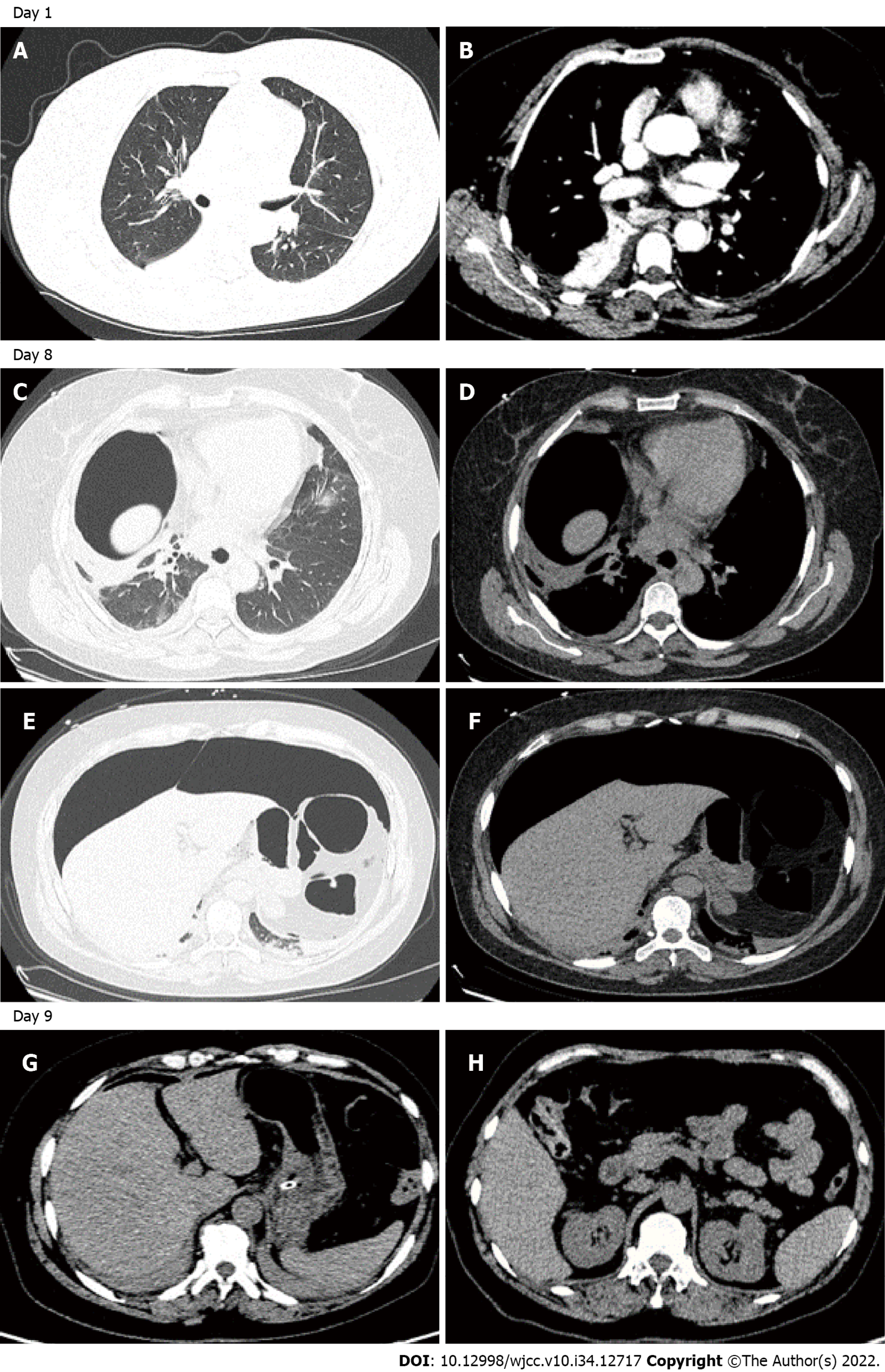
Her chest computer tomography (CT) showed infiltrates in the bilateral pulmonary lobes, localized consolidation in the right lower pulmonary lobe, and bilateral basal pleural effusions (Figure 1A and B).
Community-acquired pneumonia.
She was treated with Amoxicillin-clavulanate 1.2 g every eight hours for one week. Sputum cultures were obtained prior to antibiotic treatment and were not found to be positive. And as the patient did not have a high fever on admission, no blood culture was obtained. On the 8th day of her admission, a bronchoscopy was arranged for bronchial-alveolar lavage to detect the possible pathogens in the lower respiratory tract. Local anesthesia was initially administered with lidocaine 2% aerosol inhalation for 30 min. Midazolam 3 mg was injected intravenously 1 min before the operation, and oxygen was supplied via a 12 F nasopharyngeal cannula (NPC), approximately 5-6 cm from the tip of the catheter to the nostril, with the oxygen flow rate of 5-10 L/min. Preoperative vital signs were BP 125/86 mmHg, pulse 90 bpm, RR 16 bpm, SpO2 88% (with NPC 5 L/min). After four minutes of bronchoscopy, the patient suddenly vomited 20 mL of water, followed by severe abdominal pain. Vital signs were BP 195/91 mmHg, pulse 135 bpm, RR 25 bpm, SpO2 89%. She was immediately given nimodipine, and the flow of oxygen was increased to 15 L/min, with consideration of treatment in the intensive care unit, including ventilator management. Physical examination revealed obvious abdominal distension, as well as hardness and tenderness of the whole abdomen. Pneumoperitonium was considered and the bronchoscopy was stopped immediately, followed by emergency decompression by inserting a gastric tube for gastrointestinal (GI) decompression. Ultrasound of the abdomen indicated a tension pne
The subsequent clinical course was uneventful. Her bronchoalveolar lavage fluid sample was negative for metagenomic next generation sequencing (mNGS), ruling out corona virus disease 2019, tuber
Pneumoperitonium was a rare complication during bronchoscopy. We searched Pubmed data base and found only eight cases were reported during the last 20 years. As shown in Table 1, eight previously published cases and the current case with pneumoperitonium during bronchoscopy were reviewed. A total of nine cases were reported, including eight adults and one child. 22% (2/9) of the patients had pneumoperitonium during rigid bronchoscopy, while 78% had it at fiberoptic bronchoscopy. Four patients (44%) underwent transbronchial lung biopsy (TBLB) or transbronchial needle aspiration (TBNA). NPC was the most common oxygen supply method in six patients (66%), while the remaining one and two patients used a bag mask and mechanical ventilation (MV), respectively. In addition, sudden onset of abdominal pain or distension was the most common clinical presentation, as shown in three and five patients, respectively. However, a cardiorespiratory arrest was present in one case. Only 4 (44%) patients had isolated pneumoperitonium, and pneumothorax/pneumomediastinum were complicated with pneumoperitonium in the other 5 cases. Most of the reported cases were tension pneumoperitonium. Hypotension and respiratory failure were also present in five cases. Six patients were intubated after pneumoperitonium, while only one patient died after pneumoperitonium and the other eight recovered well. Four patients had laparotomy/laparoscopy, and gastric ruptures were found in only 3 cases.
| Ref. | Age | Sex | BSP type | Biopsy procedure | O2 supply | Symptoms during BSP | PT or PM | Isolated PP | Tension PP | Respiratory or hemodynamic failure | Intubaion and MV | Viscus rupture | Laparotomy or Conservative treatment | Outcome |
| Nikolaev et al[1], 2003 | 82 | F | Fiberoptic | TBLB | NPC | Sudden stuporotic bradycardic | PT + PM | No | Yes | No | Intubation air-bag | No | Laparoscopy | Discharged 3 d later |
| Abraham et al[2], 2011 | 76 | F | Fiberoptic | TBNA | NPC | Abdominal pain | PM | No | Yes | No | No | No | Conservative observation in ICU | Discharged 2 d later |
| Dastidar[5], 2013 | 14 mo | M | Rigid | Foreign body removal | MV | Distended abdomen | PT + PM | No | No | No | Aborted | No | Conservative observation in ICU | Discharged 1 d later |
| Bednarz et al[8], 2015 | 42 | F | Rigid | No | Bag mask | Respiratory arrest distended abdomen | No | Yes | Yes | RF and shock | Intubation | Gastric rupture | Emergent laparotomy | Recovered |
| El-kersh and Karnib[3], 2017 | 61 | F | Fiberoptic | No | NPC | Abdominal pain tachycardia tachypnea | No | Yes | Yes | RF | Intubation | Gastric rupture | Emergent laparotomy | Recovered |
| Muriana et al[6], 2018 | 80 | M | Fiberoptic | EBUS TBNA | NPC | Distended abdomen severe bradycardia arterial hypotension | No | Yes | Yes | RF and shock | Intubation | No | Needle decompression | Discharged 13 d later |
| Po et al[4], 2021 | 80 | M | Fiberoptic | BALF | MV | Distended abdomen persistent hypotension | PM | No | Yes | Shock | Intubation | NA | Refused laparotomy by family | Died |
| Pereira et al[9], 2021 | 61 | F | Fiberoptic | No | NPC | Sudden abdominal distension; cardiorespiratory arrest | PT + PM | No | Yes | RF and shock | Bag-mask ventilation & intubation | Gastric laceration | Needle decompression exploratory laparotomy | Discharged 4 d later |
| This case | 51 | F | Fiberoptic | No | NPC | Abdominal pain | No | Yes | Yes | No | No | No | Needle decompression | Discharged 5 d later |
| In summary | 42-82 yr | F 6 M 3 | Fiberoptic 7 Rigid 2 | TBLB 1 TBNA 2 Foreign body 1 | NPC 6 MV 2 bag mask 1 | Abdominal pain 3 Distended abdomen 5 hypotension 2 cardiorespiratory arrest 1 | PT + PM 3 PM 2 No 4 | No 5 Yes 4 | Yes 9 No 1 | RF + shock 3 RF 1 Shock 1 No 4 | Intubation 6 No 2 | Gastric rupture 3 No 6 | Conservative observation 2 Laparotomy 4 Needle decompression3 | Discharged 8 Died 1 |
The mechanism of pneumoperitonium during bronchoscopy is manifested by high-pressure air in the ruptured airway, alveoli, or hollow viscus[5,8,9]. In some cases, such as rigid bronchoscopy[5,8], TBLB[1], TBNA[2,6], or foreign body removal[5], pneumoperitonium occurs as an intro-airway procedural complication. Damage to the airway or the alveoli may occur due to these procedures, leading to pneumoperitonium[10]. Also, pneumothorax and pneumomediastinum could be found more frequently in these types of pneumoperitonium[11-15]. Additionally, the “Macklin” effect is one of the mechanisms related to pneumothorax or pneumomediastinum complicated with pneumoperitonium[16].
Isolated pneumoperitonium without complicated pneumothorax or pneumomediastinum is more likely to be associated with an air source from the lesion of GI tract[3,8]. However, one previously reported case showed that isolated pneumoperitonium could also be seen after TBNA[6]. Therefore, when isolated pneumoperitonium was present during bronchoscopy without an intro-airway procedure, it should be considered that there is a high possibility that the pneumoperitonium is of GI source. It was described[17] that some patients undergoing bronchoscopy under sedation and oxygen delivery by NPC experienced the development of pneumoperitoneum secondary to gastric rupture due to multiple factors, such as the reduced muscle tone in the pharynx induced by anesthesia, and thus air entering the stomach with one-way valve mechanism, resulting in NPC dislocation in the esophagus. With these risk factors, the large amounts of air supplied by the oxygen supply tube may enter the GI tract, inducing high air pressure in the hollow viscus and eventually leading to perforation at its most vulnerable site of the gastriointestinal wall. And it was speculated that when the perforation occurs in the ventral side of the GI tract, and most patients have very little content left in the GI tract after the bronchoscopy preparation, air could be the only substance that leaks into the peritoneum, with no other GI content entering into the peritoneum and causing peritonitis.
Tension pneumoperitonium was reported in the majority of the cases we reviewed, and in more than half of these cases there was acute circulatory or respiratory failure[3,4,6,8] or cardiopulmonary arrest[9], which may lead to a fatal outcome[18]. The initial step in treatment should be prompt resuscitation and life support. Tension barotrauma should be confirmed by radiological examination as soon as possible after the patient's vital signs have stabilized. At the same time, a needle or tube decompression should be considered for a better venous return and respiratory compliance, which could further improve the cardiopulmonary status. If a tension pneumoperitonium is caused by gastric or intestinal microperforation, showing only pneumoperitoneum during bronchoscopy without signs of peritonitis, non-surgical pneumoperitonium should be considered, and it could be cured by a needle or tube decompression[6].
Only four out of the nine patients with pneumoperitonium eventually underwent laparotomy or laparoscopy in our review. Three of the patients who underwent laparotomy that were confirmed gastric rupture but got repaired and recovered well, while the other patient died when his family refused the laparotomy. In addition to this, four patients who were radiologically found negative to have visceral rupture were closely monitored and eventually diagnosed with NSP and recovered with conservative therapy. Therefore, it should always be borne in mind that NSP is a form of pneumoperitonium complicated with bronchoscopy, for which surgical procedure could be avoided with a good outcome[6,7,19].
High flow oxygen supply or high positive pressure ventilation maybe a significant cause of pneumoperitonium during bronchoscopy[20]. Besides, mechanical ventilation, bag-mask ventilation, and high flow NPC have also been reported as causes of pneumoperitonium in other clinical circumstances, such as sedation or surgical procedures[14,20]. NPC was considered the most probable cause of isolated pneumoperitonium during bronchoscopy without biopsy in three cases, based on our review of previous cases, including the case we report here. Therefore, clinicians should be aware of the risk of pneumoperitonium when a high flow NPC oxygen supply is used during bronchoscopy and should monitor this complication closely during the procedure. And furthermore, not only should cardiopulmonary monitoring and resuscitation kits be prepared, but decompression kits should be prepared at the bedside during bronchoscopy for high-risk patients undergoing, for example, high flow NPC, positive ventilation, deep sedation, and invasive procedures. And when using NPC oxygenation, confirm the position of the catheter.
A protocol for the management of pneumoperitonium during bronchoscopy is proposed in Figure 2, based on the features of the case series reviewed and our case reported.
In summary, due to the serious clinical consequences, attention should be paid to the possibility of tension pneumoperitonium during bronchoscopy while the unstable cardiopulmonary status should be treated immediately. And meanwhile, varied treatments could be adopted according to whether pneumoperitonium is complicated with pneumothorax or pneumomediastinum, and whether there are signs of persistent peritonitis. When NSP is considered, conservative therapy maybe a reasonable option with good recovery. Furthermore, patients at high risk should be closely monitored.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Agrawal P, United States; Ferreira GSA, Brazil; Ishida T, Japan S-Editor: Wei ZH L-Editor: A P-Editor: Wei ZH
| 1. | Nikolaev IS, Zamir D, Weiler Z. Pneumoperitoneum complicating bronchoscopy. Isr Med Assoc J. 2003;5:131-132. [PubMed] |
| 2. | Abraham GE 3rd, Sumrall BH, Bowling MR. The air apparent: a rare complication during flexible bronchoscopy. Am J Med Sci. 2011;341:243-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | El-Kersh K, Karnib H. Tension Pneumoperitoneum Associated with Nasopharyngeal Catheter Oxygen Delivery during Bronchoscopy. Am J Respir Crit Care Med. 2017;196:785-786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Po PL, Bai HF, Lin CH, Lin CC. Pneumomediastinum that progression to tension pneumoperitoneum after bronchioloalveolar lavage: A case report. Respir Med Case Rep. 2021;32:101341. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 5. | Dastidar A. Pneumomediastinum, pneumoperitoneum and pneumothorax following iatrogenic perforation of bronchus: successful conservative management of a potentially serious complication. J Pediatr Surg. 2013;48:456-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Muriana P, Carretta A, Ciriaco P, Rossetti F, Negri G. Isolated tension pneumoperitoneum following endobronchial ultrasound-guided transbronchial needle aspiration complicated by cardiac peri-arrest: A case report. Monaldi Arch Chest Dis. 2018;88:999. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Ahmed K, Amine EG, Abdelbaki A, Jihene A, Khaoula M, Yamina H, Mohamed B. Airway management: induced tension pneumoperitoneum. Pan Afr Med J. 2016;25:125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Bednarz S, Filipovic M, Schoch O, Mauermann E. Gastric rupture after bag-mask-ventilation. Respir Med Case Rep. 2015;16:1-2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Pereira IS, Ferreira L, Tinoco E, Shiang T, Oliveira A, Pereira AI. Gastric rupture during fiberoptic bronchoscopy, a rare complication of oxygen administration by nasopharyngeal cannula: a case report. Braz J Anesthesiol. 2021;1-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Mancino L, Michieletto L, Trani B, Zamperlin A, Ceron L. Pneumomediastinum after transbronchial lung biopsy. J Bronchology Interv Pulmonol. 2010;17:167-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Naughton M, Irving L, McKenzie A. Pneumomediastinum after a transbronchial biopsy. Thorax. 1991;46:606-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Lantsberg L, Rosenzweig V. Pneumomediastinum causing pneumoperitoneum. Chest. 1992;101:1176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Kourounis G, Lim QX, Rashid T, Gurunathan S. A rare case of simultaneous pneumoperitoneum and pneumomediastinum with a review of the literature. Ann R Coll Surg Engl. 2017;99:e241-e243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Fraipont V, Lambermont B, Ghaye B, Moonen M, Edzang L, D'Orio V, Marcelle R. Unusual complication after percutaneous dilatational tracheostomy: pneumoperitoneum with abdominal compartment syndrome. Intensive Care Med. 1999;25:1334-1335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Madan K, Mehta S, Gupta N, Hadda V, Mohan A, Guleria R. Pneumomediastinum and Extensive Subcutaneous Emphysema after Cryoprobe Transbronchial Lung Biopsy. Ann Am Thorac Soc. 2016;13:2101-2103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Romero KJ, Trujillo MH. Spontaneous pneumomediastinum and subcutaneous emphysema in asthma exacerbation: The Macklin effect. Heart Lung. 2010;39:444-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Giménez Velando A, Rodriguez Nieto MJ, Flandes Aldeyturriaga J. Gastric Perforation During Bronchoscopy For The Delivery Of Oxygen Therapy By Nasopharyngeal Cannula. Arch Bronconeumol (Engl Ed). 2018;54:293-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 18. | Gross A, Diacon AH. Cardiac tamponade following transbronchial needle aspiration. Respiration. 2011;82:56-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Mularski RA, Sippel JM, Osborne ML. Pneumoperitoneum: a review of nonsurgical causes. Crit Care Med. 2000;28:2638-2644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 163] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 20. | Chapman N. Gastric rupture and pneumoperitoneum caused by oxygen insufflation via a fiberoptic bronchoscope. Anesth Analg. 2008;106:1592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |